Back to Journals » Neuropsychiatric Disease and Treatment » Volume 16
A Survey on Public Attitudes Toward Mental Illness and Mental Health Services Among Four Cities in Saudi Arabia
Authors Alsubaie S, Almathami M, Alkhalaf H , Aboulyazid A , Abuhegazy H
Received 13 June 2020
Accepted for publication 22 September 2020
Published 27 October 2020 Volume 2020:16 Pages 2467—2477
DOI https://doi.org/10.2147/NDT.S265872
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Sultan Alsubaie,1 Mohammad Almathami,1 Hanouf Alkhalaf,2 Ahmed Aboulyazid,3,4 Hesham Abuhegazy1,5
1Department of Psychiatry, Armed Forces Hospital, Khamis Mushayt, Saudi Arabia; 2Saudi Commission for Health Specialties, Riyadh, Saudi Arabia; 3Preventive Medicine, Armed Forces Hospital, Khamis Mushayt, Saudi Arabia; 4Public Health, Faculty of Medicine, Mansoura University, Mansoura, Egypt; 5Psychiatry, Faculty of Medicine for Boys, Al-Azhar University, Cairo, Egypt
Correspondence: Sultan Alsubaie
Consultant Psychiatrist, Psychiatry Department, Armed Forces Hospital, Southern Region, P.O. Box 101, Khamis Mushayt, Saudi Arabia
Tel +966503799971
Email [email protected]
Purpose: Our objectives are to assess the public attitude toward mentally ill people and mental health services and to compare the attitudes of those who have past history of mental illness, those who have been exposed to mentally ill people, and those who have not.
Materials and Methods: We conducted a cross-sectional study among subjects (n=1268) in four Saudi Arabian cities (Riyadh, Abha, Dammam, and Jizan), recruiting participants from malls and parks. All participants were administered “the knowledge and attitudes toward mental illness and mental health services scale”.
Results: Participants were divided into three groups; non-exposed to mental illness group (n=687, 54.1%), exposed to mental illness group (n=305, 24%), and having past history of mental illness group (n=276, 21.8%). Results revealed that non-exposed group had the lowest knowledge about mental illness (p < 0.001). Exposed group had the best attitude toward mentally ill people (p=0.002), mental health services (p< 0.001), the lowest impact of traditional beliefs (p< 0.001), and the best help-seeking decisions (p = 0.001). Regression models show the variables that predicted attitude toward the mentally ill were the attitude toward mental health services (p=0.001), impact of traditional beliefs (p=0.001), and residency (p=0.04). The predictors of attitude toward mental health services were impact of traditional beliefs (p< 0.001), knowledge (p< 0.001), and residency (p=0.028). And the variables that account for predicting future decisions were impact of traditional beliefs (p< 0.001), attitude toward mental health services (p=0.001), and having past history of mental illness (p=0.006).
Conclusion: This study demonstrates significant differences in attitudes toward mental illness among different groups of participants. Lesser impact of traditional beliefs and better knowledge about mental illness were the factors most associated with better attitudes toward mentally ill people and mental health services and with better help-seeking behavior.
Keywords: public, attitude, opinion, mental illness, mental health service, Saudi Arabia
Introduction
Psychiatric illnesses are a public health problem worldwide, affecting people of all age groups, psychologically and socially.1 Negative attitude toward people with mental illness is the greatest barrier to recovery, development of effective care, treatment, and prevention of mental illness.2 Public understanding of the biological correlates of mental illness increases social acceptance of persons with mental illness.2 Many studies have reported that knowledge of public attitude toward mental illness and its treatment is an important prerequisite to develop successful community-based programs.3 Cultural differences also have important implications with connection to caregiver stigma and burden.4 The recognition of mental illness depends on a precise assessment of the beliefs and norms within the individual’s cultural environment.5
A Cornell University study from 2015 showed that 67% of the public believed that mental disorder was an extreme or serious public health problem, 89% believed that physical and mental health were equally significant, and two-thirds believed that physical health was treated with major importance in the current US health care system.6 Another report had found major differences between the conceptions held by the unspecialized public and those of psychiatric experts regarding the appropriate treatment of mental disorders.7 Study of public attitudes in Germany over the last couple of decades had found an improvement in attitudes toward mental health providers and treatments; however, attitudes toward mentally ill people have remained unchanged or worsened.8 Sara Evans-Lacko et al used data from the 2003 to 2013 national Attitudes to Mental Illness surveys to examine trends in public attitudes across England before and during the Time to Change anti-stigma campaign: they discovered significant improvement in positive attitudes after the Time to Change campaign.9 In a comparison between US and Indian cultures, Marrow and Luhrmann described how some social and cultural perceptions clearly combine to lead families of different cultures to either hide family members with severe psychosis within their homes or leave them to institutions or on the streets.10
In our region, in the early 11th century, Muslim scholar Ibn Sina disapproved and challenged the concept that evil spirits could cause mental disorders.11 Mental health care in Saudi Arabia – like in most Arab countries – has passed through significant changes over the past decades to transform the mental health care system into a professionalized one that adapts to the challenges of the 21st century; however, cultural, family, and religious beliefs still have marked influences on the public understanding and attitudes toward diagnosis and treatment of mental illness.12 Studies have found that one-third of primary health care patients in Saudi Arabia have psychiatric illnesses,13 and a high proportion of the faith healers' visitors have diagnosable mental illnesses.14 Almutairi highlighted the need to investigate the gaps in knowledge within mental illness literature in Saudi Arabia, and to develop practice recommendations.15
The literature on public attitudes toward mental illnesses and mental health services in Arab countries including Saudi Arabia is more limited, and most of the studies were conducted in universities and the participants were university students.4,16–18
Our study aimed to assess a sample of the Saudi Arabian general public on attitude toward mentally ill people and mental health services; and to assess the contribution of knowledge about mental illness, impact of traditional beliefs, and level of exposure to mental illness in the prediction of subjects' attitudes toward mental illness and mental health services and their future help-seeking decisions. We hypothesized that knowledge and traditional beliefs were each independently associated with attitudes and future decisions, and that the level of exposure to mental illness independently predicts a subject’s attitudes and future decisions.
Materials and Methods
Study Design
A cross-sectional survey was carried out in the period from February 2017 to May 2017. We recruited the participants from malls and parks in four Saudi Arabian cities: Riyadh, Dammam, Abha, and Jizan. Ethical approval from ethical review committee (H-06-KM-001) of Armed Forces Hospital Southern Region (AFHSR), Khamis Mushait, Saudi Arabia was granted before data collection. The study objectives were explained to all participants, in addition to obtaining informed consent. All data were stored in a safe and secure place that is only accessible by researchers. This study was conducted in accordance with the Declaration of Helsinki.
Inclusion criteria included to be a Saudi citizen, Arabic speaker, able to read and write, and 18 years of age or above. Exclusion criteria were: being non-Saudi, non-Arabic speaker, unable to read and write, less than 18 years old, or having disability that affects communication (blindness, deafness).
Data Collection
The questionnaires were applied by trained volunteer researchers: all of them have a university degree, and they were properly trained on the administration of the questionnaires. The participants were asked to complete a demographic information form as well as the knowledge and attitude toward mental illness and mental services scale, which usually takes about 20 minutes to complete. The questionnaires were completed and collected at the same venue.
Study Tools
- The demographic information form includes age, gender, education, residency, marital state, and job status.
It also includes two questions that required yes or no answers:
- Have you have ever experienced a mental illness that required you or your care givers to consult a mental health professional?
- Have you ever known or shared in giving care to a mentally ill person?
According to the answers to these two questions we differentiate our sample into 3 groups:
Who answered no to both questions.
Who answered no to the first question and yes to the second.
Who answered yes to the first question, regardless of their answer to the second one.
The Knowledge and Attitude Toward Mental Illness and Mental Services Scale
The scale was developed by the main researcher in Arabic language; it consisted of 32 statements, and response option included: agree=2, do not know =1, and disagree=0. The statements are summed in four subscales with one final question regarding the participant's decision if he developed mental symptoms in the future:
- The Knowledge about Mental Illness Subscale: it is an 11-statement scale to measure the knowledge about mental illness (types, causes, and management of mental illnesses). The statement numbers are 1–3–4–7–9–11–14–18–23–27–31. The total scores range from 0 (disagree) to 22 (agree); the higher the score, the more knowledge about mental illness.
- The Attitude toward Mentally Ill People Subscale: it is a 9-statement scale to measure the attitude toward mentally ill people. The statement numbers are 5–10–13–17– 21–24–26–29–32. The total scores range from 0 (disagree) to 18 (agree); the higher the score, the more negative attitude toward mentally ill people.
- The Attitude toward Mental Health Services Subscale: it is a 7-statement scale to measure the attitude toward mental health services. The statement numbers are 2–8–12–16–19–22–28. The total scores range from 0 (disagree) to 14 (agree); the higher the score, the more negative attitude toward mental health services.
- The Impact of Traditional Beliefs on the Attitude toward Mental Illness Subscale: it is a 5-statement scale to measure the traditions and beliefs toward mental disorders. The statement numbers are 6–15–20–25–30. The total scores range from 0 (disagree) to 10 (agree); the higher the score, the more negative impact of traditional beliefs on the attitude toward mental illness.
- Future help-seeking decision if someone developed mental symptoms: this final question has four possible responses: I will consult a mental health provider, a faith healer, both 1 and 2, and I do not know.
The questionnaire was piloted on a small number of participants (n=30). The wording and suggested answers were modified for some statements based on the feedback from the pilot sample. A multi-disciplinary committee covering psychiatry, psychology, and epidemiology reviewed the content of the questionnaire for content validity. Reliability was assessed through test-retest reliability method, the questionnaire re-administered to the same volunteers (n= 57) after a 4-week period with 0.83 concordance, and Cronbach’s alpha for internal consistency was 0.86.
Sample Size
By applying a convenience sampling technique, the study approached 1563 subjects, and 1268 of them returned completed questionnaires, a response rate of 81.1%. There were significant differences between completers and non-completers in terms of age (non-completers were older than completers, p=0.023) and gender (more males among non-completers, p=0.04).
Statistical Analysis
Independent variables were attitude toward mentally ill, attitude toward mental health services, and future help-seeking decision if the subject developed symptoms of mental illness. The data were analyzed using SPSS for IBM version 22 software system. Descriptive statistics (mean, standard deviation, and percentages) were used to describe the quantitative, categorical, and outcome variables. Pearson’s chi-square test was used to examine the association between the categorical outcome variables, Student’s t-test for continuous variables, one way for correlation between variables, t-test for equality of means to compare between groups. Multiple regression analyses were used to detect independent variables predicting two main outcomes, attitude toward mentally ill people and attitude toward mental health services, while binary regression analyses with Wald test was used to detect independent variables that predict future help-seeking decisions. A p-value of <0.05 was used to report statistical significance and precision of estimates.
Results
Basic Characteristics of the Sample
The mean age of participants was 27.5±8.5 years, with an age range of 18–64 years; 60.6% of participants were females, 56.3% were singles, 46% were students, while 40.5% had a job. The vast majority of our sample either went to intermediate or secondary schools (49%), or universities (45.7%); 21.8% reported they had some mental illness before, and 24% reported they know someone with mental illness. Therefore, we divided our sample according to exposure to mental illness into three groups:
Group 1 (Non-Exposed Group)
Those who reported having no previous history of mental illness and not knowing anybody with mental illness (n=687; 54.1%).
Group 2 (Exposed Group)
Those who reported having no previous history of mental illness but knowing somebody with mental illness (n=305; 24%).
Group 3 (mental illness group)
Those who reported they had previous history of mental illness (n=276; 21.8%).
Comparison of the Three Studied Groups
There was a significant difference in age between the 3 groups (p<0.001), the mental illness group being the oldest, while the non-exposed group was the youngest (29.3±9.1 vs. 26.6± 7.9). There were no significant differences in gender, but marital status shows significant differences (p=0.01), 60.6% of non-exposed group being single compared to 50.2% of exposed group and 52.5% of mental illness group. University education was recorded among 41.3% of non-exposed group participants compared to 54.3% of mental illness group (p =0.001), Table 1.
 |
Table 1 Socio-Demographic Characteristics of Sampled Population for Assessing Knowledge and Attitude Towards Mental Illness and Mental Health Services, Saudi Arabia |
Table 2 demonstrates significant differences between groups in knowledge (p<0.001), non-exposed group having the lowest mean knowledge score compared to the other two groups. There were significant differences in attitude toward mentally ill people, and toward mental health services (p= 0.002 and <0.001 respectively). Exposed group possessed the best attitude toward mentally ill people and mental health services, while mental illness group possessed the poorest attitude (M±SD= 5.9±3.4 vs. 6.8±4.1; and 3.08±2.4 vs. 4.2±3.2, respectively). There were significant differences in impact of traditional beliefs on the attitude toward mental illness (p<0.001). Exposed group had the best impact while mental illness group had the worst impact (2.5±2.4 vs. 3.5±2.7). Future help-seeking decisions were also significantly different (p<0.001), exposed group being the most willing to consult mental health providers while mental illness group was the least willing to do so (46% vs. 30.8%); conversely mental illness group was the most willing to consult faith healers, while exposed group was the least likely to do so (4.7% vs. 3%); however, the mental health professionals were the preferred source of help among all subjects, almost ten-fold the help-seeking from traditional healers (30–46% vs. 3–4.7%).
 |
Table 2 Knowledge and Attitude of Population Towards Mental Illness and Mental Health Services According to the Study Groups, Saudi Arabia |
Correlation Analyses
The impact of traditional beliefs is negatively associated with knowledge, attitude toward mental health services, and mentally ill people (p < 0.001 for all). On the other hand, attitude toward mental health services is positively associated with both knowledge and attitude toward mentally ill people (p < 0.001 for both), Table 3.
 |
Table 3 Correlation Between Age, Knowledge, Attitude Toward Mentally Ill, Attitude Toward Mental Health Services, and Impact of Traditional Beliefs |
Multivariate Regression Models
Attitude Toward Mental Health Services
About 40% of the variance in predicting attitude toward mental health services was accounted for in the total model (R2= 0.397). After covarying with age, gender, education, residency, marital status, knowledge, impact of traditional beliefs, and exposure to mental illness, the independent predictors were impact of traditional beliefs, knowledge, and residency. Lesser impact of traditional beliefs, and greater knowledge about mental illness predicted better attitude toward mental health services (t=26.66, p= 0.001, and t= −4.56, p= 0.0001) respectively, and being resident in Riyadh predicted worse attitude toward mental health services (t=2.19, p= 0.03). Exposure to mental illness was not significantly associated with attitude toward mental health services (t= −415, p= 0.678), Table 4.
 |
Table 4 Multiple Regression Models: Variables Predicting Attitude Toward Mental Health Services |
Attitude Toward Mentally Ill People
Table 5 demonstrates that 40% of variance in predicting attitude toward mentally ill people was accounted for in the total model (R2= 0.399). After covarying for gender, residency, attitude toward mental health services, impact of traditional beliefs, and exposure to mental illness, the independent variables that predicted attitude toward the mentally ill were attitude toward mental health services, impact of traditional beliefs, and residency. Better attitude toward mental health services and lesser impact of traditional beliefs predicted better attitude toward mentally ill people (t=13.27, p= 0.001, and t= 11.7, p= 0.001) respectively, and being resident in Riyadh predicted poor attitude toward the mentally ill (t= −2.05, p= 0.04). Exposure to mental illness was not significantly associated with attitude toward mentally ill (t=0.012, p= 0.990).
 |
Table 5 Multiple Regression Models: Variables Predicting Attitude Toward Mentally Ill |
Future Help-Seeking Decisions
Around 21% of variance in predicting future decisions was accounted for in the total model (R2= 0.21). After covarying for gender, residency, knowledge, attitude toward mentally ill, attitude toward mental health services, impact of traditional beliefs, and exposure to mental illness, the impact of traditional beliefs, attitude toward mental health services, and exposure to mental illness were the independent variables that account for predicting future decisions. Lesser impact of traditional beliefs (Wald= 116.9, p< 0.001) and better attitude toward mental health services (Wald= 11.75, p= 0.001) predicted greater help-seeking from mental health professionals in future decisions, while having a past history of mental illness (β= −0.49, Wald= 7.68, p= 0.006) significantly predicted avoiding mental health professionals in help-seeking decisions, Table 6.
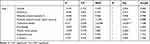 |
Table 6 Binary Regression Models: Variables Predicting Future Decisions |
Figure 1 depicts the interrelations between different study variables as derived from multiple regression models. Traditional beliefs are negatively associated with knowledge, attitude toward mental health services and mentally ill individuals, and future help-seeking decisions; while knowledge is positively associated with attitude toward mental health services, which in turn is positively associated with both attitude toward mentally ill and future decisions, and finally mental illness group is negatively associated with future decisions.
 |
Figure 1 Interrelation between study variables and end point variables. |
Discussion
The purpose of this study was to examine the public knowledge and attitude toward mental illness and future decision-making regarding mental health. We found that mental health professionals were the preferred source of help among all subjects; the help-seeking from mental health professionals was almost ten-fold the help-seeking from traditional healers (30–46% vs. 3–4.7%). The Current State of Psychiatry in Saudi Arabia report of 2013 compared the components of services with an old 1983 report. It identified the vast changes that had been implemented in service providing, involving general health services, specialized mental health hospitals, and private practice, and the increase in numbers of psychiatrists, psychiatric nurses, psychologists, and social workers to almost the world averages.19 Qureshi et al had reported that there are many active consumer organizations, family organizations, and non-governmental organizations who advocate for mental health.20
Primary analyses found that exposed participants had a significantly better attitude toward mentally ill people and mental health services, lesser impact of traditional beliefs, and more healthy help-seeking behavior in comparison to participants who have past history of mental illness. However, after controlling for age, sex, residency, education, marital status, having a job, knowledge, and traditional beliefs, we found that level of exposure to mental illness was no longer significantly associated with either attitude toward mentally ill people, or toward mental health services but only can predict future decision-making. Subjects with past history of mental illness were significantly less likely to consult mental health professionals (β= −0.49, p= 0.006). These findings go against our hypotheses; however, they are similar to Angermeyer and Dietrich's meta-analyses which found thirty studies reporting that people had more positive attitudes if they were familiar with mental illness. The opposite was found in only one instance. And in another 30 studies no association between familiarity and attitudes was reported.21 Nevertheless, it goes against many other studies, like the Hong Kong cross-sectional study that found that attitude was positively associated with family history of mental illness;22 the Egyptian study on university students, which found that students with family history of mental illness hold more positive beliefs about mental illness;5 and Angermeyer et al who have concluded that a strong desire for social distance from mentally ill people decreased if there is appropriate knowledge about mental illness, which means that exposure to mental illness resulted in a positive attitude.23 Our controversial results may be explained by high expectations of our young well-educated sample. But the negative help-seeking behavior of subjects having past history of mental illness may raise some worry about the kind of experience they had with medical facilities; however, it needs further exploration through more precise and longitudinal studies to unravel this strange finding.
Traditional beliefs were independently and significantly negatively associated with knowledge, attitude toward mentally ill people, and mental health services. Even after controlling for covariates it was strongly associated with our end points of interest: the more impact of traditional beliefs predicted poorer attitude toward mental health services and mentally ill people, and worse help-seeking decisions, with a large effect size for predicting all of them (β=0.60, t= 26.6, p <0.001; (β =0.33, t= 11.7, p= 0.001; and (β=0.41, Wald= 116.9, p< 0.001; respectively). Conversely, knowledge was positively associated with attitude toward mental health services (β= 0.10, t= 4.56, p<0.001). Larger amount of knowledge significantly predicted a better attitude toward mental health services. This runs in concordance with the Saudi study on medical students that shows positive changes in the students' attitude toward psychiatry, intervention efficacy, role definition, and functioning of psychiatrists after rotation in psychiatry,17 and partially with the Angermeyer et al metanalysis which found that proper identification of mental illnesses was associated with higher expectations from treatments and a greater recommendation to visit a psychiatrist.24 The 2013 report on the mental health system in Saudi Arabia prioritized enhancing public education programs on mental illnessas this improves early detection and proper help-seeking for those with mental illnesses.20 Another report from Saudi Arabia has highlighted the importance of designing education programs to improve public awareness of mental illnesses, as well as their causes, consequences, and treatments.15
We found that attitude toward mental health services was independently associated with both attitude toward mentally ill, and healthy decision-making, suggesting that if somebody had a good impression about service, he will recommend it with confidence.
We surprisingly found that residency was a significantly associated with a subject’s attitude toward the mentally ill and mental health services; participants from the capital city, Riyadh, had the poorest attitudes. This is in contrast to the results of several international studies5,21,25 which found that, comparing urban to rural areas, the rural areas had a more negative attitude toward mentally ill people. Having a look at our local community, Alosaimi et al14 had found that most users of faith healers in Riyadh city (78%) had mental illnesses, with depressive disorders the most prevalent (34.9%), and anxiety disorders the next (18.7%). It is difficult to give an explanation for our findings; however, the Alosaimi study can shed some light on the reality, although it does not give an explanation for the differences between Riyadh inhabitants and other areas of the kingdom other than their high expectations. It deserves a more specifically designed study.
Limitations
The study has several limitations that hinder generalization of our findings and provide direction for further research: first, our study recruits the participants from parks and shopping malls, which hinders representation of rural, older, and illiterate people; their inclusion could change the spirit of our results. Second, our sample does not resemble the general population of Saudi Arabia in some aspects: the mean age is 27.5±8.5, females are overrepresented, and the vast majority of our sample have intermediate or high school education which is not the case in our community; these factors make our sample not really representative of the community and limits the ability to generalize our findings. A large-scale study on a representative sample could give us a better idea about the attitudes and help-seeking decisions in our community. Third, the cross-sectional design has its inherent limitation, that it cannot address the causal relationships between variables. Longitudinal research in a large representative sample could shed more light on how exposure and other factors can affect the attitudes and future decisions. Fourth, the subjective nature of information: although the knowledge and attitude are a merely subjective experience, relying on subjects' reports of whether they had been exposed to mentally ill people or had previous mental illness – without any formal diagnoses, second party confirmation, or determination to which extent they were involved in caring for others with mental illness – is another limitation to this study. Finally, we did not account for mental health and general health conditions that might be associated with attitudes and help-seeking decisions.
Despite these limitations, our study incorporated several methodological improvements over the prior investigations of public attitudes and help-seeking decisions. These include the sampling from four major cities, including mixed rather than homogeneous group of participants (students), and the simultaneous assessment of the level of exposure to mental illness and mentally ill people and correlating it to their attitudes. The study has found that about 22% of participants reported they had past history of mental illness, which is consistent with World Health Organization (WHO) estimates of prevalence of mental illnesses.26,27
Conclusion
The current study on knowledge and attitude toward mental illness in four major cities in Saudi Arabia had revealed that almost one-fifth reported they had some previous mental illness, and they had the unhealthier decisions regarding help-seeking in the future. The study demonstrated that larger amount of knowledge and lesser impact of traditions is associated with better attitude toward mental health services, and hence the lesser impact of traditional beliefs lead to better attitude toward mentally ill people and healthier expected help-seeking decisions.
Public education about psychiatric illnesses is highly recommended. Assessment and knowledge of people's attitudes towards mental illness, mental health providers, and mental health services help in creating plans and strategies and adopting methods to make these attitudes more positive, which helps in better outcome and recovery. Integration of psychiatric patients in the community as well as mental health services with other medical specialties will decrease the stigma toward psychiatric patients and mental health providers.
Author Details
Author/co-authors contact details: 1- Dr.Sultan Alsubaie [email protected]. 2- Mohammad Almathami [email protected]. 3- Hanouf Alkhalaf [email protected]. 4- Ahmed Aboulyazid [email protected]. 5- Hesham Abuhegazy [email protected].
Acknowledgments
The authors would like to acknowledge the support from ethical review committee from AFHSR, Khamis Mushait, Saudi Arabia; the review committee who reviewed our scale for construct validity, Dr Heba Elkeshishy PhD, Dr Ahmed Desouki MSc, and Dr Mahmoud Abu rehab PhD; and the volunteer researchers as well.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Baumeister H, Härter M. Prevalence of mental disorders based on general population surveys. Soc Psychiatry Psychiatr Epidemiol. 2007;42(7):537–546. doi:10.1007/s00127-007-0204-1
2. Schomerus G, Schwahn C, Holzinger A, et al. Evolution of public attitudes about mental illness: a systematic review and meta-analysis. Acta Psychiatr Scand. 2012;125(6):440–452. doi:10.1111/j.1600-0447.2012.01826.x
3. Bhugra D. Attitudes towards mental illness. A review of the literature [review]. Acta Psychiatr Scand. 1989;80(1):1–12. doi:10.1111/j.1600-0447.1989.tb01293.x
4. Ciftci A, Jones N, Corrigan PW. Mental health stigma in the muslim community. J Muslim Ment Health. 2013;7(1). doi:10.3998/jmmh.10381607.0007.102
5. Dessoki HH, Hifnawy TM. Beliefs about mental illness among university students in Egypt. Eur J Psychol. 2009;5(1). doi:10.5964/ejop.v5i1.284
6. Pew Research Center, Cornell University. Public attitudes about mental health. [Internet]. 2015 [cited April 28, 2015]. Available from http://ropercenter.cornell.edu/public-attitudes-mental-health/.
7. Angermeyer MC, Matschinger H. Public attitude towards psychiatric treatment. Acta Psychiatr Scand. 1996;94(5):326–336. doi:10.1111/j.1600-0447.1996.tb09868.x
8. Angermeyer MC, Matschinger H, Schomerus G. Attitudes towards psychiatric treatment and people with mental illness: changes over two decades. Br J Psychiatry. 2013;203(2):146–151. doi:10.1192/bjp.bp.112.122978
9. Evans-Lacko S, Corker E, Williams P, et al. Effect of the time to change anti-stigma campaign on trends in mental-illness-related public stigma among the english population in 2003–13: an analysis of survey data. Lancet Psychiatry. 2014;1(2):121–128. doi:10.1016/s2215-0366(14)70243-3
10. Marrow J, Luhrmann TM. The zone of social abandonment in cultural geography: on the street in the United States, inside the family in India. Cult Med Psychiatry. 2012;36(3);493–513.
11. Rahman F. Health and Medicine in the Islamic Tradition. Chicago: ABC International Group, Inc.; 1998.
12. Koenig HG, Zaben F, Sehlo MG, et al. Mental health care in Saudi Arabia: past, present and future. Open J Psychiatry. 2014;4(2):113–130. doi:10.4236/ojpsych.2014.42016
13. Al-Khathami AD, Ogbeide DO. Prevalence of mental illness among Saudi adult primary-care patients in Central Saudi Arabia. Saudi Med J. 2002;23(6):721–724.
14. Alosaimi FD, Alshehri Y, Alfraih I, et al. Prevalence of psychiatric disorders among visitors to faith healers in Saudi Arabia. Pak J Med Sci. 2014;30(5):1077–1082. doi:10.12669/pjms.305.5434
15. Almutairi AF. Mental illness in Saudi Arabia: an overview. Psychol Res Behav Manag. 2015;8:47–49. doi:10.2147/prbm.s79268
16. Rayan A, Jaradat A. Stigma of mental illness and attitudes toward psychological help-seeking in Jordanian University Students. Res Psychol Behav Sci. 2016;4(1):7–14. doi:10.12691/rpbs-4-1-2
17. El-Gilany H, Amr M, Iqbal R. Students‘ attitudes toward psychiatry at Al-Hassa Medical College, Saudi Arabia. Acad Psychiatry. 2010;34(1):71–74. doi:10.1176/appi.ap.34.1.71
18. AlAdawi S, Atsu S, Dorvlo A-ISS, et al. Perception of and attitude towards mental illness in Oman. Int J Soc Psychiatry. 2003;48(4):305–317. doi:10.1177/002076402128783334
19. Koenig HG, Al Zaben F, Sehlo MG, Khalifa DA, Al Ahwal MS. Current state of psychiatry in saudi Arabia. Int J Psychiatry Med. 2013;46(3):223–242. doi:10.2190/pm.46.3.a
20. Qureshi A, Al-Habeeb AA, Koenig HG. Mental health system in Saudi Arabia: an overview. Neuropsychiatr Dis Treat. 2013;9:1121–1135. doi:10.2147/ndt.s48782
21. Angermeyer MC, Dietrich S. Public beliefs about and attitudes towards people with mental illness: a review of population studies. Acta Psychiatr Scand. 2006;113(3):163–179. doi:10.1111/j.1600-0447.2005.00699.x
22. Tang AC. Cross-sectional survey: public attitude toward mental illness in China. Int Arch Nurs Health Care. 2015;1(1):3. doi:10.23937/2469-5823/1510025
23. Angermeyer MC, Matschinger H, Patrick W. Familiarity with mental illness and social distance from people with schizophrenia and major depression: testing a model using data from a representative population survey. Schizophr Res. 2004;69(2,3):175–182. doi:10.1016/s0920-9964(03)00186-5
24. Angermeyer MC, Auwera SV, Carta MG, Schomerus G. Public attitudes towards psychiatry and psychiatric treatment at the beginning of the 21st century: a systematic review and meta-analysis of population surveys. World Psychiatry. 2017;16(1):50–61. doi:10.1002/wps.20383
25. Melissa C, Marvaki C, Gourni M, Tsalkanis A, Pilatis N. People’s attitudes towards patients with mental illness in Greece. 2004;27. Available from: www.nursing.gr.
26. World Health Organization. WHO Mental Health Gap Action Program (Mhgap). Geneva: World Health Organization; 2013.
27. World Health Organization. Mental Health Atlas 2011. Geneva: World Health Organization; 2011:82.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
