Back to Journals » International Journal of General Medicine » Volume 16
A Retrospective Study on the Three-Port Technique of Laparoscopic Common Bile Duct Exploration for the Management of Cholelithiasis and Choledocholithiasis
Authors Zhao C , Xu Z, Hu W, Ge C, Zhang Z, Dai Z, Zhang S, Tang N, Wang W, Gu J , Chen C , He S
Received 4 April 2023
Accepted for publication 7 August 2023
Published 11 August 2023 Volume 2023:16 Pages 3435—3445
DOI https://doi.org/10.2147/IJGM.S415752
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hossam El-Din Shaaban
Chunlong Zhao,1,2,* Zipeng Xu,1,* Weidong Hu,1,* Chen Ge,1 Zhengwei Zhang,1 Zhengxing Dai,3 Shuo Zhang,4 Neng Tang,4 Weiguo Wang,3 Jiayu Gu,3 Chaobo Chen,1,4,5 Songbing He2
1Department of General Surgery, Xishan People’s Hospital of Wuxi City, Wuxi, People’s Republic of China; 2Department of General Surgery, The First Affiliated Hospital of Soochow University, Suzhou, People’s Republic of China; 3Department of Interventional and Vascular Surgery, Xishan People’s Hospital of Wuxi City, Wuxi, People’s Republic of China; 4Department of Hepatic-Biliary-Pancreatic Surgery, the Affiliated Drum Tower Hospital of Nanjing University Medical School, Nanjing, People’s Republic of China; 5Department of Immunology, Ophthalmology & ORL, Complutense University School of Medicine, Madrid, Spain
*These authors contributed equally to this work
Correspondence: Chaobo Chen; Songbing He, Email [email protected]; [email protected]
Background: Laparoscopic cholecystectomy (LC) with laparoscopic common bile duct exploration (LCBDE) is convenient in treating cholelithiasis and choledocholithiasis due to its advantage of accelerated recovery. This retrospective study aimed to summarize the experience of cholelithiasis and choledocholithiasis treatment via three-port approach of LCBDE in Eastern China.
Methods: Patients diagnosed with cholelithiasis and choledocholithiasis between July 2019 and October 2021 were included. Patients who received LC+LCBDE+primary suturing of the common bile duct (CBD) via a three-port approach were assigned to the LCBDE-P group, and those who received LC+LCBDE+T-tube drainage of CBD comprised the LCBDE-T group. The measurement data were compared between the two groups. P-values < 0.05 indicated statistical significance.
Results: A total of 88 patients were divided into two groups: LCBDE-P (n=50) and LCBDE-T (n=38). Multiple logistic regression analysis showed that LCBDE-P is associated with a shorter length of stay (OR=0.115, 95% CI: 0.040– 0.329, P< 0.001) and lower hospitalization costs (OR=0.120, 95% CI: 0.041– 0.357, P< 0.001). No significant differences between the two groups were detected in the operation time, intraoperative hemorrhage, clearance rate of CBD stones, postoperative liver function, and postoperative complications (P> 0.05).
Conclusion: The three-port approach of LCBDE is a safe and feasible strategy for managing cholelithiasis and choledocholithiasis. Compared to LCBDE-T, LCBDE-P reduces the length of hospital stay and medical costs during hospitalization.
Keywords: cholelithiasis, choledocholithiasis, laparoscopic cholecystectomy, laparoscopic common bile duct exploration, primary suture, T-tube drainage
Introduction
Cholelithiasis and choledocholithiasis are common gastrointestinal digestive diseases that may occur in 4.6–12% of all patients with cholecystectomy.1 Gallstones may enter the common bile duct (CBD) through the cystic duct, forming a state of gallstones combined with CBD stones, causing obstructive biliary tract and obstructive jaundice and leading to acute cholecystitis, cholangitis, or pancreatitis.2 Although laparoscopic cholecystectomy (LC) is the gold standard for symptomatic gallstones, the optimal choice for gallstones combined with CBD stones is debatable Currently, four methods are available for the treatment of cholelithiasis and choledocholithiasis: preoperative endoscopic retrograde cholangiopancreatography (pre-ERCP) plus LC, LC plus laparoscopic common bile duct exploration (LCDBE), LC plus intraoperative ERCP, and LC plus postoperative ERCP.3 However, whether LCBDE or ERCP is the best method to treat cholelithiasis and choledocholithiasis is yet controversial. The British Gastroenterology Society’s recently updated CBD Stones Management Guidelines pointed out no difference in efficacy, mortality, or morbidity between LBCDE and perioperative ERCP.4 The length of hospitalization (days) and total cost differed significantly, while LCBDE may decrease the length of hospitalization day and cost.5 Also, significant differences were noted in postoperative complications: bile leakage after LCBDE vs duodenal papillary sphincter injury after ERCP.6
Recently, an updated meta-analysis confirmed that LCBDE is superior to ERCP+LC in perioperative safety and short- and long-term postoperative efficacy.7 Furthermore, the current meta-analysis showed that LCBDE is safe and feasible regarding perioperative complications, operative conversion rates, operative time, and postoperative efficacy, such as CBD stone clearance rate, length of hospital stay, and stone recurrence rate. This phenomenon suggested that LCBDE is a preferred method for treating gallstones combined with CBD stones. Thus, LCBDE could be a preferred method for treating gallstones combined with the primary suture of CBD or T-tube drainage procedure.8
Although the surgeons decide whether T-tube drainage or primary suture should be used during LCBDE, the decision is controversial.8,9 A previous meta-analysis showed that when the T-tube was not used, the odds ratio of complications was reduced, and no additional benefits were observed.8 Therefore, some postoperative complications may be avoided without T-tube drainage after treating choledocholithiasis via LCBDE, and the patient’s quality of life can also be improved significantly.10 Reportedly, the ability of traditional T-tube drainage to reduce bilirubin is better than that of the primary suture of CBD in the early postoperative period. However, the difference in long-term outcomes between the two groups is not statistically significant.11 Whether these controversies are related to differences in surgical procedures is yet to be elucidated. Typically, minimally invasive surgical treatment of gallstones and CBD stones is safe and reliable, as described in the Tokyo Guidelines 2018.12
With the development of laparoscopic technology, there has been a trend towards four-port LCBDE to three-port LCBDE. Studies have shown that three-port LCBDE reduces labor costs compared to four-port LCBDE, but does not increase the incidence of complications.13 Our team has extensive experience in three-port LCBDE. Therefore, the present study aimed to summarize the treatment experience and efficacy of LCBDE combined with primary suturing of the CBD via a three-port approach to gallstones with extrahepatic biliary duct calculi.
Methods
Study Design
This retrospective study included 88 patients with gallstones combined with CBD stones admitted at Xishan People’s Hospital of Wuxi City in China between July 2019 and October 2021. All the gallstones combined with CBD stones were identified using transabdominal ultrasonography (USG) and magnetic resonance cholangiopancreatography (MRCP) preoperatively. USG was also used to confirm the absence of recurrent choledocholithiasis after surgery. The study was approved by the Ethics Committee of Xishan People’s Hospital of Wuxi City. The requirement for informed consent was waived due to the retrospective design. The study complied with the Declaration of Helsinki.
Inclusion Criteria
(1) The CBD was examined before the operation to show varying degrees of dilation (diameter ≥8 mm); (2) No evident bile duct stenosis, biliary variability, or intrahepatic bile duct stones on preoperative USG or MRCP; (3) No tumors detected in the liver, biliary tract, or pancreatic head in previous examinations; (4) Without manifestations of cholangitis, such as bile duct wall thickening and edema; (5) Laparoscopic duodenal papilla stenosis capacity is N or 0 grade;14 (6) The Minimum age ≥18 years old.
Exclusion Criteria15
(1) Stenosis of the distal CBD or dysfunction of the papillary sphincter was detected preoperatively; (2) Conversion to laparotomy; (3) Acute hepatitis or severe liver damage; (4) Heart, lung, and renal insufficiency in those who cannot tolerate laparoscopic surgery; (5) Those accompanied with a malignant tumor.16,17
Operative Technique
The surgery of LC+LCBDE+primary suture (LCBDE-P) or LC+LCBDE+T-tube drainage (LCBDE-T) was performed using the three-port method by the same surgical team. The patients were under general anesthesia and received tracheal intubation, as described previously.9,18 The T-tube drainage tube was removed 3 weeks after the operation when the T-tube angiography confirmed that the biliary tract was unobstructed after the operation.
All the patients underwent laparoscopic surgery using the “three-port method” (Figure 1A and B): a 10-mm arc-shaped incision at the lower border of the navel was used as the observation port. The main operation port (Trocar, 10 mm) was 20–30 mm below the xiphoid process. The auxiliary operation port (Trocar, 5 mm) was at the intersection of the lower 50 mm below the rib edge and the right anterior axillary line.
LCBDE-P Group
The anterior wall of the CBD was incised approximately 10–15 mm using scissors (Figure 2A). The choledochoscopy was inserted through the main operating port to explore the extrahepatic bile duct (Figure 2B). Subsequently, the calculi were removed with a mesh basket using the Olympus choledochoscopy, and the CBD incision was sutured with a 4–0 absorbable suture in one stage (continuous round-trip) (Figure 3A and B).
 |
Figure 3 Primary continuous suture of CBD. (A and B) The CBD incision was sutured with the 4–0 absorbable thread via a continuous round-trip approach. |
LCBDE-T Group
Suspension and incision of the CBD were performed; the stones were explored and extracted similarly to the LCBDE-P group. A suitable T-tube was selected and fixed into the CBD through the incision, which was closed with 4–0 absorbable sutures using simple interrupted stitching, and the T-tube was threaded out of the abdominal wall via the 10-mm port.
Data Collection
Data, including items of postoperative liver function, postoperative complications, hospitalization day, and medical cost, were collected for both LCBDE-P and LCBDE-T groups during the same period. Both groups were regularly followed up for 6 months via telephone or outpatient clinic, and all these patients were checked postoperatively through USG at 1 and 6 months, independently.
The present study aimed to compare the length of hospital stay, cost, duration of anesthesia, laboratory parameters [white blood cell (WBC) count, total serum bilirubin, alkaline phosphatase (ALP), alanine aminotransferase (ALT), aspartate aminotransferase (AST), gamma-glutamyl transpeptidase (GGT), C-reactive protein (CRP) levels], and clinical outcomes between patients undergoing LC+LCBDE, primary suture of CBD vs T-tube drainage.
Statistical Analysis
The data were analyzed using SPSS 22.0 (IBM, Armonk, NY, USA). The continuous data were expressed as means ± standard deviations and analyzed using Student’s t-test. Categorical data were presented as frequencies and scores and were analyzed using Fisher’s exact test. Univariate and multivariate logistic regression analyses were performed to estimate the odds ratio (OR) and the 95% confidence intervals (CIs) for hospitalization (days) and medical cost (RMB), including operational styles, site of postoperative complications, operative time, intraoperative hemorrhage, stone subtype, gender, age, body weight, preoperative WBCs, preoperative direct bilirubin, preoperative total bilirubin, preoperative ALT, and preoperative AST. The data of hospitalization and medical cost were dichotomized into two groups using median value as the cutoff in logistic regression analysis. P<0.05 indicated statistical significance.
Results
Characteristics of the Patients
A total of 159 patients were diagnosed with gallstones combined with CBD stones at Xishan People’s Hospital of Wuxi City. Of these, 88 were included in this study from July 2019 to October 2021 based on the exclusion and inclusion criteria. Among 159 patients, 3 were excluded due to anesthesia intolerance, and 62 were treated with laparotomy because of factors such as previous abdominal surgery, inability to tolerate laparoscopic surgery, or conversion to laparotomy after the second laparoscopic surgery. A total of 94 patients were treated with LC+LCBDE, of which 6 were excluded because of the conversion to laparotomy. Finally, 38 patients were treated with LCBDE-T, and the remaining 50 were treated with the LCBDE-P process (Figure 4).
 |
Figure 4 Flow diagram. |
No statistically significant differences were detected between-group in parameters, such as gender, age, body weight, WBC count, bellyache, combined gastrointestinal ulcer, pancreatitis, cholangitis, obstructive jaundice, fever, nausea and/or vomiting, direct bilirubin (DB), total bilirubin (TB), ALT, and AST (all P>0.05, Table 1).
 |
Table 1 Characteristic and Clinical Features of Patients |
Analysis of the Intraoperative Characteristics
Compared to the LCBDE-T group, the operative time was shorter in the LCBDE-P group, combined with less intraoperative hemorrhage, but not significantly. The clearance rate of CBD stones in both groups was 100%. Similarly, no statistically significant differences were detected between the two groups detected in the stone subtype of CBD (P>0.05, Table 2).
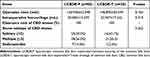 |
Table 2 Analysis of the Intraoperative Characteristics |
Analysis of Postoperative Liver Function
Next, we adjusted the data, representing the preoperative value minus the postoperative value on day 3. The comparison of LCBDE-P with the LCBDE-T group did not show any significant between-group differences, such as ΔDB, ΔTB, ΔALT, and ΔAST (P>0.05, Table 3).
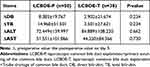 |
Table 3 Analysis for the Characteristics of Postoperative Liver Function in All Patients |
Economic Benefits
Compared to the LCBDE-T group, the length of hospitalization was significantly decreased in the LCBDE-P group. This finding was in line with that of medical costs in the LCBDE-T group vs the LCBDE-P group during the hospitalization (P<0.001, Table 4).
 |
Table 4 Economic Benefits of LCBDE-P vs LCBDE-T |
Postoperative Complications
Two cases of postoperative bile leakage, 1 case of abdominal infection, and 2 cases of abdominal infection were found in the LCBDE-T group; however, no significant differences were detected compared to the LCBDE-P group (P>0.05, Table 5).
 |
Table 5 Postoperative Complications of LCBDE-P vs LCBDE-T |
Analyses of the Length of Stay and Medical Cost During Hospitalization
Logistic regression analyses for the length of stay and medical cost during hospitalization are presented in Table 6 and Table 7. LCBDE-P is an independent factor for a shorter length of stay [odds ratio (OR)=0.115, 95% confidence interval (CI): 0.040–0.329, P<0.001) and decreased hospitalization costs (OR=0.120, 95% CI: 0.041–0.357, P<0.001). Nevertheless, the operative time is an independent risk factor for prolonged hospitalization (OR=1.011, 95% CI: 1.001–1.021, P=0.033) and high hospitalization expense (OR=1.011, 95% CI: 1.000–1.022, P=0.040).
 |
Table 6 Univariable and Multivariable Analysis for the Length of Stay in All Patients |
 |
Table 7 Univariable and Multivariable Analysis for Medical Cost During Hospitalization |
Discussion
LCBDE has been used more frequently today in diagnosing and treating gallstones combined with CBD stones than in the last decade, enriching the experience of surgeons.19 However, using the primary suture of the CBD or T-tube drainage is still controversial.3 The present study aimed to summarize the experience of treating gallstones combined with CBD stones via the three-port approach of LCBDE in a medical center in Eastern China. Compared with LCBDE-T group, LCBDE-P group has shorter length of stay and lower hospitalization costs. The operation time and intraoperative hemorrhage in LCBDE-P group are less than LCBDE-T group but not statistically significant. Meanwhile, no significant differences were detected in the clearance rate of CBD stones, postoperative liver function, and postoperative complications between LCBDE-P group and LCBDE-T group.
The rapid development of minimally invasive technology and the continuous improvement of surgical instruments benefit the patients, including decreased surgical trauma, alleviated pain, and accelerated recovery.20 Therefore, to accomplish LCBDE, three ports were selected in the management approach in our surgical team since July 2019 (Figures 1–3) compared to a fifth port that may be added in addition to the standard four ports, as described previously.15,18 Herein, 88 patients accomplished LCBDE via a three-port method in our hospital, except 6 patients who converted to laparotomy because of unclear anatomy of the Calot triangle (Figure 4).
Since LCBDE was first described in 1991,21 the removal of CBD stones can be performed via two methods: an approach to cystic duct incision or CBD incision according to the characteristics of the patients.22,23 In this study, the patients accepted the approach to CBD incision for removing stones; the clearance rate of the CBD stones was 100% in both groups without a statistically significant difference (Table 2). In clinics, flexible and proficient control of choledochoscopy and tacit cooperation with the assistant surgeon is key in improving CBD stone removal efficiency. Subsequently, repeated choledochoscopy is an effective way to avoid residual CBD stones. In addition, the CBD incision was sutured with a 4–0 absorbable thread in one stage (continuous round-trip) in the LCBDE-P group (Figure 3), performed after the clearance of CBD stones and without postoperative bile leakage, cholangitis, and abdominal infection (P>0.05, Table 5). The choledochotomy was sutured with 4–0 or 5–0 absorbable sutures in a continuous or interrupted manner in the primary suture, after the CBD stones are removed.24 Interestingly, compared to Wang et al,25 the operation time of LCBDE-P was shorter, with less intraoperative hemorrhage than that of LCBDE-T in our study, but without a statistical difference (P>0.05, Table 2). This phenomenon could be attributed to the placement of the T-tube via interrupted suture, thereby requiring more time compared to the primary suture of CBD; also, the T-tube may interfere with the surgeon’s suturing approach, prolonging the operation time. However, patients accomplished continual primary sutures of the CBD depending on their individual characteristics with respect to the indications.16,26 Therefore, this study suggested that the patients received primary suture of the common bile duct or T-tube drainage depending on whether they meet the corresponding indications and should be evaluated by the surgeons.
In the present study, all patients who underwent the LCBDE procedure, irrespective of primary suture or T-tube drainage, were recovered and discharged from the hospital (Table 3 and Table 4). Similarly, the three-port method of LCBDE decreases the scar in the abdomen, as the method is minimally invasive, thereby improving the aesthetics. Simultaneously, the patient’s liver function recovered rapidly after surgery. Thus, the preoperative value minus the postoperative value on day three was expressed as “Δ”, representing the liver function changes pre- and postoperatively. However, no statistical between-group difference was observed in the postoperative liver function (Table 3, P>0.05). Unlike previous studies,25,27,28 we chose postoperative day 3 as the critical variable because most patients recovered soon and were well after the operation, with almost normal liver function on postoperative day 5. Strikingly, compared to the LCBDE-T group, the length of hospitalization and the medical costs were decreased significantly in the LCBDE-P group (P<0.0001, Table 4). Furthermore, both univariate and multivariate regression analyses confirmed that LCBDE-P was an independent factor associated with the length of and medical costs during hospitalization (P<0.0001, Table 6 and Table 7). After three months of follow-up, short-term complications were as follows: 2 cases of postoperative bile leakage, 1 case of abdominal infection, and 2 cases of cholangitis in the LCBDE-T group, but no significant differences were observed compared LCBDE-T group with the LCBDE-P group (P>0.05, Table 5). This finding differed from the recently published results,25 which could be due to the small sample size in our study. For complications, patients with postoperative bile leakage recovered gradually by extending the placement of abdominal drainage tubes and preventing abdominal infection simultaneously. Postoperative abdominal infection and cholangitis patients returned to normal after receiving anti-infection treatment. According to these results, our experience confirmed that the three-port method of LCBDE is safe and feasible. Moreover, the continual primary sutures of the CBD are efficient and economical in treating cholelithiasis and choledocholithiasis under well-controlled indications. Thus, a novel concept of minimally invasive surgical treatment of cholelithiasis has been designed: ultra-minimally invasive, aesthetic, and no-scar.29 Importantly, LCBDE should be carried out by highly selected expert surgeons with advanced experience and technology in minimally invasive biliary tract surgery. Simultaneously, using abdominal puncture Trocars to explore and improve the novel strategy of choledocholithotomy under endoscopy is conducive to embodying the advantages of minimally invasive biliary tract surgery, which might benefit a large number of patients with choledocholithiasis.
Nevertheless, the present study has some limitations. It is a retrospective analysis in a single medical center with only a small number of cases from high-level hospitals, no long-term follow-up, and no comparison group. The heterogeneity is limited, and patients were from the Jiangsu province, lacking a multicenter and regional comparative analysis. Additional feedback from patients undergoing the procedure is needed to promote this strategy.
Conclusions
This study summarized the experience in treating cholelithiasis and choledocholithiasis in a medical center in Eastern China. Despite improved technology, CBD’s three-port method and primary running suture are safe and feasible strategies for treating cholelithiasis and choledocholithiasis. LCBDE-P is an independent factor associated with the length of hospital stay and medical costs during hospitalization in treating patients diagnosed with cholelithiasis and choledocholithiasis.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author (Chaobo Chen) upon reasonable request. For any queries, kindly contact [email protected].
Ethics Approval and Consent to Participate
The need for individual consent was waived by the committee (No. xs2022ky004). This article was a retrospective study, there are no commercial interests involved, patient parental consent to review their medical records was not required by the ethics Committee of Xishan People’s Hospital of Wuxi City. This study strictly kept the patients’ information confidential. The study complied with the Declaration of Helsinki.
Acknowledgments
Chaobo Chen and Songbing He should be considered joint corresponding authors for this study.
Funding
This study was supported by a research project of Wuxi Municipal Health Commission (Project, No. M202160), Project of National Science Foundation of Jiangsu Province of China (BK20191172), Project of Gusu Medical Key Talent of Suzhou City of China (GSWS2020005), and Project of New Pharmaceutics and Medical Apparatuses of Suzhou City of China (SLJ2021007).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Shojaiefard A, Esmaeilzadeh M, Ghafouri A, Mehrabi A. Various techniques for the surgical treatment of common bile duct stones: a meta review. Gastroenterol Res Pract. 2009;2009:840208. doi:10.1155/2009/840208
2. Baiu I, Hawn MT. Choledocholithiasis. JAMA. 2018;320(14):1506. doi:10.1001/jama.2018.11812
3. Ricci C, Pagano N, Taffurelli G, et al. Comparison of efficacy and safety of 4 combinations of laparoscopic and intraoperative techniques for management of gallstone disease with biliary duct calculi: a systematic review and network meta-analysis. JAMA Surg. 2018;153(7):e181167. doi:10.1001/jamasurg.2018.1167
4. Williams E, Beckingham I, El Sayed G, et al. Updated guideline on the management of common bile duct stones (CBDS). Gut. 2017;66(5):765–782. doi:10.1136/gutjnl-2016-312317
5. Muhammedoglu B, Kale IT. Comparison of the safety and efficacy of single-stage endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy versus two-stage ERCP followed by laparoscopic cholecystectomy six-to-eight weeks later: a randomized controlled trial. Int J Surg. 2020;76:37–44. doi:10.1016/j.ijsu.2020.02.021
6. Lyu Y, Cheng Y, Li T, Cheng B, Jin X. Laparoscopic common bile duct exploration plus cholecystectomy versus endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy for cholecystocholedocholithiasis: a meta-analysis. Surg Endosc. 2019;33(10):3275–3286. doi:10.1007/s00464-018-06613-w
7. Pan L, Chen M, Ji L, et al. The safety and efficacy of laparoscopic common bile duct exploration combined with cholecystectomy for the management of cholecysto-choledocholithiasis: an up-to-date meta-analysis. Ann Surg. 2018;268(2):247–253. doi:10.1097/SLA.0000000000002731
8. Yin Z, Xu K, Sun J, et al. Is the end of the T-tube drainage era in laparoscopic choledochotomy for common bile duct stones is coming? A systematic review and meta-analysis. Ann Surg. 2013;257(1):54–66. doi:10.1097/SLA.0b013e318268314b
9. Decker G, Borie F, Millat B, et al. One hundred laparoscopic choledochotomies with primary closure of the common bile duct. Surg Endosc. 2003;17(1):12–18. doi:10.1007/s00464-002-9012-6
10. Guo T, Wang L, Xie P, Zhang Z, Huang X, Yu Y. Surgical methods of treatment for cholecystolithiasis combined with choledocholithiasis: six years’ experience of a single institution. Surg Endosc. 2021;2021:1.
11. Yin Y, He K, Xia X. Comparison of primary suture and T-tube drainage after laparoscopic common bile duct exploration combined with intraoperative choledochoscopy in the treatment of secondary common bile duct stones: a single-center retrospective analysis. J Laparoendosc Adv Surg Tech A. 2021;32:612–619. doi:10.1089/lap.2021.0418
12. Wakabayashi G, Iwashita Y, Hibi T, et al. Tokyo Guidelines 2018: surgical management of acute cholecystitis: safe steps in laparoscopic cholecystectomy for acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25(1):73–86. doi:10.1002/jhbp.517
13. Peixian G, Tao S, Jinwei L, Zhengjun F. Analysis of clinical effects of three-port laparoscopic common bile duct exploration. Henan JSurg. 2022;28(2):1–3.
14. Hua-bo Z, An-ping C, Yi-jia HE, et al. Advances in minimally invasive treatment of laparoscopic common bile duct exploration and primary closure. J Hepatobiliary Pancreat Surg. 2018;30(06):525–528.
15. Quaresima S, Balla A, Guerrieri M, Campagnacci R, Lezoche E, Paganini AM. A 23 year experience with laparoscopic common bile duct exploration. HPB. 2017;19(1):29–35. doi:10.1016/j.hpb.2016.10.011
16. Yi HJ, Hong G, Min SK, Lee HK. Long-term outcome of primary closure after laparoscopic common bile duct exploration combined with choledochoscopy. Surg Laparosc Endosc Percutan Tech. 2015;25(3):250–253. doi:10.1097/SLE.0000000000000151
17. Testoni PA, Mariani A, Aabakken L, et al. Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy. 2016;48(7):657–683. doi:10.1055/s-0042-108641
18. Zerey M, Haggerty S, Richardson W, et al. Laparoscopic common bile duct exploration. Surg Endosc. 2018;32(6):2603–2612. doi:10.1007/s00464-017-5991-1
19. Manes G, Paspatis G, Aabakken L, et al. Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019;51(5):472–491. doi:10.1055/a-0862-0346
20. Huang Y, Feng Q, Wang K, Xiong X, Zou S. The safety and feasibility of laparoscopic common bile duct exploration for treatment patients with previous abdominal surgery. Sci Rep. 2017;7(1):15372. doi:10.1038/s41598-017-15782-y
21. Petelin JB. Laparoscopic approach to common duct pathology. Surg Laparosc Endosc. 1991;1(1):33–41.
22. Fang L, Wang J, Dai WC, et al. Laparoscopic transcystic common bile duct exploration: surgical indications and procedure strategies. Surg Endosc. 2018;32(12):4742–4748. doi:10.1007/s00464-018-6195-z
23. Wang H, Ou Y, Ou J, Jian Z. Contrast of therapeutic effects between CBD incision and LLHD stump in biliary tract exploration of LLS for hepatolithiasis. Surg Endosc. 2020;34(2):915–919. doi:10.1007/s00464-019-06848-1
24. Dietrich A, Alvarez F, Resio N, et al. Laparoscopic management of common bile duct stones: transpapillary stenting or external biliary drainage? JSLS. 2014;18(4):
25. Wang Y, Huang Y, Shi C, et al. Efficacy and safety of laparoscopic common bile duct exploration via choledochotomy with primary closure for the management of acute cholangitis caused by common bile duct stones. Surg Endosc. 2022;36(7):4869–4877. doi:10.1007/s00464-021-08838-8
26. Yang Y, Han L, Lin DN, et al. The safety and efficacy of primary duct closure without endoscopic nasobiliary drainage after laparoscopic common bile duct exploration. Gastrointest Tumors. 2020;7(4):117–124. doi:10.1159/000508874
27. Jiang Y, Lu J, Li W, Zhang J, Li L. Primary closure after laparoscopic common bile duct exploration is safe and feasible for patients with non-severe acute cholangitis. Langenbecks Arch Surg. 2022;407(4):1553–1560. doi:10.1007/s00423-022-02547-z
28. Das S, Jha AK, Kumar M. Laparoscopic common bile duct exploration in cases of common bile duct stones: can LCBDE replace ERCP as first line treatment. Am J Surg. 2023. doi:10.1016/j.amjsurg.2023.03.006
29. Hu H, Zhao G, Zhang K, et al. The clinical application of a self-developed gasless laparoendoscopic operation field formation device on patients undergoing cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2020;30(5):441–446. doi:10.1097/SLE.0000000000000809
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


