Back to Journals » Patient Preference and Adherence » Volume 16
Adaptation and Validation of the Spanish Version of Decisional Conflict Scale in People with Migraine in Spain
Authors Guerrero-Peral AL , Porta-Etessam J, Rodríguez-Vico J, Núñez M, Ciudad A, Díaz-Cerezo S, Garí-Peris C, Pérez-Sádaba FJ, Lizán L, Santos-Lasaosa S
Received 30 July 2022
Accepted for publication 3 December 2022
Published 15 December 2022 Volume 2022:16 Pages 3291—3302
DOI https://doi.org/10.2147/PPA.S384333
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Ángel Luis Guerrero-Peral,1 Jesús Porta-Etessam,2 Jaime Rodríguez-Vico,3 Mercedes Núñez,4 Antonio Ciudad,4 Silvia Díaz-Cerezo,4 Carla Garí-Peris,5 Francisco Javier Pérez-Sádaba,5 Luis Lizán,5 Sonia Santos-Lasaosa6
1Headache Unit, Neurology Department, Hospital Clínico Universitario de Valladolid, Valladolid, Spain; 2Neurology Department, Hospital Clínico San Carlos, Madrid, Spain; 3Neurology Department, Fundación Jimenez Diaz, Madrid, Spain; 4Medical Department, Eli Lilly, Madrid, Spain; 5Outcomes’ 10, Castellón, Spain; 6Neurology Department, Hospital Clínico Universitario Lozano Blesa, Zaragoza, Spain
Correspondence: Mercedes Núñez, Eli Lilly, Av. de la Industria, 30, Alcobendas, Madrid, 28108, Spain, Tel +34 647447827, Email [email protected]
Purpose: We aimed to validate the Spanish version of the Decisional Conflict Scale (DCS) and analyze its psychometric properties in people with migraine.
Patients and Methods: The DCS validation comprised two phases. First, a translation and cross-cultural adaptation following the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) Good Practices: 1-preparation, 2-independent forward translation, 3-reconciliation, 4-back-translation, 5-harmonization, 6-clinical review, and 7-content validation in a group of migraine patients. Second, the analysis of the psychometric properties. The reliability or internal consistency of the DCS scale and subscales was assessed using Cronbach’s α value. The item-subscale correlation was also evaluated. A floor and ceiling effects for DCS score was considered when at least 15% of respondents obtained DCS > 90 (ceiling) or < 10 (floor). The construct validity was studied through the correlation between the DCS subscales and by the correlation between the DCS and other questionnaires (Decision Self-Efficacy Scale [DSES] and 9-item Shared Decision-Making [SDM-Q-9]). Spearman’s coefficients were estimated for the correlations.
Results: The cross-cultural adaptation was conducted on 17 patients who completed the questionnaire in a mean of 2.4 ± 1.1 minutes. Generally, more than 75% of them considered that DCS items were adequate, easy to understand, and relevant. The psychometric properties were evaluated in a sample of n=128 patients. Accordingly, the internal consistency of DCS was high, with a Cronbach’s α of 0.97 for the scale and between 0.87 to 0.96 for subscales. Also, a slight floor effect was observed, with 24.2% of patients having DCS scores < 10. The correlation between subscales exceeded Spearman’s coefficient of 0.7. Whereas the correlation between the DCS and the other questionnaires was generally moderate (Spearman’s coefficient > 0.4).
Conclusion: The Spanish version (Spain) of the DCS has very acceptable psychometric properties (reliability and construct validity) and good potential for assessing decisional conflicts among migraine patients.
Keywords: migraine, decision-making, decisional conflict scale, psychometric properties, adaptation, Spanish
Introduction
Migraine is a chronic neurological disorder characterized by recurring headache attacks.1 Particularly affects younger women and is one of the most prevalent worldwide, with 1.1 billion cases in 2019.2 Headache attacks can vary considerably between and within patients over time. They are often incapacitating and excruciating and are accompanied by bothersome symptoms such as nausea, vomiting, photophobia, or phonophobia.1. There is a wide range of treatments available— such as various acute and preventive drugs and non-pharmacological therapies— which have been expanded in recent years with novel mechanism-based drugs.3 All these therapeutic options might lessen the migraine’s burden, but they can also present a challenge to the already difficult therapeutic management of the disease.3
In migraine, the interpretation and response to pain as well as its impact on patient’s life vary widely between and within individuals4. At the same time, response to medication in migraine is also highly variable and subjective.5 This can make it difficult to make treatment decisions compared to other chronic conditions. Therefore, selecting a suitable and effective therapy for migraines can be a complex task for both physicians and patients. Therapeutic decisions pose what is called a decisional conflict, which is defined as a personal uncertainty about which course of action to take when a choice among competing options involves risk, regret, or challenge to personal life values.6 The decisional conflict scale (DCS) tool is available to identify the decisional conflict that patients might experience regarding health care decisions.7 This tool might help physicians understand how uncertain patients are about therapeutic decisions and take the appropriate measures, such as providing patients with more information about the treatment options, promoting their engagement with their treatment, and making them more involved in therapeutic decision-making.8,9 The involvement of migraine patients in their treatment is particularly important since the control of the disease seems to improve when patients actively participate in their treatment decisions.10
The DCS has been widely used in research11 in multiple populations and settings, demonstrating its value as a decision-making evaluation measure11 and has been adapted into numerous languages.12–16 However, until now, the DCS has not been adapted to Spanish from Spain. Thus, we aimed to validate the Spanish version of the DCS for the people with migraine in Spain. Our specific objectives were to cross-culturally adapt the DCS to the Spanish population and analyze its psychometric properties.
Materials and Methods
The validation of the Spanish DCS version was performed in two consecutive phases: the first consisted of the translation and cross-cultural adaptation to Spanish (from Spain); the second was to analyze the psychometric properties of the resulting version of the DCS.
The DCS is a 16-item scale comprising five dimensions or subscales: uncertainty (3 items), feeling informed (3 items), clarity related to personal values (3 items), feeling supported (3 items), and effective decision-making (4 items). Each item is measured on a 5-point Likert scale ranging from 0 (strongly agree) to 4 (strongly disagree), leading to a total score of between 0 and 64, which is converted into a standardized score from 0 (no decisional conflict) to 100 (highest decisional conflict). Scores below 25 are associated with being able to implement a decision, whereas those above 37.5 are associated with decision delay.17
Translation and Cross-Cultural Adaptation
The translation and cross-cultural adaptation of the original DCS were carried out between April and July 2020. It was performed following the International Society for Pharmacoeconomics and Outcomes Research (ISPOR), which recommended 7 steps:18 from the translation and harmonization of the Spanish version of the DCS to the cross-cultural adaptation or cognitive debriefing (pilot study) (Supplementary Figure 1). Patients’ sample size was estimated according to the ISPOR guidelines,18 which recommended a group of 5 to 8 patients of a specific region for the cross-cultural adaptation of an instrument. Thus, we considered a sample size of approximately 8 migraine patients per site as patients were recruited from two centers located in two different regions in Spain.
For the pilot test (carried out between May and July 2020), migraine patients treated at two headache outpatient clinics from two Spanish public hospitals were invited to an interview if a) they were 18 years or older, b) had the ability to participate in shared decision-making, c) had the ability to understand and answer the questions of the questionnaire, d) had provided their written informed consent to participate.18
Patients were given the questionnaire on paper and were subsequently interviewed by telephone so that they could read the questions during the interview. They were first made to answer the DCS (thinking aloud), and the response time to the questionnaire was collected. Then, patients were asked to give their opinion on the DCS length and presentation. Additionally, patients were asked to explain each item in their own words and rate them individually with respect to their understandability, adequacy of the response options, ease of responding, and relevance to the conflict in decision-making. They rate their level of agreement with responses with a 5-point Likert scale (from 1 [strongly disagree] to 5 [strongly agree]). The surveys were distributed and data were collected between May and June 2020 (Details of the survey for the cross-cultural adaptation are presented in the Supplementary Table 1).
Psychometric Properties
The last step for the DCS validation consisted of the analysis of the psychometric properties of the DCS Spanish version. This analysis was set out as part of a main intervention study aimed at evaluating the impact of a training course for neurologists on migraine patients’ decisional conflict. Migraine patients were treated at 4 public Spanish hospitals and were invited to answer an online questionnaire if a) they were 18 years or older, b) had the ability to participate in shared decision making, c) had the ability to understand and answer the questions of the questionnaires used; d) were undergoing acute and/or preventive pharmacological treatment and whose doctors were considering a change in this treatment; e) had provided their written informed consent to participate. The migraine patients’ sample size of 132 was estimated to meet the main objective of the intervention study. Nevertheless, it was confirmed that this sample was sufficient for the psychometric properties’ analysis in terms of internal validity (Cronbach’s α test).19 Accordingly, a minimum sample size of 20 was obtained using the Bonett et al20 formula and assuming a Cronbach’s α value greater than 0.7, a power of 90%, and an alpha risk of 0.05.
Patients completed the DCS in addition to two other surveys related to the decision-making process: the Decision Self-Efficacy Scale (DSES),21 which assesses patient’s self-confidence in making informed decisions, and the 9-item Shared Decision-Making (SDM-Q-9) questionnaire,22 which measures the degree of involvement of patients in the shared decision-making process. For the DCES, each item is measured on a 5-point Likert scale ranging from 0 (lower confidence) to 4 (greater confidence), leading to a total score between 0 and 44; whereas for the SDM-Q-9, each item is rated on a 6-point Likert scale from 0 (strongly disagree) to 5 (strongly agree), leading to a total score between 0 and 45. Both scores are converted into a 0 to 100 scale, with 100 being the highest level of patients’ self-confidence (for DCES) or involvement in decision-making (for SDM-Q-9).
Physicians collected patients’ socio-demographic (age, gender, education level) and clinical (type of migraine, time since diagnosis, number of previous treatment failures, assessment of change of pharmacological treatment, and decision after change) variables. Patients were included in the study between September 2020 and October 2021 (Details of the survey for the psychometric properties analysis are presented in Supplementary Table 2).
Ethical Considerations
The study protocol was approved by the Research Ethics Committees of the Hospital Clínico Universitario de Valladolid (Valladolid) (code: EPA 20–326). All patients who met the inclusion criteria were informed about the purpose and procedures of the studies and signed a consent form before inclusion.
Data Analysis
For the descriptive analysis, qualitative variables were estimated using absolute and relative frequencies, whereas quantitative variables were calculated by measures of central tendency and dispersion (mean, standard deviation [SD], percentile, maximum and minimum).
Cross-Cultural Adaptation
For the cross-cultural adaptation or cognitive debriefing (pilot test), the mean (±SD) of the time required to complete the DCS was calculated for the total sample of patients. In addition, for each questionnaire’s item, the relative and absolute frequencies of the patients who were awarded high (4 or 5), medium (3), or low (1 or 2) scores were estimated for each of the assessed qualities: understandability, adequacy of the response options, ease of responding and relevance for the conflict in decision making. When less than 75% of patients scored high (4 or 5) on an item’s understandability, it was considered to modify that item’s wording according to the patients’ answer to the “explain this statement in your own words” question. Likewise, when less than 75% of patients scored high on the ease of responding to an item, it was considered to exclude that item from the questionnaire unless the item’s relevance was awarded high scores for more than 75% of patients.
Psychometric Properties
For the psychometric properties, the reliability, and the construct validity were analyzed.
Reliability (Internal Consistency)
The reliability, which measures the ability of the questionnaire items to measure the same construct, was assessed using Cronbach’s α value (Cronbach α ranges from 0 to 1; values > 0.7 indicated good internal consistency)23 for the total DCS scale, as well as for each of its five subscales. Additionally, the item-subscale correlation was assessed after removing the item being tested at the time to avoid an overestimation of the correlation coefficient. The subscale correlation aimed to verify that the items correlate more strongly with their own subscale than with the others. Spearman’s coefficients were calculated for these correlations.
The floor and ceiling effect for the global DCS scale, which measures the ability of the questionnaire to discriminate between the respondents with low scores (floor effect) and between those with high scores (ceiling effect), was assessed. For this purpose, the proportion of patients who obtained a global DCS score of less than 10 or more than 90 was estimated. A ceiling or floor effect was considered present if at least 15% of respondents obtained scores above 90 or below 10, respectively.24 A floor effect would involve a DCS low discriminatory ability among patients with lower decisional conflict, whereas the ceiling effect would mean a low discriminatory ability among patients with higher decisional conflict. In both cases the reliability of the questionnaire would be reduced.
Construct Validity
The construct validity, which is the correlation between scales or dimensions measuring the same construct, was first evaluated through the correlation between the subscales within the DCS questionnaire and, subsequently, by the correlation between the DCS and other questionnaires (DSES and SDM-Q-9) scores and by the matrix of correlations between DCS and SDM-Q-9 individual items (convergent validity). Spearman’s coefficients were estimated for these correlations (Supplementary Table 3 shows the interpretation of Spearman correlation where 0 would represent no correlation and 1 a perfect correlation).25 Apart from the strength of the correlations, which determined the convergent validity, correlations between DCS and scales SDM-Q-9 and DSES were predicted to be inverse: ie, it was expected that a patient with low decisional conflict (low DCS scores) had a high degree of decisional involvement (high SDM-Q-9 scores) and high self-confidence (high DSES scores) and vice versa. That way, the questionnaires’ scores were used as quality control for patients’ understandability: patients who presented higher scores than the specified cut-off points for all questionnaires (DCS >80, SDM-Q-9 >80, and DSES >70) and therefore showed a double divergence (between DCS and SDM-Q-9 and between DCS and DCSE scores), were excluded from the analysis since it was considered that they had a lack of attention and understanding of the questionnaires.
The data analysis was performed using the STATA version 14 statistical software package. Results were considered statistically significant for all the statistical tests when p < 0.05.
Results
Translation and Cross-Cultural Adaptation
After the back-forward translation, we obtained a harmonized Spanish version of the DCS. This version was then tested in a pilot study with a sample of 17 Spanish patients. Most of these patients were females (88%) and had a mean ± SD of 38.8 ± 11.1 years, and a mean time since diagnosis of 17.2 ± 12.2 years.
For patients, the mean time to complete the questionnaire was 2.4 ±1.1 minutes, and 82.4% of them considered that the DCS had an adequate length, rating it as “short”, “simple”, and “easy to answer”. In addition, most patients (88.2%) deemed the presentation of the DCS adequate.
Additionally, most patients awarded high scores to the items’ understandability, adequacy of the response options, relevance to decision-making conflict, and ease of responding (Figure 1), except for item 14, “My decision shows what is important for me”, as only 65% of patients rated it with 4 or 5 scores in terms of understanding. Item 14 was consequently modified to “My decision reflects the treatment aspects that matter most to me”. After this modification, 76.9% of participants considered the item to be easier to understand (The cross-cultural validated version of the questionnaire is shown in Supplementary Table 4).
Psychometric Properties
A total of 145 migraine patients completed the online survey after the evaluation of change of pharmacological treatment with their physicians (the average scores for DCS, SDM-Q-9, and DSES questionnaires are presented in the Supplementary Table 5). Out of 145 patients, 17 presented high scores for all questionnaires (as prespecified in the analysis methods: DCS >80, SDM-Q-9 >80, and DSES >70). Therefore, these patients were excluded from the analysis since it was considered that their answers were not correct due to lack of attention and comprehension of the questionnaires (See Supplementary Figure 2).
After the exclusion of these patients, responses from 128 patients were included in the psychometric properties assessment. The characteristics of the migraine participants (n=128) are presented in Table 1. Most (85.3%) were female with a mean age of 39.0 ±12.4 years. Patients presented a low decisional conflict with a mean score of 23.7 ± 20.6 for DCS. As expected of the low conflict, they scored high in relation to their degree of involvement in the decision-making process (79.0 ±19.4 measured by the SDM-Q-9) and in their decision self-efficacy (80.0±14.6 measured by DSES). Supplementary Table 6 shows the characteristics and questionnaire scores of the excluded patients (n=17) and the whole population (N=145). It was observed that the mean age of excluded patients was slightly lower than that of the entire population (31.1 ±10.5 vs 38.1 ±12.4). Also, a smaller proportion of these patients had higher education (29.4% vs 44.1%); they had fewer years of experience with the disease (7.9 ±8.5 vs 13.6 ±13.4), and a higher percentage had ≥ 3 previous treatment failures (35.3% vs 19.3%) when compared with the rest of the population.
 |
Table 1 Migraine Patients’ Sociodemographic and Clinical Characteristics |
Reliability (Internal Consistency)
The internal consistency was very high for the DCS scale, with a Cronbach’s α of 0.97, and for all the subscales, with Cronbach’s α ranging from 0.87 to 0.96. Additionally, a strong correlation was found between each item and its subscale (See Table 2).
 |
Table 2 Results of Internal Consistency of the DCS Subscales, Cronbach's Alpha, and Item-Subscale Correlation (n=128) |
The percentage of patients having DCS scores < 10 was above 15% (24.2%), meaning that a floor effect was observed for the DCS global scores. In turn, the percentage of patients having DCS scores > 90 was lower than 15% (2.3%); therefore, no ceiling effect was detected for the DCS.
Construct Validity
The correlation between DCS subscales was high, being especially strong (exceeding Spearman’s coefficient of 0.7) between the subscales “feeling informed” and “clarity related to personal values”, as well as between “feeling supported” and “effective decision-making” (Table 3). Moreover, the correlation between the DCS and the DSES (- 0.5600) and the SDM-Q-9 (- 0.4785) total scores was moderate.
 |
Table 3 Results of the Correlation between DCS Subscales (n=128) |
As for the convergent validity between the subscales of the DCS and the DSES and SDM-Q-9 total scores, a higher correlation was obtained between the DSES and the “feeling supported” and “effective decision-making” subscales of the DCS, as well as with the SDM-Q-9 with the “feeling informed” and “effective decision-making” subscales, although all the correlations were still moderate (Table 4).
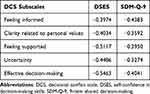 |
Table 4 Results of the Correlation Between the Subscales of the DCS and the DSES and SDM-Q-9 Total Scores |
Finally, as for the matrix of correlations, low and moderate correlations were observed between DCS and SDM-Q-9, mainly with the “effective decision-making” and the “feeling informed” subscales of the DCS (See Figure 2 for the matrix of correlations results).
 |
Figure 2 Results of the matrix of correlations between SMD-Q-9 questionnaire items and the DCS. Abbreviations: DCS, decisional conflict scale; SDM-Q-9, 9-item shared decision-making. |
Discussion
The purpose of this study was twofold: first, to translate and cross-culturally adapt the DCS for the population in Spain, and second, to assess the psychometric properties of the resulting Spanish DCS version. Additionally, this study, to our knowledge, was the first to evaluate the DCS in patients with migraine for a therapeutic decision process.
The translation and adaptation process was carried out following ISPOR recommendations.18 Overall, migraine patients in our study considered that DCS was well presented and that the questionnaire‘s items were easy to understand and relevant to measure decision-making conflict. Only one of the items was reworded to facilitate its understanding (item 14). In addition, our findings obtained from a sufficiently large sample of migraine patients showed that the Spanish version of the DCS had good psychometric properties in terms of reliability and construct validity (including convergent validity). These findings reinforce the validity and reliability previously reported for the DCS in other settings.7,13,15,16,26
As for the reliability, the DCS scale and the 5 subscales showed a very strong correlation, with Cronbach’s α exceeding 0.87. These results are concordant with that observed in other cultural and linguistic spheres: including other decisional evaluations about undergoing screening tests7,13 or treatment changes.15,16,26 These results demonstrate that the items are robust in measuring very distinctive decisional processes. The correlation between DCS subscales was also high, exceeding Spearman’s coefficient of 0.7 for the subscales’ pairs: “feeling informed” and “clarity related to personal values”, as well as “feeling supported” and “effective decision-making”, indicating that these subscales measure similar concepts within the same construct, as evidenced by the high Cronbach’s alpha values. A strong correlation between these subscales was also found in the mandarin Chinese validation of the DCS.13 In addition, the item-subscale consistency was particularly strong in our study, being greater than 0.8 for most of the items, pointing out that the items among the same subscale are strongly related to each other and that each item is relevant and useful within its subscale. These item-subscales correlations coincided with those obtained in the validation of the Japanese version of the DCS.16
As for the convergent validity of DCS with other questionnaires, Spearman’s rank correlation analysis indicated an inverse and moderate correlation between DCS and the DSES (−0.5600) and SDM-Q-9 (−0.4785) questionnaires. These inverse correlations were expected between the DCS and the other two questionnaires since lower DCS scores indicate a low decisional conflict, and these should correlate with high patient self-confidence (DSES) and high patient involvement in decision-making (SDM-Q-9) scores. In addition, the moderate correlation demonstrates the DCS evaluates concepts that are similar but not identical to those assessed with the other questionnaires, so we could consider that these questionnaires are complementary. We also observed a similar correlation between the 5 subscales of DCS and the total scores of DSES and SDM-Q-9, with this convergence being stronger for the subscale “effective decision-making” and the DSES (−0.5463) and SDM-Q-9 (−0.4041) scores. The correlation between the subscale “effective decision-making” and the SDM-Q-9 was also confirmed at the item level in our matrix analysis. Our results were in line with those of two other studies carried out in very different settings: one in patients with newly diagnosed or newly growing vestibular schwannomas in Canada,27 showing an inverse correlation between the SDM-Q-9 and DCS (−0.539), and the other conducted on Japanese patients facing a treatment decision process in primary care settings,26 where a significant inverse correlation was also obtained between the SDM-Q-9 and DCS (−0.577; p < 0.05). In the Japanese study, a correlation between the 5 subscales of DCS and the SDM-Q-9 scores was also found, with the subscale “clarity related to personal values” (−0.646; p < 0.05) being stronger. The similarity between our results and those obtained in other settings supports the convergence validity of DCS and SDM-Q-9 questionnaires and confirms the compatibility of both questionnaires with very different settings and cultures.
Finally, our results indicate that the Spanish version of the DCS was a valid tool for assessing decisional conflicts among migraine patients facing a treatment change. Patients, in general, had low decisional conflict punctuations and high self-confidence and level of involvement in the decision-making process. In this sense, mean DCS values (23.7 ± 20.6) for migraine patients were lower than those identified for other populations.13,14,16 These results are not surprising as previous studies showed that migraine patients are generally very actively involved in their treatment care and decision-making process28 as they face a very bothersome condition and they desperately seek out treatment to provide them with rapid and complete pain relief.29 The fact that migraine patients have, in general, low decisional conflict might explain the slight floor effect of the DCS scores found in our population, as the distribution of patients’ answers was slightly skewed to lower scores (< 10). This effect might mean that the DCS has a lower ability to discriminate between patients with lower scores (low decisional conflict) than between those with higher scores (high decisional conflict scores). The floor effect might imply that minor improvements in decisional conflict among patients with low scores (low decisional conflict) would not be completely detected. On the other hand, the absence of the ceiling effect might imply that any eventual increase in patients’ decisional conflict might be successfully detected in this population, regardless of patients’ scores.
This study has some limitations which should be mentioned. The first relates to the fact that our data rely on patient-reported outcomes measures to assess patients’ perspectives on the decision-making process. We acknowledge that patient self-reported measures are subjective and might be affected by different factors associated with patients themselves, such as their expectations or previous experiences with treatment, or external factors such as their interactions with the healthcare providers or their socioeconomic situation. Despite this possible limitation, we believed our results were robust as we addressed patients’ perspectives about decision-making with three different tools representing different approaches and obtained the expected correlations between them. A second limitation might be related to the fact that we did not include the test-retest reliability or the divergent construct validity in the psychometric analyses. The test-retest reliability was not feasible in our study since patients only completed the questionnaires once. As for divergent construct validity, since the questionnaires measured different aspects of the SDM and were therefore related, we considered it more appropriate to test for convergent than divergent validity. Another limitation could be linked to our results’ generalization, as we excluded a small group of patients with atypical answers. This exclusion might have impaired the representativeness of the migraine population since this group of patients were younger and had, in general, a lower educational level, experience with the disease, or a greater percentage of failure with previous treatments than the rest of the population. In any case, it cannot be established that their characteristics influenced their responses. Also, we believe that it was necessary to exclude them since their answers might have affected the integrity of the psychometric properties analysis. Another implication of these patients with divergent responses is that they may have difficulty understanding the scoring of DCS, particularly considering that it differs from other ratings (higher scores indicate lower agreement and greater decisional conflict). Healthcare professionals should therefore consider this potential difficulty when administering the DCS to patients. A fourth limitation could be the fact that patients were treated at high specialization clinics for headache management. Therefore, the low decisional conflict obtained and the high involvement of patients in decision-making may not reflect the reality of all patients living with migraines in our settings.
Conclusion
The Spanish version of the DCS was well accepted by migraine patients in Spain, with very acceptable psychometric properties in terms of internal consistency and convergent validity. Our results not only confirm the convergent validity between the DCS and SDM-Q-9 scales observed in other settings, but also with the DSES scale, indicating that the greater the patient’s self-confidence, the less decisional conflict. Furthermore, this tool has demonstrated a good potential for use in assessing decisional conflicts among migraine.
Acknowledgments
The authors wish to thank Lucía Pérez-Carbonell at Outcomes’10 (Castellón, Spain) for their assistance with the medical writing.
Funding
Eli Lilly Spain has financed the publication of this article.
Disclosure
ALGP, JPE, JRV and SSL declare they have no conflicts of interests to disclose. MN, AC and SDC are employees of Eli Lilly, Madrid, Spain. CGP, FJPS and LL work for an independent research entity, Outcomes’10, that received funding from Eli Lilly to conduct the project and for medical writing.
References
1. Dodick DW. Migraine. Lancet. 2018;391(10127):1315–1330. doi:10.1016/S0140-6736(18)30478-1
2. Safiri S, Pourfathi H, Eagan A, et al. Global, regional, and national burden of migraine in 204 countries and territories, 1990 to 2019. Pain. 2022;163(2):e293–e309. doi:10.1097/j.pain.0000000000002275
3. Ashina M, Buse DC, Ashina H, et al. Migraine: integrated approaches to clinical management and emerging treatments. Lancet. 2021;397(10283):1505–1518. doi:10.1016/S0140-6736(20)32342-4
4. Kim S, Bae DW, Park SG, Park JW. The impact of pain-related emotions on migraine. Sci Rep. 2021;11(1):577. doi:10.1038/s41598-020-80094-7
5. Blumenfeld AM. Clinician-patient dialogue about preventive chronic migraine treatment. J Prim Care Community Health. 2020;11:2150132720959935. doi:10.1177/2150132720959935
6. LeBlanc A, Kenny DA, O’Connor AM, Légaré F. Decisional conflict in patients and their physicians: a dyadic approach to shared decision making. Med Decis Making. 2009;29(1):61–68. doi:10.1177/0272989X08327067
7. O’Connor AM. Validation of a decisional conflict scale. Med Decis Making. 1995;15(1):25–30. doi:10.1177/0272989X9501500105
8. Steiner TJ, Jensen R, Katsarava Z, et al. Aids to management of headache disorders in primary care (2nd edition): on behalf of the European headache federation and lifting the burden: the global campaign against headache. J Headache Pain. 2019;20(1):57. doi:10.1186/s10194-018-0899-2
9. Buse DC, Gillard P, Arctander K, Kuang AW, Lipton RB. Assessing physician-patient dialogues about chronic migraine during routine office visits. Headache. 2018;58(7):993–1006. doi:10.1111/head.13314
10. Silberstein SD, Goadsby PJ, Lipton RB. Management of migraine: an algorithmic approach. Neurology. 2000;55(9 Suppl 2):S46–S52.
11. Garvelink MM, Boland L, Klein K, et al. Decisional conflict scale use over 20 years: the anniversary review. Med Decis Making. 2019;39(4):301–314. doi:10.1177/0272989X19851345
12. Urrutia M, Campos S, O’Connor A. Validación de una versión en español de la Escala de Conflicto Decisional [Validation of a Spanish version of the decisional conflict scale]. Rev Med Chil. 2008;136(11):1439–1447. Spanish. doi:10.4067/s0034-98872008001100010
13. Xiang JM, Sun K, Zhao Q, Li HB, Gao LL. Psychometric assessment of the mandarin version of the decisional conflict scale with pregnant women making prenatal test decisions. Patient Prefer Adherence. 2022;16:149–158. doi:10.2147/PPA.S346017
14. Lam WW, Kwok M, Liao Q, et al. Psychometric assessment of the Chinese version of the decisional conflict scale in Chinese women making decision for breast cancer surgery. Health Expect. 2015;18(2):210–220. doi:10.1111/hex.12021
15. Koedoot N, Molenaar S, Oosterveld P, et al. The decisional conflict scale: further validation in two samples of Dutch oncology patients. Patient Educ Couns. 2001;45(3):187–193. doi:10.1016/S0738-3991(01)00120-3
16. Kawaguchi T, Azuma K, Yamaguchi T, et al. Development and validation of the Japanese version of the decisional conflict scale to investigate the value of pharmacists’ information: a before and after study. BMC Med Inform Decis Mak. 2013;13:50. doi:10.1186/1472-6947-13-50
17. O’Connor AM. User manual-decisional conflict scale; 2021. Available from: https://decisionaid.ohri.ca/eval_dcs.html.
18. Wild D, Grove A, Martin M, et al. Principles of good practice for the translation and cultural adaptation process for Patient-Reported Outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value Health. 2005;8(2):94–104. doi:10.1111/j.1524-4733.2005.04054.x
19. Bujang MA, Omar ED, Baharum NA. A review on sample size determination for cronbach’s alpha test: a simple guide for researchers. Malays J Med Sci. 2018;25(6):85–99. doi:10.21315/mjms2018.25.6.9
20. Bonett D. Sample size requirements for testing and estimating coefficient alpha. J Educ Behav Stat. 2002;27:335–340. doi:10.3102/10769986027004335
21. User manual. Available from: https://decisionaid.ohri.ca/docs/develop/user_manuals/UM_decision_selfefficacy.pdf.
22. Simon D, Schorr G, Wirtz M, et al. Development and first validation of the shared decision-making questionnaire (SDM-Q). Patient Educ Couns. 2006;63(3):319–327. doi:10.1016/j.pec.2006.04.012
23. Apuntes de consistencia interna de las puntuaciones de un instrumento de medida [Notes on the internal consistency of the scores of a measuring instrument]. Available from: https://www.uv.es/friasnav/AlfaCronbach.pdf.
24. Terwee CB, Bot SD, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42. doi:10.1016/j.jclinepi.2006.03.012
25. Spearman’s correlation. Available from: http://www.statstutor.ac.uk/resources/uploaded/spearmans.pdf.
26. Goto Y, Miura H, Son D, et al. Psychometric evaluation of the Japanese 9-item shared decision-making questionnaire and its association with decision conflict and patient factors in Japanese primary care. JMA J. 2020;3(3):208–215.
27. Graham ME, Westerberg BD, Lea J, et al. Shared decision making and decisional conflict in the management of vestibular schwannoma: a prospective cohort study. J Otolaryngol Head Neck Surg. 2018;47(1):52. doi:10.1186/s40463-018-0297-4
28. Peters M, Abu-Saad HH, Vydelingum V, Dowson A, Murphy M. Patients’ decision-making for migraine and chronic daily headache management. A qualitative study. Cephalalgia. 2003;23(8):833–841. doi:10.1046/j.1468-2982.2003.00590.x
29. Xu X, Ji Q, Shen M. Patient preferences and values in decision making for migraines: a systematic literature review. Pain Res Manag. 2021;2021:9919773. doi:10.1155/2021/9919773
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.