Back to Journals » International Journal of General Medicine » Volume 15
Age- and Gender-Related Differences in the Hemodynamic Status of Patients with Mild or Moderate Hypertension
Authors Marjanovic M, Stojanov V, Marjanovic I, Vukcevic-Milosevic G, Radivojevic N, Matic D
Received 3 May 2022
Accepted for publication 28 June 2022
Published 5 July 2022 Volume 2022:15 Pages 6043—6053
DOI https://doi.org/10.2147/IJGM.S372092
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Marija Marjanovic,1 Vesna Stojanov,1,2 Ivan Marjanovic,2,3 Gordana Vukcevic-Milosevic,1 Nenad Radivojevic,1 Dragan Matic1,2
1Clinic for Cardiology, University Clinical Centre of Serbia, Belgrade, Serbia; 2Faculty of Medicine, University of Belgrade, Belgrade, Serbia; 3Ophthalmology Clinic, University Clinical Centre of Serbia, Belgrade, Serbia
Correspondence: Dragan Matic, Clinic for Cardiology, University Clinical Centre of Serbia, Dr Koste Todorovića 8, Belgrade, 11000, Serbia, Tel +381 63 208 975, Email [email protected]
Purpose: The aim of this study was to use non-invasive impedance cardiography (ICG) to determine the hemodynamic status of patients with grade 1 and grade 2 hypertension in relation to gender and age.
Patients and Methods: We analyse prospectively collected data of 158 patients with grade 1 or grade 2 arterial hypertension. Patients were grouped according to age: 1) < 50 years and 2) ≥ 50 years. Hemodynamic status of patients was assessed by using non-invasive ICG. For the purpose of this study two hemodynamic parameters were used: a) systemic vascular resistance index (SVRI) and b) left cardiac work index (LCWI). The primary endpoint was the hemodynamic status of patients. The secondary endpoint was hypertension-mediated organ damage.
Results: Increased SVRI was assessed in 80% of patients, more common in the ≥ 50 years group than in the < 50 years group (88.5% vs 64.8%; p < 0.01). The occurrence of increased systemic vascular resistance correlates hierarchically with increasing age. Elevated LCWI (hypervolemia and/or hyperinotropy) was present in 63% of patients, more often in males than females (70.3% vs 57.1%; p < 0.05) as well in those < 50 years than in older patients (70.4% vs 59.6%; p < 0.05). Patients with diabetes were less likely to have hypervolemia/hyperinotropy than those without diabetes (46.7% vs 67.2%; p < 0.01). Hypervolemia/hyperinotropy (46.7%) and hypovolemia/hypoinotropy (43.3%) were present in a similar percentage of diabetic patients. Left ventricular hypertrophy was found in 30 patients (19%). Patients with left ventricular hypertrophy were more commonly male (66.7% vs 42.2%; p = 0.016) and had increased systemic vascular resistance (96.7% vs 77.3%; p = 0.015) compared to the patients without left ventricular hypertrophy. Hypertensive retinopathy grade III was found in 14 patients (8.9%). Elevated daytime systolic pressure, diabetes and increased age are independent predictors of grade III hypertensive retinopathy. Patients with reduced renal function had higher mean systolic blood pressure (p < 0.05), were more commonly male (p < 0.01) and older (p < 0.01) than those without reduced renal function.
Conclusion: Although there are certain correlations between hemodynamic disorders and age and gender, specific hemodynamic status of an individual patient with hypertension cannot reliably be predicted on the basis of age and gender. The measurement of hemodynamic parameters by ICG can guide the clinician to select appropriate antihypertensive therapy to the patients’ hemodynamic pathophysiologic condition.
Keywords: hypertension, hemodynamics, impedance cardiography
Introduction
Numerous observational studies have shown an independent and continuous link between high blood pressure and a number of cardiovascular events, including haemorrhagic and ischemic stroke, myocardial infarction, sudden death, heart failure, peripheral arterial disease, renal failure, and the need for dialysis.1 Furthermore, there is ample evidence that lowering blood pressure can significantly reduce premature morbidity and mortality in patients with hypertension.2,3 Although blood pressure can be lowered by changing lifestyle and using effective antihypertensives, the degree of control achieved is not satisfactory, either in Europe or worldwide.4–6
Hypertension is a multifactorial disease, but the hemodynamic components of blood pressure physiology include factors that affect intravascular volume, cardiac inotropy and systemic vascular resistance. Physicians do not usually have the means to determine the hemodynamic causes of hypertension, so the choice of antihypertensive is often made independent of the patient’s hemodynamic status.7 This results in only a limited reduction in blood pressure.
Impedance cardiography (ICG) is a non-invasive, low-cost technology which easily measures a patient’s hemodynamic status in physician offices. ICG has been used in both primary care as well as hypertension speciality settings. Several studies have used ICG to evaluate hemodynamic parameters and demonstrated that ICG-guided therapy improves blood pressure control.
The aim of this study is to determine the hemodynamic status of patients with grade 1 and grade 2 hypertension in relation to gender and age using non-invasive ICG, which can be a guide when selecting appropriate antihypertensive therapy.
Materials and Methods
Study Population
We analysed data from 158 patients diagnosed with grade 1 (140–159/90–99 mm Hg) or grade 2 (160–179/100–109 mm Hg) essential arterial hypertension – according to current European Society of Cardiology/European Society of Hypertension guidelines.8 The study was conducted at the Multidisciplinary Centre for Polyclinic Diagnostics, Assessment and Treatment of Blood Pressure Disorders at the Clinic for Cardiology, University Clinical Centre of Serbia. Patient data were collected prospectively and entered into a dedicated electronic database.
This study included male and female patients aged over 18 with (1) increased blood pressure for at least 3 months, not treated with antihypertensive medications and (2) arterial hypertension improperly controlled with 1 or 2 antihypertensive medications (blood pressure values ≥140/90 mm Hg clinically and ≥130/80 mm Hg average of 24h on ambulatory blood pressure monitoring), but after discontinuation of therapy (after 2 weeks washout period) these patients met the criteria of the grade 1 and grade 2 hypertension. Those who exceeded blood pressure value of 179/109 mm Hg were excluded from the study. Patients were excluded if they had a history of heart failure, left ventricular ejection fraction <40%, atrial fibrillation, significant valvular heart disease, severe renal disease, nephrotic syndrome, cirrhosis, chronic obstructive pulmonary disease, polyneuropathy, or peripheral vascular disease.
Study Design, Definitions, and Endpoints
On the first visit, an initial clinical evaluation was conducted. Patients receiving antihypertensive therapy were advised to discontinue it, reduce salt intake, and to take captopril sublingually in case of increased blood pressure.
On the second visit (after 2 weeks) all patients underwent the following examinations:
- An interview and physical examination, including office blood pressure measurement in the seated position using the oscillometric technique,
- 24h-ambulatory blood pressure monitoring (ABPM)
- Impedance cardiography (ICG),
- Electrocardiogram (ECG),
- Laboratory tests (fasting glucose, creatinine, lipid profile),
- Echocardiographic examination, and
- Fundus examination.
The interview and physical examination were performed with special consideration given to a patient’s history of cardiovascular risk factors (hyperlipidaemia, obesity, smoking, and diabetes).
All patients underwent ABPM (Spacelabs Healthcare 90207, United States) with measurements taken every 30 minutes during the day (6 a.m. to 10 p.m.) and every 60 minutes during the night (10 p.m. to 6 a.m.). The results were interpreted according to current guidelines.8
ICG-aided measurement of hemodynamic parameters was performed using a BioMed NCCOM3 (United States) device while the patient was resting in a supine position in the morning (7.30 to 9.00 a.m.). The ICG method measures the resistance provided by chest tissue during the passage of alternating current. Changes in thoracic impedance during the cardiac cycle mainly depend on changes in the width and volume of the thoracic aorta. Numerous hemodynamic parameters can be determined using impedance cardiography with simultaneous electrocardiographic imaging and mean arterial pressure determined by oscillometry.
For the purposes of this study, two hemodynamic parameters were used:
- Systemic Vascular Resistance Index (SVRI), which provides insight into the state of the vasoactivity of peripheral arteries, ie, afterload. This parameter is used to determine whether the patient has vasodilation (SVRI value 305–1624 dyne x sec x m2/cm5), normal vasoactivity (SVRI value 1675–2588 dyne x sec x m2/cm5) or vasoconstriction (SVRI value 2639–3796 dyne x sec x m2/cm5);
- Left Cardiac Work Index (LCWI), which provides insight into the intravascular volume status and/or the cardiac inotropy status, which, together, point to the magnitude of the preload. This parameter is used to determine whether a patient has hypovolemia and/or hypoinotropy (LCWI 0.65–3.33 kg x m/m2), normovolemia and/or normoinotropy (LCWI value 3.44–5.16 kg x m/m2) or hypervolemia and/or hyperinotropy (LCWI value 5.27–7.96 kg x m/m2). The LCWI parameter is the product of mean arterial pressure (MAP) and cardiac index (CI), with CI depending on stroke volume and heart rate. Thus, in the absence of heart failure (which was a condition for inclusion in our study), an increase in LCWI values occurs due to hypervolemia and/or tachycardia.
Diabetes was assessed on the basis of anamnestic data on any prescribed antidiabetic therapy or blood glucose levels ≥7 mmol/L (fasting) or ≥11.1 mmol/L in any random blood sample.
Hyperlipidaemia was determined on the basis of cholesterol levels above 5.2 mmol/L and/or triglycerides above 1.7 mmol/L.
Body mass index (BMI) ≥30 was considered obese.
In order to determine hypertension-mediated organ damage, left ventricular hypertrophy, hypertensive fundus changes, and reduced renal function were assessed.
Left ventricular hypertrophy was determined with an echocardiographic examination (left ventricular wall thickness ≥1.1 cm).
Hypertensive retinopathy was graded according to Keith-Wagner-Barker classification from grade I to grade IV.9
Renal function was assessed based on estimated glomerular function rate (eGFR). The value of eGFR <60 mL/min/1.73 m2 was considered reduced renal function.
The primary endpoint was the hemodynamic status of patients. The secondary endpoint was hypertension-mediated organ damage.
The study protocol was approved by the Ethics Committee of Faculty of medicine, University of Belgrade, and was conducted according to the principles of the Declaration of Helsinki. Informed consent was obtained from all patients.
Statistical Methods
All patients involved in the study were grouped according to age: 1) <50 years and 2) ≥50 years. Demographic characteristics, risk factors, different types of hypertension, daytime blood pressure rhythm, hemodynamic status, and hypertension-mediated organ damage were analysed in relation to the gender and age of the patients.
Continuous variables with a normal distribution are expressed as mean ± SD, while those with skewed distribution are expressed as median (interquartile range). The Kolmogorov–Smirnov test was used to examine the normality of data distribution. Categorical variables are expressed as number of patients as well as percentages. Differences in continuous variables between groups were examined by the Student’s t-test for normally distributed data, and by the Mann–Whitney U-test for data with skewed distribution. Differences in categorical variables between groups were compared using the chi2 test. Predictors of hypertension-mediated organ damage were identified by univariate and multivariate binary logistic regression analysis. Demographic characteristics (age, gender), all the risk factors (diabetes mellitus, hyperlipidaemia, obesity, current smoking), 24-h systolic pressure, 24-h diastolic pressure, daytime systolic pressure, daytime diastolic pressure, night-time systolic pressure, night-time diastolic pressure, increased vascular resistance and increased cardiac work index were included into model. P < 0.05 was considered statistically significant. Statistical analysis of the results was performed using the Statistical Package for the Social Sciences - SPSS V.19.1 for Windows.
Results
Baseline Characteristics
The study included a total of 158 patients with grade 1 or grade 2 hypertension (74 men), with an average age of 54.6±14.9 years (range: 20 to 84 years). The women were older than the men; there were no differences in the distribution of risk factors in relation to gender. In the older group of patients (≥50 years), hyperlipidaemia was more common, as was diabetes, than in patients <50 years (Table 1).
 |
Table 1 Baseline Characteristics of Patients According to Age and Gender |
In relation to gender, there were no differences in the prevalence of certain types of hypertension (systolic/diastolic, isolated systolic, and isolated diastolic) (p = 0.166). However, in relation to age, the difference was statistically very significant (p < 0.001).
When viewed according to decade of life, systolic/diastolic hypertension is the most prevalent up to the sixth decade. In the seventh decade, the prevalence of isolated systolic hypertension increases, which becomes dominant in the eighth decade of life (Figure 1).
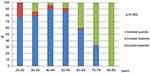 |
Figure 1 Prevalence of different types of hypertension according to decade of life. |
Hemodynamic Status of Patients with Hypertension
The vasoactive status of patients with hypertension is shown in Figure 2. Most common was increased peripheral vascular resistance, with cases of reduced vascular resistance accounting for a significantly lower percentage, and normal vasoactivity the least common.
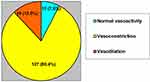 |
Figure 2 Vasoactive status in patients with arterial hypertension. |
There was no significant difference in vasoactive status in relation to gender, but there was a significant difference in relation to age. In the ≥50 years group, increased peripheral vascular resistance was significantly more common than in the <50 years group (88.5% vs 64.8%; p = 0.002). The prevalence of increased vascular resistance correlated hierarchically with increasing age (Figure 3).
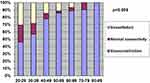 |
Figure 3 Vasoactive status according to decade of life. |
An assessment of the intravascular volume status/cardiac inotropy status, ie, preload, was performed by determining the Left Cardiac Work Index (LCWI), which contains data on inotropy in addition to information on intravascular volume. The majority of patients with hypertension had hypervolemia/hyperinotropy, a significantly smaller number had hypovolemia/hypoinotropy, and the smallest number had normovolemia/normoinotropy (Figure 4).
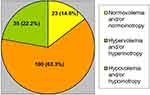 |
Figure 4 Preload state in patients with arterial hypertension. |
Hypervolemia/hyperinotropy was more common in males than in females (70.3% vs 57.1%; p = 0.04), as well as in those younger than 50 than in older patients (70.4% vs 59.6%; p = 0.024).
Patients with diabetes were less likely to have hypervolemia/hyperinotropy than those without diabetes (46.7% vs 67.2%; p = 0.009). Hypervolemia/hyperinotropy (46.7%) and hypovolemia/hypoinotropy (43.3%) were present in a similar percentage of diabetic patients.
Hypertension-Mediated Organ Damage
Left ventricular hypertrophy was found in 30 patients (19%). All patients with left ventricular hypertrophy had higher mean blood pressure values ( ) (24-h systolic pressure, systolic daytime and systolic night-time, diastolic daytime and diastolic night-time) than patients without left ventricular hypertrophy, and the difference was statistically significant (p < 0.05).
) (24-h systolic pressure, systolic daytime and systolic night-time, diastolic daytime and diastolic night-time) than patients without left ventricular hypertrophy, and the difference was statistically significant (p < 0.05).
Patients with left ventricular hypertrophy were more commonly male (66.7% vs 42.2%; p = 0.016) and had vasoconstriction (96.7% vs 77.3%; p = 0.015) compared to patients without left ventricular hypertrophy. There was no difference in the prevalence of hypervolemia/hyperinotropy in patients with or without left ventricular hypertrophy.
Univariate logistic regression analysis showed that the predictors of left ventricular hypertrophy were male gender, systolic daytime, systolic night-time, and 24-hour systolic pressure, as well as diastolic night-time pressure and vasoconstriction (Table 2). Multivariate regression analysis was unable to identify any independent predictors of left ventricular hypertrophy.
 |
Table 2 Predictors of Left Ventricular Hypertrophy in Patients with Hypertension |
Severe hypertensive retinopathy (grade III) was found in 14 patients (8.9%). No patients had grade IV hypertensive retinopathy. In addition, hypertensive retinopathy grade I was found in 55 patients (34.8%) and hypertensive retinopathy grade II in 65 patients (41.1%). Only 24 patients (15.2%) showed no signs of hypertensive retinopathy. The analysis only included changes classed as hypertensive retinopathy grade III, since grade I and grade II are not specific to hypertension but can also occur as part of the degenerative process in blood vessels during aging.
Patients with grade III hypertensive retinopathy were significantly more often older than 50 (92.9% vs 63.2%; p = 0.025) and more likely to have diabetes (50.0% vs 16.0%; p = 0.002) and isolated systolic hypertension (50.0% vs 23.6%; p = 0.032). Increased vascular resistance was more common in these patients, but this difference was not statistically significant. Multivariate regression analysis showed that independent predictors of hypertensive retinopathy grade III are an increase in age, diabetes mellitus, and elevated systolic daytime blood pressure (Table 3).
 |
Table 3 Predictors of Grade III Hypertensive Retinopathy in Patients with Arterial Hypertension |
Reduced renal function assessed as eGFR <60mL/min/1.73m2 was found in 20 patients (12.7%). Patients with reduced renal function had higher mean systolic blood pressure values (24h systolic, daytime systolic, night-time systolic; p < 0.05), were more commonly male (51.4% vs 15.0%; p < 0.01) and more often older than 50 years (100.0% vs 60.9%; p = 0.001), then patients without reduced renal function. Multivarible regression analysis showed that independent predictors of reduced renal function were male gender and age per 1-year increase.
Discussion
The main findings of our study are: 1) In more than ¾ patients (80%) with grade 1 and grade 2 hypertension, the root cause of hypertension is increased systemic vascular resistance, the occurrence of which correlates hierarchically with increasing age; 2) Elevated left cardiac work index (hypervolemia and/or hyperinotropy) is present in more than half the patients (63%), more often in males and patients younger than 50; 3) 24-h systolic and diastolic night-time hypertension with increased peripheral vascular resistance and being male are predictors of left ventricular hypertrophy; 4) elevated systolic daytime pressure, diabetes mellitus and increasing age are independent predictors of grade III hypertensive retinopathy; 5) systolic hypertension (24h, daytime and night-time), male gender, and increasing age are predictors of reduced renal function.
In our study, mixed systolic/diastolic hypertension was the most common type of essential hypertension in patients up to 70 years of age, with the highest incidence in the fifth decade. Epidemiological studies have shown that this type of hypertension is the most common form of hypertension in middle-aged people and that it is associated with significantly elevated peripheral vascular resistance. Most of these patients first have so-called “early” hypertension due to increased cardiac output. Over time, cardiac output normalises, but due to continuous exposure to high blood pressure, constantly increased peripheral resistance develops.10
In this study, isolated systolic hypertension, which was closely linked to diabetes, was the dominant type in those over 70. According to Staessen et al, the prevalence of this type of hypertension increases exponentially with age, is more pronounced in females and smokers, and at an earlier age is more common in patients with diabetes than those without.11 The main cause of isolated systolic hypertension is increased aortic stiffness, while an increase in peripheral vascular resistance is less significant. In young people, isolated systolic hypertension occurs due to increased cardiac output or increased aortic stiffness. Although previously considered a benign condition, isolated systolic hypertension is today viewed as a major risk factor for strokes and coronary heart disease.
Isolated diastolic hypertension was the rarest type of hypertension in this study. A quarter of young patients in the third decade of life had this form of hypertension with the frequency decreasing with age. Isolated diastolic hypertension is thought to occur in individuals with previously normal or high normal blood pressure.10 By following these patients, it was determined that isolated diastolic hypertension later develops into systolic/diastolic hypertension. As with systolic/diastolic hypertension, the main hemodynamic abnormality linked to isolated diastolic hypertension is also increased peripheral vascular resistance.
In creating the various hemodynamic phenotypes of elevated blood pressure (increased vascular resistance, increased cardiac output and increased fluid volume), a central role has been shown to play the renin-angiotensin system, the sympathetic nervous system and the adrenal-mineral corticoid axis. Measurement of the hemodynamic profile with ICG provides insight into the degrees of activations of these neurohormonal systems.
In our study, increased systemic vascular resistance was more common in males than females, but without statistical significance. Increased vascular resistance was significantly affected by age. We found that the prevalence of increased vascular resistance is strongly linked to increasing age, reaching 90% in the seventh decade of life. Hyperlipidaemia contributes to the development of increased vascular resistance.
The results of our study are in line with the findings of other authors who established that aging is linked to a decrease in cardiac output and an increase in peripheral vascular resistance. In a study of 640 healthy individuals evaluated as renal donors, Taler et al found that advancing age was linked to an increase in blood pressure, a rise in systemic vascular resistance, and a decrease in cardiac output.12 The hemodynamic changes that accompanied aging were similar in men and women, although blood pressure and cardiac output were lower and heart rate and systemic vascular resistance were higher in women.
In our study, increased preload (hypervolemia and/or hyperinotropy) expressed through the left cardiac work index (LCWI) was significantly more common in males than females, while patients younger than 50 were more likely to have an increased preload than older patients. This could be connected to excessive dietary salt intake. The presence of tachycardia in these patients may indicate the presence of increased sympathetic activity.
Although in our study increased vascular resistance is present in 80% of patients with its prevalence increasing with advancing age, a significant percentage of middle-aged people do not have increased vascular resistance. As for younger hypertensive patients, more than 20% exhibited normal vascular resistance with 30% even having reduced peripheral vascular resistance. Although most patients in our study had an increased preload, 30% of female patients, nearly 30% of those under the age of 50, and more than 40% of those with diabetes had a decreased preload. The results of our study showed that the root cause of hypertension is specific to each patient; the hemodynamic disorder in question cannot be generalised.
According to the treatment algorithms for ICG-guided antihypertensive therapy, an elevated systemic vascular resistance would recommend the selection or up titration of an angiotensin-converting enzyme inhibitor (ACEI), angiotensin II receptor blocker (ARB) or dihydropyridine calcium-channel blocker (CCB) – depending on each patient’s clinical conditions. The presence of hypervolemia would recommend the selection of up titration or addition of a diuretic. An elevated cardiac inotropy status would recommend the selection or up titration of a beta blocker or nondihydropiridine calcium-channel blocker (CCB).13
Several studies have shown that control of arterial blood pressure is better and more quickly achieved when therapy is prescribed based on hemodynamic disorder data obtained through ICG rather than standard methods of adjusting therapy in patients with hypertension.
In the study by Taler et al, satisfactory control of blood pressure (values below 140/90 mmHg) was 70% more frequent in the group of patients treated in accordance with ICG findings compared to patients treated in the standard way.14 In the former, a greater reduction in systemic vascular resistance was achieved and more intensive diuretic therapy was used based on the hypervolemia values determined.
A similar study conducted by Smith et al has shown that patients assigned treatment according to hemodynamic parameters had a statistically significantly higher success rate and achieved lower systolic and diastolic blood pressure levels due to lower systemic vascular resistance than those in empirical care group, while cardiac output did not change or differ between the hemodynamic and empirical groups.15
A study by Krzesiński et al has shown that office systolic and diastolic blood pressure and night-time ambulatory diastolic blood pressure were lower in the hemodynamic group of patients with a higher use of beta-blockers and calcium antagonists compared to empirical group.16
ESC/ESH 2018 Clinical Practice Guidelines for the Management of Arterial Hypertension recommend a single pill treatment strategy with two-drug fixed combinations with the preferred use an ACE inhibitor or ARB, combined with a CCB and/or a thiazide – like diuretics.8 However, because of different doses of antihypertensive medications in fixed combinations, it would be useful to get insight of underlying status of patients by ICG method, which can guide the clinician to select a single-pill combination which is expected to have the best therapeutic effect in blood pressure control.
In our study, left ventricular hypertrophy was found in 19% of patients. Patients with left ventricular hypertrophy had higher levels of systolic pressure (daytime, night-time, and 24-hour) that were statistically highly significant (p < 0.001) and significantly higher diastolic daytime and night-time pressure readings (p < 0.05) than patients without left ventricular hypertrophy. In addition, patients with left ventricular hypertrophy were significantly more often male and had a higher systemic vascular resistance index value than patients without hypertrophy (p < 0.05).
The findings of our study are in line with the findings of the Framingham Study, which showed that the prevalence of echocardiographically determined left ventricular hypertrophy is 15–20% in patients with mild hypertension and increases in patients with severe hypertension.17 Mehta et al showed that there is a much better correlation between left ventricular mass and average daily 24-hour blood pressure levels compared to office blood pressure.18
Left ventricular hypertrophy is a strong predictor of cardiovascular mortality. Vakili et al showed that the risk of adverse cardiovascular events was 2.3 times higher in patients with left ventricular hypertrophy, independent of other risk factors.19 Studies have shown that the use of antihypertensive drugs can lead to regression of left ventricular hypertrophy and improve the prognosis for patients.
In the present study, the majority of patients were found to only have a mild degree of hypertensive fundus changes and only a small number had advanced, grade 3 hypertensive retinopathy. Severe hypertensive retinopathy was strongly associated with high blood pressure during the day, increasing age, and diabetes. The risk of developing severe hypertensive retinopathy in patients who had diabetes in addition to hypertension was more than three times higher than in patients without diabetes.
According to Wong and Schmieder, there is solid evidence that signs of advanced hypertensive retinopathy are strongly associated with subclinical cerebrovascular disease and may predict the occurrence of clinical events such as stroke, coronary heart disease, congestive heart failure and death of cardiovascular origin, regardless of blood pressure levels and other traditional risk factors.20,21 Therefore, a fundus examination continues to play an important role in a therapeutic approach and risk assessment of patients with hypertension.8
Hypertension is the second most important cause of chronic kidney disease after diabetes. The diagnosis of hypertension – induced renal damage is based on the finding of reduced renal function and/or the detection of albuminuria. Progressive reduction in eGFR indicates progressive loss of renal function and is independent and additive predictor of increased cardiovascular risk and progression of renal disease.8 In our study, reduced renal function (based on eGFR) was found in 12.7% of patients and was associated with increased systolic pressure, but independent predictors were male gender and increasing age.
Limitations
Our study has some limitations. Firstly, only two hemodynamic parameters obtained by impedance cardiography (SVRI and LCWI) were used in the study to assess the hemodynamic status of patients with hypertension. The application of more hemodynamic parameters would provide a more detailed insight into hemodynamic abnormalities in these patients. Secondly, the left ventricular hypertrophy was determined with left ventricular wall thickness instead of left ventricular mass. Thirdly, ambulatory blood pressure device was programmed to record blood pressure at 60 min. intervals during the night, instead of every 30 minutes. Further, our study involved a small number of patients with hypertension, in particular a small number with hypertension-mediated organ damage, so the strength of the study is not very large. Our results refer to a specific population of hypertensive patients without other cardiovascular diseases. Thus, the application of these observations on general populations needs to be carefully considered.
Conclusion
Although these study using ICG technology show certain correlations between hemodynamic disorders and age and gender, hemodynamic measures show significant variations within each given group of patients with grade 1 and grade 2 hypertension. Because of heterogeneity of hemodynamic findings, the specific hemodynamic status of an individual patient cannot reliably be predicted on the basis of age and gender. Hemodynamic information obtained by ICG can guide the clinician to select appropriate antihypertensive therapy to the patients’ hemodynamic pathophysiologic condition.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913.
2. Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–967. doi:10.1016/S0140-6736(15)01225-8
3. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32:2285–2295. doi:10.1097/HJH.0000000000000378
4. Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310:959–968. doi:10.1001/jama.2013.184182
5. Falaschetti E, Mindell J, Knott C, et al. Hypertension management in England: a serial cross-sectional study from 1994 to 2011. Lancet. 2014;383:1912–1919. doi:10.1016/S0140-6736(14)60688-7
6. Tocci G, Rosei EA, Ambrosioni E, et al. Blood pressure control in Italy: analysis of clinical data from 2005–2011 surveys on hypertension. J Hypertens. 2012;30:1065–1074. doi:10.1097/HJH.0b013e3283535993
7. Viigimaa M, Talvik A, Wojciechowska W, et al. Identification of the hemodynamic modulators and hemodynamic status in uncontrolled hypertensive patients. Blood Press. 2013;22:362–370. doi:10.3109/08037051.2013.782900
8. Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–3104. doi:10.1093/eurheartj/ehy339
9. Keith NM, Wagener HP, Barker NW. Some different types of essential hypertension: their course and prognosis. Am J Med Sci. 1974;268:336–345. doi:10.1097/00000441-197412000-00004
10. Cheriyan J, McEniery CM, Wilkinson IB. Essential hypertension. In: Hypertension. New York: Oxford University Press Inc; 2010:49–110.
11. Staessen J, Amery A, Fagard R. Isolated systolic hypertension in the elderly. J Hypertens. 1990;8:393–405. doi:10.1097/00004872-199005000-00001
12. Taler S, Driscoll N, Tibor M, et al. Changes in hemodynamic patterns with age in normotensive subjects (Abstract). Am J Hypertens. 2004;17:373. doi:10.1016/j.amjhyper.2004.03.447
13. Ferrario CM, Flack JM, Strobeck JE, Smits G, Peters C. Individualizing hypertension treatment with impedance cardiography: a meta-analysis of published trials. Ther Adv Cardiovasc Dis. 2010;4:5–16. doi:10.1177/1753944709348236
14. Taler SJ, Textor SC, Augustine JE. Resistant hypertension: comparing hemodynamic management to specialist care. Hypertension. 2002;39:982–988. doi:10.1161/01.HYP.0000016176.16042.2F
15. Smith RD, Levy P, Ferrario CM. Value of non-invasive hemodynamics to achieve blood pressure control in hypertensive subjects. Hypertension. 2006;47:771–777. doi:10.1161/01.HYP.0000209642.11448.e0
16. Krzesiński P, Gielerak GG, Kowal JJ. A “patient-tailored” treatment of hypertension with use of impedance cardiography: a randomized, prospective and controlled trial. Med Sci Monit. 2013;19:242–250. doi:10.12659/MSM.883870
17. Devereux RB. Hypertensive cardiac hypertrophy: pathophysiologic and clinical characteristics. In: Laragh JH, Brenner BM, editors. Hypertension, Pathophysiology, Diagnosis and Management.
18. Mehta SK, Rame JE, Khera A, et al. Left ventricular hypertrophy, subclinical atherosclerosis, and inflammation. Hypertension. 2007;49:1385–1391. doi:10.1161/HYPERTENSIONAHA.107.087890
19. Vakili BA, Okin PM, Devereux RB. Prognostic implications of left ventricular hypertrophy. Am Heart J. 2001;141:334–341. doi:10.1067/mhj.2001.113218
20. Wong TY, Mitchell P. Hypertensive retinopathy. N Engl J Med. 2004;351:2310–2317. doi:10.1056/NEJMra032865
21. Schmieder RE. Hypertensive retinopathy: a window to vascular remodelling in arterial hypertension. Hypertension. 2008;51:43–44. doi:10.1161/HYPERTENSIONAHA.107.100230
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
