Back to Journals » Infection and Drug Resistance » Volume 16
A Retrospective Study on the Burden of Malaria in Northeastern Ethiopia from 2015 to 2020: Implications for Pandemic Preparedness
Authors Daba C , Atamo A , Debela SA , Kebede E , Woretaw L, Gebretsadik D , Teshome D , Tefera Y, Gebrehiwot M
Received 20 December 2022
Accepted for publication 2 February 2023
Published 11 February 2023 Volume 2023:16 Pages 821—828
DOI https://doi.org/10.2147/IDR.S399834
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Chala Daba,1 Amanuel Atamo,1 Sisay Abebe Debela,2 Edosa Kebede,3 Lebasie Woretaw,1 Daniel Gebretsadik,4 Daniel Teshome,5 Yonatal Tefera,6 Mesfin Gebrehiwot1
1Department of Environmental Health, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia; 2Department of Public Health, College of Medicine and Health Sciences, Salale University, Fitche, Ethiopia; 3Departement of Medical Laboratory Science, College of Medicine and Health Sciences, Ambo University, Ambo, Ethiopia; 4Department of Medical Laboratory Science, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia; 5Department of Anatomy, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia; 6Adelaide Exposure Science and Health, School of Public Health, University of Adelaide, Adelaide, Australia
Correspondence: Chala Daba, Email [email protected]
Background: Regardless of various prevention and control strategies, malaria continues to be a significant public health problem in Ethiopia. As there are few studies on malaria trend analysis in Northeastern Ethiopia, it hinders the evaluation of ongoing and prioritization of new malaria intervention strategies, particularly during the period of pandemics. Therefore, the present study investigated the trend of malaria prevalence in Northeastern Ethiopia from 2015 to 2020.
Methods: An institution-based retrospective study was employed to assess the trend of malaria prevalence over a 6-year period (2015– 2020) in three districts (Jile tumuga, Aruma fursi, and Dawachefa) of Northeastern Ethiopia. Data were extracted from clinical records of malaria cases by trained medical laboratory technologists. The associations between the prevalence of malaria and independent variables (age group, malaria transmission season, and districts) were assessed using chi-square test. P-values with a cut-off point of 0.05 were used to determine statistically significant associations.
Results: In our study area, a total of 212,952 malaria suspected patients were diagnosed over the 6 years. Of these, 33,005 (15.5%) were confirmed malaria cases. The identified Plasmodium species were Plasmodium falciparum and P. vivax, accounting for 66.4% and 33.6%, respectively. These with the age of > 15 years old were the most affected (41.9%). The highest numbers of malaria cases (34.6%) were recorded during spring season (September to November). The prevalence of Plasmodium species showed a significant association with age (X2=9.7; p=0.002), districts (X2=13.5; p< 0.001), and malaria transmission season (X2=16.5; p< 0.001).
Conclusion: In our study area, P. falciparum is the dominant species. We noted that malaria remains a public health concern and fluctuates throughout the years. Therefore, national, regional, zonal, and district health bureaus should strengthen the ongoing and devise appropriate prevention and control strategies even during the period of pandemics.
Keywords: malaria trend, season, P. falciparum and P. vivax, Northeast Ethiopia
A Letter to the Editor has been published for this article.
Introduction
Globally, malaria is one of the major public health concerns.1 According to a World Health Organization (WHO) report, around 241 and 227 million malaria cases were reported in 2020 and 2019, respectively. Similarly, the mortality rate showed a 12% increase from 2019 to 2020.2 Beyond mortality and morbidity, malaria causes a huge economic loss.3 For instance, a WHO report estimated US$3.5 billion spending on malaria-related concerns in 2020 alone.2 Regionally in 2018, the highest proportion of malaria burden was recorded in Africa, with 213 million (93%) cases and 380,000 deaths (94%), followed by the South-East Asia region, where 3.4% of all malaria cases were recorded.4
Plasmodium falciparum and P. vivax are the most common malaria causing protozoans principally in developing countries.5 In Ethiopia, 2.9 million confirmed malaria cases were reported in 2019 alone; of which 4,782 people died.6 Malaria transmission is seasonal, peaking from September to December following the main rainy season. A slower transmission season also occurs during April and May.7 The Ethiopian Ministry of Health reported that 75% of the country is malarious. As a result, nearly 70% of the population is at risk of contracting malaria.8–10
The burden of malaria varied through time in different regions of Ethiopia. For instance, evidence from different studies revealed that the prevalence could be as high as 32.7% in Southwest Ethiopia,11 29.8 in Jimma town,16 21.7% in Dembia district,12 8.6% in Southern Central Ethiopia,13 6.9% in North Ethiopia,15 and 5% in Bahir Dar city.14 Evidence from these different studies indicated that educational level,17 absence of Insecticide Treated Bed Net (ITN), and lack of information about malaria,18 residence, and age19 are the determinant factors for its prevalence.
Northeastern Ethiopia, particularly Oromia special zone, is one of the malarious areas in Ethiopia, where malaria infection is a significant public health problem. The prevalence of malaria in this zone was reported to be 12.5%, with Plasmodium falciparum being the dominant parasite species.41 Unfortunately, most of the previous malaria trend analysis studies were based on a single healthcare facility (either health center or hospital), which could not represent the actual malaria burden in a certain area.13–15,20,21 Besides, although a previous study analyzed the changing malaria trend in this malaria-endemic area prior to the onset of COVID-19,41 there are no comprehensive reports during the period of COVID-19. Thus, this study aimed at assessing the prevalence of malaria in three districts of Northeastern Ethiopia from 2015 to 2020.
Methods and Materials
Study Area and Population
This study was conducted in health institutions of the three districts (namely Jile tumuga, Aruma fursi, and Dawachefa) of Oromia special zone of Amhara regional state, Northeastern Ethiopia (Figure 1). In this study, among the seven districts (Artuma fursi, Bati, Dawachefa, Dewe-Harewa, Jile tumuga, Kemissie, and Bati towns) of Oromia special zone, three districts were selected using the lottery method. The area is considered as lowland with an average annual temperature greater than 37°C. Geographically, the study area is located between 10°45’N 39°45’E, and 11°15′N 40°15′E, respectively. According to the information obtained from the districts health officers, malaria is one of the most prevalent seasonal diseases in the area. Indeed, to control the burden of malaria, the districts are taking various interventions, such as distribution of Long Lasting Insecticidal nets (LLIN) and indoor residual spraying. The study participants were all clients who were registered on the laboratory logbooks of health facilities for blood film examination.
 |
Figure 1 Map showing the location of our study area. |
Study Design and Period
A facility-based retrospective cross-sectional study design was conducted by reviewing laboratory records of health institutions to extract data on malaria morbidity from January to February 2021.
Data Collection and Quality Control
Malaria data recorded between October 1, 2015 and December 30, 2020 were extracted from records kept at the health institutions. The total number of malaria suspected cases and blood films examined, etiology species types, age, and district were extracted by well-trained medical laboratory experts. In the study area, microscopy is considered as a confirmatory procedure to detect the presence and type/species of Plasmodium parasite. In Ethiopia, as a standard operating procedure to detect malaria parasite,20 thick blood films were taken as positive if one or more malaria parasites have been observed; and, negative if no parasites were seen after examining 1,000 white blood cells. Similarly, thin smears were considered positive for malaria if one or more malarial parasites were seen; and, negative if no asexual form of Plasmodium species was observed in 200 high-power fields.22
Inclusion and Exclusion Criteria
All clients who were registered on the laboratory logbooks of health facilities were included and any data, such as the demographic characteristics (age and districts) and malaria diagnosis results, which were not properly recorded, were excluded from the analysis.
Study Variables
In this study, the outcome variable was the prevalence of malaria and the independent variables were month, season, year, and demographic characteristics (age and districts).
Data Analysis
The extracted data were entered into Excel version 13 and exported to SPSS version 25 for data analysis. Descriptive statistics were applied to summarize the data, show seasonal variability, and show the trend in malaria prevalence over the years. Malaria parasite proportions were compiled by age, districts, and malaria transmission season. The association between prevalence of malaria and independent variables (age group, malaria transmission season, and districts) were assessed using chi-square test. P-values with a cut-off point of 0.05 were used to determine a statistically significant association. Malaria prevalence is considered as the ratio between the number of people infected with Plasmodium and the total number of people examined.
Ethical Consideration
Ethical approval was obtained from Wollo University, College of Medicine and Health Sciences. A support letter was also provided by each district health office administration. Written informed consent was obtained from the adult participants and guardians/parents for those below 18 years old. All the research procedures were performed in accordance with the Helsinki Declaration and WHO’s good clinical practices guidelines.
Results
Annual Trend of Malaria Prevalence
Over the 6-year period (2015–2020), a total of 212,952 malaria-suspected patients had requested blood film examination at the health institutions of the three districts (Table 1). In this study, the overall prevalence of malaria over the 6-years was 15.5%. The prevalence of malaria cases varied throughout those years. The number of confirmed malaria cases progressively increased from 2015 to 2016 and from 2019 to 2020. The highest confirmed malaria cases were reported in 2016, when 8,031 out of 43,681 suspected patients were confirmed to have malaria. Conversely, the lowest prevalence of malaria cases was observed in 2019. The number of confirmed malaria cases declined from 2017 to 2019 (Table 1). The prevalence showed an increasing trend from 2019 to 2020.
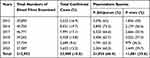 |
Table 1 Malaria Case Distribution Over Time in Three Districts of Northeastern Ethiopia from 2015 to 2020 |
Proportion of Malaria Cases in Relation to Districts
In the current study, the highest proportion of malaria cases were reported at Artuma fursi, 15,686 (47.5%). The lowest proportion of confirmed malaria cases was observed at Dawachefa (4,767, 14.5%). A significant association was detected between the proportion of Plasmodium species and districts (X2=13.5; p<0.001) (Table 2).
 |
Table 2 Proportion of Malaria Cases (n=33,005) Among Age Groups of the Study Population, Districts and Seasons in Northeastern Ethiopia from 2015 to 2020 |
Plasmodium Parasite Distribution with Age Groups
Among the diagnosed Plasmodium species, falciparum was the dominant parasite species, accounting for 66.4% (Table 1). Even though malaria cases were observed in all age groups, the highest affected age group was those greater than 15 years old followed by 5–15 years old. Age was also significantly associated with the prevalence of malaria (X2=9.7; p=0.002) (Table 2).
Seasonal and Monthly Variation of Malaria Cases
The highest malaria transmission was reported during spring (September–November) (34.6%). Regarding Plasmodium species, the highest cases of P. falciparum were recorded during summer followed by spring season. On the other hand, the highest confirmed cases of P. vivax were observed during spring (Table 2). Concerning monthly variability, the maximum confirmed malaria cases were observed during July, August, and September. However, the minimum confirmed malaria cases were detected during March and February (Figure 2).
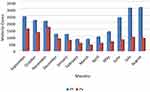 |
Figure 2 Trend analysis of malaria cases by months from 2015 to 2020 (Plasmodium falciparum: 21,924; Plasmodium vivax: 11,081). |
Discussion
There are numerous ongoing malaria prevention and control interventions being implemented in Ethiopia over years in which their effectiveness is not well-addressed. In our study area, the overall prevalence of malaria burden over 6-years was 15.5% which was lower than the study reports in Kola Diba, Northwest Ethiopia (75%),25 Benishangul-Gumuz regional state, Western Ethiopia (51.8%),23 Woreta town (48%),28 Omo zone of Southern Ethiopia (41.5%),27 Northwest Ethiopia (36.1%),24 Abeshge, South-central Ethiopia (33.8%),26 Northwest part of Ethiopia (21.8%),12 and Wollega zone (20.07%).29 The lower prevalence of malaria in the present study might probably be linked with the study period, differences in weather conditions, and community awareness about malaria transmission and control mechanisms. In fact the burden of malaria is strongly associated with weather conditions, being more prevalent in warmer areas.43 Indeed, our finding was relatively similar with the studies conducted in Kombolcha (7.5%)21, Metema (17%)30, and Arsi Negelle (11.4%).31
Plasmodium falciparum was the more frequently reported species (66.4%) followed by P. vivax (33.6%) during the last 6-years. This finding was consistent with studies conducted in different parts of Ethiopia: Arsi Negelle,31 Kombolcha town,21 Ataye,20 Bahir Dar city,14 and Kola Diba.25 The finding was also in line with an Ethiopian Federal Ministry of Health report.32 However, reports from Jimma,16 Wolkite town,13 and Butajira area33 indicated the dominance of P. vivax, which indicates the shift of the malaria parasite probably due to drug resistance, climatic conditions, and the relapsing ability of the species.42,43 Besides, the existing malaria intervention activities are focusing on P. falciparum; therefore, ignorance of P. vivax might contribute to the trend shift. Unlike P. falciparum, P. vivax can also be reactivated in the absence of a mosquito bite. In addition to the conventional intervention activities, such as provision of impregnated bed net and application of insecticide residual spray, that are helpful for the control of Plasmodium species and its vector, it might be highly advantageous to use radically curative treatments in supervised modality in malaria endemic areas.44,45
The burden and prevalence of malaria cases varied through the years. Evidence from this study showed that the prevalence of malaria increased from 2015 to 2016 and it was higher in 2020 as compared with 2019. This finding was consistent with the retrospective studies from Ataye town20 and Northwest Ethiopia,12 which reported an increasing trend of malaria during 2015 and 2016.20 On the other hand, the finding of the present study contradicted studies reported from Boricha district34 and Southwest Ethiopia.35 The increased prevalence of malaria during 2020 was possibly linked with the emergence of the COVID-19 pandemic in which many resources were shifted for the control and prevention of this disease rather than other infectious diseases, such as malaria.20 However, the prevalence of malaria decreased from 2017 to 2019. This might be associated with the implementation of various malaria prevention and control interventions, including an insecticide treated bed net (ITN), indoor residual spraying (IRS), and environmental management to achieving a sustainable development goal by reducing the infection by 2030. Moreover, the realization of a health extension package program is believed to partly contribute to the decline of malaria cases in the study area during 2019.41
Regarding the distribution of malaria cases by districts, the highest proportion was reported in Artuma fursi (47.5%) followed by Jile tumuga (38%). This difference in the distribution of malaria burden in the districts might be due to variations in temperature and climatic condition. This finding is supported by a study in Amhara regional state.41 Similarly, the study participants greater than or equal to 15 years were highly affected (41.9%). This finding was consistent with retrospective studies performed in Kola Diba,25 Kombolcha,21 Ataye, North Shoa,20 Gondar,12 Addi Arkay health center,24 Abeshge town,26 and Raya Azebo.36 The high proportion among the productive age group could be associated with their engagement in field farm activities, which could increase their exposure to Anopheles mosquito bites.
Season also has an association with the prevalence of malaria, which is in line with the notion that the transmission of malaria is largely associated with “environmental, climatic, seasonal and behavioral factors”.40 In our study area, the highest malaria transmission was recorded during spring (34.6%) followed by summer (34.2%), which is congruent with study findings from Northwest Ethiopia,12 Southwest Ethiopia,35 and Northern Ethiopia.36 In most parts of Ethiopia, the peak season for the transmission of malaria is from September to December, following the major rainy season.37 Seasonal rainfall and temperature variability is known to affect the breeding habitats and larval development of mosquito vectors, and the growth rate of the malaria parasites within their vector.38,39
Limitations of the Study
The current research work had some limitations. The findings could have been stronger if the study had included qualitative information about malaria intervention and control activities that are implemented during the 6 years in the three districts. This study also did not include case fatality rate and the prominent clinical condition of malaria infection. Incomplete laboratory registration book was also another limitation.
Conclusions
Malaria continues to be a significant community health concern in our study area. The highest confirmed malaria cases were reported in 2016. Plasmodium falciparum was the dominant parasite species. The prevalence of malaria was high particularly during spring and summer seasons. The most affected group of the population were the productive age groups (>15 years old). Collaborative efforts between different governmental (eg, national, regional, zonal, and district health bureaus) and non-governmental stakeholders are recommended to reduce the burden of malaria. Therefore, strengthening the ongoing and devising appropriate prevention and control strategies are necessary particularly during the period of pandemics.
Data Sharing Statement
Datasets analyzed during the current study are available from the corresponding author upon reasonable request.
Acknowledgments
The authors acknowledge Wollo University for all the genuine support. Our gratitude also goes to the manager of the health institutions and data collectors for their cooperation.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sakeni M, Khorram A, Majdzadeh R, Raiesi A. Indoor residual spraying coverage and acceptability rates to control malaria and the householders’ reasons of acceptance or rejection of spraying, in South-East of Iran. Int J Infect. 2015;2(4):1–9. doi:10.17795/iji-31548
2. World Health Organization. World Malaria Report 2021. Geneva: World Health Organization; 2021. Licence: CC BY-NC-SA 3.0 IGO.
3. USAID. Ethiopia malaria operational plan; 2020: 1–107. Available from: www.pmi.gov.
4. World Health Organization. World Malaria Report 2019. Geneva: World Health Organization; 2019. Licence: CC BY-NC-SA 3.0 IGO.
5. World Health Organization. Achieving the Malaria MDG Target: Reversing the Incidence of Malaria 2000–2015. World Health Organization; 2015.
6. Girum T, Shumbej T, Shewangizaw M. Burden of malaria in Ethiopia, 2000–2016: findings from the Global Health Estimates 2016. Trop Dis Travel Med Vaccines. 2019;5(1):1–7. doi:10.1186/s40794-019-0090-z
7. Abeku TA, Oortmarssen GJ, Borsboom G, de Vlas SJ, Habbema JDF. Spatial and temporal variations of malaria epidemic risk in Ethiopia: factors involved and implications. Acta Trop. 2003;7:331–340. doi:10.1016/S0001-706X(03)00123-2
8. Howes RE, Battle KE, Golding N, Hay SI. Plasmodium Vivax Thematic Review: Epidemiology: A Thematic Review Prepared for the Writing Committee for the Development of the WHO of Global Strategic Plan on Plasmodium Vivax Control and Elimination. Geneva: World Health Organization; 2014:103.
9. Federal Ministry of Health. Guideline for Malaria Epidemic Prevention and Control in Ethiopia.
10. Adugna A. Malaria in Ethiopia; 2007. Available from: www.ethiodemographyandhealth.org.
11. Geshere G, Dabassa A, Petros B. Trend of malaria prevalence in Ilu Galan, Bako Tibe, and Danno Districts of West Shoa Zone, Oromiya Region, Ethiopia. J Biol Chem Res. 2014;31(2):678–693.
12. Addisu A, Tegegne Y, Mihiret Y, Setegn A, Zeleke AJ. A 7-year trend of malaria at primary health facilities in Northwest Ethiopia. J Parasitol Res. 2020;2020:1–5. doi:10.1155/2020/4204987
13. Solomon A, Kahase D, Alemayehu M. Trend of malaria prevalence in Wolkite health center: an implication towards the elimination of malaria in Ethiopia by 2030. Malar J. 2020;19:112. doi:10.1186/s12936-020-03182-z
14. Yimer M, Hailu T, Mulu W, Abera B, Ayalew W. A 5-year trend analysis of malaria prevalence with in the catchment areas of Felegehiwot Referral Hospital, Bahir Dar city, northwest-Ethiopia: a retrospective study. BMC Res Notes. 2017;10(1):4–7. doi:10.1186/s13104-017-2560-6
15. Berhe B, Mardu F, Legese H, Negash H. Seasonal distribution and seven year trend of malaria in North West Tigrai: 2012–2018, Ethiopia. Trop Dis Travel Med Vaccines. 2019;5:15. doi:10.1186/s40794-019-0091-y
16. Alemu A, Abebe G, Tsegaye W, Golassa L. Climatic variables and malaria transmission dynamics in Jimma town, South West Ethiopia. Parasit Vectors. 2011;4:30. doi:10.1186/1756-3305-4-30
17. Ediau M, Babirye JN, Tumwesigye NM, et al. Community knowledge and perceptions about indoor residual spraying for malaria prevention in Soroti district, Uganda: a cross-sectional study. Malar J. 2013;12(1):1–9. doi:10.1186/1475-2875-12-170
18. Gontie GB, Wolde HF, Baraki AG. Prevalence and associated factors of malaria among pregnant women in Sherkole district, Benishangul Gumuz regional state, West Ethiopia. BMC Infect Dis. 2020;20:573. doi:10.1186/s12879-020-05289-9
19. Tadesse F, Andrew W, Deressa W. Prevalence and associated risk factors of malaria among adults in East Shewa Zone of Oromia Regional State, Ethiopia: a cross-sectional study. BMC Public Health. 2018;18:25. doi:10.1186/s12889-017-4577-0
20. Feleke DG, Gebretsadik D, Gebreweld A. Analysis of the trend of malaria prevalence in Ataye, North Shoa, Ethiopia between 2013 and 2017. Malar J. 2018;17(1):1–6. doi:10.1186/s12936-018-2474-3
21. Gebretsadik D, Feleke DG, Fiseha M. Eight-year trend analysis of malaria prevalence in Kombolcha, South Wollo, north-central Ethiopia: a retrospective study. Parasit Vectors. 2018;11(1):1–6. doi:10.1186/s13071-018-2654-6
22. Moges B, Amare B, Belyhun Y, et al. Comparison of CareStart HRP2/pLDH COMBO rapid malaria test with light microscopy in north-west Ethiopia. Malar J. 2012;11:1–6. doi:10.1186/1475-2875-11-234
23. Alkadir S, Gelana T, Gebresilassie A. A five year trend analysis of malaria prevalence in Guba district, Benishangul- Gumuz regional state, western Ethiopia: a retrospective study. Trop Dis Travel Med Vaccines. 2020;6:18. doi:10.1186/s40794-020-00112-4
24. Tesfa H, Bayih AG, Zeleke AJ. A 17-year trend analysis of malaria at Adi Arkay, north Gondar zone, Northwest Ethiopia. Malar J. 2018;17(1):1–6. doi:10.1186/s12936-018-2310-9
25. Alemu A, Muluye D, Mihret M, Adugna M, Gebeyaw M. Ten year trend analysis of malaria prevalence in Kola Diba, North Gondar, Northwest Ethiopia. Parasit Vectors. 2012;5:173. doi:10.1186/1756-3305-5-173
26. Yimer F, Animut A, Erko B, Mamo H. Past five-year trend, current prevalence and household knowledge, attitude and practice of malaria in Abeshge, south-central Ethiopia. Malar J. 2015;14(1):1–11. doi:10.1186/s12936-015-0749-5
27. Ergete M, Sorsa S, Loha E, Asnak S. Trend of malaria cases in Hana and Keyafer health centers, south Omo zone, southern Ethiopia. Ethiop J Health Sci. 2018;28(3). doi:10.4314/ejhs.v28i3.5
28. Alelign A, Tekeste Z, Petros B. Prevalence of malaria in Woreta town, Amhara region, Northwest Ethiopia over eight years. BMC Public Health. 2018;18(1):1–6. doi:10.1186/s12889-018-5913-8
29. Gemechu T, Samuel A, Yewhalaw D. Ten years trend analysis of malaria prevalence and its correlation with climatic variables in Sibu Sire District, east Wollega zone, Oromia regional state, Western Ethiopia: a retrospective study. Sci Technol Arts Res J. 2015;4(4):99–105. doi:10.4314/star.v4i4.14
30. Ferede G, Worku A, Getaneh A, et al. Prevalence of malaria from blood smears examination: a seven-year retrospective study from Metema Hospital, Northwest Ethiopia. Malar Res Treat. 2013;2013:0–2.
31. Hailemariam M, Gebre S. Trend analysis of malaria prevalence in Arsi Negelle health center southern Ethiopia. J Infect Dis Immun. 2015;7(1):1–6. doi:10.5897/JIDI2014.0147
32. Ethiopian Public Health Institute (EPHI). Ethiopia National Malaria Indicator Survey 2015. Addis Ababa: Ethiopian Public Health Institute; 2016.
33. Woyessa A, Deressa W, Ali A, Lindtjørn B. Prevalence of malaria infection in Butajira area, south-central Ethiopia. Malar J. 2012;11:84. doi:10.1186/1475-2875-11-84
34. Dabaro D, Birhanu Z, Delenasaw D. Analysis of trends of malaria from 2010 to 2017 in Boricha District. South Ethiop Malar J. 2020;19:88. doi:10.1186/s12936-020-03169-w
35. Hawaria D, Getachew H, Zhong G, et al. Ten years malaria trend at Arjo-Didessa sugar development site and its vicinity. Southwest Ethiopia: a retrospective study. Malar J. 2019;18:145.
36. Tesfay K, Yohannes M, Bayisa S. Trend analysis of malaria prevalence in Raya Azebo district, Northern Ethiopia: a retrospective study. BMC Res Notes. 2018;11(1):1–5. doi:10.1186/s13104-018-4003-4
37. Federal Democratic Republic of Ethiopia Ministry of Health. National Strategic Plan for Malaria Prevention, Control and Elimination in Ethiopia 2011–2015. Addis Ababa, Ethiopia: Federal Democratic Republic of Ethiopia Ministry of Health; 2010.
38. Kibret S, Wilson GG, Ryder D, Tekie H. Environmental and meteorological factors linked to malaria transmission around large dams at three ecological settings. Ethiop Malar J. 2019;18:54. doi:10.1186/s12936-019-2689-y
39. Ngarakana-Gwasira ET, Bhunu CP, Masocha M, Mashonjowa E. Assessing the role of climate change in malaria transmission in Africa. Malar Res Treat. 2016;2016:7104291. doi:10.1155/2016/7104291
40. Ayele DG, Zewotir TT, Mwambi HG. Prevalence and risk factors of malaria in Ethiopia. Malar J. 2012;11(1):1–9. doi:10.1186/1475-2875-11-195
41. Tefera S, Bekele T, Getahun K, Negash A, Ketema T. The changing malaria trend and control efforts in Oromia Special zone, Amhara Regional State, North-East Ethiopia. Malar J. 2022;21(1):1. doi:10.1186/s12936-022-04149-y
42. Dasgupta S. Burden of climate change on malaria mortality. Int J Hyg Environ Health. 2018;221(5):782–791. doi:10.1016/j.ijheh.2018.04.003
43. Battle KE, Karhunen MS, Bhatt S, et al. Geographical variation in Plasmodium vivax relapse. Malar J. 2014;13(1):1–6. doi:10.1186/1475-2875-13-144
44. Thriemer K, Degaga TS, Christian M, et al. Reducing the risk of Plasmodium vivax after falciparum infections in co-endemic areas—a randomized controlled trial (PRIMA). Trials. 2022;23(1):1–2. doi:10.1186/s13063-022-06364-z
45. Poespoprodjo JR, Burdam FH, Candrawati F, et al. Supervised versus unsupervised primaquine radical cure for the treatment of falciparum and vivax malaria in Papua, Indonesia: a cluster-randomised, controlled, open-label superiority trial. Lancet Infect Dis. 2022;22(3):367–376. doi:10.1016/S1473-3099(21)00358-3
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
