Back to Journals » International Journal of General Medicine » Volume 17
A Three-Year Cross-Sectional Analysis of Depression, Anxiety, and Quality of Life in Patients with Post-COVID-19 Syndrome
Authors Bota AV, Bogdan I, Razvan DV, Ilie AC, Tudor R , Indries MF, Csep AN, Marincu I
Received 4 December 2023
Accepted for publication 24 February 2024
Published 5 March 2024 Volume 2024:17 Pages 751—762
DOI https://doi.org/10.2147/IJGM.S453247
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Redoy Ranjan
Adrian Vasile Bota,1,2 Iulia Bogdan,1– 3 David Vladut Razvan,1,2 Adrian Cosmin Ilie,4 Raluca Tudor,5 Mirela Florica Indries,6 Andrei Nicolae Csep,6 Iosif Marincu1
1Methodological and Infectious Diseases Research Center, Department of Infectious Diseases, “Victor Babes” University of Medicine and Pharmacy, Timisoara, 300041, Romania; 2Doctoral School, “victor Babes” University of Medicine and Pharmacy Timisoara, Timisoara, 300041, Romania; 3Department of Infectious Diseases, “Victor Babes” University of Medicine and Pharmacy Timisoara, Timisoara, 300041, Romania; 4Department III Functional Sciences, Division of Public Health and Management, “Victor Babes” University of Medicine and Pharmacy Timisoara, Timisoara, 300041, Romania; 5Second Discipline of Neurology, “victor Babes” University of Medicine and Pharmacy Timisoara, Timisoara, 300041, Romania; 6Department of Psycho-Neuroscience and Recovery, University of Oradea, Faculty of Medicine and Pharmacy, Oradea, 410087, Romania
Correspondence: Raluca Tudor; Andrei Nicolae Csep, Email [email protected]; [email protected]
Background: This study explores the longitudinal psychosocial impact of Long-COVID syndrome, also known as Post-COVID-19 syndrome, characterized by enduring symptoms after coronavirus disease (COVID-19) infection, over the years 2020, 2021, and 2022. It aimed to examine the variations in depression, anxiety, and quality of life among Post-COVID-19 patients during these years, hypothesizing significant inter-year differences reflecting the pandemic’s evolving influence.
Methods: Conducted at Victor Babes Hospital for Infectious Diseases and Pulmonology, Romania, this cross-sectional research involved 324 patients diagnosed with mild to moderate COVID-19, assessed six months post-hospitalization. Standardized instruments, namely Short Form (SF-36) for quality of life, Generalised Anxiety Disorder Assessment (GAD-7) for anxiety, and Patient Health Questionnaire (PHQ-9) for depression, were utilized.
Results: The study observed a consistent average patient age of around 55 years across the years. A notable increase in COVID-19 vaccination rates was recorded, rising from 20.9% in 2020 to over 70% in 2022 (p< 0.001). Trends in key post-COVID symptoms like fatigue and cognitive issues varied over the years. Importantly, there was a consistent decrease in feelings of sadness or depression, with scores declining from 7.3 in 2020 to 4.8 in 2022 (p< 0.001). The SF-36 survey indicated a steady improvement in overall health, reaching 55.8± 7.1 in 2022 (p=0.035). Both GAD-7 and PHQ-9 scores showed significant reductions in anxiety and depression over the years, with p-values of 0.030 and 0.031, respectively. Factors such as smoking status, substance use, and the initial severity of COVID-19 infection were significantly associated with depression levels.
Conclusion: The findings suggest that despite persistent physical symptoms, Long-COVID patients experienced enhancements in mental well-being and quality of life over the studied period. The increasing vaccination rates might have contributed to this improvement. Addressing modifiable risk factors like smoking and substance use could further optimize post-COVID care and mental health outcomes.
Keywords: SARS-CoV-2, COVID-19, long-COVID, quality of life, post, acute COVID
Introduction
The novel severe-acute-respiratory-syndrome-related coronavirus (SARS-CoV-2) emerged in late 2019 and rapidly evolved into a global pandemic. Beyond the immediate health implications and mortality rates associated with the acute phase of the virus, a significant portion of individuals who recover from the initial infection1 continue to experience lingering symptoms, commonly referred to as “Long-COVID” or “Post-COVID” Syndrome.2–6 Other studies highlight the challenge of diagnosing individuals who have not received a confirmed SARS-CoV-2 diagnosis, complicating the understanding and treatment of “long-haulers”. Moreover, these studies underscore the importance of recognizing both intrinsic and extrinsic factors, along with the impact of hospitalization, in influencing the progression and persistence of post-COVID symptoms.7,8
Historically, viral pandemics have not only posed immediate threats but have also been accompanied by longer-term health implications. The nature and course of these post-viral syndromes often remain elusive and are subject to ongoing research.9–11 With coronavirus disease (COVID-19), initial evidence suggests that Long-COVID symptoms can encompass a wide range of health issues, with neurological and psychological manifestations being among the most frequently reported.12–14
The relationship between post-infectious syndromes and mental health conditions such as depression and anxiety are not novel. For example, after the SARS outbreak in 2003, a significant number of survivors exhibited psychiatric morbidities and compromised quality of life even years post-recovery.15,16 With the significantly higher global impact of COVID-19, there’s an urgent need to understand the scale and scope of the vast domains of psychological and quality of life impacts on patients experiencing Post-COVID syndrome.17,18
As the pandemic progressed, differences in healthcare approaches, public health strategies, and the emergence of new SARS-CoV-2 variants each year might have influenced the prevalence and nature of Long-COVID symptoms.19,20 Time-sensitive analyses focused on various facets of the COVID-19 pandemic showed significant variations in clinical features and patients demographics. Moreover, specifically focusing on the variations in psychological aspects related to COVID-19, the study of depression, anxiety, and quality of life across three consecutive pandemic years, can offer valuable insights in-to the evolving nature of Long-COVID and its psychosocial ramifications.
This study seeks to elucidate the variations in depression, anxiety, and quality of life among patients diagnosed with Long-COVID Syndrome over three distinct years of the pandemic. We hypothesize that there will be significant differences in the manifestation and severity of these symptoms across the three evaluated years. Our primary objectives include identifying the prevalence of these symptoms in each year, determining the factors contributing to any observed differences, and understanding the broader implications for long-term healthcare strategies for Post-COVID care.
Materials and Methods
Research Design and Ethical Considerations
The study adopted a cross-sectional research design to evaluate depression, anxiety, and quality of life among Long-COVID patients spanning three years of the pandemic (2020, 2021, and 2022). This approach aimed to assess potential variations and correlations over these distinct periods, possibly reflecting the evolving nature of the pandemic and its impacts on patient health. All participants were sourced from the Victor Babes Hospital for Infectious Diseases and Pulmonology in Timisoara, Romania. The research strictly followed the ethical guidelines and obtained clearance from the Local Commission of Ethics for Scientific Research, ensuring compliance with the EU GCP Directives 2005/28/EC, ICH guidelines, and the Declaration of Helsinki (11,834/26 November 2021). Our study has been structured to adhere closely to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.21
Inclusion Criteria and Definitions
Potential participants, diagnosed with mild to moderate COVID-19, were shortlisted in collaboration with attending physicians. All participants provided informed consent before enrolling in the study. To be eligible, participants had to be adults (18 years and above) and surveyed six months after their hospitalization for SARS-CoV-2 infection. Severe cases were excluded to remove confounding variables from our results. Each year of the study sought a number of 80 participants to guarantee a robust sample size. Patients lacking explicit consent, those with a history of chronic respiratory or psychiatric ailments, and those submitting incomplete survey responses were excluded. For clarity, Post-COVID Syndrome or Long-COVID refers to persisting symptoms that last beyond four weeks from the initial onset, despite evidence suggesting SARS-CoV-2 viral replication cessation, as defined by the Center for Disease Control (CDC).22
The decision to focus on adults diagnosed with mild to moderate COVID-19 and surveyed six months post-hospitalization was informed by existing literature highlighting the relevance of this period in capturing the long-term impacts of the virus.23 This timeframe and patient severity categorization were chosen based on evidence suggesting their significant likelihood of experiencing persistent post-COVID symptoms. Severe cases were excluded to reduce heterogeneity and potential confounding effects related to the intensity of acute care received. The criteria were designed to ensure the study’s focus remained on understanding the quality of life, depression, and anxiety among long-COVID patients without the confounding influence of pre-existing chronic conditions or severe acute illness.
Variables
Each patient’s data encompassed age, gender, socio-economic background, and medical history. The core focus was on their quality of life, mental health status, specifically depression and anxiety, and the possible differences in these parameters across the three evaluated years. All collected data were anonymized according to European Union General Data Protection Regulations.
Surveys Employed
To holistically assess the participants’ experiences, three widely recognized tools, validated in Romanian, were administered online. The Short Form (SF-36) Health Survey24 was used to measure the quality of life, encompassing eight scales: physical functioning, role limitations due to physical health, pain, general health, energy/fatigue, social functioning, role limitations due to emotional health, and emotional well-being. For assessment of anxiety and depression, the GAD-7 (Generalized Anxiety Disorder 7-item scale)25 and PHQ-9 (Patient Health Questionnaire-9) were used respectively.26 The GAD-7 quantifies anxiety symptoms, and the PHQ-9 evaluates the severity of depressive symptoms. Besides these standardized tools, supplementary questions were incorporated to understand the specific COVID-19 experiences of each patient, capturing details on symptoms, hospitalization, and post-recovery health status.
The SF-36 Health Survey does not have specific cutoff values, being a descriptive tool used to assess various dimensions of health-related quality of life. Scores from each of the eight domains range from 0 to 100, with higher scores indicating better health status or less disability. The GAD-7 has the following cutoff values for assessing the severity of anxiety symptoms: 0–4: Minimal anxiety; 5–9: Mild anxiety; 10–14: Moderate anxiety; 15–21: Severe anxiety. The PHQ-9 has cutoff values for assessing the severity of depressive symptoms: 0–4: Minimal or none; 5–9: Mild depression; 10–14: Moderate depression; 15–19: Moderately severe depression; 20–27: Severe depression.
To address the concern regarding methodological bias in our cross-sectional study, we implemented several strategies. We minimized selection bias by employing a consecutive sampling technique for recruiting participants from the Victor Babes Hospital for Infectious Diseases and Pulmonology in Timisoara, Romania, ensuring that all eligible patients during the study period were considered. Information bias was addressed through the standardized administration of validated questionnaires (SF-36, GAD-7, PHQ-9) by trained personnel, and by employing a rigorous data entry and validation process to ensure accuracy in the collected data. Confounding factors were identified a priori, and statistical adjustments were made during analysis through multivariate regression techniques to control for potential confounders such as age, gender, socio-economic status, and baseline health status.
Statistical Analysis
Data management and analysis were conducted utilizing the statistical software SPSS version 26.0 (SPSS Inc., Chicago, IL, USA). The sample size was calculated based on a convenience sampling method, with a minimum of 180 respondents at a 95% confidence level and 10% margin of error. Continuous variables were represented as mean ± standard deviation (SD), while categorical variables were expressed in terms of frequencies and percentages. To analyze the changes between more than two means of continuous variables, the ANOVA test was utilized. The Chi-square test was utilized for the categorical variables. A multivariate regression analysis evaluated the depression risk. A p-value threshold of less than 0.05 was set for statistical significance. All results were double-checked to ensure accuracy and reliability.
Results
Background Characteristics
The background characteristics of patients across the three years (2020, 2021, and 2022) were compared. In 2020, a total of 86 patients participated, while 102 and 136 patients were part of the study in 2021 and 2022, respectively. Upon analyzing the age distribution, the mean age was observed to be around 55 years among all three years. However, the age variations among the three years were not statistically significant. The Body Mass Index (BMI) of the participants did not show any significant difference across the years, with mean values of 24.5, 25.1, and 24.8 for the respective years and a p-value of 0.768.
The proportion of participants who reported smoking was consistent across the years, with 20.9% in 2020, 21.6% in 2021, and 22.1% in 2022, yielding a p-value of 0.990, indicating no significant difference. Similarly, occasional alcohol use was reported by 58.1%, 58.8%, and 55.9% of the participants in 2020, 2021, and 2022, respectively, with a p-value of 0.943. Substance use saw a noticeable increase from 9.3% in 2020 to 17.6% in 2022, although this rise was not statistically significant with a p-value of 0.319. The majority of the participants across all three years hailed from urban areas, constituting around 65% of the sample.
In terms of education, there was a diverse representation across the years with no significant differences (p-value: 0.322). High school, college, and university-educated participants were fairly evenly distributed. However, there was a significant increase in COVID-19 vaccinations from 20.9% in 2020 to over 70% in 2022, with a p-value of <0.001, indicating a highly significant increase in vaccination rates over the years. The Charlson Comorbidity Index (CCI >2) and the relationship status (single) of participants did not exhibit significant differences over the three years. Meanwhile, there was a noticeable shift in COVID-19 severity from mild to moderate over the years, but this change was marginally above the threshold for statistical significance with a p-value of 0.106, as described in Table 1.
 |
Table 1 Background Characteristics |
COVID-19 Outcomes
In the analysis presented in Table 2, fatigue or tiredness post-COVID diagnosis was notably more pronounced in 2020, with patients reporting an average score of 8.2. This trend showed a gradual decline in the subsequent years, settling at 7.3 in 2021 and further to 5.6 by 2022 (p<0.001). Cognitive challenges, such as experiencing brain fog or memory issues, exhibited a fluctuating trend across the years. While 2020 recorded a mean score of 6.2, this dropped to 4.5 in 2021. However, by 2022, a surge was observed, with the score increasing to 7.4 (p<0.001). Shortness of breath and other respiratory challenges post-recovery were also noteworthy, with the scores decreasing consecutively across the years: 7.8 in 2020, 6.7 in 2021, and reaching 5.1 by 2022 (p<0.001).
 |
Table 2 Unstandardized Survey Results to Assess Post-COVID Symptoms and Complications |
In terms of the emotional impact, feelings of sadness, hopelessness, or depression affecting daily life post-COVID-19 showed a clear decreasing pattern over the three years. The score started at 7.3 in 2020 and declined to 6.1 in 2021 and further to 4.8 by 2022 (p<0.001). When assessing their current mental well-being in comparison to the pre-COVID period, patients reported a decline over the years: from a score of 6.5 in 2020 to 5.5 in 2021 and further dipping to 4.3 by 2022 (p<0.001). Interestingly, regarding persistent heart-related symptoms post-recovery, an opposite trend was evident. Starting from a score of 4.6 in 2020, there was an increase to 5.8 in 2021 and further to 6.9 by 2022 (p<0.001).
Analysis of Standardized Surveys
The Physical component of the SF-36 survey revealed a progressively improving trend over the pandemic years. In 2020, participants reported a mean score of 50.6±6.0, which slightly rose to 52.1±5.7 in 2021. The year 2022 witnessed a more pronounced enhancement in the physical health status with a score of 55.8±6.4. The observed differences across the three years were statistically significant, as indicated by a p-value of less than 0.001. Similarly, the Mental component of the SF-36 survey exhibited an improvement across the years. Participants in 2020 had a mean score of 51.4±5.3. This score experienced a modest increase in 2021 to 52.8±7.0, and further ascended to 55.0±6.2 in 2022. These year-to-year changes in mental health status were significant, with a p-value of 0.012. Taking into consideration the Total score of the SF-36 survey, which encapsulates both physical and mental health status, a gradual rise was evident. The score was 52.5±6.8 in 2020, increased slightly to 53.7±6.2 in 2021, and reached 55.8±7.1 in 2022. The statistical significance of this overall progression was confirmed with a p-value of 0.035, as seen in Table 3 and Figure 1.
 |
Table 3 SF-36 Survey Results Stratified by COVID-19 Pandemic Years |
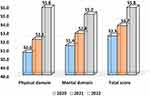 |
Figure 1 Analysis of the SF-36 questionnaire results during the COVID-19 pandemic. |
The GAD-7, which measures symptoms of General Anxiety Disorder, exhibited a de-cline in scores across the years, indicative of diminishing anxiety symptoms among the participants. In 2020, participants registered a mean score of 7.4±2.1. This slightly decreased to 6.9±3.4 in 2021 and further descended to 6.0±2.7 in 2022. The overall downward trajectory in the GAD-7 scores from 2020 to 2022 was statistically significant, with a p-value of 0.030, suggesting that patients might be experiencing reduced anxiety symptoms over the pandemic years.
Similarly, the PHQ-9 survey, which gauges depression symptoms, also presented a reducing trend. Participants in 2020 recorded a mean score of 5.1±1.8, which underwent a marginal decrease to 4.8±2.0 in 2021. The score was observed to further drop to 4.2±1.7 in 2022. The difference in PHQ-9 scores from 2020 to 2022 was significant, evidenced by a p-value of 0.031, as described in Table 4 and Figure 2. This indicates that the severity of depression symptoms among patients seemed to lessen over the three years.
 |
Table 4 GAD-7 and PHQ-9 Survey Results Stratified by COVID-19 Pandemic Years |
 |
Figure 2 Analysis of the GAD-7 and PHQ-9 questionnaire results during the COVID-19 pandemic. |
Analyzing Table 5, age showed a slight association with depression, having an odds ratio (OR) of 1.03. However, the confidence interval (CI) spanning from 0.98 to 1.08, combined with a p-value of 0.187, suggests that this relationship was not statistically meaningful. In contrast, BMI did not present a significant positive association with depression. Another determinant that emerged as significant was the current smoking status. Patients who reported current smoking exhibited a heightened risk for depression, as evidenced by an OR of 1.45 and a p-value of 0.005. Similarly, substance use also emerged as a notable factor, showing an OR of 1.38 and a significant p-value of 0.006. Interestingly, as anticipated, the severity of the COVID-19 disease was significantly associated with de-pression. Patients with more severe COVID-19 symptoms displayed an OR of 1.29, supported by a p-value of 0.002.
 |
Table 5 Regression Analysis for Depression Determinants Based on the PHQ-9 |
A pivotal finding from the table was the relationship between the SF-36 scores and depression. Both physical and mental scores from the SF-36 survey were inversely related to depression. Higher physical scores, with an OR of 0.93 and a p-value of 0.011, and higher mental scores, with an OR of 0.90 and a more pronounced p-value of 0.001, were associated with reduced depression risks. Lastly, examining the role of anxiety, the GAD-7 score, which represents symptoms of anxiety, exhibited a strong correlation with depression. The OR was a no Table 1. 45, and the p-value was less than 0.001, underlining its significance, as seen in Figure 3. Three other independent variables, namely fatigue post-COVID diagnosis, feelings of sadness post-COVID-19, and the evaluation of one’s mental well-being after COVID, also manifested strong, statistically significant relationships with depression.
 |
Figure 3 Regression analysis results. |
Discussion
The transition from 2020 to 2022 brought forth remarkable insights into the lives of patients grappling with Long-COVID Syndrome. The uniformity in age distribution and BMI over these years ensures that these fundamental variables likely did not introduce ex-ternal variability into our observations related to mental health and quality of life. Within this stable demographic framework, the study delved into understanding the pandemic variations in depression, anxiety, and overall quality of life, especially as they manifested six months post-hospital discharge.
Noteworthy is the pronounced decline in fatigue or tiredness post-COVID diagnosis from 2020 to 2022. This suggests a potential adaptability or perhaps medical interventions over time that could be aiding in alleviating some of the intense fatigue experienced by patients initially, or the fact that all restrictions have been completely removed by 2023 and people can be more active.27–29 On the other hand, cognitive challenges exhibited a seesaw pattern, with a significant rise again by 2022. This inconsistency might be indicative of the complex and multifaceted nature of Long-COVID’s impact on cognitive functioning, as other recent studies reporting increasing incidence of neurologic symptoms after COVID-19, with brain fogginess reaching as high as 50% of those affected by Long-COVID.30,31 Concurrently, the consecutive decrease in respiratory challenges post-recovery across the years is promising, potentially hinting at better post-COVID respiratory care or natural improvement over time, as well as the recent development of cardiopulmonary rehabilitation techniques.32–34
From an emotional perspective, the marked decrease in feelings of sadness, hopelessness, or depression affecting daily life is encouraging. This trend might reflect the resilience of the human spirit, the effectiveness of coping mechanisms, or improved support systems as the pandemic progressed, concurrently with the feeling of hope after the vaccination campaign and the pandemic reaching to an end.35–37 Correspondingly, the decline in scores related to overall mental well-being from 2020 to 2022 raises concerns. It suggests that while acute symptoms of sadness might be waning, there’s an overarching sentiment of worsened mental well-being post-COVID compared to pre-COVID times.
The observed enhancement in both the physical and mental components of the SF-36 survey across the pandemic years is striking. It suggests that despite the prolonged battle with Long-COVID, patients’ perception of their physical and mental health seems to be on an upward trajectory. However, heart-related post-recovery symptoms paint a contrasting story, with a consistent increase over the years, with approximately 20% of Long-COVID patients accusing feelings of chest pain, palpitations and dyspnea.38 This underlines the need for ongoing cardiovascular monitoring in patients with Long-COVID.
Moreover, diving into the intricate relationship between depression and various determinants, several factors stood out. Smoking status and substance use, both showing statistically significant higher rates in patients with depressive symptoms, indicating their potential roles as exacerbating factors for depression among Long-COVID patients.39,40 The inverse relationship between SF-36 scores and depression underscores the intertwined nature of physical and mental health. The connection between heightened anxiety symptoms (GAD-7 score) and depression further reaffirms the complex interplay between these two conditions in the backdrop of Long-COVID.
In other recent studies, various psychiatric symptoms were identified among Long COVID patients. Anxiety was observed with a prevalence between 7% and up to almost 50%,41,42 while depression was noted with a prevalence ranging from 4.4% to 35.9%.43 Other identified symptoms included PTSD, sleep disturbances, somatic symptoms, cognitive deficits, and obsessive-compulsive disorder, with prevalence rates going up to as much as 70%.43 These findings were assessed using a range of validated questionnaires, including the GAD-7 for anxiety, PHQ-9 for depression, and PSQI for sleep disturbances, similarly to our study.
Regression analyses in the recent literature identified multiple risk factors for depression in Long-COVID patients. Being female was commonly associated with depression,44 though a few studies found no gender correlation.43 Young age was identified as a significant risk factor in one study, even though in our study age was not a statistically significant risk factor for depression in Long-COVID patients.45 Other factors linked to depression included a medical history of psychiatric diagnoses, certain laboratory results like elevated IL-6 levels, and specific COVID-19 related experiences, such as loss of family members to the virus and hospitalization.46 Multivariate analysis further pinpointed being female, prior psychiatric diagnosis, and initial post-infection depression as key risk factors.43
Even though depressive symptoms and depression are key aspects of mental health status, anxiety plays another significant role in COVID-19 patients. For anxiety, recent studies found that being female and younger age emerged as notable risk factors, with most studies confirming the former.47 However, one study found no gender correlation with anxiety.48 Factors like previous psychiatric diagnoses and specific COVID-19 experiences, including personal perception of disease severity and having family members infected, were also related to anxiety.47 Furthermore, various non-significant risk factors for psychiatric symptoms, such as marital status and duration of hospital stay, were also reported, although not in the current study.49
The COVID-19 pandemic also impacted significant gender-specific challenges encountered during home quarantine. Kaplan’s findings,50 revealed heightened levels of burnout and loneliness among housewives, underscore the compounded stress due to increased domestic responsibilities, with little change in the distribution of household labor. This research is pivotal in contextualizing the broader health outcomes observed in our study, emphasizing the nuanced vulnerabilities women face, particularly those adhering to traditional domestic roles. By juxtaposing these findings with our data, we underscore the necessity of addressing gender-specific factors in pandemic response strategies to mitigate the long-term psychological effects on distinct demographic groups.
The observed improvements in mental well-being and quality of life among Long-COVID patients over the years, despite the persistence of physical symptoms, underscore a critical avenue for healthcare providers. Given the documented stress and dissatisfaction among clinicians during the COVID-19 period due to prolonged exposure to stressful situations,51,52 our study’s insights can inform strategies to mitigate these challenges. Specifically, adopting emotional intelligence in patient care, as strongly recommended, can be a transformative approach for healthcare professionals in managing Post-COVID conditions. This involves recognizing and addressing the emotional and psychological needs of patients, which our findings suggest can significantly influence recovery trajectories and quality of life improvements. Incorporating strategies to enhance emotional intelligence among clinicians could not only improve patient outcomes but also bolster clinicians’ resilience and satisfaction in their roles.53 Furthermore, our study highlights the importance of addressing modifiable risk factors, such as smoking and substance use, in the post-COVID care continuum. By integrating these evidence-based recommendations and our study’s findings, healthcare providers can better support the complex needs of Long-COVID patients, potentially accelerating their recovery and enhancing overall well-being. This approach aligns with the evolving understanding of Long-COVID as a multifaceted condition, necessitating a comprehensive and empathetic care strategy.
While the study offers valuable insights into the longitudinal effects of Long-COVID on patients’ mental health and quality of life, several limitations should be noted. Firstly, the cross-sectional nature of the study design prevents tracking individual progress over time, which could provide a more nuanced understanding of symptom trajectories. As a result, it is impossible to ascertain causal relationships between the onset of Long-COVID and the observed depression, anxiety, and quality of life metrics. Additionally, sourcing all participants from a single hospital, Victor Babes Hospital for Infectious Diseases and Pulmonology in Timisoara, Romania, might introduce selection bias and limit the generalizability of the findings to broader populations. Furthermore, excluding patients with severe COVID-19 cases and those with pre-existing chronic respiratory or psychiatric conditions means the findings might not encompass the entire spectrum of Long-COVID experiences. This exclusion criterion might inadvertently overlook patients whose mental health symptoms originate or are exacerbated from severe COVID-19 or from a combination of Long-COVID with prior health challenges.
Conclusion
There was a marked decline in the severity of depressive and anxiety symptoms from 2020 to 2022. Concurrently, the quality of life, as measured by the SF-36 survey, showed consistent improvement. Factors like current smoking status, substance use, and the se-verity of the initial COVID-19 infection were notably linked with increased depression risk. While there was an overall improvement in patients’ psychological well-being, an increase in heart-related post-COVID symptoms emerged as a significant concern for future care strategies.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lovato A, Rossettini G, de Filippis C. Sore throat in COVID-19: comment on ”Clinical characteristics of hospitalized patients with SARS-CoV-2 infection: a single arm meta-analysis”. J Med Virol. 2020;92(7):714–715. doi:10.1002/jmv.25815
2. Muralidar S, Ambi SV, Sekaran S, Krishnan UM. The emergence of COVID-19 as a global pandemic: understanding the epidemiology, immune response and potential therapeutic targets of SARS-CoV-2. Biochimie. 2020;179:85–100. PMID: 32971147; PMCID: PMC7505773. doi:10.1016/j.biochi.2020.09.018
3. Dey A, Das R, Misra HS, Uppal S. Coronavirus disease 2019: scientific overview of the global pandemic. New Microbes New Infect. 2020;38:100800. PMID: 33133611; PMCID: PMC7591944. doi:10.1016/j.nmni.2020.100800
4. Muntean D, Horhat FG, Bădițoiu L, et al. Multidrug-resistant gram-negative bacilli: a retrospective study of trends in a tertiary healthcare unit. Medicina. 2018;54(6). doi:10.3390/medicina54060092
5. Toma AO, Prodan M, Reddyreddy AR, et al. The epidemiology of malignant melanoma during the first two years of the COVID-19 pandemic: a systematic review. Int J Environ Res Public Health. 2022;20(1):305. doi:10.3390/ijerph20010305
6. Ludwig S, Zarbock A. Coronaviruses and SARS-CoV-2: a Brief Overview. Anesth Analg. 2020;131(1):93–96. PMID: 32243297; PMCID: PMC7173023. doi:10.1213/ANE.0000000000004845
7. Fernández-de-Las-Peñas C, Palacios-Ceña D, Gómez-Mayordomo V, Cuadrado ML, Florencio LL. Defining Post-COVID Symptoms (Post-Acute COVID, Long COVID, Persistent Post-COVID): an Integrative Classification. Int J Environ Res Public Health. 2021;18(5):2621.
8. Fernández-de-Las-Peñas C. Long COVID: current definition. Infection. 2022;50(1):285–286. doi:10.1007/s15010-021-01696-5
9. Bhadoria P, Gupta G, Agarwal A. Viral pandemics in the past two decades: an overview. J Family Med Prim Care. 2021;10(8):2745–2750. PMID: 34660399; PMCID: PMC8483091. doi:10.4103/jfmpc.jfmpc_2071_20
10. Turaiche M, Feciche B, Gluhovschi A, et al. Biological profile and clinical features as determinants for prolonged hospitalization in adult patients with measles: a monocentric study in Western Romania. Pathogens. 2022;11(9):1018. doi:10.3390/pathogens11091018
11. Baker RE, Mahmud AS, Miller IF, et al. Infectious disease in an era of global change. Nat Rev Microbiol. 2022;20(4):193–205. PMID: 34646006; PMCID: PMC8513385. doi:10.1038/s41579-021-00639-z
12. Fericean RM, Rosca O, Citu C, et al. COVID-19 clinical features and outcomes in elderly patients during six pandemic waves. J Clin Med. 2022;11(22):6803. doi:10.3390/jcm11226803
13. Hameed R, Bahadur AR, Singh SB, et al. Neurological and psychiatric manifestations of long COVID-19 and Their [18F]FDG PET Findings: a Review. Diagnostics (Basel). 2023;13(14):2353. PMID: 37510097; PMCID: PMC10378471. doi:10.3390/diagnostics13142353
14. Sapna F, Deepa F, Sakshi F, et al. Unveiling the mysteries of long COVID syndrome: exploring the distinct tissue and organ pathologies linked to prolonged COVID-19 symptoms. Cureus. 2023;15(9):e44588. PMID: 37795061; PMCID: PMC10545886. doi:10.7759/cureus.44588
15. Mak IW, Chu CM, Pan PC, Yiu MG, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. 2009;31(4):318–326. PMID: 19555791; PMCID: PMC7112501. doi:10.1016/j.genhosppsych.2009.03.001
16. Zürcher SJ, Kerksieck P, Adamus C, et al. Prevalence of mental health problems during virus epidemics in the general public, health care workers and survivors: a rapid review of the evidence. Front Public Health. 2020;8:560389. PMID: 33262966; PMCID: PMC7688009. doi:10.3389/fpubh.2020.560389
17. Isasi F, Naylor MD, Skorton D, Grabowski DC, Hernández S, Patients RVM. Families, and communities COVID-19 impact assessment: lessons learned and compelling needs. NAM Perspect. 2021;2021:
18. O’Connor DB, Aggleton JP, Chakrabarti B, et al. Research priorities for the COVID-19 pandemic and beyond: a call to action for psychological science. Br J Psychol. 2020;111(4):603–629. PMID: 32683689; PMCID: PMC7404603. doi:10.1111/bjop.12468
19. Fericean RM, Citu C, Manolescu D, et al. Characterization and outcomes of SARS-CoV-2 infection in overweight and obese patients: a dynamic comparison of COVID-19 pandemic waves. J Clin Med. 2022;11:2916. doi:10.3390/jcm11102916
20. Pisaturo M, Russo A, Pattapola V, et al.; CoviCam Group. Clinical characterization of the three waves of COVID-19 occurring in southern Italy: results of a multicenter cohort study. Int J Environ Res Public Health. 2022;19(23):16003. PMID: 36498078; PMCID: PMC9738780. doi:10.3390/ijerph192316003
21. Cuschieri S. The STROBE guidelines. Saudi J Anaesth. 2019;13(Suppl 1):S31–S34. doi:10.4103/sja.SJA_543_18
22. Chippa V, Aleem A, Anjum F. Post-Acute Coronavirus (COVID-19) Syndrome. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK570608/.
23. Stephenson T, Pinto Pereira SM, Nugawela MD, et al.; CLoCk Consortium. Long COVID-six months of prospective follow-up of changes in symptom profiles of non-hospitalised children and young people after SARS-CoV-2 testing: a national matched cohort study (The CLoCk) study. PLoS One. 2023;18(3):e0277704. doi:10.1371/journal.pone.0277704
24. Lins L, Carvalho FM. SF-36 total score as a single measure of health-related quality of life: scoping review. SAGE Open Medicine. 2016;4:2050312116671725. doi:10.1177/2050312116671725
25. Johnson SU, Ulvenes PG, Øktedalen T, Hoffart A. Psychometric properties of the general anxiety disorder 7-item (GAD-7) Scale in a heterogeneous psychiatric sample. Front Psychol. 2019;10:1713. PMID: 31447721; PMCID: PMC6691128. doi:10.3389/fpsyg.2019.01713
26. Levis B, Benedetti A, Thombs BD; DEPRESsion Screening Data (DEPRESSD) Collaboration. Accuracy of patient health questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ. 2019;365:1476. Erratum in: BMJ. 2019 Apr 12;365:1781. PMID: 30967483; PMCID: PMC6454318. doi:10.1136/bmj.l1476
27. Yu Y, Lau MMC, Ling RHY, Lau JTF. Time to lift up COVID-19 restrictions? Public support towards living with the virus policy and associated factors among Hong Kong General Public. Int J Environ Res Public Health. 2023;20(4):2989. PMID: 36833683; PMCID: PMC9958650. doi:10.3390/ijerph20042989
28. Martín Sánchez FJ, Martínez-Sellés M, Molero García JM, et al. Insights for COVID-19 in 2023. Rev Esp Quimioter. 2023;36(2):114–124. PMID: 36510683; PMCID: PMC10066911. doi:10.37201/req/122.2022
29. Regunath H, Goldstein NM, Guntur VP. Long COVID: where Are We in 2023? Mo Med. 2023;120(2):102–105. PMID: 37091941; PMCID: PMC10121126.
30. De Luca R, Bonanno M, Calabrò RS. Psychological and cognitive effects of long COVID: a narrative review focusing on the assessment and rehabilitative approach. J Clin Med. 2022;11(21):6554. PMID: 36362782; PMCID: PMC9653636. doi:10.3390/jcm11216554
31. Nouraeinejad A. Brain fog as a long-term sequela of COVID-19. SN Compr Clin Med. 2023;5(1):9. PMID: 36466122; PMCID: PMC9685075. doi:10.1007/s42399-022-01352-5
32. Dumitrescu A, Doros G, Lazureanu VE, et al. Post-severe-COVID-19 cardiopulmonary rehabilitation: a comprehensive study on patient features and recovery dynamics in correlation with workout intensity. J Clin Med. 2023;12:4390. doi:10.3390/jcm12134390
33. Pescaru CC, Crisan AF, Marc M, et al. A systematic review of telemedicine-driven pulmonary rehabilitation after the acute phase of COVID-19. J Clin Med. 2023;12:4854. doi:10.3390/jcm12144854
34. Suppini N, Oancea C, Fira-Mladinescu O, et al. Post-infection oscillometry and pulmonary metrics in SARS-CoV-2 patients: a 40-day Follow-Up Study. Diseases. 2023;11:102. doi:10.3390/diseases11030102
35. Papava I, Dehelean L, Romosan RS, et al. The impact of hyper-acute inflammatory response on stress adaptation and psychological symptoms of COVID-19 patients. Int J Environ Res Public Health. 2022;19:6501. doi:10.3390/ijerph19116501
36. Cheng K, Wu C, Gu S, Lu Y, Wu H, Li C. WHO declares the end of the COVID-19 global health emergency: lessons and recommendations from the perspective of ChatGPT/GPT-4. Int J Surg. 2023;109(9):2859–2862. PMID: 37246993; PMCID: PMC10498859. doi:10.1097/JS9.0000000000000521
37. Dehelean L, Papava I, Musat MI, et al. Coping strategies and stress related disorders in patients with COVID-19. Brain Sci. 2021;11:1287. doi:10.3390/brainsci11101287
38. DePace NL, Colombo J. Long-COVID syndrome and the cardiovascular system: a review of neurocardiologic effects on multiple systems. Curr Cardiol Rep. 2022;24(11):1711–1726. PMID: 36178611; PMCID: PMC9524329. doi:10.1007/s11886-022-01786-2
39. Wu Z, Yue Q, Zhao Z, et al. A cross-sectional study of smoking and depression among US adults: NHANES (2005–2018). Front Public Health. 2023;11:1081706. PMID: 36794066; PMCID: PMC9922891. doi:10.3389/fpubh.2023.1081706
40. Ranjit A, Buchwald J, Latvala A, et al. Predictive association of smoking with depressive symptoms: a longitudinal study of adolescent twins. Prev Sci. 2019;20(7):1021–1030. PMID: 31069603; PMCID: PMC6718365. doi:10.1007/s11121-019-01020-6
41. Sykes DL, Holdsworth L, Jawad N, Gunasekera P, Morice AH, Crooks MG. Post-COVID-19 symptom burden: what is long-COVID and how should we manage it? Lung. 2021;199(2):113–119. doi:10.1007/s00408-021-00423-z
42. Romero-Duarte Á, Rivera-Izquierdo M, Guerrero-Fernández de Alba I, et al. Sequelae, persistent symptomatology and outcomes after COVID-19 hospitalization: the ANCOHVID multicentre 6-month follow-up study. BMC Med. 2021;19(1):1–13.
43. Zakia H, Pradana K, Iskandar S. Risk factors for psychiatric symptoms in patients with long COVID: a systematic review. PLoS One. 2023;18(4):e0284075. PMID: 37027455; PMCID: PMC10081737. doi:10.1371/journal.pone.0284075
44. Huarcaya-Victoria J, Barreto J, Aire L, et al. Mental health in COVID-2019 survivors from a general hospital in Peru: sociodemographic, clinical, and inflammatory variable associations. Int J Ment Health Addict. 2021:1–22. doi:10.1007/s11469-021-00659-z
45. Taquet M, Dercon Q, Luciano S, Geddes JR, Husain M, Harrison PJ. Incidence, co-occurrence, and evolution of long-COVID features: a 6-month retrospective cohort study of 273,618 survivors of COVID-19. PLoS Med. 2021;18(9):e1003773. doi:10.1371/journal.pmed.1003773
46. Huang C, Huang L, Wang Y, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397(10270):220–232. doi:10.1016/S0140-6736(20)32656-8
47. Dankowski R, Sacharczuk W, Duszyńska D, et al. Depression and anxiety in patients recently recovered from coronavirus disease (COVID‑19). Neuropsychiatria i Neuropsychologia. 2021;16(1):11–16.
48. Grover S, Sahoo S, Mishra E, et al. Fatigue, perceived stigma, self-reported cognitive deficits and psychological morbidity in patients recovered from COVID-19 infection. Asian J Psychiatr. 2021;64:102815. doi:10.1016/j.ajp.2021.102815
49. Frontera JA, Yang D, Lewis A, et al. A prospective study of long-term outcomes among hospitalized COVID-19 patients with and without neurological complications. J Neurol Sci. 2021;426:117486. doi:10.1016/j.jns.2021.117486
50. Kaplan V. The burnout and loneliness levels of housewives in home-quarantine during Covid-19 pandemic. Cyprus Turkish J Psychiatry Psychol. 2021;3(2):115. doi:10.35365/ctjpp.21.2.13
51. Fontanini R, Visintini E, Rossettini G, Caruzzo D, Longhini J, Palese A. Italian Nurses’ experiences during the COVID-19 pandemic: a qualitative analysis of internet posts. Int Nurs Rev. 2021;68(2):238–247. PMID: 33730760; PMCID: PMC8250969. doi:10.1111/inr.12669
52. Rossettini G, Peressutti V, Visintini E, et al. Italian nurses’ experiences of the COVID-19 pandemic through social media: a longitudinal mixed methods study of Internet posts. Digit Health. 2022;8:20552076221129082. PMID: 36211800; PMCID: PMC9536097. doi:10.1177/20552076221129082
53. Rossettini G, Conti C, Suardelli M, et al. COVID-19 and health care leaders: how could emotional intelligence be a helpful resource during a pandemic? Phys Ther. 2021;101(9):pzab143. PMID: 34101807; PMCID: PMC8418206. doi:10.1093/ptj/pzab143
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
