Back to Journals » Journal of Pain Research » Volume 10
A prospective, double-blinded, randomized comparison of ultrasound-guided femoral nerve block with lateral femoral cutaneous nerve block versus standard anesthetic management for pain control during and after traumatic femur fracture repair in the pediatric population
Authors Elsey NM, Tobias JD , Klingele KE , Beltran RJ , Bhalla T, Martin D, Veneziano G , Rice J, Tumin D
Received 7 April 2017
Accepted for publication 14 June 2017
Published 4 September 2017 Volume 2017:10 Pages 2177—2182
DOI https://doi.org/10.2147/JPR.S139106
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor E Alfonso Romero-Sandoval
Nicole M Elsey,1 Joseph D Tobias,1–3 Kevin E Klingele,4 Ralph J Beltran,1,2 Tarun Bhalla,1,2 David Martin,1,2 Giorgio Veneziano,1,2 Julie Rice,1,2 Dmitry Tumin1,2
1Department of Anesthesiology and Pain Medicine, Nationwide Children’s Hospital, 2The Ohio State University, 3Department of Pediatrics, Nationwide Children’s Hospital and The Ohio State University College of Medicine, 4Department of Orthopedic Surgery and Sports Medicine, Nationwide Children’s Hospital and The Ohio State University, Columbus, OH, USA
Background: Traumatic injury of the femur resulting in femoral fracture may result in significant postoperative pain. As with other causes of acute pain, regional anesthesia may offer a benefit over conventional therapy with intravenous opioids. This study prospectively assesses the effects of femoral nerve blockade with a lateral femoral cutaneous nerve block (FN-LFCN) on intraoperative anesthetic requirements, postoperative pain scores, and opioid requirements.
Materials and methods: Seventeen pediatric patients (age 2–18 years) undergoing surgical repair of a traumatic femur fracture fulfilled the study criteria and were randomly assigned to general anesthesia with either an FN-LFCN block (n = 10) or intravenous opioids (n = 7). All patients received a general anesthetic with isoflurane for maintenance anesthesia during the surgical repair of the femur fracture. Patients randomized to the FN-LFCN block group received ultrasound-guided nerve blockade using ropivacaine (0.2%/0.5% based on patient weight). At the conclusion of surgery, the airway device was removed once tracheal extubation criteria were achieved, and patients were transported to the post-anesthesia care unit (PACU) for recovery and assessment of pain by a blinded study nurse.
Results: The final study cohort included 17 patients (n = 10 for FN-LFCN block group; n = 7 for the intravenous opioid group). Although the median of the maximum postoperative pain scores in the regional group was 0, this did not reach statistical significance when compared to the median pain score of 3 in the intravenous opioid group. Likewise, no difference between the two groups was noted when comparing intraoperative anesthetic requirements, opioid requirements (intraoperative, in the post-anesthesia recovery room, and in the inpatient ward), and the time to first opioid requirement postoperatively in the inpatient ward.
Conclusion: This prospective, randomized, double-blinded study failed to demonstrate a clear benefit of regional anesthesia over intravenous opioids intraoperatively and postoperatively during repair of femoral shaft fractures in the pediatric population.
Keywords: pediatric, femur fracture repair, femoral nerve block
Introduction
One of the most common pediatric orthopedic traumatic injuries presenting for operating repair is a femoral shaft fracture. The surgical management of a femoral shaft fracture usually involves placement of an intra-medullary femoral nail or a submuscular bridge plate, both of which require an incision in the lateral distal third of the thigh.1 The use of a femoral nerve block (FNB), in both adults and children with femoral shaft fractures, has been well documented as a method to reduce the use of intravenous opioids and allow for painless transport, examination, and cast/splint application.2–6 Several European institutions advocate the performance of an FNB in the emergency department in children with an isolated femoral shaft fracture to improve analgesia and fracture immobilization.3–7 An FNB provides sensory anesthesia to the anterior and medial aspects of the thigh, and variable coverage of the femur and knee. However, there is little to no coverage of the lateral aspect of the thigh.8 Given the surgical approach to repairing a fracture of the femur and the sensory innervation of the femoral nerve, additional regional anesthesia techniques must be utilized in order to provide sensory coverage of the lateral thigh. Using ultrasound guidance, Miller has reported the successful blockade of the lateral femoral cutaneous nerve (LFCN), which provides sensory innervation to the lateral thigh, in a pediatric patient undergoing surgical repair of a fracture of the femur.9
To date, there have been no studies conducted in the pediatric population to evaluate the benefit and efficacy of combined ultrasound-guided femoral nerve and LFCN (FN-LFCN) blocks for pain management in pediatric patients undergoing surgical repair of femoral fractures. The current study prospectively compared postoperative opioid consumption pain relief in pediatric patients undergoing repair of traumatic fracture of the femur who have received either an FN-LFCN block or a standard anesthetic with intravenous opioids for analgesia without the use of regional anesthesia. The primary hypothesis was that postoperative opioid consumption would be reduced in the FN-LFCN block group.
Materials and methods
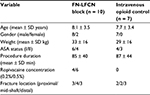
This single-center, prospective, double-blinded, randomized study was approved by the Institutional Review Board at Nationwide Children’s Hospital (IRB12-00820, IRB16-00338) and registered at ClinicalTrials.gov (NCT01759407). Written informed consent (and patient assent when age appropriate) was obtained from the parent or legal guardian of all patients enrolled in the study. Patients were eligible for inclusion if they were presenting for repair of traumatic fracture of the femur, were between 2 and 18 years old, had American Society of Anesthesia (ASA) physical status 1 or 2, and weighed ≥10 kg. The location of the femoral fracture (proximal, mid-shaft, or distal) was not considered when evaluating patients for study eligibility. Patients with comorbid cardiac, neurologic, or pulmonary diseases (not including asthma), requiring concomitant procedures, a positive urine pregnancy test, abnormal neurovascular examination or vascular compromise in the injured leg, a history of bleeding disorder or the use of therapeutic dose anticoagulants, or with an allergy to ropivacaine (Fresenius Kabi USA, Lake Zurich, Illinois, USA) or other amide-class anesthetic agents were excluded from enrollment. Patients were randomized (via a computer-generated entry provided in a sealed envelope) to either the FN-LFCN block or intravenous opioid group (control). An unplanned interim analysis (described further) was performed after 19 of 40 patients were enrolled, due to difficulty recruiting eligible subjects, and the study was discontinued at that point due to statistical futility. Of the 19 patients enrolled in the study, two were withdrawn due to deviations from the study protocol; the remaining 17 patients (15/2 male/female, age 8 ± 3 years) completed the study and had been randomly assigned to either the FN-LFCN block group (n = 10) or the intravenous opioid control group (n = 7).
Premedication with oral or intravenous midazolam, anesthesia induction via mask inhalation or intravenous medications, and the use of an oral endotracheal tube or laryngeal mask airway (LMA) were all at the discretion of the primary pediatric anesthesiologist. No opioids were administered during the induction of anesthesia. Following the induction of anesthesia and securing of the airway, the primary anesthesia team (attending anesthesiologist, certified registered nurse anesthetist, resident, or fellow) exited the operating room and the primary investigator or co-investigator entered the room. This was done in order to maintain the blinding of the primary anesthesia team to the randomization process. For patients randomized to the FN-LFCN block group, the investigator performed the ultrasound-guided femoral and LFCN blocks; otherwise, they merely monitored the patients in the control group. Ropivacaine with epinephrine was used as the local anesthetic for nerve blocks, with a cumulative dose of 2 mg/kg between the two block sites. Ropivacaine 0.2% with epinephrine 1:200,000 was used for patients between 10 kg and up to 25 kg in weight; ropivacaine 0.5% with epinephrine 1:200,000 was used for patients ≥25 kg. The maximum total volume delivered was 20 mL, with 75% of the total dose at the femoral site and the remaining 25% delivered at the lateral femoral cutaneous nerve site. Following placement of the blocks, the patient was prepped for the surgical procedure. At this time, the primary anesthesia team returned to the operating room for the remainder of the case.
Maintenance anesthesia consisted of isoflurane titrated to maintain the heart rate and blood pressure within 10% of the baseline values. The end-tidal volume of inhalational agent was recorded every 15 min. If hemodynamic parameters could not be maintained with isoflurane at an end-tidal concentration of 2%, supplemental fentanyl (1 µg/kg) was then administered. Upon completion of the surgical procedure, isoflurane was discontinued, the patient’s airway device was removed once appropriate criteria were met, and the patient was transferred to the post-anesthesia care unit (PACU).
In the PACU, a study nurse, who was blinded to the patient’s treatment group, assigned a pain score using the Objective Pain Scale at 5, 10, 20, and 30 min.10 Supplemental doses of intravenous fentanyl (0.5 µg/kg) were administered if the pain score was >4. Neither acetaminophen nor ketorolac was administered to the patient either intraoperatively or in the PACU. Patients were discharged from the PACU when discharge criteria were met per the Aldrete score. Upon discharge from the PACU, the principal investigator or co-investigator documented whether nerve blocks were used as well as whether medications were administered intraoperatively and in the PACU. At 24 h postoperatively, patients were either evaluated on the inpatient ward or contacted by telephone, if already discharged, in efforts to record a pain score.
Statistical analysis
All administered opioid doses were converted to an equivalent oral morphine dose (mg/kg) using the conversions listed in Table 1.11,12 Opioid requirements (intraoperative, in PACU, and on the ward) were compared using two-tailed unpaired t-tests, unless opioid consumption in a given period (eg, in PACU) was not normally distributed. The study was initially powered to detect a 1 standard deviation (SD) decrease in postoperative opioid consumption in the LFCN block group (at a confidence level of 95%), requiring 20 patients in each group to attain 86% power. An interim analysis of conditional power was performed after the first 19 patients were enrolled over a 3-year period. At this interim analysis, the conditional power of demonstrating a 1 SD decrease in opioid consumption on the ward in the FN-LFCN block group (if enrollment was to be completed as planned) was 8%. As the conditional power of the study fell below a conventional futility threshold (20%), the study was discontinued for statistical futility, and further analyses were performed as described further.
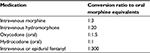  | Table 1 Equianalgesic opioid conversions used in the study Notes: Data from Gammaitoni et al.11 |
Apart from opioid consumption, the study groups were compared on time to first opioid administration on the inpatient ward; maximum Objective Pain Scale scores in the PACU; and intraoperative inhalation anesthetic agent end-tidal requirement (expressed as ET-Iso%). Continuous variables were summarized using means with SDs, and compared using unpaired t-tests; whereas non-normally distributed variables were summarized as medians with interquartile ranges (IQRs) and compared using Wilcoxon rank-sum tests. In an exploratory post hoc analysis, the patient population was divided by location of femur fracture (proximal, mid-shaft, or distal) to determine if the fracture location was associated with opioid requirements. Opioid consumption was compared across fracture locations using ANOVA for normally distributed data and a Kruskal–Wallis test for non-normally distributed data. Data analysis was performed in Stata/IC 13.1 (College Station, TX, USA: StataCorp, LP), and two-tailed p < 0.05 was considered statistically significant.
Results
Nineteen patients were enrolled in the study, of whom two were withdrawn due to deviations from the study protocol. The remaining 17 patients (15/2 male/female, age 8 ± 3 years) were randomly assigned to the FN-LFCN block group (n = 10) or the intravenous opioid control group (n = 7). Demographic characteristics, procedure duration, and ropivacaine concentration are summarized for the two study groups in Table 2. Study outcomes, including opioid consumption, postoperative Objective Pain Scale scores, and intraoperative inhalational agent requirements, are compared according to group assignment in Table 3. Opioid consumption values were normally distributed for the intraoperative dose and the dose received on the ward, but not for dose received in PACU. Opioid consumption on the ward did not significantly differ between the FN-LFCN block group (0.69 ± 0.33 ME mg/kg) and the control group [0.45 ± 0.28 ME mg/kg; difference of 0.24 ME mg/kg; 95% confidence interval (CI) of difference: −0.08, 0.57 ME mg/kg; p = 0.131]. Similarly, intraoperative and PACU opioid consumption did not significantly differ between the two groups (Table 3).
The median pain score in the PACU was 0 [interquartile range (IQR): 0, 0] in the FN-LFCN block group and 3 (IQR: 0, 4) in the control group. The difference between the groups did not reach statistical significance (95% CI: 0, 4; p = 0.056). The median end-tidal isoflurane concentration was 1.1% in the FN-LFCN block group (IQR 1.0, 1.4) and 1.5% in the control group (IQR 1.0, 1.7). The difference in the medians between the groups was 0.3% (95% CI −0.2, 0.6; p = 0.348). In the FN-LFCN block group, median time between PACU discharge and first opioid dose on the ward was 3.3 h (IQR: 2.8 h, 5.3 h), compared to 3.8 h (IQR: 2.9 h, 8.1 h) in the control group (95% CI: −2.2, 3.7; p = 0.558). In an exploratory analysis of opioid requirement according to the location of the femur fracture (proximal, mid-shaft, distal; Table 4), ANOVA F-tests found no statistically significant variation in the opioid dose intraoperatively (p = 0.853) or on the inpatient ward (p = 0.818); and a Kruskal–Wallis test found no statistically significant variation in opioid dose in the PACU (p = 0.947).
Discussion
The current study evaluated the efficacy of a regional anesthetic technique (FN + LFCN block) when compared to intravenous opioids in treating pain following operative repair of femoral fractures in the pediatric population. The use of a regional anesthetic technique did not result in improved analgesia as assessed by pain scores, did not decrease the intraoperative requirements of inhalational anesthetic agent, did not decrease intraoperative and postoperative opioid requirements, and did not increase the length of time to the administration of the first opioid after admission to the inpatient ward. The interim statistical analysis of the primary and secondary outcomes found that there was unlikely to be an advantage for the FN-LFCN block group should the study have been continued to the target number of 40 participants. The study was powered for a comparison of postoperative opioid consumption, and it would have been futile to continue it for the purpose of demonstrating lower opioid consumption in the FN-LFCN block group. However, difference in PACU pain scores, although not statistically significant (p = 0.056), can be interpreted as weak evidence in favor of the FN-LFCN block group for a difference in pain scores in the immediate postoperative period However, this potential improvement in analgesia did not result in a reduction in opioid needs during the postoperative period. Although the difference in medians approached clinical significance (some pain vs no pain), 2/7 patients in the control group did not report any pain in the PACU; therefore, even with this observed difference in medians, we cannot be confident that patients receiving the standard treatment do experience significant pain in the PACU. In light of the weak evidence suggesting a reduction in PACU pain scores among subjects in the FN-LFCN block group, a further study may be needed to evaluate the effectiveness of regional techniques for improved pain control in pediatric patients undergoing the surgical repair of femur fractures.
A potential explanation for the lack of significant analgesic benefit from an FN-LFCN block in the operative patient is related to the innervation of the femur, which not only demonstrates interpatient variability but also variation of the site of the femoral fracture (upper, middle, or lower femur). Although the primary innervation of the periosteum of the femur is the femoral nerve, there is additional innervation by the obturator and sciatic nerves. Variations in the type of surgical repair may impact the distribution that requires postoperative coverage to ensure adequate analgesia. There were multiple surgical techniques utilized for fracture repair within this study, including submuscular plating, intramedullary nailing, open reduction with internal fixation, flexible nailing with spica casting, and closed reduction with femoral shaft manipulation. Depending on the surgical approach taken for repair, an FN-LFCN block may have been insufficient to totally cover the required incision sites associated with the various fracture repair methods. Furthermore, the mechanism of injury may play a role in the degree of pain incited by the injury, such that lower-energy injury mechanisms may cause less periosteal disruption than high-energy mechanisms. Furthermore, variations in the initial care including splinting, application of traction, or simple immobilization of the fracture in the emergency department may serve to significantly reduce the amount of pain experienced by the patient. These variations in the initial care, level of fracture, method of surgical repair, as well as mechanism of injury would require a significantly greater and, likely, unobtainable number of patients in the study cohort. Most importantly, the postoperative pain scores in both groups were low with median pain scores (0–10 scale) of 0 in the regional anesthesia group and 3 in the intravenous opioid group. Although the attainment of a median pain score of 0 in the regional anesthesia group versus 3 in the intravenous opioid group might suggest a beneficial effect of regional anesthesia, the p-value achieved was only 0.056 and, therefore, the null hypothesis was rejected.
The concentration of the local anesthetic utilized for the nerve block may impact the degree of surgical anesthesia provided, together with the need for intraoperative and postoperative opioids. Given dosing limitations and the need to limit the total dose to ≤4 mg/kg of ropivacaine, 0.2% was used in the younger patients. However, based on the data obtained from this study, there was no difference in the number of patients requiring either intraoperative or postoperative opioids on comparing the postoperative outcome based on the concentration of the local anesthetic agent (0.2% vs 0.5%). Further interpretation of these findings may be limited by our study’s lack of data on block duration and time to regaining consciousness after the discontinuation of general anesthesia.
To date, there have been no other prospective, randomized, double-blinded trials published that investigated the use of femoral nerve blocks following surgical repair of femoral shaft fractures in either the adult or pediatric population. There is one ongoing study listed with ClinicalTrials.gov to prospectively investigate femoral nerve blockade for postoperative pain relief in pediatric patients undergoing surgical repair of femoral shaft fractures; however, there has been no study data released at this point. In the non-surgical adult population, using a prospective, randomized, but non-blinded study protocol, regional anesthetic techniques (3-in-1 block or FNB) have been shown to decrease morphine requirements and lower pain scores when compared to use of opioids alone.13–15 In a non-blinded, prospective, randomized study in a non-surgical population, Wathen et al reported lower pain scores in pediatric patients with a femur fracture who received a fascia iliaca compartment nerve block in the ED when compared to intravenous morphine.16 When comparing the entire 6-h study period pain scores, pain scores were approximately 15% lower in patients who received a fascia iliaca compartment nerve block. Additionally, with the regional anesthetic technique, the duration of analgesia was longer, less supplemental analgesic medication was required, and medical staff satisfaction scores were higher. In addition to these trials, other retrospective studies, case series, and case reports have demonstrated the successful use of regional anesthesia in the emergency department for the management of pain in both pediatric and adult patients with femoral shaft fractures.17,18
Our prospective, randomized, double-blinded study failed to demonstrate a statistical significance in pain scores and opioid requirements in pediatric patients with femur fracture who were treated with FN-LFCN blockade. As demonstrated by our study, this is a relatively heterogeneous population with variations in age, mechanism of injury, post-injury care, and the site of the femoral fracture (proximal, mid-shaft, or distal), which makes accruement of an adequate homogeneous study cohort problematic. The median pain scores were low in both groups (0 with regional anesthesia and 3 with opioids), suggesting that effective analgesia can be achieved with the aggressive use of opioids. One of the advantages of regional anesthesia remains its opioid-sparing effect, with the potential to limit opioid-induced adverse effects. Given the limited incidence of comorbid conditions, a significantly larger cohort would be required to demonstrate such an effect, given the low incidence of opioid-related adverse effects in the pediatric population. Furthermore, although we have previously demonstrated that regional anesthesia may facilitate outpatient discharge after specific orthopedic procedures, all of the patients in the current cohort were scheduled for inpatient care following their procedure, thereby eliminating this potential benefit.19
Disclosure
The authors report no conflicts of interest in this work.
References
Kuremsky MA, Frick SL. Advances in the surgical management of pediatric femoral shaft fractures. Curr Opin Pediatr. 2007;19(1):51–57. | ||
Simion C, Suresh S. Lower extremity peripheral nerve blocks in children. Tech Reg Anesth Pain Manag. 2007;11:222–228. | ||
Stewart B, Smith CT, Teebay L, Cunliffe M, Low B. Emergency department use of a continuous femoral nerve block for pain relief for fractured femur in children. Emerg Med J. 2007;24(2):113–114. | ||
Chu RS, Browne GJ, Cheng NG, Lam LT. Femoral nerve block for femoral shaft fractures in a paediatric emergency department: can it be done better? Eur J Emerg Med. 2003;10(4):258–263. | ||
Mutty CE, Jensen EJ, Manka MA Jr, Anders MJ, Bone LB. Femoral nerve block for diaphyseal and distal femoral fractures in the emergency department. J Bone Joint Surg Am. 2007;89(12):2599–2603. | ||
Tobias JD. Continuous femoral nerve block to provide analgesia following femur fracture in a paediatric ICU population. Anaesth Intensive Care. 1994;22(5):616–618. | ||
Fletcher AK, Rigby AS, Heyes FL. Three-in-one femoral nerve block as analgesia for fractured neck of femur in the emergency department: a randomized, controlled trial. Ann Emerg Med. 2003;41(2):227–233. | ||
Baker MD, Gullett JP. Ultrasound-guided femoral nerve blocks. Pediatr Emerg Care. 2015;31(12):864–868. | ||
Miller BR. Combined ultrasound-guided femoral and lateral femoral cutaneous nerve blocks in pediatric patients requiring surgical repair of femur fractures. Pediatr Anesth. 2011;21(11):1163–1164. | ||
Hannallah RS, Broadman LM, Belman AB, Abramowitz MD, Epstein BS. Comparison of caudal and ilioinguinal/iliohypogastric nerve blocks for control of post-orchiopexy pain in pediatric ambulatory surgery. Anesthesiology. 1987;66(6):832–834. | ||
Gammaitoni AR, Fine P, Alvarez N, McPherson ML, Bergmark S. Clinical application of opioid equianalgesic data. Clin J Pain. 2003;19(5):286–297. | ||
Guinard JP, Carpenter RL, Chassot PG. Epidural and intravenous fentanyl produce equivalent effects during major surgery. Anesthesiology. 1995;82(2):377–382. | ||
Somvanshi M, Tripathi A, Meena N. Femoral nerve block for acute pain in fracture shaft femur in an emergency ward. Saudi J Anaesth. 2015;9(4):439–441. | ||
Neubrand TL, Roswell K, Deakyne S, Kocher K, Wathen J. Fascia iliaca compartment nerve block versus systemic pain control for acute femur fractures in the pediatric emergency department. Pediatr Emerg Care. 2014;30(7):469–473. | ||
Turner AL, Stevenson MD, Cross KP. Impact of ultrasound-guided femoral nerve blocks in the pediatric emergency department. Pediatr Emerg Care. 2014;30(4):227–229. | ||
Wathen JE, Gao D, Merritt G, Georgopoulos G, Battan FK. A randomized controlled trial comparing a fascia iliaca compartment nerve block to a traditional systemic analgesic for femur fractures in a pediatric emergency department. Ann Emerg Med. 2007;50(2):162–171. | ||
Grossbard GD, Love BR. Femoral nerve block: a simple and safe method of instant analgesia for femoral shaft fractures in children. Aust N Z J Surg. 1979;49(5):592–594. | ||
McGlone R, Sadhra K, Hamer DW, Pritty PE. Femoral nerve block in the initial management of femoral shaft fractures. Arch Emerg Med. 1987;4(3):163–168. | ||
Schloss B, Bhalla T, Klingele K, Phillips D, Prestwich B, Tobias JD. A retrospective review of femoral nerve block for postoperative analgesia after knee surgery in the pediatric population. J Pediatr Orthop. 2014;34(4):459–461. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.