Back to Journals » Clinical Ophthalmology » Volume 17
A Randomized, Prospective, Observer-Masked Study Comparing Dropless Treatment Regimen Using Intracanalicular Dexamethasone Insert, Intracameral Ketorolac, and Intracameral Moxifloxacin versus Conventional Topical Therapy to Control Postoperative Pain and Inflammation in Cataract Surgery
Authors Donnenfeld ED , Hovanesian JA , Malik AG, Wong A
Received 22 May 2023
Accepted for publication 8 August 2023
Published 15 August 2023 Volume 2023:17 Pages 2349—2356
DOI https://doi.org/10.2147/OPTH.S422502
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Eric D Donnenfeld,1 John A Hovanesian,2 Aysha G Malik,1 Aidan Wong1
1Ophthalmic Consultants of Long Island, New York, NY, USA; 2Harvard Eye Associates, Laguna Hills, CA, USA
Correspondence: Eric D Donnenfeld, Ophthalmic Consultants of Long Island (OCLI), 711 Stewart Avenue, Suite 160, Garden City, New York, NY, 11530, USA, Tel +1 516-500-4200, Fax +1 516-742-0017, Email [email protected]
Purpose: To evaluate clinical efficacy and patient preference for a dropless treatment regimen compared to conventional topical therapy in patients undergoing cataract surgery.
Patients and Methods: In this prospective, contralateral eye study, patients with bilateral cataract were randomized to receive either intracanalicular dexamethasone insert, intracameral phenylephrine 1%/ketorolac 0.3%, and intracameral moxifloxacin (50 μg) (study group) or topical moxifloxacin 0.5%, ketorolac 0.5%, and prednisolone acetate 1.0% QID (control group). The second eye underwent cataract surgery 2 weeks later and was treated with the opposite treatment. All patients were evaluated at Days 1, 7, 14, 28, and 3 months. The primary outcome measure was postoperative ocular pain. Secondary outcomes included summed ocular inflammation score (SOIS; the sum of the mean anterior chamber cells and anterior flare score), the patient preference for medication protocol between the two eyes, and patient out-of-pocket cost of medications. Safety outcome measures included CDVA, intraocular pressure, central retinal thickness (CRT), and the incidence of reported AEs.
Results: The proportion of patients with no pain was similar in both groups at all postoperative visits (p> 0.05). No statistically significant difference in SOIS score was observed between the two groups at any visit. A strong majority of the patients (94.7%) preferred the study eye’s dropless regimen over the control eye’s conventional topical therapy regimen. No statistically significant difference in mean intraocular pressure (IOP) was observed at any postoperative visit, except at Week 1. The mean CDVA was also similar in both groups at all postoperative visits (p> 0.05). The postoperative mean CRT was comparable between the two groups.
Conclusion: A dropless treatment regimen is as effective as topical eyedrop administration. A higher proportion of patients who underwent bilateral cataract surgery preferred the dropless treatment regimen over the patient-administered eye drop regimen.
Keywords: dropless cataract surgery, intracanalicular dexamethasone insert, dropless vs topical eyedrop administration, sustained-release steroid delivery, drop-free treatment regimen
Introduction
Eyedrops are a well-established, convenient, and noninvasive method for delivering anti-infective and anti-inflammatory drugs to the anterior segment of the eye following cataract surgery. However, topical drug delivery is associated with several limitations that can adversely affect visual outcomes and patient satisfaction.1
Poor drug bioavailability is a major concern associated with eye drops. It has been estimated that less than 5% of the drug reaches intraocular tissues,2,3 mainly due to the precorneal loss following topical administration, the corneal-epithelial barrier, and drug loss through the conjunctival-scleral route.4,5 Topical eyedrop administration, by nature of its intermittent application, also results in variable drug concentration over time, with peak concentrations (immediately after instillation) potentially increasing the risk for side effects, and trough concentrations (before the next instillation) potentially producing an insufficient pharmacologic effect.6 In addition, topical medications are preserved, which can have a deleterious effect on the ocular surface, degrading quality of vision and patient satisfaction with cataract surgery.
Diligent patient compliance with postoperative medications is paramount to ensure optimal outcomes following cataract surgery. However, the noncompliance rate for ocular medications has been shown to be approximately 30%.5,7 A compliance monitoring study in cataract and glaucoma patients reported a low adherence rate, with almost 50% of the doses omitted.8 An et al documented that as high as 92% of post-cataract patients exhibited inappropriate drop administration, such as missing the eye, instilling too many drops, contaminating the bottle tip by touching the ocular surface, and failing to wash their hands before administration.9 In the elderly, poor dexterity, tremors, and poor near vision all add to the difficulty of instilling drops.10 Additionally, tapering regimens may be complex for some patients to understand, especially in the context of dementia or cognitive difficulties.10 The high cost of the medications is potentially another reason for patient noncompliance.5
Topical eyedrop administration imposes an additional burden on the patients, their caregivers, and healthcare professionals. Unlike glaucoma patients, most cataract patients do not use eyedrops regularly and require preoperative training by ophthalmic staff to ensure proper and safe eye drop instillation.9 Moreover, physicians’ offices may receive a high volume of calls from patients or pharmacies regarding substitutions for or questions about the post-cataract eye drops that have been prescribed. It has been estimated that all these responsibilities account for up to 3000 staff hours annually.10
Because of the aforementioned limitations, dropless cataract surgery is an attractive concept. Previous studies have shown that sustained-release steroid delivery can be as effective as topical administration in controlling inflammation, without the compliance challenges.6,11–14 Intracameral delivery of antibiotics has become commonplace and is now the preferred strategy in some regions or surgery centers.15,16 The purpose of this study was to evaluate clinical efficacy and patient preference for a drop-free treatment regimen consisting of intracanalicular insert dexamethasone plus intracameral phenylephrine, ketorolac, and moxifloxacin vs conventional topical therapy.
Materials and Methods
This randomized, contralateral eye, prospective clinical study included subjects with bilateral cataract scheduled to undergo sequential surgery in both eyes. On initial consultation, the subjects were randomized by a random number generator to receive either the study regimen or conventional topical therapy in the first eye. The second eye underwent cataract surgery 2 weeks later and received the opposite treatment. Institutional Review Board approval was obtained from Advarra IRB, and the trial was registered on Clinicaltrials.gov (NCT04205916). Before beginning any study-related procedures, written informed consent was obtained from all patients. The study was conducted in accordance with the ethical principles of the Declaration of Helsinki and its amendments.
In the eyes randomized to the study group, a dexamethasone intracanalicular insert (Dextenza, Ocular Therapeutix, Bedford, MA) was inserted into the lower punctum at the time of surgery, intracameral phenylephrine 1%/ketorolac 0.3% (Omidria, Rayner, Memphis, TN) was used during surgery, and intracameral moxifloxacin (50 micrograms) (ImprimisRx, San Diego, CA) was administered at the conclusion of the surgery. Eyes randomized to the control group received topical moxifloxacin 0.5% QID (4 times a day) 1 day prior to surgery and for 10 days postoperatively, ketorolac 0.5% QID 1 day prior to surgery and for 1 month postoperatively, and prednisolone acetate 1.0% QID for the first postoperative 2 weeks and BID (2 times a day) for the following 2 weeks.
All subjects included in the study were ≥22 years of age at the time of the screening visit with anatomically normal, healthy eyes free of pathology other than cataract, had preoperative corneal astigmatism of 3.0 D or less in both eyes, and had the potential for a post-operative Snellen corrected distance visual acuity (CDVA) of 20/30 or better in both eyes.
Subjects with a history of trauma or disease in the nasolacrimal area; puncta >0.9 mm before dilation; any ocular pain or discomfort in either eye at the screening visit or on the day of intracanalicular insertion, or any signs of intraocular inflammation (cells/flare) in either eye at the screening visit were excluded. Patients who had prior intraocular surgery within the last 6 months or were expected to undergo surgical intervention (including limbal relaxing incision (LRI) and arcuate incision (AI)) and/or ocular laser treatment before or during the study period, or had any systemic or local disease or were using systemic or ocular medications that may affect the study results were also excluded. Patients with known allergy or sensitivity to any of the study medications and those known to be steroid responders were also excluded.
Intraoperative exclusion criteria included surgical complications, such as posterior capsular rupture or zonular dialysis, disruption of anterior hyaloid face, vitreous loss, capsulorhexis tear, floppy iris syndrome, the use of trypan blue, capsular tension ring or other intraocular device other than the IOL, inability to place IOL in the capsular bag, significant anterior chamber hyphema, or zonular rupture.
Patients were followed postoperatively at Days 1, 7, 14, 28, and 3 months and the following assessments were performed by a masked observer: Ocular pain, distance visual acuity, optical coherence tomography (OCT) of the macula, anterior chamber cell and flare, cataract density grade, dilated fundus examination, and intraocular pressure (IOP). Any adverse events (AEs) were also recorded. Starting on Day 1 for the first eye and then again at each visit, patients were asked to evaluate their pain level on a scale of 0–10, where 0 is no pain and 10 is the greatest pain.
The Comparison of Ophthalmic Medications for Tolerability (COMTOL) questionnaire, which has been validated for consistency, reliability, and reproducibility, was used to assess the medication preference, frequency and severity of medication side effects, and to determine how the side effects impaired daily routines or affected the quality of life.17
The primary outcome measure was postoperative ocular pain. Secondary outcomes included summed ocular inflammation score (SOIS; the sum of the mean anterior chamber cells and anterior flare score), the patient preference of medication protocol as measured by COMTOL, and patient out-of-pocket cost of medications. Safety outcome measures included CDVA, intraocular pressure, central retinal thickness (CRT), and the incidence of reported AEs.
Statistical Analysis
No formal sample size calculation was performed. Data analysis was performed using Microsoft Excel and SPSS software (version 27.0) for Windows (IBM SPSS Statistics 27, IBM Inc., Armonk, NY). The normality of scale data was checked using the Kolmogorov–Smirnov test and quantile-quantile plots. For normally distributed scale data, paired-sample t test was used to compare the means between the two groups. For data that were not normally distributed scale data/ordinal data, the non-parametric counterpart Wilcoxon signed-rank test was used. McNemar’s test was used for paired nominal data. The level of significance for all statistical analyses was set at 0.05.
Results
A total of 41 patients with a mean age of 69.9 ± 7.1 years (range: 57 to 86 years) were enrolled in the study. The study population was 58.5% female and 41.5% male. At baseline, there were no statistically significant differences between the study and control eyes in Lens Opacity Classification System (LOCS) grade of cataract, CRT, or IOP.
Primary Outcome Measure
The proportion of patients with no pain was similar in both groups at all postoperative visits (p>0.05, McNemar’s test), with 100% of eyes in both groups having no pain at the Month 1 and Month 2 postoperative visits (Table 1). The mean pain level was 0.81 ± 1.27 (range: 0 to 5) in the study group and 1.03 ± 1.60 (range: 0 to 6) in the control group.
 |
Table 1 Proportion of Patients with No Pain |
Secondary Outcome Measures
Table 2 shows the mean SOIS score in the experimental and control groups. No statistically significant difference in SOIS score was observed between the two groups at any visit.
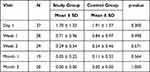 |
Table 2 Mean Postoperative SOIS Score |
A strong majority of the patients (94.7%) preferred the study eye’s dropless regimen over the control eye’s conventional topical therapy regimen (p<0.001).
Patients reported that their quality of life was not affected or only minimally affected by either treatment regimen. The proportion of patients in the study group who experienced side effects a few times, rarely, or not at all was similar to that in the control group (Table 3).
 |
Table 3 The Proportion of Patients Experiencing Each Side Effect a Few Times, Rarely, or Not at All |
Likewise, when the bothersomeness of the side effects was analyzed, the two groups were also found to be comparable (Table 4). Patients reported that their daily activities (driving during the day or at night, carrying groceries, climbing stairs, walking several blocks, or reading newspapers) were essentially unaffected by either of the two treatment regimens, with no statistically significant differences between the two groups.
 |
Table 4 The Proportion of Patients Who are Not at All or Only Minimally Bothered by Each Side Effect |
Safety Outcome Measures
At baseline, the mean IOP in the study and control eyes was 15.2 ± 3.0 mmHg and 15.1 ± 3.0 mmHg, respectively. IOP was reduced to 12.9± 3.3 mmHg in the study group and 13.3 ± 3.1 mmHg in the control group at the Month 2 visit. No statistically significant difference in IOP was observed between the two groups at any postoperative visit (p>0.05), except at Week 1 (p=0.023), with a relatively lower mean IOP in the study group than the control group (Table 5). The mean CDVA was also similar in both groups at all postoperative visits (p>0.05) (Table 6). The postoperative mean CRT was comparable between the two groups.
 |
Table 5 Mean Intraocular Pressure (mmHg) at Baseline and Each Postoperative Visit |
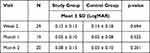 |
Table 6 Mean Corrected Distance Visual Acuity (LogMAR) at Postoperative Visits |
Cost of Medications
The mean out-of-pocket cost of medications, as reported by the patients, at the 1-month postoperative visit was $26 (range: $0 to $207) for the study eyes without drops and $184 (range: $90-$425) for the control eyes with topical therapy.
Discussion
The intracanalicular dexamethasone insert provides cataract surgeons with an additional tool in their armamentarium that may reduce or eliminate the need for patient adherence to a topical regimen while providing continuous delivery of a non-preserved corticosteroid.
Efficacy and safety of the sustained-release dexamethasone intracanalicular insert have been evaluated in three Phase 3 trials. In these trials, patients were randomized to either the dexamethasone insert, or a vehicle insert following cataract surgery. Researchers documented statistically significant less pain and lower inflammation scores for the dexamethasone intracanalicular insert compared to placebo.6,12 Later, a study evaluated the outcomes of a traditional eyedrop regimen [topical antibiotic, non-steroidal anti-inflammatory drug (NSAID) and steroids] in the control group to the dexamethasone ophthalmic insert, used along with a topical antibiotic and NSAID in the study group. This contralateral eye study in patients undergoing bilateral refractive lens exchange (RLE) found comparable inflammation control between the two groups.13 The present study compared the traditional eyedrop regimen to a completely drop-free regimen (intracameral antibiotic, intracameral NSAID, and intracanalicular dexamethasone insert) in the study group.
The present study found similar clinical outcomes for the study and control groups. The SOIS score, CDVA, IOP, and percentage of patients with no pain were similar in both treatment groups (Tables 1–6). These results suggest that corticosteroids, whether delivered topically or via intracanalicular insert in conjunction with an intracameral or topical NSAID, prevent inflammation and decrease postoperative pain, and demonstrate that a drop-free treatment regimen is as effective as the standard eyedrop regimen. We also believe the intraocular administration of the NSAID, ketorolac, achieves high tissue levels immediately following surgery, which works synergistically with the dexamethasone intracanalicular insert to suppress postoperative inflammation.
Most patients (95%) in the study preferred the dropless treatment regimen over the eyedrop regimen they used in the fellow eye, despite there being no difference in pain or other clinical parameters. Of note, more than 250 drops were instilled in the control group eyes over a one-month perioperative period, compared to none in the study group. When compared to other sustained-release platforms, the intracanalicular insert may lead to improved patient comfort due to the added benefit of punctal occlusion and improved ocular surface lubrication. The dropless treatment regimen circumvents concerns associated with poor medication compliance and alleviates the treatment burden of a complex postoperative regimen of topical eyedrops in cataract surgery patients.6 Moreover, with a dropless treatment regimen, patients may avoid a trip to the pharmacy and reduce their out-of-pocket costs for surgery-related medications. Patients reported a mean savings of $158 for the eyes that did not undergo the topical drop regimen, although this was not independently verified by investigators.
Both the topical and intracanalicular mode of drug delivery are similar in terms of reversibility of the treatment modality. In the event of an adverse reaction, topical drop administration might be stopped while the insert can be removed from the canaliculus via saline irrigation or manual expression.6 However, the intracanalicular mode of delivery has a number of advantages over topical drops. The dexamethasone insert provides a more consistent distribution of the drug each day, without dramatic peaks and troughs related to instillation. Moreover, the constant dispersion of a low-dose corticosteroid on the ocular surface requires less of the active ingredient to produce the same effect, which may be more beneficial for healing than pulsed doses of topical drops.6,13 The drug released from the insert is preservative-free, which may help eliminate the risk of preservative-induced toxicity and ocular surface damage.6 And, because the dexamethasone insert occludes the canaliculus, it may help to reduce the rate of tear film clearance from the ocular surface. It is well known that cataract surgery triggers dry eye symptoms, and instability of the tear film is the main reason for dry eyes following cataract surgery.18
The percentage of patients experiencing no pain in the study group was consistent with those reported in previous studies. The pain outcomes in the control group were also good, which may be attributed in part to the good drop compliance observed in the control group of the present study. More than 80% of the patients in the control group either did not miss or rarely missed a dose of eyedrops, and 19% missed a dose only a few times. In typical practice outside of a prospective study, patients’ compliance with the eyedrop regimen may be lower and outcomes may not be as favorable.
The small sample size is a limitation of this study. Future studies with a larger sample size may be required to confirm the findings.
Conclusion
This contralateral eye study demonstrates that a dropless treatment regimen employing two food and drug administration (FDA) approved medication delivery systems; steroid delivery via an intracanalicular insert and intracameral delivery of the NSAID and an off-label intraocular antibiotic is as effective as topical eyedrop administration in controlling pain and inflammation after cataract surgery but is strongly preferred by patients.
Abbreviations
SOIS, Summed ocular inflammation score; QID, 4 times a day; BID, 2 times a day; CDVA, Corrected distance visual acuity; OCT, Optical coherence tomography; AE, Adverse events; COMTOL, Comparison of ophthalmic medications for tolerability; CRT, Central retinal thickness; LOCS, Lens opacity classification system; IOP, Intraocular pressure; NSAID, Non-steroidal anti-inflammatory drugs; RLE, refractive lens exchange; FDA, Food and Drug Administration.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author, (EDD), upon reasonable request.
Acknowledgments
Raman Bedi, MD (IrisARC - Analytics, Research & Consulting) and Jan Beiting (Wordsmith Consulting) provided statistical and editorial assistance in the preparation of the manuscript. Partial results of this paper were presented at the 2020 ASCRS Virtual Annual Meeting.
Funding
Funding to conduct this study and for editorial assistance was provided by Ocular Therapeutix. The authors retained full control of manuscript content.
Disclosure
Drs. Donnenfeld and Hovanesian are consultants to Ocular Therapeutix and Rayner. Dr Donnenfeld also reports grants from Omeros. Dr Hovanesian also reports grants, personal fees from EyePoint, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Assil KK, Greenwood MD, Gibson A, Vantipalli S, Metzinger JL, Goldstein MH. Dropless cataract surgery: modernizing perioperative medical therapy to improve outcomes and patient satisfaction. Curr Opin Ophthalmol. 2021;32(Suppl 1):S1–S12. doi:10.1097/ICU.0000000000000708
2. Gaudana R, Ananthula HK, Parenky A, Mitra AK. Ocular drug delivery. AAPS J. 2010;12(3):348–360. doi:10.1208/s12248-010-9183-3
3. Urtti A, Salminen L. Minimizing systemic absorption of topically administered ophthalmic drugs. Surv Ophthalmol. 1993;37(6):435–456. doi:10.1016/0039-6257(93)90141-S
4. Agrahari V, Mandal A, Agrahari V, et al. A comprehensive insight on ocular pharmacokinetics. Drug Deliv Transl Res. 2016;6(6):735–754. doi:10.1007/s13346-016-0339-2
5. Matossian C. Noncompliance with prescribed eyedrop regimens among patients undergoing cataract surgery—prevalence, consequences, and solutions. US Ophthalmic Rev. 2020;13(1):18–22. doi:10.17925/USOR.2020.13.1.18
6. Tyson SL, Bafna S, Gira JP, et al. Multicenter randomized phase 3 study of a sustained-release intracanalicular dexamethasone insert for treatment of ocular inflammation and pain after cataract surgery. J Cataract Refract Surg. 2019;45(2):204–212. doi:10.1016/j.jcrs.2018.09.023
7. Vandenbroeck S, De Geest S, Dobbels F, Fieuws S, Stalmans I, Zeyen T. Prevalence and correlates of self-reported nonadherence with eye drop treatment: the Belgian Compliance Study in Ophthalmology (BCSO). J Glaucoma. 2011;20(7):414–421. doi:10.1097/IJG.0b013e3181f7b10e
8. Hermann MM, Ustundag C, Diestelhorst M. Electronic compliance monitoring of topical treatment after ophthalmic surgery. Int Ophthalmol. 2010;30(4):385–390. doi:10.1007/s10792-010-9362-3
9. An JA, Kasner O, Samek DA, Levesque V. Evaluation of eyedrop administration by inexperienced patients after cataract surgery. J Cataract Refract Surg. 2014;40(11):1857–1861. doi:10.1016/j.jcrs.2014.02.037
10. Lindstrom L, Stewart Galloway R, Grzybowski M, Liegner T. Dropless cataract surgery: an overview. Curr Pharm Des. 2017;23(4):558–564. doi:10.2174/1381612822666161129150628
11. Donnenfeld ED, Solomon KD, Matossian C. Safety of IBI-10090 for inflammation associated with cataract surgery: phase 3 multicenter study. J Cataract Refract Surg. 2018;44(10):1236–1246. doi:10.1016/j.jcrs.2018.07.015
12. Walters T, Endl M, Elmer TR, Levenson J, Majmudar P, Masket S. Sustained-release dexamethasone for the treatment of ocular inflammation and pain after cataract surgery. J Cataract Refract Surg. 2015;41(10):2049–2059. doi:10.1016/j.jcrs.2015.11.005
13. Larsen J, Whitt T, Parker B, Swan R. A randomized, controlled, prospective study of the effectiveness and safety of an intracanalicular dexamethasone ophthalmic insert (0.4 Mg) for the treatment of post-operative inflammation in patients undergoing Refractive Lens Exchange (RLE). Clin Ophthalmol. 2021;15:2211–2217. doi:10.2147/OPTH.S311070
14. Hovanesian JA, Donnenfeld ED. Intracameral dexamethasone 9% vs prednisolone acetate 1% in controlling postoperative pain and inflammation in patients undergoing cataract surgery. J Cataract Refract Surg. 2022;48(8):906–911. doi:10.1097/j.jcrs.0000000000000887
15. Endophthalmitis Study Group ESoC, Refractive S. Prophylaxis of postoperative endophthalmitis following cataract surgery: results of the ESCRS multicenter study and identification of risk factors. J Cataract Refract Surg. 2007;33(6):978–988. doi:10.1016/j.jcrs.2007.02.032
16. Shorstein NH, Winthrop KL, Herrinton LJ. Decreased postoperative endophthalmitis rate after institution of intracameral antibiotics in a Northern California eye department. J Cataract Refract Surg. 2013;39(1):8–14. doi:10.1016/j.jcrs.2012.07.031
17. Barber BL, Strahlman ER, Laibovitz R, Guess HA, Reines SA. Validation of a questionnaire for comparing the tolerability of ophthalmic medications. Ophthalmology. 1997;104(2):334–342. doi:10.1016/S0161-6420(97)30314-5
18. Ishrat S, Nema N, Chandravanshi SCL. Incidence and pattern of dry eye after cataract surgery. Saudi J Ophthalmol. 2019;33(1):34–40. doi:10.1016/j.sjopt.2018.10.009
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
