Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Aggressiveness of Cancer Care at End of Life in Patients with Metastatic Breast Cancer in Jordan
Authors Abunasser M , Abu-Fares H, Abdel-Razeq S, Shamieh O, Salama O, Ashouri K, Al Qudah A , Taqash A , Abu-Jaish H, Saadah SS , Abdel-Razeq H
Received 16 June 2023
Accepted for publication 22 August 2023
Published 26 September 2023 Volume 2023:16 Pages 2873—2881
DOI https://doi.org/10.2147/JMDH.S422391
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mahmoud Abunasser,1– 3 Hala Abu-Fares,1 Sarah Abdel-Razeq,2 Omar Shamieh,2,3 Osama Salama,1 Khaled Ashouri,1 Abdullah Al Qudah,1 Ayat Taqash,4 Hala Abu-Jaish,5 Salwa S Saadah,1,2 Hikmat Abdel-Razeq1,2
1Department of Internal Medicine, King Hussein Cancer Center, Amman, Jordan; 2School of Medicine, the University of Jordan, Amman, Jordan; 3Department of Palliative Medicine, King Hussein Cancer Center, Amman, Jordan; 4Office of Scientific Affairs and Research, King Hussein Cancer Center, Amman, Jordan; 5School of Medicine, Jordan University of Science and Technology, Irbid, Jordan
Correspondence: Hikmat Abdel-Razeq, Department of Internal Medicine, King Hussein Cancer Center, 202 Queen Rania Al Abdullah Street, P.O. Box: 1269, Amman, 11941, Jordan, Tel +962-6 5300460, Ext: 1000, Email [email protected]
Background: Contrary to Western societies, more than 15% of patients with breast cancer in Jordan are diagnosed with stage IV disease. In this study, we evaluate the value of early palliative care integration in the end-of-life care of such patients.
Methods: All consecutive adult patients who died between 2014 to 2018, while under the care of our institution, with a confirmed diagnosis of breast cancer at the time of death, irrespective of place of death, were retrospectively reviewed.
Results: During the study period, a total of 433 patients, median age 51.6 years, were included in the analysis. Among the whole group, 102 (23.6%) were referred to palliative care service early (≥ 30 days prior to death), 182 (42.0%) had late referral (< 30 days from death), while 149 (34.4%) were never referred and were followed up by their medical oncologists. During the last 30 days prior to death, patients who were never referred to palliative care were more likely to visit the Emergency Room (ER) more than once (OR 1.89, 95% CI 1.20– 2.99, p = 0.006), more likely to be admitted to the hospital more than once (OR 2.27, 95% CI 1.38– 3.73, p = 0.001), and more likely to be admitted to the intensive care unit (ICU) (OR 3.07, 95% CI 1.48– 6.38, p = 0.0027). Fewer patients in the “no referral” group died with advance directives compared to those who had early or late referral; 60.8%, 75.0% and 82.5%, respectively, p = 0.0003. Survival of patients followed by medical oncologist was not better than those referred to palliative care, either late or early; median survival was 19.0, 19.1 and 23.8 months, respectively (p = 0.2338).
Conclusion: Findings suggest that earlier palliative care referral is associated with less aggressive end-of-life care, leading to less frequent ER visits, hospital and ICU admissions during the last month of life, and does not compromise survival.
Keywords: metastatic breast cancer, palliative care, end-of-life, Do not resuscitate, DNR
Introduction
With over 2.3 million new cases and 685,000 deaths from breast cancer in 2020, breast cancer continues to be the most commonly diagnosed cancer worldwide.1,2 Similar data and trends are observed in Jordan; more than 1400 new cases of breast cancer are diagnosed among Jordanians annually, and another 300 patients are treated in local hospitals from non-Jordanians living in the country or just visiting for cancer care.3 However, contrary to Western countries, more than 15% of patients are diagnosed with stage IV disease.4,5
The King Hussein Cancer Center (KHCC) is a comprehensive cancer center in Jordan, it treats over 6000 new cancer patients each year, from Jordan and the region. An inpatient palliative care consultation service was started at KHCC, as early as 2004; it was later expanded to offer outpatient palliative care for all patients regardless of their stage of disease, while hospice and home care were offered for patients with an estimated life expectancy of 6 months or less. Hospice and palliative care are delivered by a well-coordinated interdisciplinary team composed of physicians, nurses, social workers, clinical pharmacists and psychologists, and is available for all cancer patients.6
Breast cancer, especially for those with hormone receptor-positive subtypes, can be viewed as a chronic illness; it’s not unusual for patients to be treated with over 10 lines of therapy. However, a good percentage of patients may progress, despite all available therapies, and reach a stage where major decisions on further directions need to be taken. Many studies have suggested that if such decisions are left for patients to make, many would choose to receive aggressive therapy, with its associated major toxicities and potential limited benefit, despite their clinicians’ recommendations.7
The treatment of cancer patients, including those with breast cancer, near death is becoming increasingly aggressive over time.8–10 The past decade has witnessed the introduction of many new anticancer drugs, most are utilized in advanced-stage settings of breast cancer, including endocrine therapy,11–14 immunotherapy,15 and many targeted therapies,16 and more recently the antibody-drug conjugates (ADC),17–19despite the fact that many such therapies have limited benefits in refractory cases and are associated with significant adverse events, adding to the financial burden on patients, relatives and the healthcare system at large. Also, the over-utilization of such therapies will result in the delay of palliative and hospice referrals.
Breast cancer patients may have multi-dimensional needs, related to the physical, social, psychological and spiritual, that can be addressed with the integration of palliative services in their care throughout the disease trajectory. Patients with breast cancer may face significant impaired function and overall symptom burden especially in advanced stages.20
Several studies have found that the integration of palliative care early during the course of the disease has a favorable impact on aggressiveness of cancer care at end-of-life. Several indicators were utilized to assess this issue including chemotherapy use, emergency room (ER) visits and hospitalization to regular in-patient and intensive care units (ICU).21–25 Studies have shown that palliative chemotherapy in the last months of life is associated with more aggressive end-of-life care, such as ER visits and ICU admissions.26–30
The integration of palliative care for all patients with advanced cancer has been recommended early in the course of the disease and during the medical treatment.31,32 The early integration is crucial, especially in countries with limited resources, like ours, and should be linked to local clinical practice guidelines (CPG) and process and outcome key performance indicators (KPI).20
In this study we aim to assess the service utilization and the impact of palliative care service integration among breast cancer patients managed during the last 30 days before death.
Methods
This is a retrospective review of electronic medical records, conducted at King Hussein Cancer Center, the largest tertiary cancer institution in the country of Jordan. All adult patients’ charts with a confirmed diagnosis of breast cancer, who were treated and followed up at our institution, were extracted. All patients aged 18 years or older, who died between January 1st, 2014 and December 31st, 2018, and had a diagnosis of breast cancer at the time of death irrespective of place of death were included. Patients with more than one primary tumor and those who were impossible to follow up were excluded.
Data extracted included demographic data; age, gender, stage of disease at the time of diagnosis and at the time of death, treatment received, referral status to palliative care, place of death and presence or absence of advanced directives at the time of death including DNR status. Staging was obtained from the charts for all patients based on scan results and tissue diagnosis.
The study variables related to aggressiveness of care at end-of-life were evaluated utilizing 3 indicators: chemotherapy administration, number of ER visits, and hospitalization to regular units or ICU during the last 30 days of life. Additionally, exposure to palliative care services and its timing were recorded.
According to exposure to palliative care services; patients were divided into 3 groups. The first group was the “early referral” group, defined as those referred by their oncologists to palliative care service more than 30 days before death. The second group are the “late referral” group, defined as referral less than 30 days before death, both groups were followed by the palliative care team and their simultaneous follow-up with a medical oncologist was kept as needed, while the third group are the “no referral” group, who are those who were never referred to palliative care, and continued their treatment and follow up under the care of medical oncology services.
The study was approved by the Institutional Review Board (IRB) at King Hussein Cancer Center. Because of the retrospective nature of the study and lack of identifiers, a waiver of informed consent was obtained.
Statistical Analysis
In this study, patients’ characteristics are presented as counts and percentages, for categorical variables or mean and range for continuous variables. The median time from the referral to palliative care until patients’ death was calculated. Rate of chemotherapy use, visits to ER, admission to regular hospital units or ICU during the last 30 days were recorded. To analyze the treatment outcomes and hospital visits and admission, all patients were categorized based on timing of the referral to palliative care as early referral, late referral or no referral to palliative care. To compare the different groups, we used Chi-square test or Fisher’s exact test for categorical data and the Student’s t-test or non-parametric test for continuous variables, depending on the assumptions required for each test.
The overall survival (OS) time was calculated from the date of diagnosis to the date of death from any cause and survival was expressed as median with a 95% confidence interval. The Kaplan-Meier method was used to estimate OS curves and Log rank test was used to compare patients’ survival times between different groups based on factors like the timing of palliative care referral. A significance criterion of p ≤ 0.05 was used in all statistical analysis, indicating that results with a p-value of less than or equal to 0.05 were considered statistically significant. All analyses were performed using SAS version 9.4 (SAS Institute Inc, Cary, NC).
Results
During the study period, between January 1st, 2014 and December 31st, 2018, a total of 433 patients were included in the analysis. Median age was 51.6 (range, 18.7–95.7) years; only 85 (19.6%) were 65 years or older and except for 3 male patients, all were female patients. Due to the limited number of male cases during the study interval. At their first presentation, 224 (51.7%) had de novo metastatic disease while the rest had distant disease or disease recurrence during the course of their follow up, Table 1.
 |
Table 1 Patients’ Characteristics (n = 433) |
Pattern to Palliative Care Referral
In total, 102 (23.6%) patients were referred early, 182 (42.0%) referred late, while 149 (34.4%) patients were never referred to palliative care and continued their treatment and follow up under the care of medical oncology services. Patients in the last group were younger than those referred to palliative care; median age of 50.0 compared to 56.3 years, p = 0.02.
Treatment During the Last 30 Days
During the last 30 days of patients’ lives, none of the patients who were referred and followed by palliative care had chemotherapy, while 43 (28.9%) of the patients treated by their medical oncologists, and who were never referred to palliative care, were on active treatment with chemotherapy.
During the last 30 days of life, the “no referral” group were more likely to visit the ER more than once (OR 1.89, 95% CI 1.20–2.99, p = 0.006), more likely to be admitted to the hospital more than once (OR 2.27, 95% CI 1.38–3.73, p = 0.001), and more likely to be admitted to the ICU (OR 3.07, 95% CI 1.48–6.38, p = 0.0027, Table 2.
 |
Table 2 Hospitalization and ER Visits During the Last 30 Days |
Advance Directives
At time of death, 283 (74.7%) patients had advance directives and were placed as “Don’t resuscitate” (DNR). The percentage of patients who died with a DNR order varied across the 3 groups. Fewer patients in the no referral group died with DNR orders compared to those who had early or late referral; 60.8%, 75.0% and 82.5%, respectively, p = 0.0003, Table 3.
 |
Table 3 Differences Between the Three Groups According to Referral Pattern |
Place of Death
Regardless of DNR status, or time of referral to palliative care; only 44 patients (10.2%) died at home, while the majority of the deaths (n = 389, 89.8%) occurred in the hospital, nevertheless the preferred place of death was not reported in advanced directives.
Overall Survival
Patients with de novo metastatic breast cancer had worse overall survival compared to those with distant disease recurrence; 12.7 (95% CI = 11.2–15.2) months versus 29.7 (95% CI = 25.4–33.4) months, p < 0.0001 (Figure 1). However, no difference in survival, was observed between those who were managed by their medical oncologists, who were never referred to palliative care, and those who had early or late referral to palliative care; median overall survival and 95% confidence intervals were 19.0 (18.6–19.2), 23.8 (16.3–21.9) and 19.1 (15.2–23.5), respectively, p = 0.2338 (Figure 2).
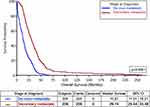 |
Figure 1 Overall survival of patients with de novo metastasis versus those with secondary metastasis. |
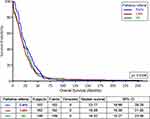 |
Figure 2 Overall survival according to referral to palliative care. |
Discussion
Studies carried out to evaluate the aggressiveness of care and use of chemotherapy for patients with breast cancer at end-of-life, especially in our region, are scarce. To our knowledge, this is the first study from the region which attempted to objectively evaluate and address the impact of palliative care referral, and its timing, on the outcome of patients with advanced-stage breast cancer. In the mind of many patients, relatives, and occasionally their oncologists, abandoning chemotherapy and referral to palliative care signals the end of the curative strategy and may lead to the shortened survival of such patients. Administration of chemotherapy or immunotherapy during the last few days of a patients’ life may not significantly contribute to their survival or overall quality of life. Our study clearly demonstrated that patients who were managed solely by their medical oncologists, never referred to palliative care services, and received chemotherapy, had comparable overall survival to those who were managed by the palliative care team without receiving active anticancer therapy. Several other studies had shown that palliative chemotherapy at end-of-life, was significantly associated with more ER visits, ICU admissions, endotracheal intubation and cardiopulmonary resuscitation.26,28,29
Though our patients were younger than those usually seen in Western societies, less than 10% of the whole cohort received any chemotherapy during the last 30 days before death, which may reflect positively on the good understanding of practicing oncologists and the value of “quality of life” in these patients and the maturity and effective integration of our palliative care services into oncology care.
Many factors may influence the use of palliative chemotherapy in these settings. Good communications between the treating oncologists and the patient and family members to outline the expectations and treatment goals, can obviously minimize aggressive interventions including the administration of chemotherapy. Active treatment with chemotherapy may give the patient, and the family, a false perception about the curability of the disease and may give them a “false hope”.33 Physicians may occasionally overestimate expectations, and even prognosis, which obviously improves with experience.34,35
Due to local social norms and family acceptance of home end-of-life care, almost 90% of our patients died at the hospital, regardless of utilization of palliative care services, DNR status or time of referral, which was similar to national trends.36 This is contrary to what is observed in Western societies. In an analysis of cancer patients using Medicare data from 2003 to 2010, only a quarter of deaths occurred in the hospital.37 The high rate of hospital death might be due to lack of community palliative care services and the lack of nursing home and hospices in Jordan in addition to the limited home care coverage or national hospice policy.36 Although our center offers home care services, these services are not available after working hours. In addition, the cost of a hospital stay for cancer patients is covered by the public insurance for all Jordanians including end-of-life care.
Many studies have shown that a considerable portion of cancer-treatment related cost is accrued during the last few months of a patients’ life. Many such studies were performed even before the introduction of very costly medications recently approved for advanced-stage breast cancer.38–40 In healthcare systems, where patients are required to contribute to this cost; even partially, financial hardship can be a serious issue that may reflect negatively on patients’ wellbeing. A questionnaire-based study tried to address the indirect costs of palliative care in end-stage cancer and concluded that more attention should be paid to home care and caregiver support to reduce inpatient care needs and control the costs of end-of-life care. Nevertheless, patients with aggressive care at end-of-life will impose higher costs compared to patients receiving less aggressive care.41
Our results suggest that earlier palliative care referral is associated with less aggressive end-of-life care, leading to less frequent ER visits, hospital and ICU admissions during the last month of life. A population-based cohort study of cancer decedents found that homecare nursing with palliative intent may decrease the need for dying cancer patients to visit the ER, for both high and low-acuity visits, compared to receiving general homecare nursing.42
A previous published study in Jordan concluded that younger patients and those with hematological malignancies were more likely to receive chemotherapy, whereas those referred to palliative care were significantly less likely to receive chemotherapy at the end-of-life.43 We found almost similar data as oncologists tend to refer elderly patients to palliative care.
Our study is not without limitations; though our center is the only tertiary referral cancer center in Jordan and treats over half of all cancer patients in the country, the data presented represents the treatment strategy of a single institution and might not reflect on the whole country. Additionally, we have not looked at the length of hospital stay across the 3 groups of patients addressed in this paper, which might have overestimated utilization especially for the palliative group. Given the retrospective nature of our study, we were not able to capture and address important variables that may affect decisions to accept palliative care referral including patients’ social setup,42 income, educational level and the effect of the many recently introduced anti-cancer therapies, including immunotherapy. We have also not assessed other disease burdens and the presence of comorbidities. A larger number of patients, in various care settings, are needed to better evaluate the issues under discussion.
Conclusions
Our study’s findings provide compelling evidence that the early integration of palliative care has significant positive impact on the quality of end-of-life care for cancer patients. Furthermore, these findings should be reflected upon to develop targeted policies that prioritize timely palliative care referrals and allocate resources to enhance community-based services. As the importance of palliative care gains recognition worldwide, further research should be encouraged to explore its long-term benefits and cost-effectiveness, facilitating the global dissemination of best practices and ultimately advancing the quality of care for cancer patients across different healthcare settings and cultural contexts.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Declarations
The study was approved by the Institutional Review Board (IRB) at King Hussein Cancer Center (approval number: 19 KHCC 64), and all procedures were performed based on the regulations of the Declaration of Helsinki. Given the retrospective nature of the study and lack of patients’ identifiers, consent to participate was waived by the IRB.
Consent for Publication
Data submitted are entirely unidentifiable, and there are no details on individuals reported within the manuscript.
Acknowledgments
The abstract of this paper was presented in-part at the annual meeting of the European Society of Medical Oncology (ESMO) held on 16-21 September, 2021 as a poster presentation with interim findings.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was not funded.
Disclosure
The authors declared that they have no conflicting interest in this work.
References
1. Arnold M, Morgan E, Rumgay H, et al. Current and future burden of breast cancer: global statistics for 2020 and 2040. Breast. 2022;66:15–23. doi:10.1016/j.breast.2022.08.010
2. Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
3. Abdel-Razeq H, Mansour A, Jaddan D. Breast Cancer Care in Jordan. JCO Glob Oncol. 2020;6:260–268. doi:10.1200/JGO.19.00279
4. Breast Cancer. American Cancer Society. Available from: https://www.cancer.org/cancer/breast-cancer.html.
5. Ministry of Health: cancer incidence in Jordan; 2015. Available from https://www.moh.gov.jo/Pages/viewpage.aspx?pageID=240.
6. Shamieh O, Hui D. A comprehensive palliative care program at a tertiary cancer center in Jordan. Am J Hosp Palliat Care. 2015;32(2):238–242. doi:10.1177/1049909113513316
7. Matsuyama R, Reddy S, Smith TJ. Why do patients choose chemotherapy near the end-of-life? A review of the perspective of those facing death from cancer. J Clin Oncol. 2006;24(21):3490–3496. doi:10.1200/JCO.2005.03.6236
8. Earle CC, Neville BA, Landrum MB, Ayanian JZ, Block SD, Weeks JC. Trends in the aggressiveness of cancer care near the end of life. J Clin Oncol. 2004;22(2):315–321. doi:10.1200/JCO.2004.08.136
9. Luta X, Maessen M, Egger M, Stuck AE, Goodman D, Clough-Gorr KM. Measuring intensity of end of life care: a systematic review. PLoS One. 2015;10(4):e0123764. doi:10.1371/journal.pone.0123764
10. Martins-Branco D, Lopes S, Canario R, et al. Factors associated with the aggressiveness of care at the end of life for patients with cancer dying in hospital: a nationwide retrospective cohort study in mainland Portugal. ESMO Open. 2020;5(6):e000953. doi:10.1136/esmoopen-2020-000953
11. Cristofanilli M, Turner NC, Bondarenko I, et al. Fulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2-negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): final analysis of the multicenter, double-blind, Phase 3 randomized controlled trial. Lancet Oncol. 2016;17(4):425–439. doi:10.1016/S1470-2045(15)00613-0
12. Goetz MP, Toi M, Campone M, et al. MONARCH 3: abemaciclib as initial therapy for advanced breast cancer. J Clin Oncol. 2017;35(32):3638–3646. doi:10.1200/JCO.2017.75.6155
13. Tripathy D, Im SA, Colleoni M, et al. Ribociclib plus endocrine therapy for premenopausal women with hormone-receptor-positive, advanced breast cancer (MONALEESA-7): a randomized phase 3 trial. Lancet Oncol. 2018;19(7):904–915. doi:10.1016/S1470-2045(18)30292-4
14. Hortobagyi GN, Stemmer SM, Burris HA, et al. Updated results from MONALEESA-2, a Phase III trial of first-line ribociclib plus letrozole versus placebo plus letrozole in hormone receptor-positive, HER2-negative advanced breast cancer. Ann Oncol. 2018;29(7):1541–1547. doi:10.1093/annonc/mdy155
15. Cortes J, Cescon DW, Rugo HS, et al. Pembrolizumab plus chemotherapy versus placebo plus chemotherapy for previously untreated locally recurrent inoperable or metastatic triple-negative breast cancer (KEYNOTE-355): a randomized, placebo-controlled, double-blind, phase 3 clinical trial. Lancet. 2020;396(10265):1817–1828. doi:10.1016/S0140-6736(20)32531-9
16. Baselga J, Cortés J, Kim SB, et al. Pertuzumab plus trastuzumab plus docetaxel for metastatic breast cancer. N Engl J Med. 2012;366(2):109–119. doi:10.1056/NEJMoa1113216
17. Robson ME, Tung N, Conte P, et al. OlympiAD final overall survival and tolerability results: olaparib versus chemotherapy treatment of physician’s choice in patients with a germline BRCA mutation and HER2-negative metastatic breast cancer. Ann Oncol. 2019;30(4):558–566. doi:10.1093/annonc/mdz012
18. Modi S, Saura C, Yamashita T, et al. Trastuzumab Deruxtecan in Previously Treated HER2-Positive Breast Cancer. N Engl J Med. 2020;382(7):610–621. doi:10.1056/NEJMoa1914510
19. Verma S, Miles D, Gianni L, et al. Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med. 2012;367(19):1783–1791. doi:10.1056/NEJMoa1209124
20. Shamieh O, Alarjeh G, Li H, et al. Care Needs and Symptoms Burden of Breast Cancer Patients in Jordan: a Cross-Sectional Study. Int J Environ Res Public Health. 2022;19(17):10787. doi:10.3390/ijerph191710787
21. Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363(8):733–742. doi:10.1056/NEJMoa1000678
22. Maltoni M, Scarpi E, Dall’Agata M, et al. Systematic versus on-demand early palliative care: a randomised clinical trial assessing quality of care and treatment aggressiveness near the end of life. Eur J Cancer. 2016;69:110–118. doi:10.1016/j.ejca.2016.10.004
23. Temel JS, Greer JA, El-Jawahri A, et al. Effects of early integrated palliative care in patients with lung and GI cancer: a Randomized Clinical Trial. J Clin Oncol. 2017;35(8):834–841. doi:10.1200/JCO.2016.70.5046
24. Triplett DP, LeBrett WG, Bryant AK, et al. Effect of palliative care on aggressiveness of end-of-life care among patients with advanced cancer. J Oncol Pract. 2017;13(9):e760–e769. doi:10.1200/JOP.2017.020883
25. Scibetta C, Kerr K, Mcguire J, Rabow MW. The costs of waiting: implications of the timing of palliative care consultation among a cohort of decedents at a comprehensive cancer center. J Palliat Med. 2016;19(1):69–75. doi:10.1089/jpm.2015.0119
26. Wu CC, Hsu TW, Chang CM, Lee CH, Huang CY, Lee CC. Palliative chemotherapy affects aggressiveness of end-of-life care. Oncologist. 2016;21(6):771–777. doi:10.1634/theoncologist.2015-0445
27. Browner I, Carducci MA. Palliative chemotherapy: historical perspective, applications, and controversies. Semin Oncol. 2005;32(2):145–155. doi:10.1053/j.seminoncol.2004.11.014
28. Saito AM, Landrum MB, Neville BA, Ayanian JZ, Earle CC. The effect on survival of continuing chemotherapy to near death. BMC Palliat Care. 2011;10:14. doi:10.1186/1472-684X-10-14
29. Wright AA, Zhang B, Keating NL, Weeks JC, Prigerson HG. Associations between palliative chemotherapy and adult cancer patients’ end of life care and place of death: prospective cohort study. BMJ. 2014;348:g1219. doi:10.1136/bmj.g1219
30. Prigerson HG, Bao Y, Shah MA, et al. Chemotherapy Use, Performance Status, and Quality of Life at the End of Life. JAMA Oncol. 2015;1(6):778–784. doi:10.1001/jamaoncol.2015.2378
31. Ferrell BR, Temel JS, Temin S, et al. Integration of palliative care into standard oncology care: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2017;35(1):96–112. doi:10.1200/JCO.2016.70.1474
32. Kaasa S, Loge JH, Aapro M, et al. Integration of oncology and palliative care: a Lancet Oncology Commission. Lancet Oncol. 2018;19(11):e588–e653. doi:10.1016/S1470-2045(18)30415-7
33. Yennurajalingam S, Rodrigues LF, Shamieh O, et al. Perception of curability among advanced cancer patients: an international collaborative study. Oncologist. 2018;23(4):501–506. doi:10.1634/theoncologist.2017-0264
34. Amano K, Maeda I, Shimoyama S, et al. The accuracy of physicians’ clinical predictions of survival in patients with advanced cancer. J Pain Symptom Manage. 2015;50(2):139–46.e1. doi:10.1016/j.jpainsymman.2015.03.004
35. Hui D, Bansal S, Park M, et al. Differences in attitudes and beliefs toward end-of-life care between hematologic and solid tumor oncology specialists. Ann Oncol. 2015;26(7):1440–1446. doi:10.1093/annonc/mdv028
36. Guo P, Chukwusa E, Asad M, et al. Changing Mortality and Place of Death in Response to Refugee Influx: a Population-Based Cross-Sectional Study in Jordan, 2005-2016. J Palliat Med. 2021;24(11):1616–1625. doi:10.1089/jpm.2020.0476
37. Goodman DC, Morden NE, Chang CH, Fisher ES, Wennberg JE. Trends in Cancer Care Near the End of Life: A Dartmouth Atlas of Health Care Brief. Lebanon (NH): The Dartmouth Institute for Health Policy and Clinical Practice; 2013.
38. Santini D, Zeppola T, Russano M, et al. PD-1/PD-L1 checkpoint inhibitors during late stages of life: an ad-hoc analysis from a large multicenter cohort. J Transl Med. 2021;19(1):270. doi:10.1186/s12967-021-02937-9
39. Garrido MM, Prigerson HG. Chemotherapy use in the months before death and estimated costs of care in the last week of life. J Pain Symptom Manage. 2016;51(5):875–881.e2. doi:10.1016/j.jpainsymman.2015.12.323
40. Garrido MM, Balboni TA, Maciejewski PK, Bao Y, Prigerson HG. Quality of Life and Cost of Care at the End of Life: the Role of Advance Directives. J Pain Symptom Manage. 2015;49(5):828–835. doi:10.1016/j.jpainsymman.2014.09.015
41. Cheung MC, Earle CC, Rangrej J, et al. Impact of aggressive management and palliative care on cancer costs in the final month of life. Cancer N Cancer. 2015;121(18):3307–3315.
42. Karches KE, Chung GS, Arora V, Meltzer DO, Curlin FA. Religiosity, spirituality, and end- of- life planning: a single-site survey of medical inpatients. J Pain Symptom Manage. 2012;44(6):843–851. doi:10.1016/j.jpainsymman.2011.12.277
43. Abdel-Razeq H, Shamieh O, Abu-Nasser M, et al. Intensity of Cancer Care Near the End of Life at a Tertiary Care Cancer Center in Jordan. J Pain Symptom Manage. 2019;57(6):1106–1113. doi:10.1016/j.jpainsymman.2019.02.01
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
