Back to Journals » Open Access Journal of Contraception » Volume 14
Adherence to Modern Contraceptives Among Female Refugee Adolescents in Northern Uganda: A Prospective Single Cohort Study
Authors Bakesiima R , Gemzell-Danielsson K , Beyeza-Kashesya J, Cleeve A, Larsson EC, Chalo Nabirye R
Received 15 July 2023
Accepted for publication 18 November 2023
Published 2 December 2023 Volume 2023:14 Pages 169—180
DOI https://doi.org/10.2147/OAJC.S430813
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Igal Wolman
Ritah Bakesiima,1,2 Kristina Gemzell-Danielsson,2,3 Jolly Beyeza-Kashesya,4 Amanda Cleeve,2,3,5 Elin C Larsson,2,3,6 Rose Chalo Nabirye7
1Department of Obstetrics and Gynaecology, School of Medicine, College of Health Sciences, Makerere University, Kampala, Uganda; 2Department of Women’s and Children’s Health, Division of Obstetrics and Gynaecology, Karolinska Institutet, Stockholm, Sweden; 3WHO Collaborating Centre, Division of Women’s Health, Karolinska University Hospital, Stockholm, Sweden; 4Department of Obstetrics and Gynaecology, Mulago Specialised Women and Neonatal Hospital, Kampala, Uganda; 5Department of Women´s Health, South General Hospital, Stockholm, Sweden; 6Department of Global Public Health, Karolinska Institutet, Stockholm, Sweden; 7Department of Nursing, Faculty of Health Sciences, Busitema University, Mbale, Uganda
Correspondence: Ritah Bakesiima, Department of Obstetrics and Gynaecology, School of Medicine, College of Health Sciences, Makerere University, Kampala, Uganda, Email [email protected]
Background: Contraceptive adherence is the current and consistent use of a contraceptive method as prescribed by a health worker or family planning provider so as to prevent pregnancy. Globally, adherence is lowest among adolescents. This has greatly contributed to the high burden of adolescent pregnancies. Adherence and reasons for discontinuation among refugee adolescents are poorly understood. The aim of this study was to determine the rates and predictors of adherence to modern contraceptives among female refugee adolescents in northern Uganda.
Methods: This was a prospective single cohort study, nested into a randomised controlled trial (RCT) assessing the effect of peer counselling on acceptance of modern contraceptives. The RCT was conducted among female refugee adolescents in Palabek refugee settlement, northern Uganda. The study involved 272 new starters of modern contraceptives who were followed up for six months from May 2019 to January 2020. The outcome was measured at one, three, and six months after receiving a contraceptive method, and the predictors of adherence were determined using Generalised Estimating Equations (GEE). Data were analysed using STATA version 14.0.
Results: Adherence rates were low and reduced over time. By the end of the six months, only 44% of the participants were using a contraceptive method. Participants using long-acting reversible contraceptives (LARC) were more likely to adhere compared to those who were using short-acting reversible contraceptives (SARC) (OR: 3.37, 95% CI: 1.914– 5.937, p< 0.001).
Conclusion: Adherence to modern contraceptives was low, leaving adolescents at risk of unintended pregnancies. Participants using LARC were more likely to adhere than those using SARC. Interventions addressing fear of side effects and partner prohibition should be studied and implemented to enable adherence to modern contraceptives.
Keywords: contraceptive adherence, contraceptive discontinuation, adolescents, refugees, teenage pregnancy
Introduction
Adolescent pregnancy remains a global burden with an estimated birth rate of 44 births per 1,000 girls aged 15 to 19 years.1 In low-resource settings, approximately 770,000 girls under 15 years of age and about 12 million aged 15 to 19 years give birth annually,2 and an additional 3 million girls aged 15 to 19 years undergo unsafe abortions annually.3 Sub-Saharan Africa has the highest rates of adolescent pregnancy and child birth globally at 99.4 births per 1000 women.4 In Uganda, adolescent births account for 14% of all births,5 the majority of which are unintended.6 However, the rates are mentioned to be higher among the refugee adolescents than among the nationals.7–9 This is so because of the insecurity and poverty faced by refugee adolescents, which leave them vulnerable to sexual exploitation, abuse, rape, transactional sex, and early or forced marriages.
Adolescent pregnant women have a higher risk of pregnancy-induced hypertension, systemic infections, puerperal endometritis, and post-partum depression compared to those aged 20 to 24 years.10 Owing to the above-mentioned complications, pregnancy and child birth are the largest contributors to mortality among adolescents world-wide.2,11
The high adolescent pregnancy rates are attributed to low contraceptive use, coupled with poor adherence to contraception.12 Use of modern contraceptives among female refugee adolescents in low-resource settings is reported to be less than 10%.2,7–13 With an aim of increasing use of modern contraceptives among female refugee adolescents, a randomised controlled trial (RCT) was conducted by Bakesiima et al in this same population to assess the effect of peer counselling on uptake of contraceptives.14 However, contraceptive uptake remained low. This low use of contraceptives is reported to be a result of fear of side effects, inadequate knowledge on contraceptives, partner prohibition, and social acceptability.2,7–15 The same reasons are believed to explain poor adherence to and discontinuation from contraceptives. Research among adolescents in Ghana showed a contraceptive adherence rate of 23%,16 while high discontinuation rates of approximately 50% were reported among adolescents in Kenya, Malawi, Morocco, and Tanzania.17,18
Several factors are reported to be associated with adherence to modern contraceptives among adolescents. These include age, education, and type of contraceptive used.19–22
In order to improve on the low adherence rates and the high discontinuation rates, it is important to understand the contributing factors. However, neither the rates nor the predictors of low adherence and high discontinuation have been established among refugee adolescents. Therefore, this study aimed to determine the rates and predictors of adherence to reversible modern contraceptives among female refugee adolescents in northern Uganda.
Methods
Study Design
This was a prospective single-cohort study, nested in a randomised controlled trial (RCT) which was aimed at assessing the effect of peer counselling, compared to routine contraceptive counselling on acceptance of modern contraceptives among female refugee adolescents.14 The current study aimed at assessing adherence to modern contraceptives among female refugee adolescents who were new starters of modern contraceptives from the RCT. The RCT was carried out among 588 female refugee adolescents aged 15 to 19 years, who were not using any contraceptives at the time of the RCT. The participants were randomised to either peer contraceptive counselling (the intervention), or routine contraceptive counselling provided at the health facilities (the control). After receiving their allocated counselling, they were assessed for contraceptive acceptance. All those who accepted to use contraceptives received their preferred method, and these are what we regarded as “new starters”. All new starters who consented to participate and were eligible were included in the current study.
This study was carried out in Palabek refugee settlement in northern Uganda, from May 2019 to January 2020. Participant recruitment occurred from May to July 2019, and participants were then followed for a period of six months till January 2020. The reason for this short follow-up period was because of the mobility of the refugees; they are always moving in and out of the settlement at will, either to go back to their native country or to look for employment opportunities outside the camp. Therefore, a longer follow-up period would result in increased loss to follow-up. The follow-ups were done at one, three, and six months after receiving a contraceptive method.
Study Setting
Palabek refugee settlement was established in April 2017 and is one of the newest refugee settlement in Uganda. It is situated at the border of Uganda and South Sudan. It hosts close to 55,000 refugees from South Sudan, 85% of whom are women and children.23 Palabek refugee settlement is burdened with adolescent pregnancy among girls aged 17 to 19 years with a prevalence of over 50%,7 and the settlement has four health centres which provide contraceptive services free of charge. The family planning services provided include contraceptive counselling, provision of condoms (both male and female), oral contraceptives, injectables, and insertion and removal of implants and intra-uterine devices (IUDs).
Study Participants
A total of 272 female refugee adolescents aged 15 to 19 years who were new starters of reversible modern contraceptives participating in the RCT were consecutively enrolled into this study. The reversible modern contraceptives available were oral contraceptives (both combined and progestin only), the depo-medroxyprogesterone acetate (DMPA) injectable, subcutaneous single-rod contraceptive implants, and copper IUD. Participants were excluded if they did not understand either English, Acholi, or Arabic (the languages commonly used within the settlement), or were physically or mentally unable to consent or answer interview questions.
Sample Size Estimation
The sample size formula for comparing means in two proportions by Hulley24 was used. An alpha of 0.05 was assumed, with a power of 80%. The proportion of adolescents who discontinued long-acting reversible contraceptives (LARCs) was taken at 35%,25 while the proportion of adolescents who discontinued other contraceptives was taken at 60% assuming a 25% difference between the two groups. The proportion of refugee adolescents on LARCs was estimated to be 12.6%.13 After factoring these into the formula, we got a sample size of 272 participants. Assuming a 10% loss to follow-up ((0.1 × 272)+272), the adjusted sample size would be 300 participants. Therefore, a total of 300 female refugee adolescents would be necessary to meet this objective.
However, we were only able to recruit 272 participants from the RCT because they were the only new starters of contraceptives who were willing to participate in this study. This sample size is smaller than the calculated and could have an effect on our estimates. This has been acknowledged as a study limitation.
Data Collection
As part of the RCT,14 baseline information like social demographics, sexual and reproductive history, type of contraceptive received, and partner’s characteristics was collected at the health centre where the participants received their contraceptives. This information was obtained with the help of an interviewer-administered questionnaire. A contact locator was developed which had the participants’ address, telephone numbers, and details of their “significant other” who could be a relative, spouse, or friend. Participants were also given a small card with their particulars and an appointment date for their next follow-up. Those who did not come to the health centre at the given appointment were traced with the help of the contact locator. In the event of a missed appointment, they were contacted by phone or home-visited within two weeks of the missed appointment. A respondent was considered lost to follow-up if she was not traced within the six months of the study. Information collected during follow-up included continued use of the contraceptive method (adherence) or discontinuation, the reason for discontinuation, switching to other contraceptive methods, reasons for switching, and side effects experienced. Two trained research assistants conducted the interviews.
Study Variables
The outcome variable was “adherence to modern contraceptives” defined as the use of any contraceptive method in an ongoing and consistent manner as prescribed.26 For adherence to be achieved, both continuation and correct use of the contraceptives are required. Hence, a participant was termed as non-adherent if: (i) the participant became pregnant during the previous month (and the pregnancy not attributed to method failure as judged by research assistants); (ii) missed her appointment; and (iii) missed taking three or more oral contraceptives during the month according to the Guttman scale.27 Self-reported non-adherence was used for all the other contraceptive methods. For the LARC methods, participants were regarded as adherent for the six-month follow-up unless they reported removal of the method. Participants who self-reported pregnancy had to undergo an assessment to determine whether the pregnancy was due to method failure or non-adherence.
The predictor variables included socio-demographics like age, highest level of education attained, marital status, occupation, sexual and reproductive history, like age at first sex, number of children alive, partner’s characteristics, and type of contraceptive given.
Statistical Methods
Data were analysed using STATA version 14.0. Continuous variables were summarised as means and standard deviations if they were normally distributed, and as medians and ranges if skewed. Categorical variables were summarised as percentages and proportions. Adherence to contraceptives was analysed as a binary variable, with adherence coded as “1” and non-adherence as “0” at the different time points. Per cent adherence at the different follow-up times was then obtained. Predictors of adherence were assessed using Generalised Estimating Equations (GEE), with the exchangeable correlation matrix, family binomial, and link logit. Bivariate analysis was done by fitting a model for each independent variable with the outcome. All the variables that gave a p-value ≤0.2 at the bivariate analysis were considered for multivariate analysis. Also considered for multivariate were variables which are known to be of significance to adherence from previous research even though they had p-values greater than 0.2.
At the multivariate analysis, GEE was run for all the variables which met criteria for it, and the non-significant ones (p>0.05) were dropped one at a time. Those which retained statistical significance were used to assess for interaction and confounding. Two-way product terms were formed between the variables and used in the assessment of interaction using the chunk test. A variable was considered a confounder if it caused a greater than or equal to 10% change in the odds ratio of adherence to contraceptive use. Odds ratios along with their 95% confidence intervals were reported, and statistical significance reported at p<0.05. Robust standard errors were used in the GEE analysis. To deal with those who were lost to follow-up, both intention to treat (ITT) and per protocol analyses were conducted.
Sensitivity Analysis
This was conducted to assess if the participants who were lost to follow-up had an impact on our study findings. We first grouped the lost to follow-up under non-adherent, and then re-analysed them under adherent, and conclusions were checked if they remained similar.
Ethical Considerations
Ethical clearance was obtained from the School of Medicine Higher Degrees Research Ethics Committee (REC REF 2018–059), and from Uganda National Council of Science and Technology (SS 4876). This study complies with the Declaration of Helsinki as indicated in the following statements. We ensured that all participants gave their written informed consent before enrolling them into the study, and guaranteed their confidentiality with the use of number codes instead of participant names. For participants below 18 years, we did not seek for parental consent because it is stated in the National Policy Guidelines and Service Standards for Sexual and Reproductive Health and Rights that all individuals seeking family planning services are eligible to receive the services regardless of their age, without need for verbal or written consent from parent, guardian, or spouse, as long as they have received prior education or counselling about the contraceptives.28 All interviews were held in private places where discussions could not be overheard.
Results
Participant Flow
A total of 279 participants were assessed for eligibility as new starters of modern contraceptives from the RCT. Amongst these, 7 were eliminated because they either did not meet the inclusion criteria (due to language barrier) or they declined to participate in the study. Therefore, 272 participants were enrolled in the study, of whom 113 were lost to follow-up (Figure 1).
 |
Figure 1 Participant flow chart. |
Baseline Characteristics of Study Participants
Most of the participants were older adolescents aged 18 to 19 years (86.6%), had attained up to primary school as their highest level of education (73.5%), and were cohabiting (46%). Two-thirds of the participants (67.3%) had ever been pregnant, and 45.9% had more than one child. Regarding the partner’s characteristics, most of the participants had partners within their age group (18 to 25 years). Most of the partners had attained up to secondary as their highest level of education (62.9%), and were unemployed (41.9%). At baseline, most of the participants were using the injectable contraceptive (45.6%). See Table 1.
 |
Table 1 Baseline Characteristics of the Study Participants (n=272) |
Adherence to Reversible Modern Contraceptives Among the Study Participants at the Different Follow-Up Points
A total of 253 participants (93%) were found to have adhered to their contraceptives at one month, 178 (65.7%) at three months, and 115 (44.7%) at six months. Altogether, 17 (6.3%) of the participants switched contraceptives due to side effects and ease of use, while 24 (8.8%) discontinued use during the six months of follow-up. The reasons for discontinuation were side effects (57.1%), partner prohibition (23.8%), and wish to have a child (19.1%). A total of 113 (44.0%) of the participants were lost to follow-up. Thirteen of the participants were found pregnant at the end of the six months of follow-up (Table 2). Participants who switched contraceptives were treated as adherent in the bivariate and multivariate analyses.
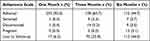 |
Table 2 Adherence to Contraceptives at Each of the Three Follow-Up Time Points |
Factors Associated with Adherence to Modern Contraceptives
At bivariate analysis, the factors found to be significant (p<0.2) were occupation, marital status, partner’s education, partner’s occupation, type of contraceptive used, and time, as shown in Table 3. These variables were included in the multivariate analysis. In addition, age, education, ever been pregnant, and number of children alive were also included in the multivariate analysis since they are known to be important for adherence from previous research. There was no difference in adherence between participants who received peer counselling and those who received routine counselling.
 |
Table 3 Factors Associated with Adherence to Contraceptives (ITT) |
In the multivariate analysis, the variables which were found to be significant (p<0.05) were type of contraceptive used and time, as shown in Table 3. These variables were assessed for interaction between each other and for confounding with other independent variables. However, there was neither interaction nor confounding. The results presented in Table 3 are for intention-to-treat (ITT) analysis.
Additional Analyses
Per Protocol Analysis
In this analysis, participants who were lost to follow-up are dropped and excluded from the analysis. Results show that the variables type of contraceptive (aOR: 4.97, 95% CI: 1.827–13.537, p=0.002 for use of LARC vs SARC) and time of follow-up (aOR: 0.02, 95% CI: 0.003–0.149, p<0.001 at 6 months) were significantly associated with adherence to modern contraceptives. These conclusions are similar to those obtained from the intention-to-treat analysis.
Sensitivity Analysis
In this analysis, participants who were lost to follow-up were treated as adherent. We assumed that they continued using their contraceptives even though they were lost to follow-up. Results from this analysis are similar to those obtained from the ITT and PP analyses. The only variables that were significantly associated with adherence to modern contraceptives were type of contraceptive (aOR: 3.81, 95% CI: 1.437–10.124, p=0.007 for use of LARC vs SARC) and the time of follow-up (aOR: 0.04, 95% CI: 0.006–0.315, p=0.002 for 6 months of follow-up).
Additional analysis was also conducted to confirm if the participants who were lost to follow-up are dissimilar from those who stayed in the study. Using the chi-square test, we found that the participants who completed the six months follow-up are not any different from those who were lost to follow-up as shown in Table 4.
 |
Table 4 Baseline Characteristics of Participants Who Were Lost to Follow-Up Compared to Those Who Completed the Study |
Discussion
In this study that was carried out to determine the rates and predictors of adherence to modern contraceptives among female refugee adolescents in northern Uganda, participants were followed up for a period of six months. We found that adherence rates reduced with time, and that less than half of the participants adhered to the initially chosen method by the end of the study. The factors found to be associated with adherence were type of contraceptive and duration of use. Participants who were using LARCs were three times more likely to adhere to their contraceptives than those who used SARCs. The low adherence rate is in line with findings from a study among non-refugee adolescents in Ghana16 and among non-refugee adolescents and young women aged 15 to 24 in a study carried out in northern California.29 This low adherence to modern contraceptives among refugee adolescents was mainly attributed to side effects and partner prohibition. Side effects have been reported as a cause of poor adherence in other studies among non-refugee adolescents.22–30 Our findings are consistent with results from studies carried out among non-refugee adolescents which also found that participants who were using LARCs were more likely to adhere.22–29 This can be attributed to the fact that LARCs provide a long-term effective contraception without relying on user behaviour/action, making it easier to adhere or comply with them.31 Furthermore, they have been preferred for their convenience of use, low failure rates, cost effectiveness,32 and high user satisfaction,33 all of which contribute to the higher adherence rates among users.
Duration of use was also significantly associated with adherence to contraceptives amongst refugee adolescents. Participants were 88% less likely to adhere to the received contraceptive at three months follow-up, and over 90% less likely to adhere at six months compared with use at one month. This could be explained by the fact that participants who had adhered up to three months and continued use to six months were mostly the LARC users.
Some of the strengths of this study are: it is one of the first studies conducted to determine contraceptive adherence among refugee adolescents. It contributes to providing important information that could guide contraceptive use among refugee adolescents. The study also used a prospective cohort design which accords it more strength to understand the reasons for discontinuation at the different time points. The several time points of follow-up at shorter intervals enabled us to determine the reasons for discontinuation with less recall trouble.
This study was not without limitations. First, adherence or continuation was self-reported, which leaves it subject to response bias. Secondly, a sample size smaller than the calculated minimum size was used due to limited numbers of new acceptors of contraceptives in the original RCT. This left the study with a lower power to estimate associations. Lastly, over 40% of our participants were lost to follow-up due to the nature of the refugee settlement where people are always moving in search for a better life, employment, education, and safety. This could have led to an underestimation of adherence rates and associated factors. However, we carried out a sensitivity analysis to better understand the impact of those lost to follow-up, and this gave us similar conclusions to those drawn from the primary analysis.
Conclusion
Adherence to reversible modern contraceptives among female refugee adolescents was very low, leaving the girls at a high risk of pregnancy and associated complications. Side effects and partner prohibition were the most reported reasons for non-adherence, so we recommend that interventions to increase knowledge on how to deal with side effects and increase partner involvement are studied and implemented. Participants who used LARCs were more likely to adhere than those who used SARCs, therefore LARCs should be recommended among adolescents, especially in refugee settings, because of their ease of use and convenience coupled with greater effectiveness. We also advise that future research in similar settings should keep it in mind that they will most likely face a high loss to follow-up, so this should be factored into their sample size estimation.
Abbreviations
RCT, randomised controlled trial; LARC, long-acting reversible contraceptives; SARC, short-acting reversible contraceptives; IUD, intra-uterine device; GEE, generalised estimating equations; ITT, intention-to-treat analysis; PP, per protocol analysis.
Data Sharing Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethical Approval and Consent to Participate
Ethical clearance was obtained from the School of Medicine Higher Degrees Research Ethics Committee (REC REF 2018-059), and from Uganda National Council of Science and Technology (SS 4876). We ensured that all participants gave their written informed consent before enrolling them into the study, and guaranteed their confidentiality with the use of number codes instead of participant names. For participants below 18 years, we did not seek for parental consent because it is stated in the National Policy Guidelines and Service Standards for Sexual and Reproductive Health and Rights that all individuals seeking family planning services are eligible to receive the services regardless of their age, without need for verbal or written consent from parent, guardian, or spouse, as long as they have received prior education or counselling about the contraceptives.28 All interviews were held in private places where discussions could not be overheard.
Acknowledgments
We would like to acknowledge the female refugee adolescents who agreed to participate in our study, our research assistants Anthony Okello, Stella Acayo, Suzan Achayo, and Richard Kidega, and the data entrant Viola Nakiwolo. Special thanks go to Errol Ssozi and Phiona Agemo for proof reading the manuscript and writing assistance.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded in part by the Swedish International Development Cooperation Agency (Sida) and Makerere University under Sida contribution No: 51180060. The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure
Professor Kristina Gemzell-Danielsson reports personal fees from Organon7MsD, Bayer, Gedeon Richter, Mithra, Natural Cycles, MedinCell, ObsEva, and Cirqle, outside the submitted work. The authors declare that they have no other competing interests for this work.
References
1. UNICEF. Early childbearing; 2019. Available from: https://data.unicef.org/topic/child-health/adolescent-health/.
2. WHO. Adolescent pregnancy; 2020. Available from: https://www.who.int/en/news-room/fact-sheets/detail/adolescent-pregnancy.
3. UNFPA. Adolescent pregnancy; 2017.
4. Affairs. UNDoEaS. World Population Prospects, 2019 Revision: age-specific fertility rates by region, subregion and country, 1950–2100 (births per 1,000 women) Estimates. Online Edition; 2021.
5. Population Division D. World Population Prospects 2017, Births by five-year age group of mother, region, subregion and country, 1950–2100; 2017.
6. Sully EA, Atuyambe L, Bukenya J, Whitehead HS, Blades N, Bankole A. Estimating abortion incidence among adolescents and differences in post abortion care by age: a cross-sectional study of post abortion care patients in Uganda. Contracept. 2018;98(6):510–516. doi:10.1016/j.contraception.2018.07.135
7. Bakesiima R, Cleeve A, Larsson E, et al. Modern contraceptive use among female refugee adolescents in northern Uganda: prevalence and associated factors. Rep Health. 2020;17(1):67. doi:10.1186/s12978-020-00921-y
8. UNHCR. Documenting Knwl, Atti Practices of Ref Status Fam Pln Svc in UNHCR’s Oper Nakivale Ref Settlement; 2011.
9. UNHCR. Annual Public Health Global Review; 2019 Available from: https://www.unhcr.org/606f10d04.pdf.
10. World Health Organisation. Global Health Estimates 2015: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2015. Geneva: World Health Organisation; 2016.
11. Grønvik T, Fossgard Sandøy I. Complications associated with adolescent childbearing in Sub-Saharan Africa: a systematic literature review and meta-analysis. PLoS One. 2018;13(9):e0204327–e. doi:10.1371/journal.pone.0204327
12. Kabagenyi A, Habaasa G, Rutaremwa G. Low contraceptive use among young females in Uganda: does birth history and age at birth have an influence? Analysis of 2011 Demographic and Health Survey. J Contracept Studies. 2016;1(1):4.
13. Tanabe M, Myers A, Bhandari P, Cornier N, Doraiswamy S, Krause S. Family planning in refugee settings: findings and actions from a multi-country study. Conflict Health. 2017;11(1):9. doi:10.1186/s13031-017-0112-2
14. Bakesiima R, Beyeza-Kashesya J, Tumwine JK, et al. Effect of peer counselling on acceptance of modern contraceptives among female refugee adolescents in northern Uganda: a randomised controlled trial. PLoS One. 2021;16(9):e0256479. doi:10.1371/journal.pone.0256479
15. Darroch J, Woog V, Bankole A, Ashford L. Adding It Up: Costs and Benefits of Meeting the Contraceptive Needs of Adolescents. New York: Guttmacher Institute; 2016.
16. Boamah E, Asante KP, Mahama E, et al. Use of contraceptives among adolescents in Kintampo, Ghana: a cross-sectional study. Open Access J Contracept. 2014;5:7–15. doi:10.2147/OAJC.S56485
17. Blanc A, Curtis S, Croft T. Monitoring contraceptive continuation: links to fertility outcomes and quality of care. Stud Fam Pln. 2002;33(2):127–140. doi:10.1111/j.1728-4465.2002.00127.x
18. Blanc A, Tsui A, Croft T, Trevitt J. Patterns and trends in adolescents’ contraceptive use and discontinuation in developing countries and comparisons with adult women; 2009. Available from: https://www.guttmacher.org/sites/default/files/article_files/3506309.pdf.
19. Clare C, Fraser C. Contraception Adherence among East Harlem Adolescents. Gynecol Obstet. 2013;3(177):2161–0932.
20. Richard M J, Okonya N, Sara G, Michelene C. Predictors of Contraceptive Adherence among Women Seeking Family Planning Services at Reproductive Health Uganda, Mityana Branch. Int J Popul Res. 2013;2015:8.
21. Usinger KM, Gola SB, Weis M, Smaldone A. Intrauterine Contraception Continuation in Adolescents and Young Women: a Systematic Review. J Pediatric Asl Gynecol. 2016;29(6):659–667. doi:10.1016/j.jpag.2016.06.007
22. Diserens C, Quach A, Mathevet P, Ballabeni P, Jacot-Guillarmod M. Adolescents’ contraception continuation in Switzerland: a prospective observational study. Swiss Med Weekly. 2017;147:w14504.
23. UNHCR. Uganda - Refugee Statistics December 2020 – palabek; 2021.
24. Hulley S. Designing Clinical Research.
25. Sznajder KK, Tomaszewski KS, Burke AE, Trent M. Incidence of discontinuation of long-acting reversible contraception among adolescent and young adult women served by an urban primary care clinic. J Pediatric Adolesc Gynecol. 2017;30(1):53–57. doi:10.1016/j.jpag.2016.06.012
26. Jay MS, DuRant RH, Litt IF. Female adolescents’ compliance with contraceptive regimens. Pediatr Clin North Am. 1989;36(3):731–746. doi:10.1016/S0031-3955(16)36700-1
27. Durant RH, Jay MS, Linder CW, Shoffitt T, Litt I. Influence of psychosocial factors on adolescent compliance with oral contraceptives. J Als Health Care. 1984;5(1):1–6. doi:10.1016/S0197-0070(84)80237-5
28. Ministry of Health. The National Policy Guidelines and Service Standards for Sexual and Reproductive Health and Rights, Uganda; 2006:19–20.
29. Raine T, Foster-Rosales A, Upadhyay UD, et al. One-year contraceptive continuation and pregnancy in adolescent girls and women initiating hormonal contraceptives. Obstet Gynecol. 2011;117(2):363–371. doi:10.1097/AOG.0b013e31820563d3
30. Lara-Torre E, Schroeder B. Adolescent compliance and side effects with Quick Start initiation of oral contraceptive pills. Contracept. 2002;66(2):81–85. doi:10.1016/S0010-7824(02)00326-8
31. Jensen JTC, Mitchell D. Speroff & Darney’s Clinical Guide to Contraception.
32. Stoddard A, McNicholas C, Peipert JF. Efficacy and safety of long-acting reversible contraception. Drugs. 2011;71(8):969–980. doi:10.2165/11591290-000000000-00000
33. Secura GM, Allsworth JE, Madden T, Mullersman JL, Peipert JF. The contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol. 2010;203(2):115.e1–.e1157. doi:10.1016/j.ajog.2010.04.017
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
