Back to Journals » Journal of Multidisciplinary Healthcare » Volume 15
Acupoint Stimulation for Enhanced Recovery After Colon Surgery: A Prospective Multicenter Randomized Controlled Trial
Authors Lu Z, Luo A, Min S, Dong H, Xiong Q, Li X, Deng Q, Liu T, Yang X, Li C, Zhao Q, Xiong L
Received 11 October 2022
Accepted for publication 8 December 2022
Published 19 December 2022 Volume 2022:15 Pages 2871—2879
DOI https://doi.org/10.2147/JMDH.S391852
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Zhihong Lu,1,* Ailin Luo,2,* Su Min,3,* Hailong Dong,1 Qiuju Xiong,3 Xinhua Li,2 Qingzhu Deng,2 Tingting Liu,1 Xue Yang,1 Chen Li,4 Qingchuan Zhao,5 Lize Xiong1,6
1Department of Anaesthesiology and Perioperative Medicine, Xijing Hospital, Fourth Military Medical University, Xi’an, People’s Republic of China; 2Department of Anaesthesiology, Tongji Hospital, Huazhong University of Science and Technology, Wuhan, People’s Republic of China; 3Department of Anaesthesiology, First Affiliated Hospital of Chongqing Medical University, Chongqing, People’s Republic of China; 4Department of Medical Statistics, Fourth Military Medical University, Xi’an, People’s Republic of China; 5Xijing Hospital of Digestive Diseases, Fourth Military Medical University, Xi’an, People’s Republic of China; 6Translational Research Institute of Brain and Brain-Like Intelligence and Department of Anesthesiology, Shanghai Fourth People’s Hospital Affiliated to Tongji University School of Medicine, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhihong Lu; Lize Xiong, Department of Anesthesiology and Perioperative Medicine, Xijing Hospital, Fourth Military Medical University, Changle West Road127, Xi’an, Shaanxi, 710032, People’s Republic of China, Tel +86-29-84775337 ; Tel +86-29-84772126, Email [email protected]; [email protected]
Purpose: The aim of this study was to evaluate the efficacy of transcutaneous electrical acupoint stimulation (TEAS) in improving bowel function and thus shortening hospital stay after laparoscopic colon surgery within the ERAS pathway.
Patients and Methods: From November 2016 to March 2018, 100 patients who underwent elective colon surgery were enrolled and 94 finished study (n = 47 for each) in three university hospitals. Patients in the TEAS group received TEAS 30 min before surgery and once a day for 3 days after surgery, while those in the Control Group received no stimulation. Primary outcome was the time to discharge.
Results: Compared with standardized postoperative care, TEAS resulted in a shorter time to first flatus (P=0.03) and time to first defecation (P=0.03), as well as a reduction in the length of hospital stay (P=0.02). Median patient-controlled analgesia (PCA) deliveries and PCA attempts at 24h, 48h and 72h after surgery were less in the TEAS group (P< 0.01). No evidence of significant advantages in postoperative pain intensity, nausea, vomiting, sleeping quality and expenses was found in the TEAS group.
Conclusion: Perioperative TEAS further shortens the time to meet discharge criteria after laparoscopic colon surgery in patients under ERAS strategy.
Keywords: transcutaneous electrical acupoint stimulation, colon surgery, laparoscopy, ERAS
Plain Language Summary
Recovery of bowel function is important for patients undergoing colorectal surgery. Enhanced recovery after surgery (ERAS) program makes great efforts on improving bowel function. In patients under ERAS program, transcutaneous electrical acupoint stimulation (TEAS) can further shorten the time to first flatus and to first defecation after colon surgery. The length of hospital stay and need of analgesics after surgery were decreased as well.
Introduction
Accumulating evidence supported that the enhanced recovery after surgery (ERAS) pathway and laparoscopic approach benefit patients undergoing colorectal resections by shortening the length of hospital stay and reducing morbidity after surgery.1–5 For patients undergoing colon surgery, the return of bowel function is especially important for ERAS.6 Shortening fasting time, early mobilization and early oral intake have been used to facilitate the recovery of bowel function.6 However, postoperative ileus still represents problems in the management.7 The time to first bowel motion was not satisfied in the laparoscopic arm in many of these trials, which is only about 1 day earlier than that in the open arm.7–9
Acupuncture-related techniques have been used to treat bowel function disorders, including irritable bowel syndrome and chronic functional constipation10–12 Perioperative acupuncture-related techniques including transcutaneous electrical acupoint stimulation (TEAS) have shown benefits including narcotic-sparing effects and fewer complications.13 Besides, acupuncture has been used to treat gastrointestinal motility disorder.14–19 Evidence of acupuncture for postoperative gastrointestinal function is accumulating. In patients undergoing major abdominal surgery, Li et al19 observed shorter time to flatus and to ambulation after TEAS. In patients undergoing laparoscopic surgery, the time to defecation was shortened as well.20 However, whether the potential benefit of TEAS on gastrointestinal function could shorten the length of stay after surgery is not clear. Therefore, the aim of this multicenter randomized trial was to evaluate whether perioperative TEAS could further improve the gastrointestinal function and shorten the time to meet the discharge criteria in patients undergoing laparoscopic colon surgery with current ERAS approaches.
Materials and Methods
Patients and Randomization
The randomized, prospective, sham controlled study was undertaken in 3 university hospitals in China (Xijing Hospital, Tongji Hospital, and First Affiliated Hospital of Chongqing Medical University). The study was approved by the Institutional Ethics Committee of each participating hospital and has been registered in ClinicalTrials.gov (NCT02921529). Written informed consent was obtained from all patients. Patients scheduled for laparoscopic colon surgery under general anaesthesia were screened. Inclusion criteria included age between 18 and 75 years, a body mass index between 18 and 30, and ASA status of I–III. Patients with contraindications for electrical stimulation, difficulty in communicating, confirmed or suspected drug abuse/addiction or alcohol abuse/addiction, or severe hepatic or renal dysfunction were excluded. Patients were randomly assigned to the TEAS or Control group in a ratio of 1:1 using a computer-generated random allocation sequence. The randomization code for each patient was put in sealed envelope and not opened until allocation.
Intervention and Blinding
For all patients, electrodes were placed at the bilateral PC6/LI4 and ST36/SP6 and connected to the stimulator (Model No. SDZ-II; Hwato electronic stimulator; Suzhou Medical Appliances Co., Ltd, Suzhou, China) (See Supplemental Digital Content 1). Patients in the TEAS group received stimulation at the bilateral PC6 and ST36 points. The device provided “disperse-dense” waves of alternating frequencies of 2 Hz and 10 Hz for 2 cycles. Increasing electrical stimulation intensity (4 mA to 11 mA) was applied to identify the threshold intensity. Stimulation began 30 min before induction and lasted for 30 min. Then the same stimulation for 30 min was given in the morning once a day for 3 days after surgery. Patients in the Control group received no stimulation.
For logistic reasons, blinding the patients was hard to perform. However, the threshold intensity was identified in all the patients, and they were told that they may or may not feel the electrical stimulation. Interventions were performed by a designated investigator who was not involved in the anaesthesia or the follow-up. The stimulator was placed in an opaque box. Investigators involved in the follow-up were blinded to the group allocation.
Procedures
Anaesthesia was induced with midazolam, propofol and fentanyl. Rocuronium was given to facilitate tracheal intubation. Intraoperative anaesthesia was maintained with a remifentanil infusion and sevoflurane. Patients were managed according to ERAS methods previously reported21,22 (see Supplemental Digital Content 2) and followed up until discharge.
The primary outcome was the time to meet discharge criteria after surgery that we previously reported21,22 (Table 1). The secondary outcomes included time to flatus, time to first defecation, and time to first oral intake; pain intensity assessed by visual analogue scale (VAS), attempts and deliveries of patient-controlled analgesia (PCA), postoperative nausea and vomiting (PONV), quality of sleeping (QoS) and quality of recovery (QoR) evaluated at 24h, 48h and 72h after surgery. QoS was assessed using visual sleeping scale and the Richard-Campbell Sleep Questionnaire (RCSQ),23 and QoR was assessed using QoR-15 questionnaire.24 Higher scores indicate better quality (Supplemental Digital Contents 3 and 4). Postoperative major complications (Supplemental Digital Content 5) and expenses were recorded as well.
 |
Table 1 Criteria for Discharge |
Statistical Analysis
We performed all the analyses in a modified intention-to-treat population, which included all the patients who had undergone randomization and all the interventions. All the patients were followed for the duration of the trial.
Based on a previous study, the average time to meet discharge criteria was 5 days for patients undergoing colorectal surgery.21 A minimum of 43 patients in each group would give 90% power to detect a decrease of 1 day for the time to discharge, with a standard deviation of 1.3 days, at an overall 2-sided P < 0.05. The sample size was inflated to 94 patients (n=47 for each) to account for a rate of withdrawals and loss to follow-up by 10%.
Data were analyzed with SAS 9.2 (USA: SAS Institute Inc., 2010). Descriptive statistics were applied to present subjects’ characters. Comparison of qualitative data between two groups was done using Chi-square test and Fisher’s exact test. And comparison of quantitative data was evaluated by t-test. Also, Satterthwaite t’ test was applied if the variances were unequal between two groups. Univariate analysis of survival data was estimated using the Log rank test. A two-tailed P-value of 0.05 was considered as statistically significant with a 95% confidence interval (95% CI).
Results
From November 2016 through March 2018, a total of 100 patients were enrolled at 3 hospitals. We randomly assigned 50 patients to each group (Figure 1). After randomization, 5 patients were excluded due to procedure converting from laparoscopic to open surgery and 1 patient was excluded due to rejection to TEAS (Figure 1). There was no significant difference between the groups with respect to demographic, anesthetic and surgical characteristics (Table 2), pre-existing diseases and pre-operative laboratory test results including nutritional status (Supplemental Digital Contents 6 and 7). Case numbers in each center were shown in Supplemental Digital Content 8.
 |
Table 2 Demographic and Surgical Characteristics of the Patients |
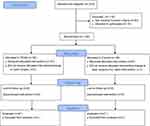 |
Figure 1 Trial profile. |
Primary Outcome
The median follow-up time was 7 days in each group. The median time to discharge was 6.0d±1.8d (95% CI, 5.5–6.5) in the TEAS group compared with 7.0d±2.4d (95% CI, 6.3–7.7, P =0.02) in the Control group (Table 3). Log rank test showed a P value of 0.02 between the two groups (Figure 2). Subgroup analysis based on type of surgery showed same results concerning time to discharge (Supplemental Digital Content 9).
 |
Table 3 Recovery Parameters of the Patients |
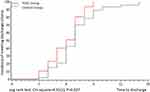 |
Figure 2 Kaplan–Meier estimation of incidence of meeting discharge criteria. |
Secondary Outcomes
The mean time to flatus and mean time defecation were 34.5 h±16.7h (95% CI, 29.6–39.4) and 42.0h±25.0h (95% CI, 34.7–49.3) respectively in the TEAS group, compared with 42.4h±22.9h (95% CI, 35.6–49.1, P =0.03) and 55.4h±29.7h (95% CI, 46.7–64.1, P=0.03) respectively in the Control group (Table 3). Log rank test of the two outcomes showed P values of 0.03 and 0.03 respectively between the two groups (Supplemental Digital Contents 10 and 11).
Incidences of PONV, the VAS at rest and at cough, and score of sleeping quality in 3 days after surgery were not different between the groups (all P >0.05). However, median PCA deliveries and PCA attempts at 24h, 48h and 72h after surgery were less in the TEAS group than in the Control (P<0.01). Median QoR-15 scores22 in the TEAS group were not different to the Control group at 48 h and 72h after surgery, but lower at 24h after surgery 50.5 (IQR 42.3–61.8) vs 44.5 (IQR35.0–57.0), P =0.04. Postoperative morbidity of infection and major complications were not different between the two groups. Mean postoperative expense was 62962±28001CNY in the TEAS group and 84,218±115 027 CNY in the Control group, with no significant difference (P=0.22, Table 3).
Discussion
This multicenter prospective randomized trial suggests that in patients being managed by the current ERAS protocol, perioperative TEAS (30 min before anaesthetic induction, and 30 min once a day for 3 days after surgery) provided additional benefit in enhanced recovery after laparoscopic colon surgery. Patients needed less opioid after surgery, and the time to meet discharge criteria and recovery of bowel function were shortened significantly.
Our study was the first multicenter randomized controlled trial on the role of TEAS for postoperative hospital stay and bowel function in laparoscopic colon surgery. There has been limited randomized controlled trials published in the English literature that examined the role of acupuncture in preventing postoperative ileus after laparoscopic colorectal surgery. In a single-center trial, Ng et al25 observed that electroacupuncture once a day for 4 days postoperatively decreased the time to flatus by 0.6 d and shortened the length of hospital stay from 8.5 to 6d. In our study, with TEAS, a non-invasive technique, we achieved enhanced recovery as well time to flatus decreased by 7.9h and time to discharge decreased by 1d. Additionally, we did TEAS both preoperatively (30min before anaesthesia induction) and postoperatively (once a day for 3 days). Previous studies have found that preoperative acupuncture-related technique potentially provided additional benefits including alleviating anxiety and decreasing anaesthetic consumption.13
The shortening of time to discharge or to flatus varied in different trials. In a trial in open colorectal surgery, Zhang et al26 found that electroacupuncture decreased the time to flatus by 9 hours, close to the 7.9 hours in our study. But Ng’s study and Li’s study found stronger effect of bowel function acceleration.19,25 And the time to first oral intake was not shortened in our study, while in Ng’s study the time to normal diet decreased by 0.8d. A possible explanation is that in our study patient were managed with ERAS protocol which encourages early oral intake and mobilization. The benefits of TEAS maybe overlapped by ERAS strategy. Ng et al acknowledged that one of the limitations of their study was that they did not use a fast-track perioperative program. They also suggested that possible combined effects of EA and the fast-track program on the clinical outcomes after laparoscopic colorectal surgery will be an important area for further research.
In our study, the cost after surgery was not different between the two groups (P=0.22). However, it should be prudent to conclude that TEAS has no cost-effective benefit. In our study, the time to meet discharge criteria was reduced by 1 day in patients receiving TEAS. It is estimated that a reduction of the length of hospital stay by 1 day may reduce the annual health care system costs in the United States by approximately US$1 billion.27 The cost-effective effect of TEAS may be shown in the hospital and overall health care system.
Mechanisms of acupuncture-related techniques improving gut function have been studied in animal and clinical studies. In patients undergoing open colon surgery, Meng et al28 failed to prove any benefit of electroacupuncture on time to first bowel movement when the patients received epidural anaesthesia, which blocked the afferent and efferent pathway. This highlights the role of neural pathway during action of acupuncture. It was also reported that vagal nerve system-induced anti-inflammatory effect may be the underlying mechanism of acupuncture improving gut function. Electroacupuncture may suppress intestinal manipulation-induced inflammation via activation of the cholinergic anti-inflammatory pathway in macrophages.29,30 Besides, in our study, the postoperative analgesics consumption was fewer during the first 3 days after surgery. The use of opioid-based analgesia is usually thought to exacerbate postoperative ileus.31–33 The decreased opioid use in our study may contribute to the better bowel function recovery.
In our study, frequency of stimulation was set at 2Hz/10Hz, which is a low frequency. Both low frequency and high frequency of electrical acupoint stimulation have been used in the prevention and treatment of postoperative ileus. In Li et al19 and Wang et al20 trials, 2/100Hz was used. While Yang et al found that 10 Hz and 30Hz are more effective in increasing the gastrointestinal motility and attenuating peripheral inflammation.34 Besides, our previous studies showed that TEAS at 2/10Hz induces opioid-sparing effect,35 which may decrease opioid-related postoperative ileus. The optimal frequency for improving gut function still needs further investigation.
The present trial has some limitations. First, investigators could not administer TEAS in a patient-blinded manner. The patient may tell the investigator who did the follow-up that he/she felt a stimuli. We tried to minimize the potential bias by applying electrodes at acupoints and testified stimulation threshold for all patients. We told the patients that they may not feel the stimulation during treatment. The stimulators were put in opaque box to blind the medical staff in the OR and in the ward. Second, flatus is sometimes regarded as an insensitive index, and the time to resume oral intake can be influenced by the patient’s perception and the clinician. We therefore adopted time to meet discharge criteria as primary endpoint and time to defecation as one secondary endpoint, because they are more objective and can be recorded by the assessor without bias. Third, though we followed ERAS approaches and encouraged the patients to resume oral intake as early as 6h after surgery, the time to oral intake was longer than 24h in both groups. Adherence to ERAS protocols should be paid attention in future studies.
Conclusion
In conclusion, this multicenter randomized controlled study suggests that TEAS could further enhance short-term recovery and shorten hospital stay after laparoscopic colon surgery in patients being managed by ERAS program. Further studies are warranted to generalize our findings.
Data Sharing Statement
Data related to the specific manuscript will be made available upon reasonable request in adherence with transparency conventions in medical research and through requests to the corresponding author ([email protected]).
Acknowledgments
The authors are grateful to Min Chen and Genlin Ji for supporting the anesthesia for the patients, Jielai Xia for suggesting the methods of statistical analysis and critical reading of the manuscript.
Funding
This work was supported by the National Key Basic Research Program of China (No. 2014CB543200), the National Natural Science Foundation of China (No. 81871028), the National Cultivation and Development Program (2021ZY019) and the Aeromedical Flow Principal Investigator Program of Air Force Medical University (2022HYPI02).
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Ni X, Jia D, Chen Y, Wang L, Suo J. Is the enhanced recovery after surgery (ERAS) program effective and safe in laparoscopic colorectal cancer surgery? A meta-analysis of randomized controlled trials. J Gastrointest Surg. 2019;23(7):1502–1512. doi:10.1007/s11605-019-04170-8
2. Ota H, Ikenaga M, Hasegawa J, et al. Safety and efficacy of an “enhanced recovery after surgery” protocol for patients undergoing colon cancer surgery: a multi-institutional controlled study. Surg Today. 2017;47(6):668–675. doi:10.1007/s00595-016-1423-4
3. García-Erce JA, Camps-Cervantes Á, Ferrando-Ortolá C. Association between use of enhanced recovery after surgery protocol and postoperative complications in colorectal surgery: the postoperative outcomes within enhanced recovery after surgery protocol (POWER) Study. JAMA Surg. 2019;154(8):725–736. doi:10.1001/jamasurg.2019.0995
4. Godellas CV, Vaince FT, Singer MA, Godellas CV, Vaince FT. Enhanced recovery after surgery: a clinical review of implementation across multiple surgical subspecialties. Am J Surg. 2020;219(3):530–534. doi:10.1016/j.amjsurg.2019.11.009
5. Ban KA, Berian JR, Ko CY. Does implementation of enhanced recovery after surgery (ERAS) protocols in colorectal surgery improve patient outcomes? Clin Colon Rectal Surg. 2019;32(2):109–113. doi:10.1055/s-0038-1676475
6. Lassen K, Soop M, Nygren J, et al. Consensus review of optimal perioperative care in colorectal surgery: Enhanced Recovery After Surgery (ERAS) Group recommendations. Arch Surg. 2009;144(10):961–969. doi:10.1001/archsurg.2009.170
7. Thillainadesan J, Yumol MF, Suen M, Hilmer S, Naganathan V. Enhanced recovery after surgery in older adults undergoing colorectal surgery: a systematic review and meta-analysis of randomized controlled trials. Dis Colon Rectum. 2021;64(8):1020–1028. doi:10.1097/DCR.0000000000002128
8. Guillou PJ, Quirke P, Thorpe H, et al. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365(9472):1718–1726. doi:10.1016/S0140-6736(05)66545-2
9. Huang Z, Li T, Zhang G, et al. Comparison of open, laparoscopic, and robotic left colectomy for radical treatment of colon cancer: a retrospective analysis in a consecutive series of 211 patients. World J Surg Oncol. 2022;20(1):345. doi:10.1186/s12957-022-02796-8
10. Wang XY, Wang H, Guan YY, Cai RL, Shen GM. Acupuncture for functional gastrointestinal disorders: a systematic review and meta-analysis. J Gastroenterol Hepatol. 2021;36(11):3015–3026. doi:10.1111/jgh.15645
11. Santucci NR, Chogle A, Leiby A, et al. Non-pharmacologic approach to pediatric constipation. Complement Ther Med. 2021;59:102711. doi:10.1016/j.ctim.2021.102711
12. Lee HY, Kwon OJ, Kim JE, et al. Efficacy and safety of acupuncture for functional constipation: a randomised, sham-controlled pilot trial. BMC Complement Altern Med. 2018;18(1):186. doi:10.1186/s12906-018-2243-4
13. Lu Z, Dong H, Wang Q, Xiong L. Perioperative acupuncture modulation: more than anaesthesia. Br J Anaesth. 2015;115(2):183–193. doi:10.1093/bja/aev227
14. Liu YH, Dong GT, Ye Y, et al. Effectiveness of acupuncture for early recovery of bowel function in cancer: a systematic review and meta-analysis. Evid Based Complement Alternat Med. 2017;2017:2504021. doi:10.1155/2017/2504021
15. Zhu YJ, Wu XY, Wang W, et al. Acupuncture for quality of life in gastric cancer patients undergoing adjuvant chemotherapy. J Pain Symptom Manage. 2022;63(2):210–220. doi:10.1016/j.jpainsymman.2021.09.009
16. Kanza Gül D, Şolt Kırca A. Effects of acupressure, gum chewing and coffee consumption on the gastrointestinal system after caesarean section under spinal anaesthesia. J Obstet Gynaecol. 2021;41(4):573–580. doi:10.1080/01443615.2020.1787363
17. Soylu D, Tekinsoy Kartın P. The effect on gastrointestinal system functions, pain and anxiety of acupressure applied following laparoscopic cholecystectomy operation: a randomised, placebo-controlled study. Complement Ther Clin Pract. 2021;43:101304. doi:10.1016/j.ctcp.2021.101304
18. Zhou X, Cao SG, Tan XJ, et al. Effects of Transcutaneous Electrical Acupoint Stimulation (TEAS) on postoperative recovery in patients with gastric cancer: a randomized controlled trial. Cancer Manag Res. 2021;13:1449–1458. doi:10.2147/CMAR.S292325
19. Li WJ, Gao C, An LX, Ji YW, Xue FS, Du Y. Perioperative transcutaneous electrical acupoint stimulation for improving postoperative gastrointestinal function: a randomized controlled trial. J Integr Med. 2021;19(3):211–218. doi:10.1016/j.joim.2021.01.005
20. Wang Y, Yang JW, Yan SY, et al. Electroacupuncture vs sham electroacupuncture in the treatment of postoperative ileus after laparoscopic surgery for colorectal cancer: a multicenter, randomized clinical trial. JAMA Surg. 2022;2022:1.
21. Feng F, Ji G, Li JP, et al. Fast-track surgery could improve postoperative recovery in radical total gastrectomy patients. World J Gastroenterol. 2013;19(23):3642–3648. doi:10.3748/wjg.v19.i23.3642
22. Feng F, Li XH, Shi H, et al. Fast-track surgery combined with laparoscopy could improve postoperative recovery of low-risk rectal cancer patients: a randomized controlled clinical trial. J Dig Dis. 2014;15(6):306–313. doi:10.1111/1751-2980.12142
23. Menear A, Elliott R, Lal LMA, Lal S, McKinley S. Repeated sleep-quality assessment and use of sleep-promoting interventions in ICU. Nurs Crit Care. 2017;22(6):348–354. doi:10.1111/nicc.12315
24. Stark PA, Myles PS, Burke JA. Development and psychometric evaluation of a postoperative quality of recovery score: the QoR-15. Anesthesiology. 2013;118(6):1332–1340. doi:10.1097/ALN.0b013e318289b84b
25. Ng SS, Leung WW, Mak TW, et al. Electroacupuncture reduces duration of postoperative ileus after laparoscopic surgery for colorectal cancer. Gastroenterology. 2013;144(2):307–313 e1. doi:10.1053/j.gastro.2012.10.050
26. Zhang Z, Wang C, Li Q, et al. Electroacupuncture at ST36 accelerates the recovery of gastrointestinal motility after colorectal surgery: a randomised controlled trial. Acupunct Med. 2014;32(3):223–226. doi:10.1136/acupmed-2013-010490
27. Sommer NP, Schneider R, Wehner S, Kalff JC, Vilz TO. State-of-the-art colorectal disease: postoperative ileus. Int J Colorectal Dis. 2021;36(9):2017–2025. doi:10.1007/s00384-021-03939-1
28. Meng ZQ, Garcia MK, Chiang JS, et al. Electro-acupuncture to prevent prolonged postoperative ileus: a randomized clinical trial. World J Gastroenterol. 2010;16(1):104–111. doi:10.3748/wjg.v16.i1.104
29. Luo D, Liu S, Xie X, Hou X. Electroacupuncture at acupoint ST-36 promotes contractility of distal colon via a cholinergic pathway in conscious rats. Dig Dis Sci. 2008;53(3):689–693. doi:10.1007/s10620-007-9929-7
30. Yang NN, Yang JW, Ye Y, et al. Electroacupuncture ameliorates intestinal inflammation by activating α7nAChR-mediated JAK2/STAT3 signaling pathway in postoperative ileus. Theranostics. 2021;11(9):4078–4089. doi:10.7150/thno.52574
31. Farmer AD, Holt CB, Downes TJ, Ruggeri E, Del Vecchio S, De Giorgio R. Pathophysiology, diagnosis, and management of opioid-induced constipation. Lancet Gastroenterol Hepatol. 2018;3(3):203–212. doi:10.1016/S2468-1253(18)30008-6
32. Sheng RY, Yan Y, Linh Dang HH. Acupuncture for hot flashes: a literature review of randomized controlled trials conducted in the last 10 years. World J Tradit Chin Med. 2021;7:397–407. doi:10.4103/wjtcm.wjtcm_27_21
33. De Giorgio R, Zucco FM, Chiarioni G, et al. Management of opioid-induced constipation and bowel dysfunction: expert opinion of an Italian multidisciplinary panel. Adv Ther. 2021;38(7):3589–3621. doi:10.1007/s12325-021-01766-y
34. Yang NN, Ye Y, Tian ZX, et al. Effects of electroacupuncture on the intestinal motility and local inflammation are modulated by acupoint selection and stimulation frequency in postoperative ileus mice. Neurogastroenterol Motil. 2020;32(5):e13808. doi:10.1111/nmo.13808
35. Wang H, Xie Y, Zhang Q, et al. Transcutaneous electric acupoint stimulation reduces intra-operative remifentanil consumption and alleviates postoperative side-effects in patients undergoing sinusotomy: a prospective, randomized, placebo-controlled trial. Br J Anaesth. 2014;112(6):1075–1082. doi:10.1093/bja/aeu001
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
