Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
Acupuncture and Tuina Treatment for Gross Motor Function in Children with Spastic Cerebral Palsy: A Monocentric Clinical Study
Authors Wang X , Teh SH, Du XG, Wang XH
Received 2 June 2023
Accepted for publication 23 August 2023
Published 30 August 2023 Volume 2023:19 Pages 1875—1886
DOI https://doi.org/10.2147/NDT.S424102
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Richard J Porter
Xing Wang,1,2 Siew Hoon Teh,1 Xiao-Gang Du,2 Xing-Hua Wang1
1M. Kandiah Faculty of Medicine and Health Sciences, Universiti Tunku Abdul Rahman, Kajang, SGR, Malaysia; 2Famous TCM Expert Heritage Studio, Xi’an Encephalopathy Hospital Affiliated to Shaanxi University of Chinese Medicine, Xi’an, Shaanxi, People’s Republic of China
Correspondence: Xing-Hua Wang, M. Kandiah Faculty of Medicine and Health Sciences, Universiti Tunku Abdul Rahman, Kajang, Selangor, Malaysia, Email [email protected]
Objective: Cerebral palsy (CP) is a condition characterized by abnormal pronunciation, posture, and movement, particularly spastic CP, which involves Gross motor dysfunction due to increased muscle tone and stiffness. This monocentric clinical study aims to evaluate the effectiveness of acupuncture and tuina (AT) in improving gross motor function and alleviating associated symptoms in children diagnosed with spastic CP.
Methods: A total of 83 eligible patients received AT treatment, while 85 patients received conventional rehabilitation treatment. Both groups underwent a 12-week treatment period following the research protocol. Pre- and post-treatment assessments included the Modified Ashworth Muscle Tension Scale (MAS), Gross Motor Function Measure (GMFM-D and GMFM-E), 6-min walking distance measurement (6MWD), and Modified Children’s Functional Independence Rating Scale (WeeFIM).
Results: After 12 weeks of treatment, when compared with baseline, the scores of MAS in both AT group and control group are decreased (p< 0.01, p< 0.01), the scores of GMFM-D, GMFME, 6MWD, WeeFIM in both group are increased (p< 0.01 in all indicators). When compared with control group, AT group had significantly lower MAS scores compared to the control group (p< 0.01), indicating reduced muscle tension. Moreover, AT group showed significantly higher scores in GMFM-D, GMFM-E, 6MWD, and WeeFIM compared to the control group (p< 0.01 in all indicators), indicating improved gross motor function and functional independence. The study also revealed an inverse correlation between the children’s age and treatment efficacy (r= − 0.496, p< 0.01 in AT group, r=− 0.540, p< 0.01 in control group), highlighting the importance of early intervention in the management of CP in children.
Conclusion: These findings suggest that AT may effectively enhance gross motor function and alleviate associated symptoms in children diagnosed with spastic CP. Moreover, early initiation of treatment is crucial to maximize therapeutic efficacy in children with spastic CP.
Trial Registration: Chinese Clinical Trial Registry, ChiCTR2200059823. Registered on 12 May 2022.
Keywords: acupuncture, cerebral palsy, modified Ashworth muscle tension scale, gross motor function, the 6-minute walking distance measurement, children’s functional Independence rating scale
Introduction
Cerebral palsy (CP) is a neurological disorder characterized by abnormal posture, pronunciation, and movement. It is attributed to damage to the developing brain, typically occurring before, during, or shortly after birth. The definition of CP has undergone changes over time, as the disorder exhibits clinical and etiological heterogeneity. Among the CP subtypes, spastic CP is the most prevalent, accounting for over 70% of all cases CP.1,2 Global population-based studies indicate a prevalence of CP, ranging from approximately 1.5 to 4 per 1000 children.3–7 In low- and middle-income countries (LMICs), the prevalence of CP is expected to be higher than in high-income countries, carrying an increased risk of severe motor impairments, poor nutritional status, and diminished health-related quality of life.8,9 The poor social adaptability of children with CP due to abnormal motor function, particularly gross motor function, brings significant mental burdens to both the children and their families. The severity of gross motor difficulties in individuals with CP can vary widely, depending on the location and extent of brain damage.10 While some individuals with CP may have only mild difficulties with movement, others may be entirely unable to walk or perform other gross motor activities independently. Research into the treatment of gross motor difficulties in individuals with CP is ongoing, with current treatment options including physical therapy,11 occupational therapy,12 medications,13 surgery,14 hippotherapy,15 and yoga16. Traditional Chinese medicine (TCM),17 especially AT,18 also plays an important role in the treatment of cerebral palsy.
AT is an essential component of TCM and has been used for thousands of years in China to treat various conditions, including CP.19–21 The effectiveness of AT treatments in treating CP has been extensively studied, with many studies showing promising results.13,22,23 One of the advantages of AT treatments is their simplicity and low cost compared to other therapies, making them particularly beneficial in LMICs, where access to expensive medical treatments may be limited. However, the individualized nature of TCM treatment can be a challenge in promoting the use of AT for CP. Each patient’s condition is unique, and practitioners must tailor treatment protocols to the patient’s specific syndrome under the guidance of TCM theory. The treatment protocol utilized in this study is based on The World Federation of Chinese Medicine Societies (WFCMS) TCM protocol, which was drafted by more than 50 experts from seven countries and regions, underwent several rounds of expert validation, and was finally adopted for validation at the 5th Standing Council of the fourth WFCMS held in Hungary in November 2019, which is standardized and easily replicable. This study aims to compare the differences between AT and conventional rehabilitation in improving gross motor function and other related symptoms in children with spastic CP. Additionally, it seeks to further elucidate the potential therapeutic efficacy of AT for treating gross motor function in children with spastic CP.
Methods/Design
Hypotheses
- There are differences in treatment outcomes between AT and conventional rehabilitation in children with spastic CP.
- AT is more effective in improving gross motor function and alleviating associated related symptoms in children with cerebral palsy.
Design
This study is a monocentric, non-randomized, clinical trial that was conducted at Xi’an Encephalopathy Hospital Affiliated to Shaanxi University of Chinese Medicine in China. The study screened all patients diagnosed with spastic CP for eligibility to receive AT treatment. The patients were divided into AT group or control group depending on their guardian’s decision. Both groups received a 12-week treatment period according to the protocol. The study adheres to the principles of the Declaration of Helsinki and good clinical practice guidelines and has obtained approval from the Research Ethics Committee (2021–18) of Xi’an Encephalopathy Hospital Affiliated to Shaanxi University of Chinese Medicine. Prior to participation in the trial, all participants provided written informed consent.
Diagnostic Criteria
The diagnostic criteria for CP and the clinical classification criteria for spastic CP have been established according to the committee members’ determinations in the Guidelines for Rehabilitation and Treatment of Cerebral Palsy in China.24 The necessary conditions for diagnosing CP include the presence of persistent central dyskinesia, abnormal motor and posture development, abnormal reflex development, as well as abnormal muscle tension and muscle strength. The reference conditions for CP diagnosis, although not essential, may include etiological basis of CP and cranial imaging evidence, such as MRI, CT, and B-ultrasound. Spastic lesions are primarily located in the corticospinal tract and can affect different parts of the body, with an increase in muscle tension primarily observed in flexor muscles. This increased muscle tension is characterized by an excessive increase in speed-dependent stretch response.
Inclusion Criteria
- Patients are diagnosed with spastic CP.
- The age of the children is between 4 and 14 years old.
- The patient’s guardian signs the informed consent form.
Exclusion Criteria
- Patients who do not meet the above diagnostic criteria.
- Patients with other serious organic diseases of heart, liver, kidney, and other important organs.
- Leukodystrophy, infantile spinal muscular atrophy, spinocerebellar ataxia syndrome, and hereditary metabolic diseases such as phenylketonuria, congenital cretinism, and congenital hydrocephalus.
- Patients who interrupt treatment in the medium term for non-curative effect reasons.
- Patients who do not cooperate with the treatment observer.
Rejection Criteria
Cases not treated according to the study protocol after inclusion.
Shedding Standard
- Patients with poor compliance (inability to come to treatment as required, children not cooperating, etc.).
- Patients who experience serious adverse events during treatment.
- Patients who withdraw from treatment on their own.
Intervention
The Control Group
Rehabilitation methods, including Bobath, occupational therapy (OT), and physical therapy (PT), are implemented in a selective manner. Experienced rehabilitation therapists create personalized rehabilitation plans for each patient based on their age, physical quality, and motor function. Rehabilitation sessions are conducted once a day, five times a week, for a duration of three consecutive months.
The AT Group
Patients are treated with AT combined with rehabilitation therapy, the same as control group.
Acupuncture treatment:
Main points of scalp acupuncture: motor area, foot movement sensation area, and balance area.
Main points of body acupuncture: Ganshu (BL18), Pishu (BL20), Taichong (LR3), Taibai (SP3), Yanglingquan (GB34), and Sanyinjiao (SP6).
Acupuncture methods: For scalp acupuncture, strong stimulation is used, catharsis is used at Taichong (LR3), and even reinforcing-reducing methods are used at other points.
Tuina treatment:
Tuina includes tuina along meridians, acupoint pressure, abnormal local muscle tuina, and abnormal posture correction. The principle of tuina is light and orderly, and the principle of manipulation is flexible and rigid.
Tuina along meridians: Upper limbs along the hand three yin meridians, hand three yang meridians sequence, lower limbs along the foot three yang meridians, foot three yin meridians sequence, using push method, roll method, and other composite techniques.
Acupoint pressure: Compound techniques such as point, kneading, and pressing were applied to the main acupoints of each meridian (referring to acupuncture).
Abnormal local muscle tuina: Soothing techniques such as kneading and holding.
Posture correction: The pulling method, shaking method, and stretching method are used for the abnormal postures of the spine and limbs.
Operation in accordance with upper limbs and lower limbs, each limb has four operations in order. Once a day, 20–30 min each time.
Acupuncture needles with a diameter of 0.35mm and a length of 25mm shall be selected. The needles shall be retained for 30 min, and hand-manipulating of needle shall be once every 15 min. Tuina mostly adopts relaxation manipulation. The practitioner will be a registered practitioner with at least 3 years of practical experience in AT.
The two groups of treatments are conducted every day with an interval of 2 days every week during weekend. One course of treatment duration is 12 weeks.
Standardization of Acupuncture Operations
Before all studies begin, acupuncturists are required to attend training according to the study protocol to ensure that acupuncture points are selected, and needle techniques performed are standardized.
Outcome Measures
We assessed the primary and secondary outcomes and conducted statistical analyses on the values of outcomes in two groups before and after treatment. The primary outcomes include modified Ashworth muscle tension scale (MAS), the Gross motor function test (GMFM-D and GMFM-E), which reflect the improvement of the patient’s gross movement. The secondary outcome includes the 6-min walking distance measurement (6MWD) and Modified children’s functional independence Rating Scale (WeeFIM), which can reflect the recovery of the patient’s walking ability and living adaptability.
Primary Outcomes
Modified Ashworth Muscle Tension Scale (MAS)
MAS is the most clinically used spasticity scale.25 It classifies muscle tone into levels 0, 1, 1+, 2, 3, and 4. In this study, 0, 1, 2, 3, 4, and 5 points are given, respectively, translating the spasticity assessment from qualitative to quantitative.
The Gross Motor Function Test (GMFM-88)
The GMFM 88 test consists of 5 functional areas: A (lying and rolling), B (sitting), C (crawling and kneeling), D (standing), E (walking and running and jumping). 51, 60, 42, 39, and 72 points are scored, respectively. In this study, only D and E are applications, which are converted according to the full score of 100 points. The higher the score, the better the motor ability.26
Secondary Outcomes
The 6-Minute Walking Distance Measurement (6MWD)
6MWD is the most widely used method to measure walking distance and walking endurance in children.27 The measurement is performed on a flat treadmill for a preset period of 6 min and the distance walked in 6 min is measured.
Children’s Functional Independence Rating Scale (WeeFIM)
WeeFIM is designed for children and adolescents aged 6 months to 18 years with functional disabilities and developmental delays.28 The assessment includes 18 specific items of motor function (self-care, sphincter control, transfer, walking) and cognitive function (communication, social cognition), each scored on a scale of 1 to 7, ranging from full dependence to full independence, and provides a good reflection of daily living and social adjustment skills with high reliability and validity.
All the above observations were measured once before the start of treatment and once after the end of treatment by a senior rehabilitation therapist who was unaware of the treatment group.
Sample Size Calculation
The sample size for this study was calculated by G-Power (V.3.192). The software has the capability to accommodate a wide range of clinical research designs. Additionally, its parameter configuration can prevent potential complexity that may arise from the two primary outcomes in this study. The specific parameter settings are as follows: Power 95% with a significance level of α = 0.05. Effect size = 0.3, 67 participants wouldbe required for each group. Considering the expected shedding rate of 20%, the sample size for each cohort should not be less than 85.
Statistical Analysis
IBM® SPSS® Statistics version 22 (Statistical Product and Service Solutions Statistics, IBM, Inc., Armonk, NY, USA) was used for data analysis. Firstly, the Shapiro–Wilk test was used to check for normal distribution and the t-test to assess group homogeneity. In addition, t-tests for paired samples were used to measure differences between baseline and post-treatment scores, and t-tests for independent samples to test for differences between groups. Spearman correlation analysis is used to analyze the correlation between factors and efficacy.
Blinding
In this study, AT practitioners and participants were not blinded to group assignment due to the unique nature of TCM and the difficulty of blinding participants and practitioners. It would be optimal to have those collecting the study results blinded; however, this is not possible in the current protocol. Instead, for the evaluation and data analysis of the primary and secondary study outcomes, the group members will be blinded.
Adherence
Health education is provided to guardians of children with cerebral palsy through a WeChat group, and monthly meetings are held with them through a combined online and offline model to share their experiences of their child’s development. These strategies are expected to help improve adherence.
Results
Demographics
In this study, 231 patients diagnosed with spastic CP were screened during the study period from Oct 2021 to Sep 2022 (Figure 1). Among 230 patients, 19 did not meet the inclusion criteria, while 212 patients were eligible. Among the 212 eligible patients, 42 refused to participate in the study. 170 were assigned to AT groups and control groups, according to the decision of the guardian. Among the 85 selected participants in AT group, 2 dropped out. Results of 168 participants were included in the statistical analysis.
 |
Figure 1 CONSORT flow chart. |
The basic characteristics of the eligible participants are listed in Table 1. In all basic characteristic data, there was no difference between the two groups, including age, gender, classification of spastic CP, birth history, and Gross Motor Function Classification System (GMFCS) of the children.
 |
Table 1 Characteristics of Patients in Various Group |
Primary Outcome
Effects of at Treatment on MAS and GMFM
MAS and GMFM measurements were performed before treatment and after treatment in two groups. As shown in Table 2 and Figure 2A–C). There was no significant difference between the two groups in the baseline of the MAS (AT group: 2.71 ± 0.65 vs Control group: 2.88 ± 0.71; p = 0.107), GMFM-D (AT group: 62.78 ± 11.53 vs Control group: 63.45 ± 9.97; p = 0.690), and GMFM-E (AT group: 42.31 ± 9.75 vs Control group: 42.51 ± 10.22; p = 0.901). The intra-group comparison of two groups revealed that the average score of MAS, GMFM-D, and GMFM-E significantly changed after the treatment (p < 0.01) compared with the baseline. After treatment the between-group comparison showed that the score of MAS of AT group was significantly lower compared to the control group (AT group: 1.36 ± 0.48 vs Control group: 1.92 ± 0.58; p < 0.01). The score of GMFM-D and GMFM-E of AT group was significantly higher compared to the control group (AT group: 78.96 ± 7.73 and 55.61 ± 9.68 vs Control group: 72.28± 7.71 and 48.38 ± 8.87; p < 0.01).
 |
Table 2 Changes in Efficacy Measures of AT and Control Groups |
Secondary Outcomes
Effects of at Treatment on 6MWD and WeeFIM
According to Table 2 and Figure 2D and E, there was no significant difference between the two groups in the baseline of the 6MWD (AT group: 142.48 ± 5.13 vs Control group: 142.66 ± 5.42; p = 0.828), WeeFIM (AT group: 70.53± 13.19 vs Control group: 68.82 ± 11.57; p = 0.374). The intra-group comparison of two groups revealed that the average score of 6MWD and WeeFIM significantly changed after the treatment (p<0.01) compared with the baseline. After treatment, the between-group comparison showed that the score of 6MWD and WeeFIM of AT group was significantly higher compared to the control group (AT group: 182.65 ± 6.53 and 97.42 ± 10.22 vs Control group: 167.32 ± 10.28 and 82.24 ± 11.68; p < 0.01).
Correlation Between Basic Characteristic and Efficacy Improvement Rate
The 6MWD can reflect the overall recovery of the child, we use score of 6MWD after treatment minus score of 6MWD before treatment)/score of 6MWD before treatment to represent the efficacy improvement rate. After Spearman correlation analysis, it was found that children’s age was negatively correlated to the efficacy. Other information is not relevant to the efficacy, as shown in Table 3 and Figure 3.
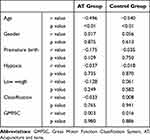 |
Table 3 Correlation Between Basic Information and Efficacy Improvement Rate |
Adverse Events
In this study, no patients experienced adverse reactions such as serious adverse events or other adverse events.
Discussion
This is an initial, single-center, non-randomized clinical study to evaluate the effect of standardized AT on gross motor in children with spastic CP.
Spastic CP refers to a group of syndromes characterized by abnormal central nervous system development leading to increased muscle tone and hyperactive tendon reflexes in the limbs.29 Clinically, spastic CP is classified based on predominant motor syndrome, which includes spastic hemiplegia, spastic diplegia, and spastic quadriplegia.30 This condition results in reduced muscle strength, limited joint movement, and impaired motor function. Furthermore, it also inhibits the coordination of synergistic and antagonistic muscles during movement, thus affecting balance control and causing gross motor dysfunction.31,32 Therefore, the management of spastic CP aims to reduce muscle tone in the affected muscle groups, improve joint range of motion, and enhance walking ability in affected children. According to the International Classification of Functioning, Disability, and Health for Children and Youth (ICF-CY), the therapeutic objectives for cerebral palsy management have evolved from treating injury and disability to promoting health, mobility, and participation in daily life.33,34 In this study, we aim to restore gross motor function related to spastic CP using simple, cost-effective, and standardized TCM (AT) methods.
Several studies have demonstrated that acupuncture is an effective method to reduce muscle tone in spastic muscle groups, improve joint mobility, and enhance gross motor function and walking ability in children with CP.23,35 In a study by Dian E. Putri, acupuncture group exhibited a significant reduction in the Modified Ashworth Scale score compared to the control group (p = 0.003)36. Similarly, YH Ji investigated the therapeutic impact of acupuncture combined with repetitive transcranial magnetic stimulation for the management of spastic CP in children with spleen-kidney deficiency and observed an improvement in cerebral hemodynamics and motor function.37 In contrast to prior studies on acupuncture for CP, this study employs standardized acupuncture treatment, which eliminates the need for varied treatments based on the child’s condition. This standardized approach provides a promising avenue for applying acupuncture to enhance gross motor function and walking ability in children with CP living in LMICs. Scalp acupuncture targets the motor area, foot movement sensation area, and balance area, which can alleviate neurological dysfunction and improve motor function and daily living ability in stroke patients, as evidenced by functional magnetic resonance imaging studies.38,39 The key acupuncture points employed in this study are Ganshu (BL18), Pishu (BL20), Taichong (LR3), Taibai (SP3), Yanglingquan (GB34), and Sanyinjiao (SP6). These points have been shown to regulate muscle contracture, muscle weakness, posture abnormalities, etc.,40 and stimulate brain electrical activity. Additionally, they increase the secretion of neurotransmitters and improve blood circulation in brain tissue, thereby improving clinical efficacy. Moreover, the therapeutic effects of these acupoints correspond to the TCM concept of spastic CP mostly belonging to the syndrome of liver exuberance and spleen deficiency.41
Recovery of motor function is a multifaceted process that involves several factors such as muscle tone, strength, endurance, sensation, and coordination.42 As a kind of peripheral intervention, tuina is a passive mechanical therapy that is a cost-effective adjunct therapy. A study by J Chen revealed that tuina effectively improves motor function and reduces spasticity in stroke survivors.17 In addition, tuina has demonstrated efficacy in improving gross motor function in children, especially in the sitting position.43 A retrospective study demonstrated that Rougan Tongdu Tuina combined with point-pressing tuina therapy during the neonatal period could significantly improve the neurodevelopment of children.44 In our study, the acupoints of tuina are similar to those of acupuncture, but we utilize tuina therapy along the meridians. In addition to relieving spasticity, meridian stimulation can also expand blood vessels, promote circulation, activate cells, and restore damaged functions.45,46
This study utilized MAS, GMFM88, 6MWD, and WeeFIM as evaluation indicators to assess the effectiveness of AT therapy in improving gross motor function in children with spastic CP. Following 12 weeks of treatment, both AT and control groups exhibited decreased MAS scores, improved GMFM scores, 6MWD, and WeefIM scores. Reduction in dystonia, improved walking ability, and increased functional independence were observed in both groups, suggesting that both AT treatment and rehabilitation training can effectively improve gross motor function in children with spastic CP, which is consistent with previous studies. Systematic reviews have also indicated that acupuncture is a promising and safe therapy for CP.47,48 Additionally, integrative medicine rehabilitation (IMR) has been shown to be effective and safe for treating motor dysfunction, language disorder, and social-emotional disorders in children with CP.49 However, it is important to note that AT group, which received a combination of AT therapy based on rehabilitation, demonstrated better improvement in all indicators than the control group, which only underwent rehabilitation training. These findings confirm the specific efficacy of AT therapy. The mechanism of this therapy is based on the theory of medicine theory, which suggests that AT can promote the activation of the motor cortex and repair damage, effectively relieving muscle spasm in the limbs and improving the function of the gross motor nerve.17 This theory has been supported by multi-modality MRI combined with dynamic electroencephalogram analysis.50 Another study51 showed acupuncture can improve expression of nerve growth-related proteins, enhancement of ATPase activity, and regulation of the brain microenvironment. Stimulation through AT can more effectively promote the activation of deep spinal stabilizing muscles,52 increase muscle strength, and improve movement control so that children can obtain more muscle strength and exercise opportunities for limb movement control required for effective movement, thus improving the movement function of the trunk and lower limbs of the children to a greater extent, improving their gross motor function, further improving the static and dynamic balance ability of sitting and standing, and improving their walking ability. Meanwhile, our results indicate that younger children had a better response to both AT and rehabilitation treatment, suggesting that they have a greater potential for neuroplasticity and functional recovery and children with cerebral palsy should be treated as soon as possible.
However, it is important to note that our study has some limitations. First, the sample size was relatively small, which may limit the generalizability of our findings. Second, our study found a relationship between age and treatment efficacy. The reason that other factors involved have no relationship may be the sample size too. To recruit more children with cerebral palsy to participate in this study, we decided not to limit our selection to randomized controlled trials.53 Despite the limitations inherent in our study, we believe that the use of standardized AT techniques for the treatment of spastic CP has shown significant efficacy and substantial potential for widespread applicability, particularly in LMICs. We acknowledge that there is room for improvement in certain aspects of our study due to our limited personal resources. Nonetheless, our findings suggest that there is potential for future research to explore the effectiveness and mechanisms of AT techniques in improving motor function and overall quality of life for children with spastic CP and highlight the importance of considering individual differences in age when evaluating the efficacy of treatments for children. By doing so, health-care providers may be better able to tailor treatments to individual needs and maximize their efficacy. Future studies with larger sample sizes and more comprehensive data collection may further refine our understanding of these relationships and provide insights for clinical practice.
Data Sharing Statement
The datasets used or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval
The study has obtained approval from the Research Ethics Committee (2021-18) of Xi’an Encephalopathy Hospital Affiliated to Shaanxi University of Chinese Medicine.
Acknowledgments
The authors are grateful to all participants and clinicians who participated in this study.
Funding
The construction project of the National Famous Senior TCM Experts Heritage Studio of Hujie Song.
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Sadowska M, Sarecka-Hujar B, Kopyta IJ. treatment. Cerebral palsy: current opinions on definition, epidemiology, risk factors, classification and treatment options. Neuropsychiatr Dis Treat. 2020;16:1505–1518. doi:10.2147/NDT.S235165
2. Vitrikas K, Dalton H, Breish DJ. Cerebral palsy: an overview. Am Fam Physician. 2020;101(4):213–220.
3. Arneson CL, Durkin MS, Benedict RE, et al. Prevalence of cerebral palsy: autism and developmental disabilities monitoring network, three sites, United States, 2004. Disabil Health J. 2009;2(1):45–48. doi:10.1016/j.dhjo.2008.08.001
4. Bhasin TK, Brocksen S, Avchen RN, Van Naarden Braun K. Prevalence of four developmental disabilities among children aged 8 years; metropolitan Atlanta developmental disabilities surveillance program, 1996 and 2000; 2006.
5. Paneth N, Hong T, Korzeniewski S. The descriptive epidemiology of cerebral palsy. Clin Perinatol. 2006;33(2):251–267. doi:10.1016/j.clp.2006.03.011
6. Johnson A. Prevalence and characteristics of children with cerebral palsy in Europe. Dev Med Child Neurol. 2002;44(9):633–640. doi:10.1017/S0012162201002675
7. Chauhan A, Singh M, Jaiswal N, Agarwal A, Sahu JK, Singh P. Prevalence of cerebral palsy in Indian children: a systematic review and meta-analysis. Indian J Pediatr. 2019;86(12):1124–1130. doi:10.1007/s12098-019-03024-0
8. Jahan I, Muhit M, Hardianto D, et al. Epidemiology of cerebral palsy in low‐and middle‐income countries: preliminary findings from an international multi‐centre cerebral palsy register. Dev Med Child Neurol. 2021;63(11):1327–1336. doi:10.1111/dmcn.14926
9. Jahan I, Al Imam MH, Muhit M, et al. Epidemiology of cerebral palsy among children in the remote Gorkha district of Nepal: findings from the Nepal cerebral palsy register. Disabil Rehabil. 2022;45:1–10.
10. Patel DR, Neelakantan M, Pandher K, Merrick JJ. Cerebral palsy in children: a clinical overview. Transl Pediatr. 2020;9(Suppl 1):S125. doi:10.21037/tp.2020.01.01
11. Størvold GV, Jahnsen RB, Evensen KAI, Bratberg GH. Is more frequent physical therapy associated with increased gross motor improvement in children with cerebral palsy? A national prospective cohort study. Disabil Rehabil. 2020;42(10):1430–1438. doi:10.1080/09638288.2018.1528635
12. Ko EJ, Sung IY, Moon HJ, et al. Effect of group-task-oriented training on gross and fine motor function, and activities of daily living in children with spastic cerebral palsy. Phys Occup Ther Pediatr. 2020;40(1):18–30. doi:10.1080/01942638.2019.1642287
13. Yan S, Hai C, Chengyan TCM. Effect of the medication injection site on treatment efficacy in pediatric cerebral palsy: conventional sites vs acupoints. J Tradit Chin Med. 2019;39(05):716.
14. Edwards TA, Prescott RJ, Stebbins J, Wright J, Theologis TJ. What is the functional mobility and quality of life in patients with cerebral palsy following single-event multilevel surgery? J Child Orthop. 2020;14(2):139–144. doi:10.1302/1863-2548.14.190148
15. Menor-Rodríguez MJ, Sevilla Martín M, Sánchez-García JC, Montiel-Troya M, Cortés-Martín J, Rodríguez-Blanque RJJo CM. Role and effects of hippotherapy in the treatment of children with cerebral palsy: a systematic review of the literature. J Clin Med. 2021;10(12):2589. doi:10.3390/jcm10122589
16. Mak CK, Whittingham K, Boyd CP. Experiences of children and parents in MiYoga, an embodied mindfulness yoga program for cerebral palsy: a mixed method study. Complement Ther Clin Pract. 2019;34:208–216. doi:10.1016/j.ctcp.2018.12.006
17. Chen Z, Huang Z, Li X, et al. Effects of traditional Chinese medicine combined with modern rehabilitation therapies on motor function in children with cerebral palsy: a systematic review and meta-analysis. Front Neurosci. 2023;17:1097477.
18. Gao J, He L, Yu X, et al. Rehabilitation with a combination of scalp acupuncture and exercise therapy in spastic cerebral palsy. Complement Ther Clin Pract. 2019;35:296–300. doi:10.1016/j.ctcp.2019.03.002
19. Fan Y, Gong L, Yan J, et al. Clinical observation on treatment of knee osteoarthritis by acupuncture and tuina therapy. J Acupunct Tuina Sci. 2010;8:390–393.
20. Huang Y, Miao Z, Lai C, et al. Acupuncture combined tuina for oculomotor paralysis: a protocol for systematic review and meta-analysis. Medicine. 2022;101:2.
21. Yang W, Guo X, Lu Q, Pan T, Wang H, Wang HJM. Acupuncture plus Tuina for chronic insomnia: a protocol of a systematic review and meta-analysis. Medicine. 2021;100:47.
22. Li N, Jin B-X, Zhao Y, et al. Clinical observation on muscle regions of meridians needling method in improving upper limb function for children with cerebral palsy of spastic hemiplegia type. J Acupunct Tuina Sci. 2020;2020:295–301.
23. Xu Y, Shao Z, Yu Y, et al. Therapeutic efficacy of acupuncture plus Tuina for spastic cerebral palsy and discussion of its mechanism. Pediatr Rheumatol Online J. 2022;20(2):111–118. doi:10.1186/s12969-022-00767-7
24. Li X. Revision of guidelines, definitions, classification and diagnostic criteria for cerebral palsy.
25. Harb A, Kishner S. Modified Ashworth scale. In: StatPearls. StatPearls Publishing; 2021.
26. Te Velde A, Morgan C. Gross Motor Function Measure (GMFM-66 & GMFM-88) User’s Manual, Book Review. LWW; 2022.
27. Fitzgerald D, Hickey C, Delahunt E, Walsh M, O’Brien TJ. Six-minute walk test in children with spastic cerebral palsy and children developing typically. Pediatr Phys Ther. 2016;28(2):192–199. doi:10.1097/PEP.0000000000000224
28. Jang J-S, Jeon J-Y, Kim H, Jang J-S. Validity and reliability of functional Independence measure for children (WeeFIM) for children with cerebral palsy. Inquir. 2022;59:00469580211072454. doi:10.1177/00469580211072454
29. Burgess A, Reedman S, Chatfield MD, et al. Development of gross motor capacity and mobility performance in children with cerebral palsy: a longitudinal study. Dev Med Child Neurol. 2022;64(5):578–585. doi:10.1111/dmcn.15112
30. Te Velde A, Morgan C, Novak I, Tantsis E, Badawi CM. Early diagnosis and classification of cerebral palsy: an historical perspective and barriers to an early diagnosis. J Clin Med. 2019;8(10):1599. doi:10.3390/jcm8101599
31. Więch P, Ćwirlej-Sozańska A, Wiśniowska-Szurlej A, et al. The relationship between body composition and muscle tone in children with cerebral palsy: a case-control study. Nutrients. 2020;12(3):864. doi:10.3390/nu12030864
32. Nashner L, Shumway-Cook A, Marin OJ. Stance posture control in select groups of children with cerebral palsy: deficits in sensory organization and muscular coordination. Exp Brain Res. 1983;49(3):393–409. doi:10.1007/BF00238781
33. Illum NO, Bonderup M, Gradel KO. Environmental needs in childhood disability analysed by the WHO ICF, child and youth version. Dan Med J. 2016;63(6):A5238.
34. Mukhtiar K, Ibrahim S, Ahmed PN. Application of ICF-CY core sets in children with spastic cerebral palsy. J Pediatr Neurol. 2020;18(01):017–021.
35. L-X L, Zhang -M-M, Zhang Y, J H. Acupuncture for cerebral palsy: a meta-analysis of randomized controlled trials. Neural Regen Res. 2018;13(6):1107. doi:10.4103/1673-5374.233455
36. Putri DE, Srilestari A, Abdurrohim K, Mangunatmadja I, Wahyuni LK. Wahyuni LKJJoa, studies m. The effect of laser acupuncture on spasticity in children with spastic cerebral palsy. J Acupunct Meridian Stud. 2020;13(5):152–156. doi:10.1016/j.jams.2020.09.001
37. Y-H J, Sun BJZcyj AR, Sun B-D. Effect of acupuncture combined with repetitive transcranial magnetic stimulation on motor function and cerebral hemodynamics in children with spastic cerebral palsy with spleen-kidney deficiency. Zhen Ci Yan Jiu. 2019;44(10):757–761. doi:10.13702/j.1000-0607.190154
38. Zanardi R, Maieron M, Tomasino B. Modulation of hand motor-related area during motor imagery and motor execution before and after middle 2/5 of the MS6 line scalp acupuncture stimulation: an fMRI study. Brain Cogn. 2016;103:1–11. doi:10.1016/j.bandc.2016.01.002
39. Cui F, Zou Y, Tan Z, Dong P, Wu YF. Rehabilitation of motor function and curative effect of scalp acupuncture in patients with hemiplegia after stroke: studies on fMRI and DTI. J Beijing Univ Trad Chinese Med. 2013;20(4):34–38.
40. Mou Z-J, L-Y H, Song H-J, Cheng Q, Liu B-Y. Rule of point selection in treatment of cerebral palsy in children with acupuncture based on data mining of 1584 electronic medical records. Chin Acupunct Moxibust. 2021;41(3):355–358. doi:10.13703/j.0255-2930.20200410-k0006
41. Ma B, Lei S, Zhang J, Li H, Zheng H. Analysis of investigation results of TCM syndrome differentiation of cerebral palsy. J Tradit Chin Med. 2013;28(12):3545–3547.
42. Francisco GE, McGuire JR. Poststroke spasticity management. Stroke. 2012;43(11):3132–3136. doi:10.1161/STROKEAHA.111.639831
43. Z-h L, L C, Science T. Effect of tuina on neurodevelopment in premature infants with brain injury. J Acupunct Tuina Sci. 2013;11:7–12.
44. Geng L, Yang Y. Retrospective study of Rougan Tongdu Tuina combined with point-pressing massage therapy on neurodevelopment in children with delayed motor development at very early stage. Transl Pediatr. 2021;10(12):3202. doi:10.21037/tp-21-558
45. Jia Y, Qiu Z, Sun X, Shen Y, Zhou Q, Li SJM. Acupotomy for patients with trigger finger: a systematic review protocol. Medicine. 2019;98(42).
46. Chen K, Shu S, Yang M, Zhong S, Xu TR. Meridian acupuncture plus massage for children with spastic cerebral palsy. Am J Transl Res. 2021;13(6):6415.
47. Hu J, Wang X, Liu X, et al. Effectiveness and Safety of Acupuncture for children with cerebral palsy: an overview of systematic reviews. Eur J Integr Med. 2022;2022:102199.
48. Tang Y, Cao Z, Xia Y, Liu Y, Zhang WJM. Effectiveness and safety of pure acupuncture and moxibustion in the treatment of children with cerebral palsy: a protocol for systematic review and meta analysis. Medicine. 2021;100:4.
49. Lee M-J, Yun Y-J, S-a Y, Shin Y-B, Kim S-Y, J H. Integrative medicine rehabilitation for children with cerebral palsy: a study protocol for a multicenter pragmatic randomized controlled trial. Trials. 2020;21(1):1–10.
50. Chen D, Bao C, Geng Y-X, et al. Effect of “Tonifying Kidney and Invigorating Brain” acupuncture in children with spastic cerebral palsy analyzed by multi-modality MRI combined with dynamic electroencephalogram. Medicine. 2020;99:30.
51. Zixuan W, Xiangwei F, Kaiyun C, Xuefeng Y, Jing TCM. Effects of three kinds of head acupuncture therapies on regulation of brain microenvironment and rehabilitation of nerve function in rats with cerebral palsy. J Tradit Chin Med. 2021;41(2):276.
52. Wright BD. Acupuncture for the treatment of neuromuscular conditions in dogs and cats, with emphasis on intervertebral disc disease. J Am Holist Vet Med Assoc. 2021;63:23–33.
53. Wang X, Kattan M. Cohort studies: design, analysis, and reporting. Chest. 2020;158(1):S72–S78. doi:10.1016/j.chest.2020.03.014
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


