Back to Journals » International Journal of General Medicine » Volume 16
A Simplified Risk Score to Predict In-Hospital Newly-Diagnosed Atrial Fibrillation in Acute Ischemic Stroke Patients
Authors Saengmanee T, Thiankhaw K , Tanprawate S, Soontornpun A, Wantaneeyawong C, Teekaput C, Sirimaharaj N, Nudsasarn A
Received 15 February 2023
Accepted for publication 11 April 2023
Published 18 April 2023 Volume 2023:16 Pages 1363—1373
DOI https://doi.org/10.2147/IJGM.S406546
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Thanachporn Saengmanee,1,* Kitti Thiankhaw,1,2,* Surat Tanprawate,1,2 Atiwat Soontornpun,1,2 Chayasak Wantaneeyawong,1,2 Chutithep Teekaput,1,2 Nopdanai Sirimaharaj,1,2 Angkana Nudsasarn2
1Division of Neurology, Department of Internal Medicine, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand; 2The Northern Neuroscience Centre, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand
*These authors contributed equally to this work
Correspondence: Kitti Thiankhaw, Division of Neurology, Department of Internal Medicine, Faculty of Medicine, Chiang Mai University, 110, Inthawaroros Road, Sriphum, Chiang Mai, 50200, Thailand, Tel +66 5393 5899, Fax +66 5393 5481, Email [email protected]; [email protected]
Purpose: Atrial fibrillation (AF) is a significant cause of stroke, and newly diagnosed AF (NDAF) is typically detected in the early period of stroke onset. We aimed to identify the factors associated with in-hospital NDAF in acute ischemic stroke patients and developed a simplified clinical prediction model.
Methods: Patients with cryptogenic stroke aged 18 years or older who were admitted between January 2017 and December 2021 were recruited. NDAF was determined by inpatient cardiac telemetry. Univariable and multivariable regression analyses were used to evaluate the factors associated with in-hospital NDAF. The predictive model was developed using regression coefficients.
Results: The study enrolled 244 eligible participants, of which 52 NDAFs were documented (21.31%), and the median time to detection was two days (1– 3.5). After multivariable regression analysis, parameters significantly associated with in-hospital NDAF were elderly (> 75 years) (adjusted Odds ratio, 2.99; 95% confident interval, 1.51– 5.91; P = 0.002), female sex (2.08; 1.04– 4.14; P = 0.04), higher admission national institute of health stroke scale (1.04; 1.00– 1.09; P = 0.05), and presence of hyperdense middle cerebral artery sign (2.33; 1.13– 4.79; P = 0.02). The area under the receiver operating characteristic curve resulted in 0.74 (95% CI 0.65– 0.80), and the cut-point of 2 showed 87% sensitivity and 42% specificity.
Conclusion: The validated and simplified risk scores for predicting in-hospital NDAF primarily rely on simplified parameters and high sensitivity. It might be used as a screening tool for in-hospital NDAF in stroke patients who initially presumed cryptogenic stroke.
Keywords: acute ischemic stroke, newly diagnosed atrial fibrillation, clinical prediction model, risk scoring
Introduction
Stroke is still an important public health issue nowadays due to disability and mortality, especially ischemic stroke shows 80% of all strokes.1 Manipulation of unmodifiable and potentially modifiable risk factors contributed to decreased recurrence events in ischemic stroke.2 Cardioembolic stroke etiology is found following large-artery atherosclerosis and small-vessel occlusion or lacune.3 A Wernicke’s aphasia or global aphasia without hemiparesis, a Valsalva maneuver at the moment of stroke onset, the co-occurrence of cerebral and systemic emboli, and abrupt onset to the maximal deficit are some clinical characteristics that have been suggestive of cardioembolic stroke, whilst lacunar clinical presentations, and especially multiple lacunar infarcts, make cardioembolic origin unlikely.4 Previous Thai and Asian studies have shown that cryptogenic stroke or stroke of undetermined etiology, according to the Trial of ORG 10172 in Acute Stroke Treatment (TOAST) classification, is 20 to 40% of all strokes,5 and antiplatelet is the mainstay treatment for cryptogenic stroke.6 On the contrary, anticoagulation is appropriate for secondary stroke prevention for ischemic stroke patients with atrial fibrillation.7
Newly diagnosed trial fibrillation (NDAF) was detected in approximately ten percent of all strokes, and the most common period to detect it was within 72 hours from stroke onset.8 Many studies, like the EMBRACE and CRYSTAL trials, evaluated invasive and noninvasive cardiac monitoring to detect NDAF.9,10 While in an ischemic stroke or transient ischemic event, NDAF frequently has quite a paroxysmal pattern. Although several risk scores for predicting NDAF following an ischemic stroke or transient ischemic attack (TIA) were developed, the usefulness of these scores to anticipate NDAF in clinical practice is still uncertain since the established risk scores performed inconsistently in terms of their detection accuracy.11 Moreover, in Thailand and many countries that encountered resource-limited facilities, accession to outpatient or long-term cardiac monitoring for every stroke patient was limited.12–15 Therefore, our objective was to identify the factors that predict in-hospital NDAF in acute ischemic stroke patients and to develop a simplified risk score to predict NDAF and select the patients for proper cardiac monitoring. Moreover, the additional outcomes were used to evaluate the incidence of NDAF detection during admission and the mean duration of NDAF detection during the in-hospital period.
Materials and Methods
Study Population
The retrospective study was conducted at Maharaj Nakorn Chiang Mai Hospital, a large tertiary care hospital of the Faculty of Medicine, Chiang Mai University. The Institutional Review Board of the Faculty of Medicine, Chiang Mai University, approved this study protocol (Study Code: MED-2565-08890). Acute ischemic stroke patients who were admitted to the Acute Stroke Unit between January 2017 and December 2021, initially diagnosed with cryptogenic ischemic stroke, defined as symptomatic cerebral infarcts, with no known plausible etiology at initial diagnostic evaluation,16 and aged 18 years or over were enrolled in the study. Stroke was described as a sudden onset of focal neurological deficit in a brain location attributed to the consistent vascular territory. The other types of strokes, which were large-artery atherosclerosis (LAA), cardioembolism (CE), small-vessel occlusion (SVO or lacune), and stroke of other determined etiology, were excluded. Also, patients with previous or first AF diagnosed at the Emergency Department were excluded from the study (Figure 1).
 |
Figure 1 Study flow chart and patient selection procedure. |
Data Collection and Outcomes
The primary study outcome is newly-diagnosed atrial fibrillation (NDAF), defined as a new-onset AF developed during hospitalization, which was detected by 12-lead electrocardiography (ECG), inpatient cardiac telemetry, or echocardiography. The data were collected from electronic medical records, including demographic characteristics, medical history, laboratory data, stroke severity, electrocardiographic parameters, echocardiographic parameters, cardio-thoracic ratio, and neuroimaging parameters. Stroke severity was evaluated by the National Institute of Health Stroke Scale (NIHSS) and modified Rankin Scale (mRS) on admission. Electrocardiographic parameters contained P-wave terminal force in V1 (PTFV1) (Figure 2A–C) and P-wave dispersion (PWD) (Figure 3A–C), which was measured from the surface ECG using WebPlotDigitizer version 4.6 (https://automeris.io/WebPlotDigitizer).17 Left atrial diameter (LADM) and left ventricular ejection fraction (LVEF) were collected from the official echocardiography report by a certified board cardiologist. Neuroimaging parameters, including hyperdense middle cerebral artery sign (HMCAS) refers to focal hyperdensity of the MCA on brain noncontrast computed tomography (NCCT),18 cortical lesion, scatter lesion, and hemorrhagic transformation, were obtained from the official radiographic report by a certified board neuroradiologist and were blinded to the study outcomes.
Statistical Analysis
Categorical variables are reported as numbers with proportions and evaluated by Pearson χ2 test or Fisher exact 2-sided test when appropriate. If continuous variables are in a normal distribution, it is presented as mean with standard deviation (SD) and evaluated by a two-tailed Student’s t-test. On the other hand, for abnormal distribution of continuous variables, it is reported as median with interquartile range (IQR) and comparison between the two groups by Mann–Whitney U (Wilcoxon rank sum) test. Univariable analysis was presented with an odds ratio (OR) with a 95% confidence interval (CI), and variables with statistical significance or P-value less than 0.2 or considered as clinical significance were used in multivariable logistic regression analysis. Regarding the predictive score, the significant predictors were weighted by their coefficient and valued for specificity and sensitivity using receiver operating characteristic (ROC) curve plotting. The area under the receiver operating characteristic (AuROC) was also calculated to evaluate the test accuracy. All P-values were considered statistically significant when they were less than 0.05. All analyses were performed using licensed Stata statistical software version 16.1.
Results
Demographics and Parameters
A total of 244 eligible patients were enrolled in the study. Fifty-two stroke patients with NDAF detected were hospitalized with a mean duration of NDAF detection of three days after the stroke onset. The baseline characteristics are shown in Table 1 between patients with or without NDAF. The NDAF group showed a significant 10.8 years higher age (74.6 vs 63.8 years, P < 0.001), predominately female, higher admission NIHSS (16 vs 11 points, P = 0.001), mild lower hemoglobin levels, and lesser low-density lipoprotein-cholesterol (LDL-C) levels. The other characteristics were not significantly different. Table 2 shows cardiac biomarkers, electrocardiography, echocardiography, and neuroimaging parameters of the patients between the two groups. The patients with NDAF have a higher high-sensitivity troponin T (hs-TnT) level (17 vs 13 ng/L, P = 0.03), larger LADM (39.9 vs 35 mm, P < 0.001), higher cardio-thoracic ratio (61.0 vs 56.9, P < 0.001), the more frequent presence of HMCAS (67.3% vs 45%, P = 0.004) and the more frequent presence of hemorrhagic transformation.
 |
Table 1 Baseline Characteristics of the Patients |
 |
Table 2 Cardiac Biomarkers, Electrocardiography, Echocardiography, and Neuroimaging Parameters of the Patients |
Regression Analysis
Univariable analysis and multivariable logistic regression analysis are shown in Tables 3, 4, and Supplementary Table S1. Four significant independent variables for univariable analysis include age, female sex, admission NIHSS score, and HMCAS. After multivariable logistic regression was analyzed, they were still potent, including age greater than or equal to 75 (adjusted odds ratio (aOR), 2.99; 95% confident interval (CI), 1.51–5.91; P = 0.002), female sex (2.08; 1.04–4.14; P = 0.04), admission NIHSS score (1.04; 1.00–1.09; P = 0.05), and HMCAS/MCA dot sign (2.33; 1.13–4.79; P = 0.02).
 |
Table 3 Univariable Analysis |
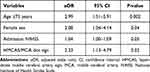 |
Table 4 Multivariable Analysis |
Model Development
All four significant predictors were assigned to item scores for in-hospital NDAF by calculated coefficients and are shown in Table 5. Firstly, age in years was divided into two groups (greater than or equal to 75 = 1, less than 75 = 0). Females were 1, and male was 0. Admission NIHSS score was divided into two groups (greater than or equal to 8 = 1, 0 to 7 = 0). For HMCAS/MCA dot sign, presence = 1, and absence = 0.
 |
Table 5 Significant Predictors and Assigned Item Scores for In-Hospital Newly Diagnosed Atrial Fibrillation |
Model Validation
To test the accuracy of the predictive score, the receiver operating characteristic analysis (ROC) is performed in Figure 4. The area under the receiver operating characteristics (AuROC) curve is 0.74 (95% CI 0.65–0.80), which can be interpreted as the fair diagnostic accuracy of the test. The Hosmer–Lemeshow test, a tool for testing goodness of fit for logistic regression models, shows the lowest line corresponding to the predicted population, which means that the test has good calibration (Supplementary Figure S1). From Supplementary Table S2, the cut-point at two shows that the sensitivity is 86.54%, while the specificity is 42.31%, the positive predictive value (PPV) of 30.00% (26.67–33.56), and a negative predictive value (NPV) of 91.67% (84.40–95.72). This shows high sensitivity to detect NDAF as a screening tool. The odds ratio of a cut point of 2 is 1.5 (95% CI 0.91–2.45; P = 0.09). While a score of 0 to 1 shows an odds ratio of 0.32 (0.12–0.75; P = 0.005) (Supplementary Table S3) which means that a lower score than the cut-point of two is less for in-hospital NDAF detection.
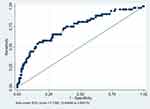 |
Figure 4 Area under receiver operating characteristics (AuROC) curve. |
Discussion
Since AF is a potential risk for stroke, AF detection is beneficial for stroke patients and affects suitable medication for secondary prevention as anticoagulants.7 Also, early recurrent embolization is one of the most important indicators of in-hospital mortality in acute ischemic stroke patients due to AF.19 Interestingly, long-term cardiac monitoring has some limitations in detecting NDAF, including accessibility and unaffordability.12 Thus, we aim to study the risk factors which predict in-hospital NDAF in acute ischemic stroke patients who performed cardiac monitoring during admission and to develop a simplified risk score to choose high-risk candidates for the benefits of further cardiac monitoring. Our study focused on baseline demographics in almost ischemic stroke patients and demonstrated that significant variables for NDAF were age greater than or equal to 75, female sex, admission NIHSS score greater than or equal to eight, and presence of HMCAS/MCA dot sign after univariable analysis and multivariable logistic regression analysis. Some variables with statistical significance, elevated hemoglobin, might not be correlated with the risk of atrial fibrillation due to U-shaped association and were not utilized in the final model development.20 Each parameter got one score by its coefficients. The accuracy of the predictive score with a cut-point of two was an acceptable performance, and also good calibration was shown by the Hosmer–Lemeshow test. Thus, this predictive score is satisfactory for the screening tool to detect in-hospital NDAF in acute ischemic stroke patients who were initially presumed cryptogenic stroke etiology.
Compared to previous studies, the iPAB score contains three parameters, including those identified by the history of arrhythmia or antiarrhythmic agent use, atrial dilation, defined as a diameter greater than 40 millimeters, and B-type natriuretic peptide (BNP) elevation. For an increase in BNP levels, if the value was greater than or equal to 50, 90, and 150 picograms per milliliter, there were 1, 2, and 3 points, respectively.21 Regarding the HAVOC score, there are hypertension, age, valvular heart disease, peripheral vascular disease, obesity, congestive heart failure, and coronary artery disease.21–23 The iPAB score was developed using Asian populations with a sensitivity of 93% and a specificity of 71% with a total score above 2. The HAVOC score, on the other hand, was based on European populations. The accuracy of the score was 78.0%, and the area under the curve was 68.7% (95% CI, 62.1–73.3%). The relevant parameter with our findings was old age, but the difference was a neuroimaging parameter which was interesting and supported the results of the previous study on the relationship between HMCAS/MCA dot sign and acute ischemic stroke etiology.18,24 HMCAS can be found by brain NCCT in 59% of patients with cardioembolism, according to the TOAST classification, even though it cannot be used solely as a marker for determining the subtypes of stroke etiology.25 Hemorrhagic transformation (HT) is another interesting neuroimaging parameter for which our findings found the association with NDAF from the univariable analysis with marginal nonstatistical significance. The study on the early hemorrhagic transformation of brain infarction, which was prospectively conducted by Paciaroni et al, found cardioembolism to be a predictor of HT with an odds ratio of 2.36 (95% CI 1.44–3.68), and the magnitude of the effect is more pronounced with parenchymal hemorrhage (PH) (5.25, 2.27–12.14).26 These findings highlighted the usefulness of neuroimaging markers together with other clinical parameters to identify acute ischemic stroke patients with probable NDAF.
Although the incidence of AF is more significant in men than women, recent studies have shown a higher prevalence of female AF patients than in males.27–29 This condition might be because women typically live longer than men. Therefore, the female gender can be a potential risk factor for NDAF, corresponding with the elderly age found in our cohort. For a higher NIHSS score which indicates the severity of a stroke, severe stroke is also associated with large vessel cardioembolism from AF, as correlated with many previous studies.30,31 Cardioembolic stroke is typically presented with total or partial anterior circulation infarction, TACI, or PACI, respectively, according to the Oxfordshire Community Stroke Project (OCSP) clinical stroke classification, which resulted in a significant disabling stroke on admission.32,33
ECG parameters, including PTFV1 and PWD, are widely recognized as suggestive of atrial enlargement, which is related to a higher risk for NDAF.34–37 Bayes syndrome, an under-recognized clinical condition defined by advanced interatrial block, should be taken into consideration and examined as a potential cause of cryptogenic stroke. It may be the cause of cryptogenic ischemic strokes.38 Our findings found more elevated markers of atrial cardiopathy, hs-TnT, and LADM, although these findings did not correspond to focused ECG parameters, PTFV1 and PWD. We aimed to enhance the measurement accuracy by using WebPlotDigitizer, but the aberration still occurred and resulted in nondifference between groups with and without NDAF. It might be implied that these ECG markers of atrial dysfunction are still needed further investigation for clinical application. Moreover, for the secondary outcome, in our cohort, approximately one-fifth of patients who initially presumed cryptogenic stroke were identified with NDAF (52 among 244 participants, 21.3%). In addition, we found that the common period to detect NDAF was two days after the symptoms of stroke onset, with an interquartile range from one to three and a half days. The earliest is within the first day after admission and goes to day twelfth for the maximum detection. Our results have corresponded with the previous studies that found the diagnosis of atrial fibrillation, even serious cardiac arrhythmias following stroke, is usually established within 72 hours.8,39,40 These emphasize the essentials of in-hospital cardiac monitoring, and patients with the characteristics mentioned above have a high probability of being NDAF.
To the present, there are increased data on the cost-effectiveness of screening for atrial fibrillation among the general population and in a particular subgroup, especially after ischemic stroke. A study by Schnabel et al demonstrated that AF was identified in approximately 0.2% of the middle-aged population using a single timepoint 12-lead ECG screening, but those 65 years of age and above may achieve cost-effectiveness for screening.41 This is consistent with an analysis from the STROKESTOP study that showed that a broad AF screening strategy in an elderly population is cost-effective.42 In individuals after ischemic stroke, due to its higher expenses and decreased sensitivity, continuous 24 h ECG recording was less cost-effective than intermittent ECG.43 Our results highlight the importance of clinical prediction models as a clinical utility tool to investigate silent AF in patients recently suffering from acute ischemic stroke.
There are many strengths of our study. Firstly, our study was based on the population we were interested in, and the parameters were generally suitable. Additionally, the predictive score, which contains four parameters, is simplified to remember and be applicable. Due to its good calibration quality, it can be used as a screening tool for patients with a higher yield for NDAF detection. Finally, we attempted to use an objective measurement of PTFV1 and PWD, the WebPlotDigitizer, instead of an isolated manual measurement, even if these ECG parameters were not significant in our study. Regarding these strengths, our simplified risk scoring is feasible for further exploration in external validation models. It might have an implication in clinical practice as a screening tool to select acute cryptogenic ischemic stroke who might be resulted in high diagnostic yield in resource-limited settings.
However, we acknowledged some limitations of the present study. Some missing data have occurred because of the retrospective study, and a conducting prospective study in the future may be more suggestive. Second, the number of patients included in our study was relatively small due to a single-center retrospective study. If the magnitude of the total population was larger, some parameters might show statistical significance. Lastly, although our predictive score produced a high-sensitivity yield, which makes it suitable for a screening tool, the specificity of the cut point is quite fair. We encourage further well-controlled prospective studies to establish a definite predictive yield regarding the independent parameters found in this study.
Conclusions
Regarding the findings of the current study, we have developed and validated the simplified risk score to predict in-hospital newly-diagnosed atrial fibrillation in acute ischemic stroke patients contains four parameters which are elderly age, female sex, higher admission NIHSS score, and presence of HMCAS/MCA dot sign purpose to screen and select candidates for further cardiac monitoring to increase the yield of the NDAF detection, especially within the first forty-eight hours after the stroke onset. NDAF remains an important etiology of ischemic stroke, initially cryptogenic, accounting for 21.3% in our cohort, and applying the aforementioned clinical parameters increased the chance of detecting acute ischemic stroke patients with occult or transient cardiac arrhythmias. To determine the significance of such scores for clinical decision-making and preventive intervention, additional research with large prospective cohorts and randomized control trials is needed.
Data Sharing Statement
The authors confirm that the data supporting the findings of this study are available within the article and its Supplementary Materials. The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethical Approval and Informed Consent
The Research Ethics Committees of the Faculty of Medicine, Chiang Mai University, approved this study protocol (Study Code: MED-2565-08890). The requirement for informed consent was waived because the retrospective and non-interventional study collected data from the previous electronic medical record and did not involve personal privacy and commercial interests. The study involves no more than minimal risk to subjects, and the waiver will not adversely affect the rights and welfare of the subjects. The data were anonymized or maintained with confidentiality. The publication of this study follows the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funding was received for carrying out this study and preparing the manuscript.
Disclosure
The authors have no conflicts of interest in this work to declare.
References
1. Tsao CW, Aday AW, Almarzooq ZI, et al. Heart disease and stroke statistics-2022 update: a report from the American Heart Association. Circulation. 2022;145(8):e153–e639. doi:10.1161/CIR.0000000000001052
2. Juli C, Heryaman H, Ang E-T, Defi IR, Gamayani U, Atik N. The number of risk factors increases the recurrence events in ischemic stroke. Eur J Med Res. 2022;27(1):1–7. doi:10.1186/s40001-022-00768-y
3. Suwanwela NC. Stroke epidemiology in Thailand. J Stroke. 2014;16(1):1. doi:10.5853/jos.2014.16.1.1
4. Arboix A, Oliveres M, Massons J, Pujades R, García‐Eroles L. Early differentiation of cardioembolic from atherothrombotic cerebral infarction: a multivariate analysis. Eur J Neurol. 1999;6(6):677–683. doi:10.1046/j.1468-1331.1999.660677.x
5. Kolominsky-Rabas PL, Weber M, Gefeller O, Neundoerfer B, Heuschmann PU. Epidemiology of ischemic stroke subtypes according to TOAST criteria: incidence, recurrence, and long-term survival in ischemic stroke subtypes: a population-based study. Stroke. 2001;32(12):2735–2740. doi:10.1161/hs1201.100209
6. Jauch EC, Saver JL, Adams HP, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870–947. doi:10.1161/STR.0b013e318284056a
7. Kamel H, Healey JS. Cardioembolic stroke. Circ Res. 2017;120(3):514–526. doi:10.1161/CIRCRESAHA.116.308407
8. Sposato LA, Klein FR, Jáuregui A, et al. Newly diagnosed atrial fibrillation after acute ischemic stroke and transient ischemic attack: importance of immediate and prolonged continuous cardiac monitoring. J Stroke Cerebrovasc Dis. 2012;21(3):210–216. doi:10.1016/j.jstrokecerebrovasdis.2010.06.010
9. McCarthy L. Ambulatory ECG monitoring for 30 d increased AF detection more than 24 h of ECG monitoring after cryptogenic stroke. Ann Intern Med. 2014;161(10):JC2. doi:10.7326/0003-4819-161-10-201411180-02002
10. Sanna T, Diener H-C, Passman RS, et al. Cryptogenic stroke and underlying atrial fibrillation. N Engl J Med. 2014;370(26):2478–2486. doi:10.1056/NEJMoa1313600
11. Kishore AK, Hossain MJ, Cameron A, Dawson J, Vail A, Smith CJ. Use of risk scores for predicting new atrial fibrillation after ischemic stroke or transient ischemic attack—a systematic review. Int J Stroke. 2022;17(6):608–617. doi:10.1177/17474930211045880
12. Onder H, Yilmaz S. The rationale of holter monitoring after stroke. Angiology. 2017;68(10):926–927. doi:10.1177/0003319717703003
13. Kausar SA. The latest national clinical guideline for stroke. Clin Med. 2017;17(4):382–383. doi:10.7861/clinmedicine.17-4-382
14. Sutamnartpong P, Dharmasaroja PA, Ratanakorn D, Arunakul I. Atrial fibrillation and paroxysmal atrial fibrillation detection in patients with acute ischemic stroke. J Stroke Cerebrovasc Dis. 2014;23(5):1138–1141. doi:10.1016/j.jstrokecerebrovasdis.2013.09.032
15. Lee SH, Sun Y. Detection and predictors of paroxysmal atrial fibrillation in acute ischemic stroke and transient ischemic attack patients in Singapore. J Stroke Cerebrovasc Dis. 2015;24(9):2122–2127. doi:10.1016/j.jstrokecerebrovasdis.2015.05.021
16. Saver JL, Solomon CG. Cryptogenic stroke. N Engl J Med. 2016;374(21):2065–2074. doi:10.1056/NEJMcp1503946
17. He J, Tse G, Korantzopoulos P, et al. P-wave indices and risk of ischemic stroke: a systematic review and meta-analysis. Stroke. 2017;48(8):2066–2072. doi:10.1161/STROKEAHA.117.017293
18. Barber PA, Demchuk AM, Hudon ME, Pexman JHW, Hill MD, Buchan AM. Hyperdense sylvian fissure mca “dot” sign. Stroke. 2001;32(1):84–88. doi:10.1161/01.STR.32.1.84
19. Arboix A, García-Eroles L, Massons J, Oliveres M. Predictive clinical factors of in-hospital mortality in 231 consecutive patients with cardioembolic cerebral infarction. Cerebrovasc Dis. 1998;8(1):8–13. doi:10.1159/000015809
20. Lim W-H, Choi E-K, Han K-D, Lee S-R, Cha M-J, Oh S. Impact of hemoglobin levels and their dynamic changes on the risk of atrial fibrillation: a nationwide population-based study. Sci Rep. 2020;10(1):1–8. doi:10.1038/s41598-019-56847-4
21. Yoshioka K, Watanabe K, Zeniya S, et al. A score for predicting paroxysmal atrial fibrillation in acute stroke patients: iPAB score. J Stroke Cerebrovasc Dis. 2015;24(10):2263–2269. doi:10.1016/j.jstrokecerebrovasdis.2015.06.019
22. Favilla CG, Ingala E, Jara J, et al. Predictors of finding occult atrial fibrillation after cryptogenic stroke. Stroke. 2015;46(5):1210–1215. doi:10.1161/STROKEAHA.114.007763
23. Kwong C, Ling AY, Crawford MH, Zhao SX, Shah NH. A clinical score for predicting atrial fibrillation in patients with cryptogenic stroke or transient ischemic attack. Cardiology. 2017;138(3):133–140. doi:10.1159/000476030
24. Na Songkhla K, Tantirittisak T, Hanchaiphiboolkul S, Wattanasen Y. Relationship between the ischemic stroke subtypes and risk factors included clinical outcome from Prasat Neurological Institute stroke registry. J Thai Stroke Soc. 2019;13(1–2):3–12.
25. Sangpetch S, Wantaneeyawong C, Soontornpun A, Tiyapun N, Tanprawate S, Thiankhaw K. Implications of the presence of hyperdense middle cerebral artery sign in determining the subtypes of stroke etiology. Stroke Res Treat. 2021;2021:6593541. doi:10.1155/2021/6593541
26. Paciaroni M, Agnelli G, Corea F, et al. Early hemorrhagic transformation of brain infarction: rate, predictive factors, and influence on clinical outcome: results of a prospective multicenter study. Stroke. 2008;39(8):2249–2256. doi:10.1161/STROKEAHA.107.510321
27. Ko D, Rahman F, Schnabel RB, Yin X, Benjamin EJ, Christophersen IE. Atrial fibrillation in women: epidemiology, pathophysiology, presentation, and prognosis. Nat Rev Cardiol. 2016;13(6):321–332. doi:10.1038/nrcardio.2016.45
28. Piccini JP, Hammill BG, Sinner MF, et al. Incidence and prevalence of atrial fibrillation and associated mortality among Medicare beneficiaries, 1993–2007. Circ Cardiovasc Qual Outcomes. 2012;5(1):85–93. doi:10.1161/CIRCOUTCOMES.111.962688
29. Tamirisa KP, Dye C, Ekeruo I, Volgman AS. Atrial fibrillation in women: from epidemiology to treatment. Curr Cardiovasc Risk Rep. 2022;16(12):207–217. doi:10.1007/s12170-022-00707-w
30. Figueiredo MM, Rodrigues AC, Alves MB, Neto MC, Silva GS. Score for atrial fibrillation detection in acute stroke and transient ischemic attack patients in a Brazilian population: the acute stroke atrial fibrillation scoring system. Clinics. 2014;69(4):241–246. doi:10.6061/clinics/2014(04)04
31. Lee JD, Kuo YW, Lee CP, Huang YC, Lee M, Lee TH. Development and validation of a novel score for predicting paroxysmal atrial fibrillation in acute ischemic stroke. Int J Environ Res Public Health. 2022;19(12):7277.
32. Bamford J, Sandercock P, Dennis M, Burn J, Warlow C. Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet. 1991;337(8756):1521–1526. doi:10.1016/0140-6736(91)93206-O
33. Travis LH, Flemming KD, Brown RD, Meissner I, McClelland RL, Weigand SD. Awareness of stroke risk factors, symptoms, and treatment is poor in people at highest risk. J Stroke Cerebrovasc Dis. 2003;12(5):221–227. doi:10.1016/j.jstrokecerebrovasdis.2003.09.002
34. Li TYW, Yeo LLL, Ho JSY, et al. Association of electrocardiographic P-wave markers and atrial fibrillation in embolic stroke of undetermined source. Cerebrovasc Dis. 2021;50(1):46–53. doi:10.1159/000512179
35. Huang Z, Zheng Z, Wu B, et al. Predictive value of P wave terminal force in lead V1 for atrial fibrillation: a meta-analysis. Ann Noninvasive Electrocardiol. 2020;25(4):e12739. doi:10.1111/anec.12739
36. Acampa M, Lazzerini PE, Martini G. How to identify patients at risk of silent atrial fibrillation after cryptogenic stroke: potential role of p wave dispersion. J Stroke. 2017;19(2):239–241. doi:10.5853/jos.2016.01620
37. Kamel H, Longstreth WT, Tirschwell DL, et al. The AtRial cardiopathy and antithrombotic drugs in prevention after cryptogenic stroke randomized trial: rationale and methods. Int J Stroke. 2019;14(2):207–214. doi:10.1177/1747493018799981
38. Arboix A, Martí L, Dorison S, Sánchez MJ. Bayés syndrome and acute cardioembolic ischemic stroke. World J Clin Cases. 2017;5(3):93. doi:10.12998/wjcc.v5.i3.93
39. Kallmünzer B, Breuer L, Kahl N, et al. Serious cardiac arrhythmias after stroke: incidence, time course, and predictors--a systematic, prospective analysis. Stroke. 2012;43(11):2892–2897. doi:10.1161/STROKEAHA.112.664318
40. Sposato LA, Cipriano LE, Saposnik G, Ruíz Vargas E, Riccio PM, Hachinski V. Diagnosis of atrial fibrillation after stroke and transient ischaemic attack: a systematic review and meta-analysis. Lancet Neurol. 2015;14(4):377–387. doi:10.1016/S1474-4422(15)70027-X
41. Schnabel RB, Wallenhorst C, Engler D, et al. Refined atrial fibrillation screening and cost-effectiveness in the German population. Heart. 2022;108(6):451–457. doi:10.1136/heartjnl-2020-318882
42. Lyth J, Svennberg E, Bernfort L, et al. Cost-effectiveness of population screening for atrial fibrillation: the STROKESTOP study. Eur Heart J. 2022;44(3):196–204. doi:10.1093/eurheartj/ehac547
43. Levin L-Å, Husberg M, Sobocinski PD, et al. A cost-effectiveness analysis of screening for silent atrial fibrillation after ischaemic stroke. Ep Europace. 2015;17(2):207–214. doi:10.1093/europace/euu213
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


