Back to Journals » Psoriasis: Targets and Therapy » Volume 8
Abatacept for the treatment of adults with psoriatic arthritis: patient selection and perspectives
Authors Noisette A , Hochberg MC
Received 11 February 2018
Accepted for publication 10 May 2018
Published 11 July 2018 Volume 2018:8 Pages 31—39
DOI https://doi.org/10.2147/PTT.S146076
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Uwe Wollina
Ashley Noisette, Marc C Hochberg
Division of Rheumatology and Clinical Immunology, Department of Medicine, University of Maryland School of Medicine, Baltimore, MD, USA
Abstract: Psoriatic arthritis (PsA) is a heterogeneous disease with several clinical subtypes including peripheral arthritis, dactylitis, enthesitis, nail disease, and axial arthritis. Nonsteroidal anti-inflammatory drugs, glucocorticoids, and conventional disease-modifying agents are used as first line in the treatment of active PsA. For moderate-to-severe PsA failing conventional therapy, antitumor necrosis factor inhibitors have historically been the drugs of choice. In recent years, novel interleukin-23/interleukin-17 pathway targets such as ustekinumab and secukinumab, and phosphodiesterase-4 inhibitor apremilast have been approved for use in the United States and Europe. Two sets of recommendations for the management of PsA were published in 2016 with consideration for these newer therapies. Since then, the results from a Phase III randomized controlled trial demonstrated that abatacept has efficacy in the treatment of PsA. Abatacept, a cytotoxic-T-lymphocyte-associated antigen 4 (CTLA-4)–Ig human fusion protein, acts to prevent naïve T-cell activation through the inhibition of the critical CD28 co-stimulatory signal. In the 2017 Active Psoriatic Arthritis Randomized Trial (ASTRAEA), 424 participants were randomized 1:1 to receive subcutaneous abatacept 125 mg weekly versus placebo. At week 24, 39.4% of those who received abatacept achieved a minimum of 20% improvement in the American College of Rheumatology (ACR) response compared to 22.3% in the placebo arm, a statistically significant finding (P<0.001). The 2011 Phase II study published by Mease et al demonstrated statistically significant improvements in the ACR20 response by week 169 in participants treated with intravenous abatacept 10 mg/kg (48%) and 30/10 mg/kg (42%) when compared with placebo (19%). This article reviews the data supporting the efficacy of abatacept in the management of PsA and attempts to place this agent in the context of other biologic disease-modifying antirheumatic drugs and targeted small molecules used in the treatment of patients with PsA.
Keywords: biologic DMARD, psoriasis, T-cell inhibition, targeted small molecules
Introduction
Psoriatic arthritis (PsA) is a chronic, potentially debilitating and deforming inflammatory arthritis that occurs in an estimated 6–41% of individuals with a history of skin psoriasis (PSO).1 In 1973, Moll and Wright2 outlined five clinical phenotypes of PsA, including distal interphalangeal joint arthritis, peripheral oligoarthritis, peripheral polyarthritis, axial arthritis (sacroiliitis or spondylitis), and arthritis mutilans, proposing the first classification criteria for this disease. The criteria included the presence of an inflammatory arthritis, either peripheral or axial, occurring in a patient with PSO who usually had a negative test for rheumatoid factor in the serum. Presently, the classification criteria developed by the Classification Criteria for Psoriatic Arthritis (CASPAR) Study Group are the most widely used entry criteria for enrollment in clinical trials in PsA.3 Individual criteria are as follows: personal history or family history of PSO, juxta-articular new bone formation on radiography, dactylitis, psoriatic nail disease, and a negative rheumatoid factor.3 All components are worth one point with the exception of a current history of PSO, which is worth two points.3 A score of ≥3 has a sensitivity exceeding 90% and a specificity approaching 100% for identifying individuals with PsA.3
Management through 2016
Historically, the treatment of PsA has involved the use of nonsteroidal anti-inflammatory drugs (NSAIDs), glucocorticoids, and conventional disease-modifying antirheumatic drugs (cDMARDs). Ash et al4 performed a systematic literature review as a part of the development of the 2012 European League against Rheumatism (EULAR) recommendations for the management of PsA. In this review, it was concluded that NSAIDs were efficacious in patients with PsA and that methotrexate (MTX), sulfasalazine, cyclosporine, and leflunomide were effective for peripheral arthritis.4 Unlike in rheumatoid arthritis (RA), these drugs have not been shown to modify disease progression.5,6 Furthermore, there is little evidence available on the effectiveness of cDMARDs on dactylitis, enthesitis, or axial disease.7 The class of parenterally administered biologic disease-modifying agents (bDMARDs) known as tumor necrosis factor inhibitors (TNFis) was first studied in the early part of this century and was included in the 2012 EULAR recommendations where they were recommended in PsA patients with predominant axial disease, severe enthesitis or after treatment failure with NSAIDs, and at least one cDMARD.8 After failing TNFi therapy, only up to 40% of individuals will respond to a second TNFi drug, illustrating the need for new targets in the treatment of PsA.9
The EULAR recommendations were updated in 2015 to reflect the availability of the orally administered targeted synthetic DMARD apremilast, a phosphodiesterase 4 inhibitor, and the new bDMARDs such as secukinumab and ustekinumab that target the interleukin-17 (IL-17) and interleukin-12/23 (IL-12/23) pathways, respectively.10–13 The Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA) also published recommendations for the treatment of PsA in 2016; the major differences were the latter’s inclusion of dermatologists and the focus on specific domains of involvement such as peripheral arthritis, axial disease, enthesitis, dactylitis, nail disease, and skin disease.7 There have been two subsequent studies commenting on the similarities and differences between these recommendations.14,15
The role of abatacept
The T cell plays an integral role in the pathogenesis of PsA and has been studied as a potential pharmacologic target.16,17 Abatacept is a naïve T-cell activation inhibitor that has been approved for the treatment of RA in both Europe and the United States for over a decade.18 Data from a large Phase III randomized controlled trial (RCT) of 424 patients with PsA failing conventional therapy support the use of abatacept in the treatment of PsA.19 This article reviews the role of the T cell in the pathophysiology of PsA and the current data on abatacept in PsA with consideration for disease phenotypes and extra-articular manifestations.
The T cell and PsA pharmacotherapy
The pathogenesis of PsA is complex, multifactorial, and not fully understood. Recently, Ritchlin et al20 published an article in the New England Journal of Medicine noting clear genetic predispositions, mediated by class I major histocompatibility complex (MHC) antigens as well as polymorphisms in genes encoding the IL-23 receptor and nuclear factor kappa B, and environmental risk factors including obesity and prior joint trauma as key factors in the pathophysiology of PsA. Although PsA occurs in individuals with a personal or strong family history of PSO, not all patients with PSO develop PsA illustrating that that these conditions may have similar but varying underlying pathogeneses.
T-cell-released IL-17 has been identified as a proinflammatory and osteoclastogenic cytokine in the pathogenesis of PsA.21,22 In 2014, Menon et al21 published a small study providing evidence that IL-17-producing T cells, mainly CD8+ T cells, are elevated in the synovial fluid of those with PsA compared to RA. This study also found that the presence of elevated IL-17-producing CD4-negative T cells correlated with elevated inflammatory markers, active synovitis, and erosive disease.21 These findings suggest that IL-17-producing CD4-negative T cells are the major drivers of disease activity in PsA.21 These findings are in contrast to a 2012 study by Raychaudhuri et al23 who illustrated that CD4+ T helper cells were the major producer of IL-17. These conflicting reports of whether IL-17 is predominately produced by CD4– or CD4+ cells were attributed to different stimulation protocols used in these two notable studies.21 These results illustrate the central role of IL-17-producing T cells (Th17) in the pathogenesis of active PsA.
TNF and IL-23/IL-17 pathways have been targeted successfully in the treatment of both PSO and PsA.20 Secukinumab and ixekizumab are IL-17-targeted biologics currently approved in the United States for the treatment of PsA.24,25 Ustekinumab, although not a direct IL-17 target, inhibits the IL-12/IL-23 pathway, which leads to decreased Th17 cytokine production and IL-17 release.26 TNFi drugs have been shown in some studies to decrease T-cell infiltration of the synovium of those with PsA, which is potentially one of the pathways enabling drug efficacy, along with proinflammatory cytokine inhibition.27 Of note, greater improvements in PSO than in PsA have been seen with the use of anti-IL-17 and anti-IL-23 biologics, in contrast to the use of TNFi where efficacy on joint and skin diseases appears to be equal.28
T-cell inhibitor alefacept has demonstrated statistically significant improvements in the American College of Rheumatology 20 (ACR20) response, a valid, reliable, and responsive arthritis outcome measure, when compared with placebo.29 Unlike abatacept that inhibits naïve T-cell activation, alefacept selectively targets memory T cells through the inhibition of the CD2 co-stimulatory pathway.29,30 In a 2006 study, 185 patients with PsA were randomized to receive either alefacept with concomitant MTX or placebo with MTX.29 At week 24, the ACR20 response was 54% in the alefacept group compared to 23% in the placebo group (P<0.001).29
Abatacept mechanism of action and use in RA
Abatacept is a cytotoxic-T-lymphocyte-associated antigen 4 (CTLA-4)–Ig human fusion protein that inhibits naïve T-cell activation.30 The first signal needed for T-cell activation occurs after the binding of the T-cell receptor on the naïve T cell to the MHC molecule on the antigen-presenting cell (APC).31 CD28 is present on naïve T cells and, when bound to CD80 or CD86, located on the APC, produces a co-stimulatory second signal activating the naïve T cell.32 CTLA-4 is expressed on regulatory T cells (Tregs) and, when bound to CD80/CD86, prevents the co-stimulatory binding of CD28.33
CTLA-4–Ig fusion molecule, abatacept, has been studied and proven to be effective in RA and select patients with juvenile idiopathic arthritis (JIA).34,35 The use of abatacept in both MTX-naïve early erosive RA and MTX-resistant RA has resulted in significant improvements in disease activity, functional status, and radiographic progression when compared with MTX-alone placebo arms.34,36 Similarly, abatacept has demonstrated effectiveness in the treatment of moderate-to-severe RA in patients failing TNFi therapy.32
Abatacept is available in both a weight-based, monthly intravenous (IV) infusion and a fixed-dose weekly subcutaneous (SQ) injection.37 IV and SQ abatacept appear to have similar efficacy profiles.38 Abatacept is generally well tolerated for use as monotherapy or in combination with cDMARDs.38,39
Abatacept use in PsA
There are two key studies available in the literature that illustrate the effectiveness of abatacept in the treatment of patients with moderate-to-severe PsA and active PSO failing DMARD therapy. The 6-month, Phase II RCT published by Mease et al40 in 2011 included 170 participants who fulfilled CASPAR criteria for PsA and were randomized 1:1:1:1 to receive IV abatacept at three different dosing regimens or placebo. Those who received abatacept were randomized to one of the following dosages: abatacept 3, 10, and 30/10 mg/kg; the latter was given as a 30 mg/kg loading dose followed by 10 mg/kg every 28 days.40 The loading dosages were administered at days 1, 15, and 29 after which abatacept was given on a 28-day schedule for a total treatment time of 6 months.40 At month 6, all participants received open-label abatacept at 10 mg/kg for an additional 18 months.40
The participants were required to have DMARD-resistant disease.40 In particular, MTX was considered as failure if used at ≥15 mg/week for a minimum of 2 months.40 When assessing ACR response, patients were stratified based on previous TNFi use.40 Only stable doses of MTX, NSAIDs, and corticosteroids at ≤10 mg were allowed in the study.40
The percentage of participants who met the primary endpoint (ACR20 response at day 169) was statistically significant in both the abatacept 10 mg/kg group (48%, P=0.006) and the 30/10 mg/kg group (42%, P=0.022) when compared with placebo (19%).40 At the 10 mg/kg dose, more TNFi-naïve participants achieved an ACR20 response than the TNFi-exposed group (56 versus 31%).40 Trends toward greater radiographic improvement, assessed by change in a modified Rheumatoid Arthritis Magnetic Resonance Imaging Scoring (RAMRIS) system, were seen by day 169 in those who had received abatacept compared to placebo.40 Similarly, in assessing improvements in the quality of life and functional status, more participants who received abatacept (3 mg/kg [36%], 10 mg/kg [45%], and 30/10 mg/kg [35%]) achieved a minimum clinically important difference (MCID) of the disability index of the Health Assessment Questionnaire Disability Index (HAQ-DI) when compared with placebo (19%) by day 169.40 Statistical analysis was not performed on these secondary endpoints due to the lack of power in this study.40
The Phase III ASTRAEA study assessed the efficacy and safety of SQ abatacept in 424 PsA participants who failed or were intolerant to at least one cDMARD.19 All patients fulfilled CASPAR criteria and had both active peripheral arthritis and PSO.19 Patients were randomized 1:1 to receive either a fixed dose of 125 mg abatacept SQ or placebo.19 The randomized participants were further stratified by current use of MTX, prior use of TNFi(s), and extent of active PSO.19 At week 16, those who failed to have ≥20% improvement in swollen and tender joint counts (TJCs) were switched to open-label abatacept for an additional 28 weeks.19 All other participants remained in their randomized treatment arms until week 24 when they were switched to receive open-label abatacept for an additional 28 weeks.19
The primary endpoint was the ACR20 response at week 24.19 Key secondary endpoints included improvement in physical function, lack of radiographic progression, and improvement in ACR20 response in TNFi-exposed versus TNFi-naïve subpopulations.19 Additional secondary endpoints included ACR50 and ACR70 responses and ≥50% improvement in the Psoriasis Area and Severity Index (PASI50).19
The ASTRAEA study (Table 1) found that 39.4% of participants who received abatacept achieved the primary endpoint of ACR20 response at week 24 versus 22.3% of those who received placebo (P<0.001).19 After the open-label period from weeks 24 to 44, the ACR response rates of the placebo group became similar to the abatacept treatment arm.19 The efficacy of abatacept was sustained through the extension period.19 Approximately 60% of participants in both placebo and treatment arms had a history of TNFi exposure.19 When compared with placebo, less participants in the TNFi-exposed group (36.4 versus 22.3%, nominal P=0.012) achieved an ACR20 response than in the TNFi-naïve subpopulation (44.0 versus 22.2%, nominal P=0.003).19 Higher ACR20 responses were seen in those with baseline-elevated C-reactive protein (CRP) levels particularly in the TNFi-naïve subpopulation (50 versus 23.9% placebo).19
The first secondary endpoint tested in a prespecified hierarchical fashion was the HAQ-DI response defined by a ≥0.35 improvement from baseline HAQ-DI score by week 24.19 A HAQ-DI response was achieved in 31% of those in the abatacept arm compared to 23.7% in placebo group, P=0.097.19 This result did not reach statistical significance; consequently, statistical testing was not performed on the remaining secondary endpoints.19 Most other secondary endpoints trended higher for those receiving abatacept including improvements in the quality of life assessed by the short form (SF-36) physical component summary and in radiographic progression assessed by the PsA-modified Sharp–van der Heijde score at week 24.19
Abatacept in the treatment of enthesitis, dactylitis, and other disease manifestations
In the ASTRAEA study, abatacept recipients had slightly higher improvements in PsA disease activity composite measures such as the Minimal Disease Activity (MDA) score (11.7 versus 8.1%), the Psoriatic Arthritis Disease Activity Score (PASDAS) (-1.78 versus -1.48), and the modified Composite Psoriatic Disease Activity Index (CPDAI) (-1.80 versus -1.53) when compared with the placebo arm.19 There was also a higher proportion of those treated with abatacept who achieved complete resolution of enthesitis (32.9 versus 21.2%) and dactylitis (44.3 versus 34%) at week 24 when compared with placebo.19 Neither the Mease et al40 2011 study nor the ASTRAEA study evaluated the effect of abatacept on nail disease and axial disease. A small study published in 2011 by Lekpa et al41 evaluated the effects of abatacept in seven patients with a history of TNFi-resistant axial spondylitis (AS). There was no significant therapeutic benefit noted.41
Abatacept and plaque PSO
A 1999 open-label Phase I, 28-week study of CTLA-4–Ig use in patients with PSO vulgaris, found that 19 of the 41 of those receiving CTLA-4–Ig experienced an improvement in the physician’s global assessment of disease activity score at a minimum of 50%.42 Histopathology testing showed that CTLA-4–Ig decreased epidermal thickness, hyperplasia, and T-cell infiltration of psoriatic lesions.42 Surprisingly, in the ASTRAEA study, improvements in PSO, measured by the target lesion (TL) score and PASI response, were marginal when compared with placebo.40 In the abatacept treatment arm, 26.7% achieved a PASI50 response compared to 19.6% of the placebo arm, nominal P=0.137.19 When stratifying PASI50 response by the history of TNFi exposure, ~10% more TNFi-naïve patients (32.7 versus 19.6%) reached a PASI50 response at week 24 than the TNFi-exposed participants (23.1 versus 19.6%).19 Of the TNFi-naïve population, there was an 8.4% difference in those who achieved a PASI75 response when compared with placebo (18.2 versus 9.8%).19
In the Mease et al 2011 study, there were more participants who achieved a PASI50/75, TL50/75, and investigator’s global assessment response of “clear or almost clear” in the abatacept 3 mg/kg group than in any other treatment arm.40 At day 169, the greatest difference compared to placebo was seen in the PASI50 response of 43% in the 3 mg/kg treatment arm compared to 29% in the 10 mg/kg arm, 35% in the 30/10 mg/kg arm, and 14% of the placebo arm.40 Statistical analysis was not performed on these data.
Safety of abatacept
In reviewing the incidence of adverse events in both the 2011 and 2017 abatacept in PsA trials, there is an overall low risk of infection.19,40 In the 2017 ASTRAEA study, there was one incidence of Pneumocystis jirovecii pneumonia, a serious, opportunistic infection.19 The authors note that this participant had additional comorbidities including a history of tobacco use and chronic obstructive pulmonary disease (COPD) as well as recent use of high-dose glucocorticoids, which may have contributed to this development.19 In the Phase II abatacept study, one episode of osteomyelitis and gastroenteritis was classified as drug-related serious adverse infections.40
Most of the long-term data of abatacept are derived from RA trials. Safety analysis of 4149 patients who received IV abatacept found the cumulative incidence of serious infections to be 2.87 per 100 patient-years compared to 2.60 in RA comparator cohorts.43 Pneumonia, bronchitis, and urinary tract infections have been some of the most commonly reported serious infections.43,44 Most recommend tuberculosis (TB) screening prior to treatment initiation, although there is no clear risk of TB infection with abatacept.43 Observational studies have not found evidence that abatacept is directly teratogenic or carcinogenic.43–45 Antiabatacept antibodies have been found in a small number of patients treated with abatacept without any significant effect on drug tolerance or efficacy.46 In individuals with a history of COPD, abatacept has been associated with an increased risk of respiratory infections and COPD exacerbations.39 Abatacept should be used with caution in those with a history of recurrent infections, COPD, active pregnancy, or malignancy. Interestingly, data from RA patients estimate the development of treatment-related PSO at an incidence rate of <0.6 in those treated with abatacept.43,44
Discussion
In recent years, some experts have recommended that clinicians use a patient-specific, treat-to-target approach to achieve clinical remission and/or inactivity in PsA.47 With consideration of the PsA disease spectrum and data from two key RCTs, abatacept may be considered for the treatment of peripheral joint symptoms in individuals with PsA failing cDMARDs.19,40 The greatest improvements are likely to be seen in those who are TNFi naïve and have elevated CRP levels.19
A higher proportion of those who received IV abatacept at the standard RA dosing in the Mease et al 2011 study achieved the primary endpoint when compared with placebo (48 versus 19%) than those who received SQ abatacept in the ASTRAEA study (39.9 versus 22.3%).19,40 In comparing study populations, there were more participants in the ASTRAEA study who had PSO affecting ≥3% body surface area (BSA) at baseline (~70 versus ~20%) and a history of TNFi exposure (~60 versus ~38%) when compared with the Mease et al 2011 study.19,40 Baseline swollen joint count (SJC) and TJC were similar among the two studies along with the proportion of participants on concomitant MTX and/or systemic corticosteroid.19,40
The ACR20 response, defined as a 20% improvement in SJC and TJC as well as meeting three of the five ACR core measures, was originally created to assess disease activity in RA.48 The ACR20 response has since been adopted for use as a disease activity marker in PsA, serving as the primary endpoint in most major RCTs. In reviewing individual components of the ACR20 response, particularly the mean change in SJC and TJC, there were only modest improvements when compared with placebo although all components of the ACR20 response trended higher than placebo. The more stringent ACR50, defined by a 50% improvement in the ACR criteria, and ACR70, defined by a 70% improvement in ACR criteria, were key secondary endpoints of the ASTRAEA trial. Neither the total population nor the TNFi-exposed and TNFi-naïve subpopulations demonstrated a notable difference in the ACR50 and ACR70 responses when compared with placebo.19
Composite measures such as MDA, PASDAS, and CPDAI have been developed to provide a more comprehensive assessment of disease activity with the inclusion of various manifestations seen in PsA such as enthesitis and dactylitis. These composite measures were used as secondary endpoints in the ASTRAEA study, and by week 24, there were only modest improvements when compared with placebo.19 Similar small differences were seen in the resolution of enthesitis and dactylitis as well as in slowing radiographic progression in the abatacept treatment group.19
In the 2011 study by Mease et al, higher doses of abatacept did not produce a dose–response effect in the treatment of PSO.40 With the use of abatacept 125 mg SQ weekly, only minimal improvements in the PASI75 response were seen when compared with placebo.19 In the 1999 Phase I open-label trial by Abrams et al,42 CTLA-4–Ig at 25 and 50 mg/kg achieved higher improvements in PSO than in the lower doses used in this study. Of note, the administration of CTLA-4–Ig was given at a more frequent infusion schedule than what is currently approved for the treatment of PsA and RA.42 Higher doses of both IV and SQ abatacept may be needed to achieve greater clinical improvements in skin disease. Abatacept is not approved for the treatment of PSO at this time.
Abatacept treatment efficacy and PsA pathogenesis conclusions
Biologics targeting the TNF and IL-23/IL-17 pathways have been found to have the broadest therapeutic range across the spectrum of disease seen in PsA, including efficacy on AS and PSO.7,10 It is widely accepted that T cells are crucial in the pathogenesis of both PSO and PsA.28 A subset of T cells known as Th17 cells play a central role in mediating the inflammatory response, osteoproliferation, and keratinocyte proliferation through the secretion of IL-17 and IL-22.20,28 Inhibition of naïve T cells, the precursor cell to Th17 cells, failed to demonstrate similar broad efficacy as seen with the currently available IL-23/IL-17 pathway targets.28 One possible explanation is that abatacept use does not result in full T-cell inhibition. There are several other molecules that can activate T cells including lymphocyte function-associated antigen-1 (LFA-1), CD2, and CD6.18
A small 2017 study by Szentpetery et al33 of 15 biologic-naïve PsA patients who received IV abatacept found that there were notable improvements in musculoskeletal symptoms and minimal improvements in PSO. The researchers found that with abatacept use, expression of CD4-positive fork head box transcription factor (FOXP3)-positive Tregs was decreased in the synovium but not in psoriatic lesions of study patients.33 These findings support the notion that PsA and PSO have similar but divergent pathways driving disease activity, which are likely contributing to abatacept’s varied efficacy.
Abatacept’s effectiveness in comparison to other approved biologic drugs
The 2015 EULAR guidelines named TNFi(s) as the first-line biologic class of choice in the treatment of PsA.10 This recommendation was based on better defined long-term data and clinician familiarity.10 In the treatment of PsA, there are no head-to-head studies comparing drug-to-drug efficacy of abatacept with other available bDMARDs. An indirect comparative study published by Ungprasert et al49 found that there was a higher chance of achieving an ACR20 response with etanercept, infliximab, adalimumab, golimumab, and secukinumab compared to certolizumab, ustekinumab, and apremilast. Similarly, in 2017, a systematic review and network meta-analysis published in Rheumatology International comparing non-TNFi agents identified eight RCTs that provided data over a 16–24-week period.50 In both the overall and the TNFi-naïve populations, abatacept and secukinumab were considered more efficacious than both ustekinumab and apremilast.50 Abatacept and apremilast were considered the least efficacious for improvement in PSO; neither of these agents was superior to placebo for ACR20 responses in the TNFi-experienced populations.50 Both aforementioned studies were conducted prior to the publication of the ASTRAEA trial and the OPAL Broaden (tofacitinib) study; the latter was approved for the treatment of PsA in the United States in 2017.
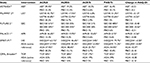
Table 1 lists data from key non-TNFi RCTs in the treatment of PsA including the results of the ASTRAEA and OPAL Broaden studies. Study outcomes such as ACR20/50, PASI75, and change in baseline HAQ-DI score met statistical significance in all drugs listed except for abatacept. It is important to note that unlike most studies in Table 1, the ASTRAEA study had a high proportion of participants with prior TNFi exposure, 60% of whom discontinued one or more TNFi drug(s) due to the lack of efficacy.19 In the TNFi-naïve subpopulation, abatacept still failed to produce a substantial difference in the ACR50 and ACR70 responses when compared with placebo.19 It appears that other available drugs may be more effective in producing more robust improvements in peripheral arthritis. Caution should be taken when comparing results from non-head-to-head RCTs given the varied patient population and study protocol of each trial.
In recent years, more bDMARDs have been approved for the treatment of PsA, and are in use in clinical practice. However, many patients fail to respond to the drugs, develop adverse events while receiving bDMARDs, and in some cases, the drugs lose efficacy after initial treatment, thus illustrating the need for a larger treatment arsenal. Molecular targets approved for RA and not currently approved for PsA include B-cell-, IL-1-, and IL-6-targeted biologics. Clazakizumab, an anti-IL-6 investigational drug, showed some promise in a 2016 Phase II RCT with improvements in PsA activity measures when compared with placebo.51 Small open-label studies with anti-IL-1 drug anakinra and anti-CD20 B-cell target rituximab have shown some small improvement in PsA.52,53 Neither abovementioned molecular targeted therapies are being pursued for use in the treatment of PsA at this time. The IL-23/IL-17 pathway continues to be the focus of future therapies for the treatment of PsA and PSO.
Conclusion
Abatacept is a potential treatment option for a select group of patients with PsA, particularly those with active peripheral arthritis. Although there were trends toward improvement in radiographic progression, enthesitis and dactylitis, abatacept had minimal effects on PSO and should not be first line in those with either moderate-to-severe skin involvement or active axial disease.19 Consideration should be given in these patients, particularly those who have failed prior TNF therapy, to newer agents such as secukinumab, ustekinumab, and tofacitinib.
Disclosure
MCH is a consultant to the Bristol Myers Squibb, Eli Lilly, EMD Serono, Flexion Therapeutics Inc., Galapagos, Genentech/Roche, IBSA Biotechniq SA, Innovative Sciences, Novartis Pharma AG, Pfizer Inc., Plexxikon, Samumed LLC, Symic Bio Inc., Theralogix LLC, TissueGene Inc., TLC Biopharmaceuticals, Inc., and Zynerba and has stock ownership in Theralogix LLC. The authors report no other conflicts of interest in this work.
References
Ogdie A, Weiss P. The epidemiology of psoriatic arthritis. Rheum Dis Clin North Am. 2015;41(4):545–568. | ||
Moll J, Wright V. Psoriatic arthritis. Semin Arthritis Rheum. 1973;3(1):55–78. | ||
Taylor W, Gladman D, Helliwell P, et al; CASPAR Study Group. Classification criteria for psoriatic arthritis development of new criteria from a large international study. Arthritis Rheum. 2006;54(8):2665–2673. | ||
Ash Z, Gaujoux-Viala C, Gossec L, et al. A systematic literature review of drug therapies for the treatment of psoriatic arthritis: current evidence and meta-analysis informing the EULAR recommendations for the management of psoriatic arthritis. Ann Rheum Dis. 2012;71(3):319–326. | ||
Gottlieb A, Korman NJ, Gordon KB, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis. Section 2. Psoriatic arthritis: overview and guidelines of care for treatment with an emphasis on the biologics. J Am Acad Dermatol. 2008;58(5):851–864. | ||
Kingsley GH, Kowalczyk A, Taylor H, et al. A randomized placebo-controlled trial of methotrexate in psoriatic arthritis. Rheumatology (Oxford). 2012;51(8):1368–1377. | ||
Coates LC, Kavanaugh A, Mease PJ, et al. Group for research and assessment of psoriasis and psoriatic arthritis 2015 treatment recommendations for psoriatic arthritis. Arthritis Rheumatol. 2016;68(5):1060–1071. | ||
Gossec L, Smolen JS, Gaujoux-Viala C, et al; European League against Rheumatism. European league against rheumatism recommendations for the management of psoriatic arthritis with pharmacological therapies. Ann Rheum Dis. 2012;71(1):4–12. | ||
Fagerli KM, Lie E, Van Der Heijde D, et al. Switching between TNF inhibitors in psoriatic arthritis: data from the NOR-DMARD study. Ann Rheum Dis. 2013;72(11):1840–1844. | ||
Gossec L, Smolen JS, Ramiro S, et al. European League Against Rheumatism (EULAR) recommendations for the management of psoriatic arthritis with pharmacological therapies: 2015 update. Ann Rheum Dis. 2016;75(3):499–510. | ||
McInnes IB, Mease PJ, Kirkham B, et al; FUTURE 2 Study Group. Secukinumab, a human anti-interleukin-17A monoclonal antibody, in patients with psoriatic arthritis (FUTURE 2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2015;386(9999):1137–1146. | ||
Kavanaugh A, Mease PJ, Gomez-Reino JJ, et al. Treatment of psoriatic arthritis in a phase 3 randomised, placebo-controlled trial with apremilast, an oral phosphodiesterase 4 inhibitor. Ann Rheum Dis. 2014;73(6):1020–1026. | ||
McInnes IB, Kavanaugh A, Gottlieb AB, et al; PSUMMIT 1 Study Group. Efficacy and safety of ustekinumab in patients with active psoriatic arthritis: 1 year results of the phase 3, multicentre, double-blind, placebo-controlled PSUMMIT 1 trial. Lancet. 2013;382(9894):780–789. | ||
Coates LC, Gossec L, Ramiro S, et al. New GRAPPA and EULAR recommendations for the management of psoriatic arthritis. Rheumatology (Oxford). 2017;56(8):1251–1253. | ||
Gossec L, Coates LC, De Wit M, et al. Management of psoriatic arthritis in 2016: a comparison of EULAR and GRAPPA recommendations. Nat Rev Rheumatol. 2016;12(12):743–750. | ||
Lories RJ, De Vlam K. Is psoriatic arthritis a result of abnormalities in acquired or innate immunity? Curr Rheumatol Rep. 2012;14(4):375–382. | ||
Benham H, Norris P, Goodall J, et al. Th17 and Th22 cells in psoriatic arthritis and psoriasis. Arthritis Res Ther. 2013;15(5):R136. | ||
Dhawale R, Moreland LW. T-cell co-stimulation. In: Hochberg MC, Silman AJ, Smolen JS, Weinblatt ME, Weisman MH, editors. Rheumatology. 5th ed. Philadelphia, PA: Elsevier; 2011:557–562. | ||
Mease PJ, Gottlieb AB, van der Heijde D, et al. Efficacy and safety of abatacept, a T-cell modulator, in a randomised, double-blind, placebo-controlled, phase III study in psoriatic arthritis. Ann Rheum Dis. 2017;76(9):1550–1558. | ||
Ritchlin CT, Colbert RA, Gladman DD. Psoriatic arthritis. N Engl J Med. 2017;376(10):957–970. | ||
Menon B, Gullick NJ, Walter GJ, et al. Interleukin-17+CD8+ T cells are enriched in the joints of patients with psoriatic arthritis and correlate with disease activity and joint damage progression. Arthritis Rheumatol. 2014;66(5):1272–1281. | ||
Raychaudhuri SK, Saxena A, Raychaudhuri SP. Role of IL-17 in the pathogenesis of psoriatic arthritis and axial spondyloarthritis. Clin Rheumatol. 2015;34(6):1019–1023. | ||
Raychaudhuri SP, Raychaudhuri SK, Genovese MC. IL-17 receptor and its functional significance in psoriatic arthritis. Mol Cell Biochem. 2012;359(1–2):419–429. | ||
Mease PJ, McInnes IB, Kirkham B, et al; FUTURE 1 Study Group. Secukinumab inhibition of interleukin-17A in patients with psoriatic arthritis. N Engl J Med. 2015;373(14):1329–1339. | ||
Mease PJ, Van Der Heijde D, Ritchlin CT, et al; SPIRIT-P1 Study Group. Ixekizumab, an interleukin-17A specific monoclonal antibody, for the treatment of biologic-naïve patients with active psoriatic arthritis: results from the 24-week randomised, double-blind, placebo controlled and active (adalimumab)-controlled period of the phase III trial SPIRIT-P1. Ann Rheum Dis. 2017;76(1):79–87. | ||
Ritchlin C, Rahman P, Kavanaugh A, et al; PSUMMIT 2 Study Group. Efficacy and safety of the anti-IL-12/23 p40 monoclonal antibody, ustekinumab, in patients with active psoriatic arthritis despite conventional non-biological and biological anti-tumour necrosis factor therapy: 6-month and 1-year results of the phase 3, multicentre, double-blind, placebo-controlled, randomised PSUMMIT 2 trial. Ann Rheum Dis. 2014;73(6):990–999. | ||
Goedkoop AY, Kraan MC, Teunissen MBM, et al. Early effects of tumour necrosis factor alpha blockade on skin and synovial tissue in patients with active psoriasis and psoriatic arthritis. Ann Rheum Dis. 2004;63(7):769–773. | ||
Boutet MA, Nerviani A, Gallo Afflitto G, Pitzalis C. Role of the IL-23/IL-17 axis in psoriasis and psoriatic arthritis: the clinical importance of its divergence in skin and joints. Int J Mol Sci. 2018;19(2):E530. | ||
Mease PJ, Gladman DD, Keystone EC, Alefacept in Psoriatic Arthritis Study Group. Alefacept in combination with methotrexate for the treatment of psoriatic arthritis: results of a randomized, double-blind, placebo-controlled study. Arthritis Rheum. 2006;54(5):1638–1645. | ||
Iannone F, Lapadula G. The inhibitor of costimulation of T cells: abatacept. J Rheumatol Suppl. 2012;89:100–102. | ||
Kremer JM, Westhovens R, Leon M, et al. Treatment of rheumatoid arthritis by selective inhibition of T-cell activation with fusion protein CTLA4Ig. N Engl J Med. 2003;349(20):1907–1915. | ||
Genovese MC, Becker J-C, Schiff M, et al. Abatacept for rheumatoid arthritis refractory to tumor necrosis factor alpha inhibition. N Engl J Med. 2005;353(11):1114–1123. | ||
Szentpetery A, Heffernan E, Gogarty M, et al. Abatacept reduces synovial regulatory T-cell expression in patients with psoriatic arthritis. Arthritis Res Ther. 2017;19(1):158. | ||
Bathon J, Robles M, Ximenes AC, et al. Sustained disease remission and inhibition of radiographic progression in methotrexate-naïve patients with rheumatoid arthritis and poor prognostic factors treated with abatacept: 2-year outcomes. Ann Rheum Dis. 2011;70(11):1949–1956. | ||
Ruperto N, Lovell DJ, Quartier P, et al; Paediatric Rheumatology INternational Trials Organization; Pediatric Rheumatology Collaborative Study Group. Abatacept in children with juvenile idiopathic arthritis: a randomised, double-blind, placebo-controlled withdrawal trial. Lancet. 2008;372(9636):383–391. | ||
Kremer JM, Genant HK, Moreland LW, et al. Effects of abatacept in patients with methotrexate-resistant active rheumatoid arthritis: a randomized trial. Ann Intern Med. 2006;144(12):865–876. | ||
Keystone EC, Kremer JM, Russell A, et al. Abatacept in subjects who switch from intravenous to subcutaneous therapy: results from the phase IIIb ATTUNE study. Ann Rheum Dis. 2012;71(6):857–861. | ||
Genovese MC, Covarrubias A, Leon G, et al. Subcutaneous abatacept versus intravenous abatacept: a phase IIIb noninferiority study in patients with an inadequate response to methotrexate. Arthritis Rheum. 2011;63(10):2854–2864. | ||
Weinblatt M, Combe B, Covucci A, Aranda R, Becker JC, Keystone E. Safety of the selective costimulation modulator abatacept in rheumatoid arthritis patients receiving background biologic and nonbiologic disease-modifying antirheumatic drugs: a one-year randomized, placebo-controlled study. Arthritis Rheum. 2006;54(9):2807–2816. | ||
Mease P, Genovese MC, Gladstein G, et al. Abatacept in the treatment of patients with psoriatic arthritis: results of a six-month, multicenter, randomized, double-blind, placebo-controlled, phase II trial. Arthritis Rheum. 2011;63(4):939–948. | ||
Lekpa FK, Farrenq V, Canouï-Poitrine F, et al. Lack of efficacy of abatacept in axial spondylarthropathies refractory to tumor-necrosis-factor inhibition. Joint Bone Spine. 2012;79(1):47–50. | ||
Abrams JR, Lebwohl MG, Guzzo CA, et al. CTLA4Ig-mediated blockade of T-cell costimulation in patients with psoriasis vulgaris. J Clin Invest. 1999;103(9):1243–1252. | ||
Weinblatt ME, Moreland LW, Westhovens R, et al. Safety of abatacept administered intravenously in treatment of rheumatoid arthritis: integrated analyses of up to 8 years of treatment from the abatacept clinical trial program. J Rheumatol. 2013;40(6):787–797. | ||
Alten R, Kaine J, Keystone E, Nash P, Delaet I, Genovese MC. Long-term safety of subcutaneous abatacept in rheumatoid arthritis: integrated analysis of clinical trial data representing more than four years of treatment. Arthritis Rheumatol. 2014;66(8):1987–1997. | ||
Kumar M, Ray L, Vemuri S, Simon TA. Pregnancy outcomes following exposure to abatacept during pregnancy. Semin Arthritis Rheum. 2015;45(3):351–356. | ||
Nash P, Nayiager S, Genovese MC, et al. Immunogenicity, safety, and efficacy of abatacept administered subcutaneously with or without background methotrexate in patients with rheumatoid arthritis: results from a phase III, international, multicenter, parallel-arm, open-label study. Arthritis Care Res. 2013;65(5):718–728. | ||
Smolen JS, Schöls M, Braun J, et al. Treating axial spondyloarthritis and peripheral spondyloarthritis, especially psoriatic arthritis, to target: 2017 update of recommendations by an international task force. Ann Rheum Dis. 2017;77(1):3–17. | ||
Felson DT, Anderson JJ, Boers M, et al. American College of Rheumatology preliminary definition of improvement in rheumatoid arthritis. Arthritis Rheum. 1995;38(6):727–735. | ||
Ungprasert P, Thongprayoon C, Davis JM. Indirect comparisons of the efficacy of biological agents in patients with psoriatic arthritis with an inadequate response to traditional disease-modifying anti-rheumatic drugs or to non-steroidal anti-inflammatory drugs: a meta-analysis. Semin Arthritis Rheum. 2016;45(4):428–438. | ||
Kawalec P, Holko P, Moćko P, Pilc A. Comparative effectiveness of abatacept, apremilast, secukinumab and ustekinumab treatment of psoriatic arthritis: a systematic review and network meta-analysis. Rheumatol Int. 2017;38(2):189–201. | ||
Mease PJ, Gottlieb AB, Berman A, et al. The efficacy and safety of clazakizumab, an anti-interleukin-6 monoclonal antibody, in a phase IIb study of adults with active psoriatic arthritis. Arthritis Rheumatol. 2016;68(9):2163–2173. | ||
Jung N, Hellmann M, Hoheisel R, et al. An open-label pilot study of the efficacy and safety of anakinra in patients with psoriatic arthritis refractory to or intolerant of methotrexate (MTX). Clin Rheumatol. 2010;29(10):1169–1173. | ||
Jimenez-Boj E, Stamm TA, Sadlonova M, et al. Rituximab in psoriatic arthritis: an exploratory evaluation. Ann Rheum Dis. 2012;71(11):1868–1871. | ||
Mease P, Hall S, FitzGerald O, et al. Tofacitinib or adalimumab versus placebo for psoriatic arthritis. N Engl J Med. 2017;377(16):1537–1550. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.