Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 17
Age at Diagnosis of Diabetes in Young Men is Associated with Albuminuria
Authors Zhang Q , Cheng L, Li B, Lu Y, Yang S, Wu Y
Received 14 December 2023
Accepted for publication 26 March 2024
Published 4 April 2024 Volume 2024:17 Pages 1543—1549
DOI https://doi.org/10.2147/DMSO.S454867
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Antonio Brunetti
Qingqing Zhang,1,2,* Liang Cheng,3,* Boliang Li,4,* Yu Lu,1 Shufang Yang,1 Yucheng Wu5
1Department of Endocrinology, The Affiliated Taizhou People’s Hospital of Nanjing Medical University, Taizhou School of Clinical Medicine, Nanjing Medical University, Taizhou, Jiangsu, People’s Republic of China; 2Department of Pan-Vascular Management Center, The Affiliated Taizhou People’s Hospital of Nanjing Medical University, Taizhou School of Clinical Medicine, Nanjing Medical University, Taizhou, Jiangsu, People’s Republic of China; 3Department of Endocrinology, the Affiliated Huai’an Hospital of Xuzhou Medical University and the Second People’s Hospital of Huai’an, Huai’an, People’s Republic of China; 4Department of Nuclear Medicine, The Affiliated Taizhou People’s Hospital of Nanjing Medical University, Taizhou School of Clinical Medicine, Nanjing Medical University, Taizhou, Jiangsu, People’s Republic of China; 5Department of Cardiology, The Affiliated Taizhou People’s Hospital of Nanjing Medical University, Taizhou School of Clinical Medicine, Nanjing Medical University, Taizhou, Jiangsu, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Shufang Yang; Yucheng Wu, The Affiliated Taizhou People’s Hospital of Nanjing Medical University, Taizhou School of Clinical Medicine, Nanjing Medical University, 366 Taihu Road, Hailing District, Taizhou, Jiangsu, 225300, People’s Republic of China, Email [email protected]; [email protected]
Background: Early-onset diabetes appears to be an aggressive phenotype of type 2 diabetes (T2D). The impact of the age of onset of T2D on albuminuria, especially high urinary albumin excretion, remains to be investigated.
Objective: To determine whether adults diagnosed with T2D between the ages of 18 and 45 more aggressively develop albuminuria.
Methods: Conducted at Taizhou People’s Hospital from November 2018 to August 2020, this cross-sectional study enrolled T2D patients. Anthropometric measures, metabolic profiles, and urinary albumin creatinine ratio were examined. Patients were categorized into early-onset (≤ 45 years) and late-onset (> 45 years) groups. Univariate and multivariate analyses were performed to identify albuminuria risk factors. Subgroups were formed based on age at diabetes diagnosis and gender. Multivariate ordinal logistic regression analysis was then conducted to identify distinct risk factors within each subgroup.
Results: Analyzing 1900 T2D patients, it was found significantly higher albuminuria prevalence in early-onset patients (35.08% vs 29.92%, P = 0.022). The risk of albuminuria in early-onset patients was 1.509 times higher than that in late-onset patients, especially among male patients, where the risk increased to 1.980. For late-onset patients, disease duration and glycated hemoglobin (HbA1c) were identified as risk factors, whereas for early-onset patients, body-mass index (BMI) and systolic blood pressure were associated with increased risk. Among male patients, age at diagnosis of diabetes, blood pressure, and BMI were identified as risk factors, while for female patients, disease duration and HbA1c played a significant role. Additionally, high-density lipoprotein cholesterol was found to be a protective factor against albuminuria.
Conclusion: Individuals diagnosed with T2D before 45 face heightened albuminuria risk, especially males. Risk factors vary by gender and onset age, highlighting the need for tailored management strategies.
Keywords: diabetes complications, diabetes mellitus, type 2, albuminuria
A Letter to the Editor has been published for this article.
Introduction
In recent decades, the prevalence of diabetes mellitus, primarily type 2 diabetes (T2D), has been increasing worldwide.1,2 While much attention has been focused on elderly T2D patients, the recognition of T2D in young individuals has been insufficient. In recent years, there has been a trend of decreasing age at onset of T2D, leading to a rapid rise in early-onset cases.3–5 For these patients, early-onset T2D implies prolonged exposure to metabolic disorders and a higher risk of chronic diabetic complications.6,7 Accumulating evidence suggests that individuals with early-onset T2D experience a more aggressive disease course and often develop vascular complications in a relatively shorter duration compared to those with late-onset T2D.8,9
The impact of onset age of T2D on albuminuria, especially high urinary albumin excretion (UAE), remains to be investigated. However, determining the exact onset time of diabetes is challenging. Therefore, we explored whether the age at diagnosis of diabetes was a risk factor for albuminuria in patients with diabetes. Since age 45 is commonly used as a cutoff point for middle-aged and young individuals, and previous studies have examined the clinical complications of diabetes patients before or after this age,10 this study divided patients into two groups based on this age threshold. The subgroups were explored to determine whether the risk factors for albuminuria differed between patients diagnosed with diabetes before or after the age of 45 years.
Methods
Study Design and Population
This descriptive cross-sectional study enrolled subjects with T2D who underwent physical examinations at Taizhou People’s Hospital between November 2018 and August 2020. T2D was diagnosed according to the ADA criteria, and subjects between 18 and 85 years old were included. Exclusion criteria comprised: 1) type 1 diabetes and other special types of diabetes; 2) definite diagnosis of other types of chronic renal diseases such as membranous nephropathy or IgA nephropathy; 3) complications with urinary tract infection or hematuria; 4) acute complications of diabetes, such as diabetic ketoacidosis; 5) use of drugs affecting albuminuria, such as renin-angiotensin system inhibitors, sodium-dependent glucose transporters 2 inhibitors, and glucagon-like peptide-1 receptor agonists. The study was approved by the Taizhou People’s Hospital Ethics Research Committee and conducted in accordance with the principles of the Declaration of Helsinki.
A final cohort of 1900 individuals was recruited, all of whom provided informed consent. Subjects were categorized as early-onset and late-onset based on the age of diabetes diagnosis (≤ 45 and > 45 years, respectively). Repeated measurements of UAE were performed and analyzed. The random urinary albumin-to-creatinine ratio (uACR) was classified as follows: normal UAE (< 30 mg/g), moderate UAE (30–299 mg/g), or high UAE (≥ 300 mg/g).
Anthropometric and Biochemical Measurements
The following parameters were collected: age, gender, weight, height, waist circumference, hip circumference, age at diagnosis, disease duration, medical history of hypertension, smoking history, and medication usage. Blood pressure was measured twice using a mercury sphygmomanometer, and the mean systolic blood pressure (SBP) and diastolic blood pressure (DBP) were recorded. Body mass index (BMI) was calculated as weight (in kilograms) divided by height (in meters squared).
All venous blood samples were collected in the morning after an overnight fast to measure fasting plasma glucose (FPG), glycosylated hemoglobin (HbA1c), total cholesterol (TC), triglyceride (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and C-peptide in all participants. Oral glucose tolerance tests were administered to all patients, with serum glucose and C-peptide concentrations measured at 60 and 120 minutes after glucose loading. The trapezoidal rule was used to calculate the area under the curve for C-peptide (CAUC) and blood glucose (GAUC), with the C-peptide release index (CRI) calculated as CAUC/GAUC.
Statistical Analysis
Enumeration data were presented as n (%), and intergroup comparisons were conducted using the χ2 test. Continuous variables were expressed as median with interquartile ranges for non-normally distributed variables, and the independent sample t-test was used for group comparisons. Univariate analysis and multivariate ordinal logistic regression analysis were conducted to identify independent factors associated with the risk of albuminuria in patients with diabetes. Subgroups were categorized based on age at diabetes diagnosis and gender, with multivariate ordinal logistic regression analysis performed to identify different risk factors within each subgroup. Statistical analyses were conducted using SPSS version 24.0 (IBM Co., Armonk, NY, USA), with all tests being two-tailed and significance level set at P < 0.05.
Results
Characteristics of Study Population
A total of 1900 patients, including 1158 male and 742 female patients, were analyzed in this study based on data integrity (Table 1). Among these 1900 patients, 1298 cases had normal UAE (68.32%), 446 cases had moderate UAE (23.47%), and 156 cases had high UAE (8.21%). The median age at diagnosis for these patients was 49 years, with a mean diabetes duration of 7 years. Statistical differences were observed in age at diagnosis, age, disease duration, BMI, hip circumference, blood pressure, blood lipids, HbA1c, creatinine, and uACR levels among the three groups. However, there were no significant differences in waist circumference, gender, smoking status, or CRI among the three groups.
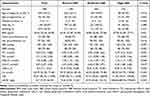 |
Table 1 Demographic Characteristics of the Patients with T2D Among Normal, Moderate and High UAE |
Risk Factors for Albuminuria in Patients with T2D
Fifteen variables, including age, disease duration, age at diagnosis, gender, smoking, BMI, waist circumference, hip circumference, SBP, DBP, CRI, TC, TG, HDL-C, and HbA1c, were selected through univariate analysis. Subsequently, eight factors with p < 0.05 in univariate analysis were included in multivariate logistic regression analysis. Finally, employing the statistical method of multivariate logistic regression analysis, the number of potential variables was reduced from eight to six, including disease duration, age at diagnosis, BMI, SBP, HDL-C, and HbA1c. The results of multivariate logistic regression analysis revealed that disease duration (OR = 1.049, 95% CI 1.020–1.080, P = 0.001), age at diagnosis (under 45 years old) (OR = 1.509, 95% CI 1.024–2.224, P = 0.038), BMI (OR = 1.100, 95% CI 1.032–1.172, P = 0.003), SBP (OR = 1.026, 95% CI 1.010–1.041, P = 0.001), and HbA1c (OR = 1.160, 95% CI 1.063–1.266, P = 0.001) were identified as risk factors for albuminuria in patients with T2DM (Table 2).
 |
Table 2 Risk Factors Associated with Albuminuria |
Risk Factors for Albuminuria in Patients with T2D in Subgroups
Due to the differing characteristics between individuals diagnosed with diabetes at a young age and those diagnosed at middle age or older, we further examined albuminuria-related risk factors within subgroups based on age at diagnosis. Among the 1900 patients, 1250 were diagnosed with diabetes after the age of 45, while 650 were diagnosed before the age of 45. The prevalence of albuminuria was 35.08% in patients diagnosed under 45 years old, compared to 29.92% in those diagnosed over 45 years old, with a statistically significant difference between the two groups (P = 0.022). Subgroup analysis revealed that in patients diagnosed over 45, disease duration (OR = 1.063, 95% CI 1.025–1.102, P = 0.001) and HbA1c (OR = 1.214, 95% CI 1.084–1.359, P = 0.001) were identified as risk factors. Meanwhile, for patients diagnosed under 45, BMI (OR = 1.182, 95% CI 1.054–1.327, P = 0.004) and SBP (OR = 1.061, 95% CI 1.031–1.092, P < 0.001) were found to be risk factors (Table 3).
 |
Table 3 Logistic Regression Analysis in Subgroups According to the Age of Diagnosis |
Subgroup analysis revealed that in female patients, disease duration (OR = 1.026, 95% CI 1.002–1.049, P = 0.030) and HbA1c (OR = 1.236, 95% CI 1.088–1.404, P = 0.001) were identified as risk factors, while HDL-C (OR = 0.101, 95% CI 0.013–0.771, P = 0.027) was found to be a protective factor. Conversely, for male patients, BMI (OR = 1.118, 95% CI 1.035–1.207, P = 0.005), SBP (OR = 1.036, 95% CI 1.013–1.060, P = 0.002), and age at diagnosis (under 45 years old) (OR = 1.980, 95% CI 1.168–3.356, P = 0.011) were identified as risk factors (Table 4).
 |
Table 4 Logistic Regression Analysis in Subgroups According to Gender |
Discussion
The prevalence of T2D among adolescents and young adults is sharply increasing, with distinct clinical complications observed in this demographic. In this population-based study, individuals diagnosed with T2D under the age of 45 exhibited a 1.509 times higher risk of moderate or high UAE compared to those diagnosed over the age of 45, with this risk increasing to 1.980 in male patients. Additionally, differences were observed in the risk factors for albuminuria between patients diagnosed with diabetes under 45 years old and those diagnosed above 45 years old. Specifically, disease duration and HbA1c were identified as risk factors for patients diagnosed over 45, while BMI and SBP were found to be risk factors for those diagnosed under 45.
In terms of the prevalence of albuminuria, a study on outpatients with T2D showed that 20.3% had moderate UAE and 6.7% had high UAE.11 This statistical results are similar: 23.5% of patients had moderate UAE and 8.2% had high UAE. A study in Wuhan showed that prevalence of albuminuria in early-onset and late-onset group was 30.6% and 24.5%, respectively, in inpatients with T2D.12 This study population consists of T2D patients in Taizhou, Jiangsu Province. It was found that the prevalence of albuminuria in patients with an age at diagnosis under 45 was higher than that in patients with an age at diagnosis over 45 (35.08% vs 29.92%). Wu et al demonstrated that young diabetes onset may amplify the effect of diabetes duration on the increased risk of chronic kidney disease.13 Early-onset diabetes appears to be an aggressive phenotypes of T2D. It seems that there are other factors that increase the risk of albuminuria in patients with early-onset diabetes. A study describing the characteristics of early-onset T2D in Chinese patients showed that most of the patients suffer pressure from life or work.6 Psychosocial stress seems to be a possible factor, which promotes the production of albuminuria through various mechanisms. Psychological stress is related to the activation of proinflammatory transcription factors that are related to late diabetes complications.14 Psychosocial stress can also activate the renin-angiotensin system, thereby increasing endogenous production of angiotensin II, known to be involved in the pathogenesis of albuminuria.15,16 More research is needed to confirm the relationship between albuminuria and psychosocial stress in early-onset diabetes.
Hyperglycemia and hypertension are the main risk factors for the development of microvascular diseases in diabetes.17,18 This study also demonstrated that HbA1c and SBP are independent risk factors for albuminuria. Consistent with prior research,17,19,20 obesity was identified as a risk factor for albuminuria. Moreover, earlier studies have linked smoking to albuminuria.17,21 However, this study did not find a significant association between smoking and albuminuria, possibly due to the absence of a smoking index. Previous studies have established LDL-C as a determinant of microvascular disease in T2D patients.22,23 Nevertheless, this study did not find an independent correlation between LDL-c and albuminuria, possibly due to statin use in some patients, which has been shown to have a protective effect on albuminuria.22,24,25
In addition, distinct risk factors for albuminuria were observed between male and female patients with diabetes. For male patients, age at diagnosis of diabetes (under 45 years old), blood pressure and BMI were identified as risk factors, whereas for female patients, disease duration and HbA1c were associated with increased risk. Furthermore, HDL-C emerged as a protective factor against albuminuria, consistent with findings from previous studies. Sacks et al reported that for every 0.2 mmol/L increase in HDL-C, the odds ratio for microvascular disease decreased by a factor of 0.92.26
However, several limitations should be acknowledged in this study. Firstly, the study design was cross-sectional, necessitating a prospective long-term follow-up study for result validation. Secondly, patient recruitment was limited to inpatients at a single center, potentially introducing selection bias. Thirdly, the data utilized in this study lacked information on family history of T2D, smoking and drinking habits, physical activity, and psychosocial stress, all of which may have influenced our outcomes. Additionally, due to the insidious onset of T2D, determining the precise age of onset can be challenging.
The present cross-sectional study demonstrates that patients diagnosed under the age of 45 have a significantly increased risk of albuminuria, particularly among male patients. Greater attention should be directed towards early-onset T2D to explore the mechanisms underlying the high incidence of complications in these patients and implement timely interventions. Additionally, the risk factors for albuminuria vary between males and females, as well as between early-diagnosed and late-diagnosed diabetes. Therefore, the focus of attention should differ for these populations.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgment
Qingqing Zhang, Liang Cheng and Boliang Li are co-first authors for this study. We thank all the participants in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Funding was from The Affiliated Taizhou People’s Hospital Affiliated of Nanjing Medical University (ZL202219, ZL202010), Taizhou People’s Hospital Scientific Research Start-Up Fund Project (QDJJ202113), and Nanjing Medical University Taizhou School of Clinical Medicine Research Project (TZKY20220203).
Disclosure
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
1. Li Y, Teng D, Shi X, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ. 2020;369:m997. doi:10.1136/bmj.m997
2. Wang L, Gao P, Zhang M, et al. Prevalence and Ethnic Pattern of Diabetes and Prediabetes in China in 2013. JAMA. 2017;317(24):2515–2523. doi:10.1001/jama.2017.7596
3. Mokdad AH, Ford ES, Bowman BA, et al. Diabetes trends in the U.S.: 1990-1998. Diabetes Care. 2000;23(9):1278–1283. doi:10.2337/diacare.23.9.1278
4. Mokdad AH, Bowman BA, Engelgau MM, et al. Diabetes trends among American Indians and Alaska natives: 1990-1998. Diabetes Care. 2001;24(8):1508–1509. doi:10.2337/diacare.24.8.1508-a
5. Pinhas-Hamiel O, Zeitler E. The global spread of type 2 diabetes mellitus in children and adolescents. J Pediatr. 2005;146(5):693–700. doi:10.1016/j.jpeds.2004.12.042
6. Yu H, Xie LF, Chen K, et al. Initiating Characteristics of Early-onset Type 2 Diabetes Mellitus in Chinese Patients. Chin Med J (Engl). 2016;129(7):778–784. doi:10.4103/0366-6999.178959
7. Hillier TA, Pedula KL. Characteristics of an adult population with newly diagnosed type 2 diabetes: the relation of obesity and age of onset. Diabetes Care. 2001;24(9):1522–1527. doi:10.2337/diacare.24.9.1522
8. Hillier TA, Pedula KL. Complications in young adults with early-onset type 2 diabetes: losing the relative protection of youth. Diabetes Care. 2003;26(11):2999–3005.
9. Al-Saeed AH, et al. An Inverse Relationship Between Age of Type 2 Diabetes Onset and Complication Risk and Mortality: the Impact of Youth-Onset Type 2 Diabetes. Diabetes Care. 2016;39(5):823–829. doi:10.2337/dc15-0991
10. Huang YC, Chen CC, Wang TY, et al. C-Reactive Protein Gene Variants and Their Serum Levels in Early Adult-onset Type 2 Diabetes Mellitus. Vivo. 2019;33(5):1685–1690. doi:10.21873/invivo.11656
11. Wakasugi S, Mita T, Katakami N, et al. Associations between continuous glucose monitoring-derived metrics and diabetic retinopathy and albuminuria in patients with type 2 diabetes. BMJ Open Diabetes Res Care. 2021;9(1):e001923. doi:10.1136/bmjdrc-2020-001923
12. Huang JX, Liao YF, Li YM. Clinical Features and Microvascular Complications Risk Factors of Early-onset Type 2 Diabetes Mellitus. Curr Med Sci. 2019;39(5):754–758. doi:10.1007/s11596-019-2102-7
13. Yen FS, Lo Y-R, Hwu C-M, et al. Early-onset type 2 diabetes <60 years and risk of vascular complications. Diabet Res Clin Pract. 2021;182:109129. doi:10.1016/j.diabres.2021.109129
14. Dalui A, Guha P, De A, et al. Assessment of stress & related albuminuria in caregivers of severe mentally ill persons. Indian J Med Res. 2014;139(1):174–177.
15. Krause EG, De Kloet AD, Scott KA, et al. Blood-borne angiotensin II acts in the brain to influence behavioral and endocrine responses to psychogenic stress. J Neurosci. 2011;31(42):15009–15015. doi:10.1523/JNEUROSCI.0892-11.2011
16. Aguilera G, Kiss A, Luo XU, et al. The renin angiotensin system and the stress response. Ann N Y Acad Sci. 1995;771:173–186. doi:10.1111/j.1749-6632.1995.tb44679.x
17. Alicic RZ, Rooney MT, Tuttle KR. Diabetic Kidney Disease: challenges, Progress, and Possibilities. Clin J Am Soc Nephrol. 2017;12(12):2032–2045. doi:10.2215/CJN.11491116
18. Cavender MA, Wirka RC. Blood pressure lowering in the prevention of type 2 diabetes. Lancet. 2021;398(10313):1778–1779. doi:10.1016/S0140-6736(21)02340-0
19. Kramer H, Reboussin D, Bertoni AG, et al. Obesity and albuminuria among adults with type 2 diabetes: the Look AHEAD (Action for Health in Diabetes) Study. Diabetes Care. 2009;32(5):851–853. doi:10.2337/dc08-2059
20. Look ARG. Effect of a long-term behavioural weight loss intervention on nephropathy in overweight or obese adults with type 2 diabetes: a secondary analysis of the Look AHEAD randomised clinical trial. Lancet Diabetes Endocrinol. 2014;2(10):801–809.
21. Ohkuma T, Nakamura U, Iwase M, et al. Effects of smoking and its cessation on creatinine- and cystatin C-based estimated glomerular filtration rates and albuminuria in male patients with type 2 diabetes mellitus: the Fukuoka Diabetes Registry. Hypertens Res. 2016;39(10):744–751. doi:10.1038/hr.2016.51
22. Marz W, Genser B, Drechsler C, et al. Atorvastatin and low-density lipoprotein cholesterol in type 2 diabetes mellitus patients on hemodialysis. Clin J Am Soc Nephrol. 2011;6(6):1316–1325. doi:10.2215/CJN.09121010
23. Navaneethan SD, Zoungas S, Caramori ML, et al. Diabetes Management in Chronic Kidney Disease: synopsis of the KDIGO 2022 Clinical Practice Guideline Update. Ann Intern Med. 2023;176(3):381–387. doi:10.7326/M22-2904
24. Lee TM, Lin M-S, Tsai C-H, et al. Add-on and withdrawal effect of pravastatin on proteinuria in hypertensive patients treated with AT receptor blockers. Kidney Int. 2005;68(2):779–787. doi:10.1111/j.1523-1755.2005.00457.x
25. Colhoun HM, Betteridge DJ, Durrington PN, et al. Effects of atorvastatin on kidney outcomes and cardiovascular disease in patients with diabetes: an analysis from the Collaborative Atorvastatin Diabetes Study (CARDS). Am J Kidney Dis. 2009;54(5):810–819. doi:10.1053/j.ajkd.2009.03.022
26. Sacks FM, Hermans MP, Fioretto P, et al. Association between plasma triglycerides and high-density lipoprotein cholesterol and microvascular kidney disease and retinopathy in type 2 diabetes mellitus: a global case-control study in 13 countries. Circulation. 2014;129(9):999–1008. doi:10.1161/CIRCULATIONAHA.113.002529
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
