Back to Journals » Open Access Emergency Medicine » Volume 15
Accuracy of Trauma on Scene Triage Screening Tool (Shock Index, Reverse Shock Index Glasgow Coma Scale and National Early Warning Score) to Predict the Severity of Emergency Department Triage: A Retrospective Cross-Sectional Study
Authors Yuksen C , Angkoontassaneeyarat C , Thananupappaisal S, Laksanamapune T, Phontabtim M, Namsanor P
Received 4 January 2023
Accepted for publication 15 March 2023
Published 21 March 2023 Volume 2023:15 Pages 79—91
DOI https://doi.org/10.2147/OAEM.S403545
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Chaiyaporn Yuksen, Chuenruthai Angkoontassaneeyarat, Sorawat Thananupappaisal, Thanakorn Laksanamapune, Malivan Phontabtim, Pamorn Namsanor
Department of Emergency Medicine, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
Correspondence: Chuenruthai Angkoontassaneeyarat, Department of Emergency Medicine, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, 270 Rama VI Road, Thung Phaya Thai, Ratchathewi, Bangkok, 10400, Thailand, Email [email protected]
Introduction: Prehospital trauma care includes on-scene assessments, essential treatment, and facilitating transfer to an appropriate trauma center to deliver optimal care for trauma patients. While the Simple Triage and Rapid Treatment (START), Revised Triage Sieve (rTS), and National Early Warning Score (NEWS) tools are user-friendly in a prehospital setting, there is currently no standardized on-scene triage protocol in Thailand Emergency Medical Service (EMS). Therefore, this study aims to evaluate the precision of these tools (SI, rSIG, and NEWS) in predicting the severity of trauma patients who are transferred to the emergency department (ED).
Methods: This study was a retrospective cross-sectional and diagnostic research conducted on trauma patients transferred by EMS to the ED of Ramathibodi Hospital, a university-affiliated super tertiary care hospital in Bangkok, Thailand, from January 2015 to September 2022. We compared the on-scene triage tool (SI, rSIG, and NEWS) and ED triage tool (Emergency Severity Index) parameters, massive transfusion protocol (MTP), and intensive care unit (ICU) admission with the area under ROC (univariable analysis) and diagnostic odds ratio (multivariable logistic regression analysis). The optimal cut-off threshold for the best parameter was determined by selecting the value that produced the highest area under the ROC curve.
Results: A total of 218 patients were traumatic patients transported by EMS to the ED, out of which 161 were classified as ESI levels 1– 2, while the remaining 57 patients were categorized as levels 3– 5 on the ESI triage scale. We found that NEWS was a more accurate triage tool to discriminate the severity of trauma patients than rSIG and SI. The area under the ROC was 0.74 (95% CI 0.70– 0.79) (OR 18.98, 95% CI 1.06– 337.25), 0.65 (95% CI 0.59– 0.70) (OR 1.74, 95% CI 0.17– 18.09) and 0.58 (95% CI 0.52– 0.65) (OR 0.28, 95% CI 0.04– 1.62), respectively (P-value < 0.001). The cut point of NEWS to discriminate ESI levels 1– 2 and levels 3– 5 was > 6 points.
Conclusion: NEWS is the best on-scene triage screening tool to predict the severity at the emergency department, massive transfusion protocol (MTP), and intensive care unit (ICU) admission compared with other triage tools SI and rSIG.
Keywords: triage, prehospital care, emergency medical services, emergency departments, trauma severity index
Introduction
The mortality risk among patients with severe traumatic injuries is 20%.1,2 To mitigate the risk of death, advanced emergency medical service (EMS) teams must access patients promptly. Immediate access enables the delivery of crucial on-scene treatment and facilitates adherence to appropriate guidelines for transporting injured patients to a designated trauma center.2 This approach is pivotal in minimizing the likelihood of death among trauma patients.
The out-of-hospital emergency triage tool is designed to prioritize patients with stroke and severe traumatic injuries. However, the current study highlights that no single triage tool is universally regarded as the gold standard or most accurate for out-of-hospital screening, particularly in traumatic injuries.3 To ensure optimal patient outcomes, a standardized emergency department (ED) screening tool should maintain a low level of undertriage (<5%) and over-triage (<35%).4 Accurate out-of-hospital emergency triage tools play a critical role in developing countries where early-stage EMS systems require effective screening tools to determine the severity of trauma patients and facilitate their transport to the appropriate trauma care facility.5–7
The Trauma Score (TS) was an early triage tool utilized for trauma patients, which incorporated the assessment of capillary refilling (CR) time and the sum of Glasgow Coma Scale (GCS) scores. However, studies have shown that the TS exhibits low sensitivity ranging from 43% to 83% while demonstrating high specificity levels of 88–99%.8 Another triage tool, the Revised Trauma Score (RTS), which includes Systolic Blood Pressure (SBP), Respiratory Rate (RR), and the sum of GCS scores, has also demonstrated relatively low sensitivity.9
Since 1986, the Field Trauma Decision Scheme (FTDS) has been employed as a triage tool in the United States, exhibiting sensitivity and specificity levels of 86% and 69%, respectively.10 Other triage tools, such as the Victorian Prehospital Trauma tool, have been utilized in France as a means of triaging patients with severe injuries.11,12 Meanwhile, the Dutch Field Triage Protocol has been employed in the Netherlands, with studies showing its ability to accurately classify severely injured patients (Injury Severity Score ≥16 points).13 The Prehospital Index (PHI) triage tool incorporates Systolic Blood Pressure (SBP), Pulse Rate (PR), Respiratory Rate (RR), and the total score of the GCS. Findings from a study suggest that a PHI score >3 points is a sensitive predictor of injury severity, ranging from 35% to 73%.14
New triage tools have been developed for sorting trauma patients in the pre-hospital setting, such as the National Early Warning Score (NEWS), which incorporates vital signs and the level of consciousness of out-of-hospital injury patients. Studies have demonstrated that this triage tool accurately predicts the likelihood of death at 1 and 30 days, with screening sensitivity and specificity levels for severely injured patients of 80% and 42%, respectively.15 The Shock Index (SI) triage tool was first utilized by Burri in 1967, incorporating the ratio of Heart Rate (HR) to Systolic Blood Pressure (SBP) (SI=HR/SBP). Research has shown that SI can predict the likelihood of death and massive blood transfusion.16,17 Another triage tool, the Reverse Shock Index Glasgow Coma Scale (rSIG), was developed by multiplying the SI with the sum of GCS scores, exhibiting greater predictive ability for the likelihood of death and massive blood transfusion compared to SI alone.18,19
Several studies have employed ED screening triage tools in the out-of-hospital setting, including the Canadian Triage and Acuity Scale (CTAS), a five-level screening system utilized in Canada. Research has shown a moderate level of agreement between triage nurses in the ED and paramedics in the out-of-hospital setting, with a kappa value of 0.437.20
The SI, rSIG, and NEWS triage tools are readily applicable in a prehospital setting. These tools can be easily employed by all levels of emergency medical responders, including basic life support and advanced life support teams, for on-scene assessments conducted outside of a hospital setting. Furthermore, the emergency medical system in Thailand currently lacks a standardized triage tool for screening out-of-hospital injuries and determining whether injured individuals should be transported to an appropriate trauma center. At present, out-of-hospital triage criteria are primarily based on patients’ clinical manifestations and the healthcare provider’s experience. The primary objective of this study was to assess the accuracy of the out-of-hospital injury assessment tools SI, rSIG, and NEWS in predicting the severity of traumatic patients upon arrival at the ED for the purpose of developing a suitable triage tool in Thailand. Additionally, the secondary objective was to determine the accuracy of these out-of-hospital injury assessment tools in predicting activation of the massive transfusion protocol (MTP) and admission to the intensive care unit (ICU).
Methods
Study Design and Setting
This study was a retrospective, cross-sectional diagnostic research conducted on emergency patients transported by an EMS team to the ED of Ramathibodi Hospital, a university-affiliated super tertiary care hospital in Bangkok, Thailand, from January 2015 to September 2022. The study received approval from the Committee on Human Rights Related to Research Involving Human Subjects, Ramathibodi Hospital, Mahidol University (COA. NO MURA2022/602). The ethics committee waived the need for participant consent since the study involved reviewing medical records. A statement covering patient data confidentiality and compliance with the Declaration of Helsinki was provided.
Participants
The domain of the study focused on injured patients who received prehospital care and were transported to the ED of Ramathibodi Hospital by the EMS team, including the basic and advanced life support teams, from January 2015 to September 2022. The eligible criteria for inclusion were patients aged between 18 and 65 years. Patients who had no available data regarding the scene or ED triage level, those who died on arrival at the ED, and pregnant patients were excluded from the study.
The primary triage data were calculated based on on-scene physiological parameters and summarized into the SI, rSIG, and NEWS scores. In addition, the ED triage nurse assessed the secondary triage using the Emergency Severity Index (ESI) triage tool to categorize injured patients into five levels (ESI 1–5). Two emergency physicians validated and adjusted the ESI triage levels to ESI levels 1–2 based on life-saving procedures.
Data Gathering and Outcome Measures
The study participants were identified from the EMS database and Emergency Medical Records (EMR). The on-scene physiologic parameters were recorded as study variables and used to calculate the SI score (HR and SBP), rSIG score (HR, SBP, and GCS score), and NEWS (RR, HR, SBP, body temperature, level of consciousness, and SpO2). The reference standard for triage was the ED triage using the five-level ESI triage system conducted by a triage nurse with five years of experience.
The recorded variables for injured patients included gender, age, dispatch code, mechanism of injury, level of consciousness, and vital signs in the prehospital and ED settings (systolic and diastolic blood pressure, heart rate, respiratory rate, body temperature, oxygen saturation, and Glasgow Coma Score). Additionally, ED lifesaving procedures such as cardiopulmonary resuscitation (CPR), tube thoracostomy, endotracheal intubation, major emergency operations, massive transfusion protocol (MTP), ICU admission, and hospital length of stay (LOS) were also recorded.
Definitions
The Shock Index (SI) is defined as the ratio between the heart rate (HR) and systolic blood pressure (SBP) (HR/SBP). The Reverse Shock Index (rSI) is defined as the ratio between SBP and HR (SBP/HR). The Reverse Shock Index Glasgow Coma Scale (rSIG) is calculated by multiplying the rSI and Glasgow Coma Scale (GCS) (rSI * GCS). The National Early Warning Score (NEWS) is a composite score that includes seven parameters: respiratory rate, heart rate, systolic blood pressure, body temperature, level of consciousness, and SpO2. These variables are summarized in Table 1.
 |
Table 1 National Early Warning Score (NEWS) |
The Emergency Severity Index (ESI) is an ED triage algorithm that utilizes five levels to stratify patients into clinically relevant groups. These groups include level 1 (a life-threatening condition), level 2 (representing a high-risk condition), and levels 3–5 (indicating urgent conditions).
Statistical Analysis
Data were analyzed by using STATA version 16.0. All study variables were compared between two groups, ESI 1–2 and ESI 3–5. We use Fisher's exact test for categorical variables and present with frequency (percentage), Student’s t-test for normal distribution continuous variables presented with mean ± standard deviation (SD), and rank-sum test for non-normal distribution continuous variable presented with median (interquartile range).
The accuracy and diagnostic indices of each score (SI, rSIG, NEWS) compared with ESI (reference standard) were calculated using univariable analysis, presented as the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), likelihood ratio positive (LR+), likelihood ratio negative (LR-) and receiver operating characteristic (AuROC) curve with a 95% confidence interval (CIs). The cut point values of SI, rSIG, and NEWS determine with maximizing specificity and sensitivity. The AuROC of SI, rSIG, and NEWS was defined as good (more than 0.90), fair (0.70–0.80), and poor (less than 0.70) to predict the severity of ED triage.
Multivariable logistic regression was used to evaluate the prediction performance of SI, rSIG, and NEWS and presented with diagnostic odds ratios (OR), 95% confidence interval (CIs), and P-value. We include all variables in the multivariable model. P-value <0.05 was statistically significant. The score with high discriminative performance (AuROC curve) increased odds ratios, and statistical significance (p-value) can predict ESI triage, representing the best prehospital triage tool among the three scores.
We used a pilot study and STATA version 16.0 to calculate the sample size. The pilot study was conducted from January to May 2022. Therefore, based on the comparing test of two independent means, two side tests, alpha error 0.05, and power of 90%. The minimized sample size of SI, rSIG, and NEWS to discriminate ESI 1–2 and ESI 3–5 were at least 182.
Results
During the study period, from January 2015 to September 2022, a total of 279 patients met the eligibility criteria and were included. Of these, 15 patients were excluded due to death at the scene or before arrival at the ED, and 46 patients were excluded due to missing variable data necessary to calculate SI, rSIG, NEWS, and ED triage levels. Ultimately, 218 patients were included in the analysis.
Table 2 presents the baseline characteristics of the study population, categorized into two groups based on their ESI triage levels: ESI1-2 (life-threatening and high-risk condition) and ESI3-5 (urgent condition). Among the 218 patients included in the analysis, 161 (73.85%) were triaged to ESI1-2 and 57 (26.15%) were triaged to ESI3-5. The mean age of patients in the ESI1-2 group was significantly lower than that in the ESI3-5 group (41.16 ± 1.44 and 52.96 ± 3.02, respectively, with a P-value <0.001). Furthermore, the ESI1-2 group had a higher proportion of male patients compared to the ESI3-5 group (81.99% and 52.63%, respectively, with a P-value <0.001). The most common incident dispatch code reported in the ESI1-2 group was a traffic accident (107, 66.46%), followed by a fall from height (44, 27.33%). In contrast, the most common dispatch code in the ESI3-5 group was a fall from height (30, 52.63%), followed by a traffic accident (25, 43.86%).
 |
Table 2 Study Population Characteristics |
The mechanism of injury in the ESI 1–2 group was predominantly motor vehicle collision (MVC) (86, 53.42%) followed by blunt injury (34, 21.12%), while in the ESI 3–5 group, it was blunt injury (27, 47.37%) related to falls from height, followed by MVC (20, 35.09%). The vital signs between the two groups were not significantly different, except for oxygen saturation (SpO2), which was lower in the ESI 1–2 group (91.69%) compared to the ESI 3–5 group (97.85%), and was significantly different (p < 0.001). Additionally, the Glasgow Coma Scale (GCS) score was significantly different between the two groups, with lower scores observed in the ESI 1–2 group.
The NEWS score was the only tool that showed a significant difference between the ESI1-2 and ESI 3–5 groups, with a score of 5.96 (IQR 2–9) and 1.30 (IQR 0–2), respectively (p < 0.001). However, there were no significant differences observed between the two groups with regard to the SI and rSIG scores.
Accuracy of SI, rSIG, and NEWS to Predict ED Triage
The optimal cut-off point value with maximizing specificity and sensitivity to predict ED triage of SI was >0.8 (specificity = 78.9, sensitivity = 37.5), rSIG was <16 (specificity = 87.7, sensitivity = 42.1), and NEWS was >6 (specificity = 98.2, sensitivity = 50.3), respectively (Table 3). The discrimination performance (AuROC, 95% CI) to predict ED triage of SI >0.8, rSIG <16, and NEWS >6 were 0.58 (95% CI, 0.52–0.65), 0.65 (95% CI, 0.59–0.70) and 0.74 (95% CI, 0.70–0.65), respectively, p < 0.001 (Figure 1). NEWS is the most accurate prehospital screening tool to predict ESI 1–2 in this study.
 |
Table 3 Predictive Power of the SI, rSIG, and NEWS to Predict ESI Levels 1–2 |
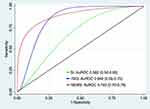 |
Figure 1 Receiver operating characteristic curve for ESI level I-2. |
Accuracy of SI, rSIG, and NEWS to Predict MTP Activation
The optimal cut-off point value with maximizing specificity and sensitivity to predict MTP activation of SI was >0.8 (specificity = 71.3, sensitivity = 61.9), rSIG was <16 (specificity = 72.4, sensitivity = 71.4), and NEWS was >6 (specificity = 70.0, sensitivity = 81.8), respectively (Table 4). The discrimination performance (AuROC, 95% CI) to predict MTP activation of SI >0.8, rSIG <16, and NEWS >6 were 0.67 (95% CI, 0.55–0.77), 0.72 (95% CI, 0.61–0.82) and 0.76 (95% CI, 0.67–0.85), respectively, p = 0.111 (Figure 2). In this study, NEWS is the most accurate prehospital screening tool to predict MTP activation.
 |
Table 4 Predictive Power of the SI, rSIG and NEWS for Intensive Care Unit (ICU) Admission |
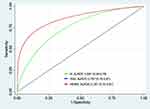 |
Figure 2 Receiver operating characteristic curve for intensive care unit (ICU) admission. |
Accuracy of SI, rSIG, and NEWS to Predict Intensive Care Unit (ICU) Admission
The optimal cut-off point value with maximizing specificity and sensitivity to predict ICU admission of SI was >0.8 (specificity = 76.2, sensitivity = 61.1), rSIG was <16 (specificity = 83.3, sensitivity = 74.1), and NEWS was >6 (specificity = 82.9, sensitivity = 74.1), respectively (Table 5). The discrimination performance (AuROC, 95% CI) to predict ICU admission of SI >0.8, rSIG <16, and NEWS >6 were 0.69 (95% CI, 0.59–0.78), 0.79 (95% CI, 0.70–0.87) and 0.79 (95% CI, 0.70–0.87, respectively, p = 0.052) (Figure 3). Both NEWS and rSIG are the most accurate prehospital screening tools to predict ICU admission in this study.
 |
Table 5 Predictive Power of the SI, rSIG and NEWS for Massive Transfusion Protocol (MTP) Activation |
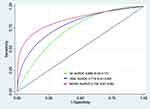 |
Figure 3 Receiver operating characteristic curve for massive transfusion protocol (MTP) activation. |
Diagnostic Odds Ratio of SI, rSIG, and NEWS
Multivariable logistic regression analysis is shown in Table 6. Adjusted for the variable of gender, age, the incident dispatch code, mechanism of injury, Glasgow coma score, ED lifesaving procedures include cardiopulmonary resuscitation (CPR), tube thoracostomy, endotracheal intubation, major emergency operation, hypotension, and vasopressor use. NEWS is the best triage tool to predict ED triage (diagnostic OR 18.98, 95% CI, 1.06–337.25, p = 0.045) MTP activation (diagnostic OR 6.01, 95% CI, 0.45–80.65, p = 0.175) and ICU admission (diagnostic OR 3.58, 95% CI, 0.31–41.37, p = 0.307).
 |
Table 6 Multivariable Logistic Regression Analysis of the Prediction Tool |
Discussion
The present study demonstrated that NEWS outperformed SI and rSIG in predicting ED triage, MTP activation, and ICU admission in trauma patients. This result indicates that NEWS should be implemented as a triage tool in prehospital trauma care, particularly in Thailand where there is no standardized prehospital triage tool. Therefore, prehospital care providers should consider incorporating NEWS into their routine practice to enhance the quality of care and improve patient outcomes.
NEWS is comprised of seven parameters including respiratory rate, heart rate, systolic blood pressure, body temperature, level of consciousness, and oxygen saturation. These parameters can be evaluated by both basic and advanced trauma teams in prehospital settings. High NEWS scores in prehospital trauma patients are associated with increased rates of ICU admission and mortality. Furthermore, the NEWS tool can be easily administered by personnel with limited experience, does not require complex equipment, and can be used in both trauma and medical conditions.21
A recent study by Siberian et al in 2022 found that prehospital NEWS scores >7 and ED ESI levels 1–2 can predict the severity of patient outcomes with high accuracy (AuROC = 0.825 and 0.897, respectively).22 This is consistent with our study which demonstrates that a NEWS score >6 can predict ESI levels 1–2, MTP activation, and ICU admission. These findings suggest that NEWS should be implemented as a standard triage tool in prehospital trauma settings, particularly in regions like Thailand where no standardized triage tool currently exists.
Observational studies conducted on both trauma and non-trauma patients have demonstrated that a high-risk NEWS score (>7 points) is associated with increased 24-hour, 48-hour, and 30-day mortality, as well as increased ICU admission rates.23,24 In addition, Abbott et al have recommended the use of NEWS by prehospital care providers as a tool to assist in the primary triage of patients requiring hospital admission or emergency transport to an appropriate trauma center facility.25 These results are consistent with our study, which found that a NEWS score >6 was the best predictive tool for ICU admission in trauma patients (OR 3.58, 95% CI: 0.31–41.37).
The study of Martin et al, a prospective observational multi-center study, found that NEWS was the prehospital triage tool that was easy to perform and had high accuracy for the assessment of high-risk patients, moreover used for second triage in the mass-casualty incident.21 NEWS2 was the new triage tool that evaluated the patients who required oxygen and measured the oxygen saturation after oxygen supplementing, which is a good triage tool for hypercapnic respiratory failure patients such as chronic obstructive pulmonary disease. Furthermore, a recent study showed no significant difference in predicting in-hospital mortality.26,27 Our study focused only on trauma patients, so we did not consider using NEWS2 in this study.
Severe hemorrhage is the primary cause of mortality among multiple trauma patients. A prehospital tool capable of predicting massive blood transfusion (MBT) activation is a potentially life-saving intervention that could reduce the time required to transport blood components from the blood bank to the operating room and increase seven-day survival rates.28 Several scoring systems have been developed to predict the need for MBT, including the ABC score, which takes into account the penetrating mechanism, ED SBP, ED HR, and a positive Focused Assessment with Sonography for Trauma (FAST) exam, as well as the MBTT score, which is calculated based on age (>60 years), BE (<−10 mEq/L), lactate (>4 mmol/L), and HR (>105/min) or SOFA score (>9).29–31 Other indicators, such as the shock index at ED arrival, can indicate hypovolemic shock and the likelihood of requiring transfusion.17
In the study by Koch et al, shock index was shown to be a good predictor, where a shock index >0.9–1.1 could predict massive blood transfusion with an RR of 1.61 (95% CI: 1.13–2.31) but could not predict ICU admission and mortality.32 In our study, the cut-off point for shock index was >0.8, which was lower than the previous study. Lee et al19 found that rSIG was a practical, rapid, and accurate predictor for massive transfusion and mortality with a lower cut-off (<9.52 points) than in our study (<16 points).
The provision of emergency medical services in Thailand is regulated and monitored by the National Institute for Emergency Medicine (NIEM) under the Emergency Medicine Act B.E. 2551, which has been in effect since 2008. The emergency response system in Thailand consists of multiple tiers, including basic life support (BLS) led by emergency medical technicians, advanced life support (ALS) led by emergency physicians or paramedics, and first responder units led by first responders.33 The emergency medical number in Thailand is 1669, and the dispatch center uses a priority dispatch protocol to categorize trauma patients as “Red”, “Yellow”, or “Green” based on the severity of their injuries. The optimal response time, scene time, and transport time for trauma patients are 8–10 minutes, 10 minutes, and 10 minutes, respectively.
Currently, there is no standardized triage protocol in Thailand for transferring trauma patients to the appropriate trauma care facility. The decision regarding the selection of a specific trauma center depends on the experience of the physician, medical insurance coverage, and the proximity of the trauma center. However, this can lead to both over- and under-triage, resulting in the transfer of trauma patients to inappropriate facilities. Additionally, severe trauma patients who are undertriaged and sent to lower-level trauma centers have higher mortality rates.34
A universal trauma triage protocol could provide an easy and practical approach for prehospital care responders at all levels. Our study showed that NEWS (>6 points) was the best predictor tool for identifying patients with ESI levels 1–2, ICU admission, and massive transfusion protocol activation, as compared to SI and rSIG. Based on these findings, we suggest that NEWS could be used as a prehospital screening tool and could be implemented by the first medical responder.
Limitation
This study has several limitations. Firstly, due to its retrospective design, a prospective cohort study would be beneficial in validating the results. Additionally, selection and information biases could potentially affect the study results. As a single-center study conducted in a university hospital with advanced equipment, the findings may not be generalizable to other settings with limited resources. Furthermore, missing data may impact the accuracy of the interpretation of the results. The study’s small sample size over a seven-year period is another limitation, which can be attributed to the location of Ramathibodi Hospital in the catchment area of three Level 1 trauma hospitals. Finally, the diagnostic odds ratio of NEWS had a large confidence interval, which raises concerns about Type 1 error.
Conclusion
The present study concludes that NEWS is superior to other triage tools, such as SI and rSIG, in predicting severity at the emergency department, massive transfusion protocol (MTP), and intensive care unit (ICU) admission. Moreover, NEWS has the potential to serve as a valuable adjunct for the prehospital evaluation of trauma patients, aiding in their allocation to trauma centers and ICU admission or activation of the trauma team and massive blood protocol.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Considerations
This study was approved by the Faculty of Medicine, Committee on Human Rights Related to Research Involving Human Subjects, Ramathibodi Hospital, Mahidol University (COA. NO MURA2022/602). The ethics committee did not require consent for this research because reviewing the medical record is the reason for the waiver and a statement covering patient data confidentiality and compliance with the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work re-ported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funding was obtained for this study.
Disclosure
The authors declare that they have no competing interests.
References
1. Kondo Y, Fukuda T, Uchimido R, et al. Advanced life support vs basic life support for patients with trauma in prehospital settings: a systematic review and meta-analysis. Front Med. 2021;8:660367. doi:10.3389/fmed.2021.660367
2. Hansen J, Rasmussen LS, Steinmetz J. Prehospital triage of trauma patients before and after implementation of a regional triage guideline. Injury. 2022;53(1):54–60. doi:10.1016/j.injury.2021.10.011
3. Bhaumik S, Hannun M, Dymond C, et al. Prehospital triage tools across the world: a scoping review of the published literature. Scand J Trauma Resusc Emerg Med. 2022;30(1):32. doi:10.1186/s13049-022-01019-z
4. The American College of Surgeons Committee on Trauma. Resources for optimal care of the injured patient; 2014. Available from: https://www.facs.org/media/yu0laoqz/resources-for-optimal-care.pdf.
5. Suryanto PV, Boyle M. EMS systems in lower-middle income countries: a literature review. Prehosp Disaster Med. 2017;32(1):64–70. doi:10.1017/S1049023X1600114X
6. Jenson A, Hansoti B, Rothman R, de Ramirez SS, Lobner K, Wallis L. Reliability and validity of emergency department triage tools in low- and middle-income countries: a systematic review. Eur J Emerg Med. 2018;25(3):154–160. doi:10.1097/MEJ.0000000000000445
7. Mould-Millman NK, Dixon JM, Sefa N, et al. The state of Emergency Medical Services (EMS) systems in Africa. Prehosp Disaster Med. 2017;32(3):273–283. doi:10.1017/S1049023X17000061
8. Morris JA, Auerbach PS, Marshall GA, Bluth RF, Johnson LG, Trunkey DD. The Trauma Score as a triage tool in the prehospital setting. JAMA. 1986;256(10):1319–1325. doi:10.1001/jama.1986.03380100093027
9. Sturms LM, Hoogeveen JM, Le Cessie S, et al. Prehospital triage and survival of major trauma patients in a Dutch regional trauma system: relevance of trauma registry. Langenbecks Arch Surg. 2006;391(4):343–349. doi:10.1007/s00423-006-0057-1
10. Newgard CD, Zive D, Holmes JF, et al. A multisite assessment of the American College of Surgeons Committee on Trauma field triage decision scheme for identifying seriously injured children and adults. J Am Coll Surg. 2011;213(6):709–721. doi:10.1016/j.jamcollsurg.2011.09.012
11. Cassignol A, Marmin J, Cotte J, et al. Correlation between field triage criteria and the injury severity score of trauma patients in a French inclusive regional trauma system. Scand J Trauma Resusc Emerg Med. 2019;27(1):71. doi:10.1186/s13049-019-0652-0
12. Cassignol A, Markarian T, Cotte J, et al. Evaluation and comparison of different prehospital triage scores of trauma patients on in-hospital mortality. Prehosp Emerg Care. 2019;23(4):543–550. doi:10.1080/10903127.2018.1549627
13. Voskens FJ, van Rein EAJ, van der Sluijs R, et al. Accuracy of prehospital triage in selecting severely injured trauma patients. JAMA Surg. 2018;153(4):322–327. doi:10.1001/jamasurg.2017.4472
14. Lavoie A, Emond M, Moore L, Camden S, Liberman M. Evaluation of the Prehospital Index, presence of high-velocity impact and judgment of emergency medical technicians as criteria for trauma triage. Cjem. 2010;12(2):111–118. doi:10.1017/S1481803500012136
15. Hoikka M, Silfvast T, Ala-Kokko TI. Does the prehospital National Early Warning Score predict the short-term mortality of unselected emergency patients? Scand J Trauma Resusc Emerg Med. 2018;26(1):48. doi:10.1186/s13049-018-0514-1
16. Pandit V, Rhee P, Hashmi A, et al. Shock index predicts mortality in geriatric trauma patients: an analysis of the National Trauma Data Bank. J Trauma Acute Care Surg. 2014;76(4):1111–1115. doi:10.1097/TA.0000000000000160
17. Mutschler M, Nienaber U, Münzberg M, et al. The Shock Index revisited - a fast guide to transfusion requirement? A retrospective analysis on 21,853 patients derived from the TraumaRegister DGU. Crit Care. 2013;17(4):R172. doi:10.1186/cc12851
18. Wan-Ting C, Chin-Hsien L, Cheng-Yu L, et al. Reverse shock index multiplied by Glasgow Coma Scale (rSIG) predicts mortality in severe trauma patients with head injury. Sci Rep. 2020;10(1):2095. doi:10.1038/s41598-020-59044-w
19. Lee YT, Bae BK, Cho YM, et al. Reverse shock index multiplied by Glasgow coma scale as a predictor of massive transfusion in trauma. Am J Emerg Med. 2021;46:404–409. doi:10.1016/j.ajem.2020.10.027
20. Leeies M, Ffrench C, Strome T, Weldon E, Bullard M, Grierson R. Prehospital application of the Canadian triage and acuity scale by emergency medical services. Cjem. 2017;19(1):26–31. doi:10.1017/cem.2016.345
21. Martín-Rodríguez F, López-Izquierdo R, Del Pozo Vegas C, et al. Accuracy of National Early Warning Score 2 (NEWS2) in prehospital triage on in-hospital early mortality: a Multi-Center Observational Prospective Cohort Study. Prehosp Disaster Med. 2019;34(6):610–618. doi:10.1017/S1049023X19005041
22. Saberian P, Abdollahi A, Hasani-Sharamin P, Modaber M, Karimialavijeh E. Comparing the prehospital NEWS with in-hospital ESI in predicting 30-day severe outcomes in emergency patients. BMC Emerg Med. 2022;22(1):42. doi:10.1186/s12873-022-00598-5
23. Silcock DJ, Corfield AR, Gowens PA, Rooney KD. Validation of the National Early Warning Score in the prehospital setting. Resuscitation. 2015;89:31–35. doi:10.1016/j.resuscitation.2014.12.029
24. Alam N, Vegting IL, Houben E, et al. Exploring the performance of the National Early Warning Score (NEWS) in a European emergency department. Resuscitation. 2015;90:111–115. doi:10.1016/j.resuscitation.2015.02.011
25. Abbott TEF, Cron N, Vaid N, Ip D, Torrance HDT, Emmanuel J. Pre-hospital National Early Warning Score (NEWS) is associated with in-hospital mortality and critical care unit admission: a cohort study. Ann Med Surg. 2018;27:17–21. doi:10.1016/j.amsu.2018.01.006
26. Kostakis I, Smith GB, Prytherch D, Meredith P, Price C, Chauhan A. The performance of the National Early Warning Score and National Early Warning Score 2 in hospitalised patients infected by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Resuscitation. 2021;159:150–157. doi:10.1016/j.resuscitation.2020.10.039
27. Smith GB, Redfern OC, Pimentel MA, et al. The National Early Warning Score 2 (NEWS2). Clin Med. 2019;19(3):260. doi:10.7861/clinmedicine.19-3-260
28. Chau-In W, Soontrapa S, Puapairoj J, et al. Study the effectiveness of massive transfusion protocol at Srinagarind Hospital Faculty of Medicine, Khon Kaen University. Srinagarind Med J. 2013;28(3):327–336.
29. Nunez TC, Voskresensky IV, Dossett LA, Shinall R, Dutton WD, Cotton BA. Early prediction of massive transfusion in trauma: simple as ABC (assessment of blood consumption)? J Trauma. 2009;66(2):346–352. doi:10.1097/TA.0b013e3181961c35
30. Akaraborworn O, Chaiwat O, Chatmongkolchart S, et al. Prediction of massive transfusion in trauma patients in the surgical intensive care units (Thai-SICU study). Chin J Traumatol. 2019;22(4):219–222. doi:10.1016/j.cjtee.2019.04.004
31. Akaraborworn O, Siribumrungwong B, Sangthong B, Thongkhao K. Massive blood transfusion for trauma score to predict massive blood transfusion in trauma. Crit Care Res Pract. 2021;2021:3165390. doi:10.1155/2021/3165390
32. Koch E, Lovett S, Nghiem T, Riggs RA, Rech MA. Shock index in the emergency department: utility and limitations. Open Access Emerg Med. 2019;11:179–199. doi:10.2147/OAEM.S178358
33. Riyapan S, Thitichai P, Chaisirin W, Nakornchai T, Chakorn T. Outcomes of emergency medical service usage in severe road traffic injury during Thai holidays. West J Emerg Med. 2018;19(2):266–275. doi:10.5811/westjem.2017.11.35169
34. van Rein EAJ, van der Sluijs R, Houwert RM, et al. Effectiveness of prehospital trauma triage systems in selecting severely injured patients: is comparative analysis possible? Am J Emerg Med. 2018;36(6):1060–1069. doi:10.1016/j.ajem.2018.01.055
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
