Back to Journals » International Journal of General Medicine » Volume 17
A Novel Radiological Scoring System for Anterior Longitudinal Ligament Injuries
Authors Li Y , Sun Y, Wu J, Gao Z, Qiu Y, Han L, Lu X
Received 6 November 2023
Accepted for publication 30 January 2024
Published 29 February 2024 Volume 2024:17 Pages 725—738
DOI https://doi.org/10.2147/IJGM.S446004
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Yang Li,1,* Yuling Sun,1,* Ji Wu,1,* Zhongya Gao,1 Youcai Qiu,1 Lin Han,2 Xuhua Lu1
1Department of Orthopaedics, Shanghai Changzheng Hospital, Naval Medical University, Shanghai, People’s Republic of China; 2Department of Orthopaedics, Third Affiliated Hospital of Naval Medical University, Shanghai, 200433, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xuhua Lu, Department of Orthopaedics, Shanghai Changzheng Hospital, Naval Medical University, No. 415 Fengyang Road, Shanghai, 200003, People’s Republic of China, Tel +86-21-81885793, Email [email protected] Lin Han, Department of Orthopaedics, Third Affiliated Hospital of Naval Medical University, Shanghai, 200433, People’s Republic of China, Email [email protected]
Background and Aim: Cervical hyperextension injury is very frequent with anterior longitudinal ligament (ALL) injury, and the ligament damage has a remarkable effect on whether and what type of operation should be performed. This study aims to establish a new scoring system for the accurate diagnosis of ALL damage.
Methods: The imaging data of the consecutive patients was measured and scored by four radiologists. Intraoperative exploration was performed by three surgeons. The crude and adjusted odds ratios (cOR and aOR) and receiver operating characteristic curve (ROC) were constructed to assess the diagnostic accuracy of the scoring system.
Results: A total of 255 patients with cervical spine trauma were included in this study. There was no statistical difference in the relationship between demographics and ALL injuries (P > 0.05). Thickness of prevertebral soft tissue (aOR = 11.922, P = 0.004), intervertebral disk angle (aOR = 13.21, P = 0.002), avulsion fracture of the anterior edge of the vertebral body (aOR = 13.844, P = 0.029), ALL disrupted in T1-weighted sequence (aOR = 18.349, P < 0.001), and high signal area in T2-weighted sequence (aOR = 20.898, P = 0.002) had significantly higher diagnostic accuracy. The scoring system’s sensitivity and specificity were 94.0% and 88.1%, respectively, and the accuracy was 90.8%.
Conclusion: The study established a new scoring system for ALL injuries based on the analysis of a series of clinical data and statistics. A total of five scoring items, a total score of 7 points, and an ALL injury may be diagnosed when the score is not less than 3 points. This scoring system enables an efficient and accurate diagnosis of all injuries.
Keywords: cervical hyperextension injury, anterior longitudinal ligament injury, cervical spine trauma, scoring system
Introduction
Cervical hyperextension injuries are spinal cord injuries in the hyperextended position caused by hyperextension violence and account for 35–60% of all types of cervical spine injuries.1,2 The cervical hyperextension injury is denoted by compression of spinal cord against the ligamentum flavum (posteriorly) and posterior aspects of the intervertebral discs and vertebral bodies (anteriorly).3,4 In the late 1800s, Sir William Thorburn reported a series of nine cervical spinal injuries in which one patient demonstrated hand function to be more severely affected than leg function.5,6 He hypothesized that this unique symptom was caused by a central gray matter hemorrhage in the spinal cord.4 Six decades later, Richard Schneider reported a series of patients with similar cervical spine trauma who had similar symptoms and more severe hand hypofunction than arm and leg, who introduced the concept of “cervical cord syndrome (CCS)” which is characterized by disproportionately more motor impairment of the upper than of the lower extremities, bladder dysfunction, usually urinary retention, and varying degrees of sensory loss below the level of the lesion.7
CCS is often accompanied by cervical spine fractures or soft tissue trauma. The most injured soft tissue is the anterior longitudinal ligament (ALL).8 The severity of the injury depends on whether the mechanical stability of the spine or the integrity of the spinal cord has been compromised. Instability can lead to further injury, pain, or deformity and often requires surgery.9
Cervical fractures can be easily diagnosed by computed tomography (CT), but accurate diagnosis of ALL injuries remains challenging for the clinicians. At current, magnetic resonance imaging (MRI) is the most widely used in the diagnosis of the injury.10–17 However, the sensitivity of the MRI is low.5,18 In addition, Goradia et al19 reported the false-negative rate up to the 71%, which is very high.
Due to the lack of an objective and precise method for evaluating ALL injury, surgeons rely on the clinical expertise. The purpose of this study is to bring forward a new scoring system for accurately measuring ALL damage.
Patients and Methods
Data Collection and Study Protocols
A total of 255 consecutive patients with cervical spine trauma between 2015 and 2023 at the Department of Spinal surgery of our hospital were included in this study. The inclusion criteria were as followed: (1) If the mechanism of injury was hyperextension; (2) the sensorimotor function of the upper limb was more severe than that of the lower limb; (3) cervical X-ray, CT and MRI examination were completed within 3 days of injury; and (4) anterior cervical surgery. The exclusion criteria were as followed: (1) imperfect or incomplete imaging data; (2) patients less than 18 years old; (3) patients with history of severe head trauma or cervical trauma or surgery; (4) combined with fractures of limbs or pelvis; (5) cervical fracture and dislocation; (6) endotracheal intubation or tracheostomy before imaging examination; (7) conservative treatment; (8) patient or family refused to consent. A preliminary scoring system was established for 81 ALL-intact patients and 65 ALL injured cases. Fifty-nine ALL intact cases and 50 ALL injured cases were used as a validation set to test the diagnostic efficiency of the scoring system.
Initially, the data of 329 patients with cervical hyperextension injury without cervical fracture were recorded. Seventy-four patients were excluded, of which 15 patients had only hand myodynamia and hyperalgesia, and CT and MRI did not indicate cervical instability and spinal cord high signal. These patients received conservative treatment, including hormones, mannitol, nutritional nerves, etc. Their symptoms were significantly improved. Forty-three patients underwent posterior surgery, including laminectomy, laminoplasty and so on. Sixteen patients’ data were incomplete or loss of follow-up.
Ethical Statement
All case data and imaging materials included in this article have obtained explicit consent from the patients themselves. All patient information has undergone de-identification to ensure the protection of patient privacy. Additionally, the patient images displayed in Figure 1 have also obtained consent from the patients.
Clinical Assessment and Management
The age, sex, body mass index (BMI), injury mechanism, and injury segments of the patient were included in the study, and the American Spinal Cord Injury Association (ASIA) scoring system20 and Japanese Orthopaedical Association21 (JOA) were used to grade the degree of spinal cord injury and quantify the motor-sensory function of the patients. MRI and CT scans were evaluated by four radiologists on an IMPAX EE workstation (Agfa HealthCare, Bonn, Germany). The gold standard for diagnosing ALL injury depends on intraoperative exploration.
Medical Imaging
All patients completed the imaging examination of X-ray, CT, and MRI within 48 hours after admission. The fracture, joint dislocation, or bone structure change of cervical vertebra mainly diagnosed on X-ray and CT, and soft tissue injury was detected mainly on MRI.17 MRI was performed with the use of a 1.5 T magnet and 3-mm section thickness for an axial and sagittal plane. CT and X-ray were used to evaluate the following indicators (Table 1 and Figures 2–4). Among them, thickness of prevertebral soft tissue (TOPST), intervertebral disk angle (IDA), avulsion fracture of the anterior edge of the vertebral body (AFOA), facet joint dislocation (FJD), ALL disrupted in T1-weighted sequence (T1D), T2-weighted sequence (T2HS), and articular capsule in T2-weighted sequence (T2AC) were measured by four radiologists.
 |
Table 1 Indexes and Observation Methods |
Statistical Analysis
All the patients included in this study were divided into two groups (ALL intact and ruptured group). The demographic characteristics of the patients (as sex, age, time of injury, etiology, ASIA score) were statistically evaluated. Continuous variables were presented in mean ± SD, and non-continuous variables were presented in frequency. The t-test and chi-square test of independent samples were used to compare the differences between the two groups. Receiver operating characteristic (ROC) curve was constructed to assess the diagnostic accuracy of the scoring system, and the accuracy was quantified by the area under the ROC curve (AUC). Univariate analyses were performed for all factors individually using binary logistic regression analysis. A multivariate binary logistic regression was applied to identify independent risk factors using variables with a P < 0.05 by univariate analysis. To manage any issues with multicollinearity, we used a stepwise method and applied an entry condition of P < 0.05 and removal condition of P > 0.05, and the final model included only significant variables having P < 0.05. Crude odds ratios (cORs) and adjusted odds ratios (aORs) and 95% confidence intervals (CI) were calculated for all variables. The result of sensitivity+specificity-1 is Youden’s index, and the maximum value of the index is cut-off value. P < 0.05 was the statistically significant criterion, all tests were calculated using SPSSv26 (IBM, Armonk, New York), all figures were using Prism 9 and the data of all images were measured by Image J Version 1.2.4.
Result
Baseline Characteristics
A total of 146 patients (65 in ALL rupture group or group 2 and 81 in the ALL-intact group or group 1) (Table 1). The average age (year) of all the included patients was 57.64 ± 10.42 and 54.34 ± 12.27. No statistical differences were found in the baseline characteristics between the two groups (P > 0.05).
Injury Mechanism
Fall was the leading cause of injury, with 95 incidents (65.07%). In the ALL intact and rupture groups, 53 (65.43%) and 42 cases (64.6%), respectively, were followed by traffic accident and falling objects. The number of car accidents in the two groups was 22 (27.16%) and 16 (24.6%), and the number of smashing injury (head and neck injuries caused by falling objects) was 6 (7.41%) and 7 (10.8%). The relationship between ALL injury and injury mechanism was not statistically significant (P > 0.05).
Patients’ ASIA and JOA Score
The ASIA D grade had the most patients (Table 2), 48 cases (59.26%) in the group 1 and 31 cases (47.7%) in the group 2, followed by ASIA C grade with a total of 50 cases (31.03%). There were 26 instances in the negative group (32.1%) and 24 cases in the positive group (36.9%). There was no obvious correlation between ASIA grade and ALL injury in this study. The overall score of the two groups was 202.04 ± 70.02 and 203.12 ± 78.25, and there was no significant statistical difference between them. JOA scores (9.93 ± 3.85 vs 10.14 ± 4.6) were also not found to be significantly different between the two groups.
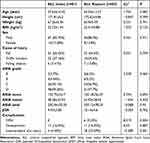 |
Table 2 Patients: Demographics and Characteristics |
Univariate and Multivariate Analysis of Risk Factors for the Two Groups
The results of univariate and multivariate logical regression analysis showed that there were differences in TOPST (aOR = 11.922, P = 0.004), IDA (aOR = 13.21, P = 0.002), AFOA (aOR = 13.844, P = 0.029), T1D (aOR = 18.349, P < 0.001), and T2HS (aOR = 20.898, P = 0.002) between the two groups (Table 3).
 |
Table 3 Univariate and Multivariate Analysis of Risk Factors for the Two Groups |
Diagnostic Evaluation Index of the T1D and T2HS
In this study, the sensitivity for T1D was 80%, with a specificity of 92.5% and the accuracy of 86.9%. For T2HS, the sensitivity was 92.3%, specificity was 64.7%, and accuracy was 75.3% (Table 4).
 |
Table 4 Diagnostic Evaluation Index of the T1D and T2HS |
Critical Value of TOPST and IDA
TOPST and IDA are continuous variables among the five indicators. The sensitivity and specificity values were calculated by ROC. Finally, a series of Youden’s index were obtained, in which the maximum value of the index was the boundary value of TOPST and IDA. The results showed that (Table 5), when TOPST is 2.3 and IDA is 17.2, the Youden’s index is the highest, which means that 2.3 and 17.2 were its cut-off value.
 |
Table 5 Critical Value of TOAST and IDA |
Cases Score and Distribution of Each Score
Imaging data of 146 cases were scored by other four radiologists. The score for each indicator is based on aOR, so T1D and T2HS score 2 points and the rest are 1 point (Table 6). The results showed that the total scores of group 1 were concentrated below 3 points, and the total scores of group 2 were mostly above 3 points (Table 7).
 |
Table 6 The Score Value of Each Indicator |
 |
Table 7 Distribution of Each Score |
Critical Value of Total Score
The Youden’s index of the total points was calculated in the same way as above, and when the total score was 3 (Table 8), the Youden’s index was the highest. In other words, when the scoring system was used to analyze the rupture of the ALL if the total point is not less than 3 points, there was a strong possibility of correctly diagnosing the injury.
 |
Table 8 Critical Value of Total Score |
Diagnostic Evaluation Index of the Scoring System
One hundred and nine patients were included in the test group, including 59 patients with ALL intact and 50 with injury, and the cases were scored for each index using the same method (Table 9). The results showed that 7 of the 59 patients had a total score higher than 3, and only 3 of the 50 had scores lower than 3. Therefore, the sensitivity of this scoring system was 91.3%, the specificity was 88.1%, and the accuracy was 90.8% (Table 10). The ROC curve results showed an AUC of 0.9356 (95% CI = 0.8783–0.9928) for this scoring system (Figure 5).
 |
Table 9 The Score of Each Index of the Test Group |
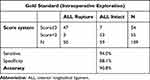 |
Table 10 Diagnostic Evaluation Index of the Scoring System |
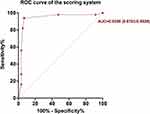 |
Figure 5 Receiver operating characteristic curve. |
Typical Cases
The typical cases of this study are presented in the attached Figures 2–4.
Discussion
Cervical hyperextension injury is the most common injuries treated in emergency departments in US hospitals with incidence rates ranging from 28 to 834 per 100,000 population each year and recently estimated at 300 per 100,000 population in Western countries,22 which is mainly characterized by CCS. Those patients with no severe neurological symptoms, no fracture and no obvious compression of the spinal cord can be treated conservatively. However, patients with ligament injury must be treated by surgery as soon as possible, which means that the stability of the cervical spine is destroyed. Dietmar’s study suggests that hyperextension instability warrants decompression and ACDF, regardless of neurological symptoms’ severity. Non-surgical treatment risks repeated hyperextension and spinal cord compression during recovery, even with cervical orthosis, potentially hindering neurological healing.23 The most injured ligament is ALL. In addition, when the cervical spine was bluntly injured, there was a statistical link between the degree of ligament damage and spinal cord injury.14,24 As a result, accurate assessment of ALL injury is critical for determining whether the patients require surgical therapy. If yes, what type of procedure should be chosen.
Compared with MRI, the sagittal image of CT can clearly show the boundary of prevertebral soft tissue. Similarly, radiologists can clearly distinguish the boundary of the vertebral body on CT images and accurately measure IDA. Flexion and extension radiograph is a common method for the diagnosis of cervical instability. Although, some patients in this study underwent flexion and extension radiographic examination, however, this method is limited as cannot be applied to patients with quadriplegia or coma. Therefore, it is not included in the scoring system. For generalization examination including for those paralyzed, first, patient maintains the supine position, the hyperextension position depends on the shoulder cushion, and the flexion position is realized by the occipital cushion (Figure 1). A total of 19 patients in this study accepted the test, and the test indicated that 7 of the unstable patients were accompanied by ALL injury (7/9, 77.78%). The sensitivity of this method was 63.64% (7/11). To improve the applicability of this method, the following issues need to be further explored, such as the height and position of the mat and the safety of the method. Diffuse idiopathic skeletal hyperostosis (DISH) is a systemic condition characterized by the presence of at least three bony bridges at the anterolateral spine opposite to the aorta. In this study, six patients were complicated with DISH, and all of them had ALL damage, all of which were in C5-7 (Figure 2). Whether DISH will affect the location and incidence of ALL damage has not been confirmed.
In this study, 146 cases were separated into ALL intact and rupture group according to the results of intraoperative exploration, the most vulnerable sector was C4/5. However, in the Thompson25 and Maeda’s findings,12 the most damaged region was C3/4, followed by C4/5. This difference in findings might be due to most of the patients with cervical hyperextension injury were ASIA D grade (54.1%, n = 81), primarily because most of the patients included at this time were without fracture and dislocation. The neurological symptoms were mild,25 and secondly, because cervical hyperextension injury frequently appeared central spinal cord injury syndrome, the common phenomenon being that severe nervous system symptoms appeared in a short time after injury, and early use of mannitol and methylprednisolone will reduce the patient’s neurological symptoms. As a result, when some patients are examined by a doctor, their physical signs will be less severe than those observed at the scene of the injury.
The scoring system includes seven markers based on clinical experience and a review of a wide number of literatures, including TOPST, IDA, AFOA and so on.12,19,26–30 C3 prevertebral soft tissue shadow was utilized to represent C1-4 because it is less impacted by skull base shadow and easier to measure. C6 indicates C5-7 because the prevertebral soft tissue shadow of C6 is less easily impacted by laryngeal movement than C4 or C5. Additionally, it is less concealed by the muscles and bones surrounding the cervicothoracic region than other lower cervical vertebral segments.26 Saifuddin’s research31 shows that in MRI’s T1-weighted image, 74–79% of ALL, T1-weighted images were the optimum pulse sequence for seeing the anterior longitudinal ligament because there was a substantial contrast between the anterior low signal ligament of the vertebral body and the intermediate and high signal intensity prevertebral soft tissue and intervertebral disc.5 Although the edema signal around the ALL damage can be seen during the acute phase of the ALL injury, it was a secondary indication that may have faded by the time the patient was checked by MRI. The results of this study showed that 91 (62.3%, n = 146) patients had prevertebral high signal intensity. Maeda’s study showed that 83% of the patients with cervical hyperextension injury without obvious fracture and dislocation had different degrees of prevertebral high signal intensity.12 According to Jonas and Johnson’s research,32,33 the facet joint capsule of the cervical vertebrae was more significant than ligaments in preserving the stability of the cervical vertebrae. According to Samartzis’s study,34 articular capsules play a vital function in the stability of cervical vertebrae. Tanishima35 feels that cervical facet joint effusion was a component that contributes to cervical instability. As a result, the high signal intensity of cervical facet dislocation and T2 weighted joint capsule was included in the research; however, the findings were unsatisfactory. The cOR of FJD was 3.138 (P = 0.108) and T2AC was 4.017 (P = 0.096). The reason is that there were less joint dislocation or joint capsule effusion in the cases we included, so the diagnostic value was not great.
When the cervical X-ray results were normal, a dynamic flexion and extension examination was performed to look for symptoms of occult ligament and intervertebral disc damage caused by subluxation or angle changes of neighboring vertebrae from flexion to extension. However, if individuals with severe pain or muscular spasms do not extend enough, this might result in erroneous negative findings.36 Wang37 argued that taking cervical flexion and extension radiographs on a frequent basis in critically wounded individuals should be avoided, as they may lead to further harm to the patients. Vaccaro,13 on the other hand, feels that patients who do not have serious cervical fractures and dislocations can have the examination performed in the presence of a surgeon. Giuliano38 suggests used motion MRI to measure the extent of cervical soft tissue damage, and the findings of that investigation support this viewpoint. Song’s study27 demonstrates that MRI can properly assess the degree of cervical soft tissue injury and suggests a soft tissue injury grading technique based on the injury degree of ALL, disc, posterior longitudinal ligament (PLL), interspinous ligament (ISL), and posterior neck muscle (PNM) of cervical vertebrae. Grand I contains ALL damage, Grand II includes ALL and disc damage, and so on; Grand V includes the five structural damages listed above. However, there were several clear limitations to this study. If only individuals with disc and PLL injury were present, they will generally produce significant cervical spinal cord injury, but they will not be identified in the grading system. Therefore, at present, cervical whiplash injury still lacks an objective and appropriate grading standard to guide the next step of treatment.
Lee39 believes that both edematous shadow and adipose tissue were hyperintense in the T2-weighted phase of MRI, and the results showed that the use of fat-suppressed T2-weighted phase can accurately evaluate ligament damage. Molière’s40 research showed that the paraspinal fat pad (PFP) can be used as an indicator at CT of an injury of cervical spine posterior ligamentous complex (PLC). Similarly, the study of predicting ALL injury by paraspinal fat changes will be included in the next research plan.
A single imaging study alone cannot accurately determine ALL injury. Shiau et al26 analyzed radiographs of 826 patients with cervical spine trauma and concluded that C3 and C6 prevertebral soft-tissue thickening can predict upper and lower cervical soft-tissue injury, respectively, but further MRI is needed to determine whether ligament or disc injury is involved. Numerous studies recommended that patients with cervical trauma using CT since the utility of X-ray in acute cervical trauma is limited.26,41 Even if the CT results were negative, cervical ligament damage cannot be ruled out. This viewpoint was supported by Onoue’s study,42 which indicated that 31% of cervical CT negative cases had significant damage discovered by MRI, indicating that it is better to employ both MRI and CT in patients with blunt cervical trauma.43 Even MRI, which is accurate in soft-tissue imaging, has been unsatisfactory in diagnosing ALL injuries. The results of Haris et al 18 showed that the sensitivity of MRI in the diagnosis of ALL injury was only 66.6%. Our results showed a sensitivity of 80% and an accuracy of 86.9% for T1D. The sensitivity of T2HS was 92.3%, but the specificity was only 64.7% (Table 4).
This study has several limitations. First, since cases of ALL injury are very valuable, to reduce bias in the data, statistical experts do not recommend grading injury with a small caseload as done in the current study. Secondly, if only TOPST and T2HS are positive, the system cannot confirm the location of the injury, because AFOA, IDA and T1D can localize the injury site. Therefore, localization of the injury should be the focus of future research. T
Conclusion
The study established a new scoring system (Table 11) for ALL injury (ALLISS) by measuring a series of clinical data and statistical analysis, a total of five scoring items, the total score of 7 points, and ALL injury may be diagnosed when the score is not less than 3 points. ALLISS enables efficient and accurate diagnosis of ALL injury. However, further studies especially prospective clinical trials are needed before the final recommendations are made.
 |
Table 11 Scoring System of ALL Injury |
Availability of Data and Materials
All the data contained in this study are authentic and reliable.
Ethics Declarations
This study was performed in line with the principles of the Declaration of Helsinki. This study was approved by the Ethics Committee of Shanghai Changzheng Hospital, Naval Medical University (IRB: 2020-12-0547). Both verbal and written informed consent were obtained from all individual participants included in the study.
Consent for Publication
All data about this study are contained and presented in this document.
Acknowledgments
We thank the University Affiliated Hospital of Shanghai Hospital of Traditional Chinese Medicine (Project ZY3-LCPT-2-1005), Science and Technology Innovation Action Plan from The Science and Technology Commission of Shanghai Municipality (23Y11903100), and Investigator-initiated Clinical Research Projects Conducted in the Demonstration Research Ward of Shanghai Changzheng Hospital (2023YJBF-PY04) for their financial support. Gratitude is also extended to the patients who participated in our study, providing invaluable data. Lastly, we appreciate the editorial team of this journal for their insightful review and guidance.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Project of the University Affiliated Hospital of Shanghai Hospital of Traditional Chinese Medicine, (ZY3-LCPT-2-1005); Science and Technology Innovation Action Plan from The Science and Technology Commission of Shanghai Municipality (23Y11903100); Investigator-initiated Clinical Research Projects Conducted in the Demonstration Research Ward of Shanghai Changzheng Hospital (2023YJBF-PY04).
Disclosure
All authors declare that they have no conflicts of interest in this work.
References
1. Tominaga Y, Ndu AB, Coe MP, et al. Neck ligament strength is decreased following whiplash trauma. BMC Musculoskelet Disord. 2006;7(1):103. doi:10.1186/1471-2474-7-103
2. Rodriquez AA, Barr KP, Burns SP. Whiplash: pathophysiology, diagnosis, treatment, and prognosis. Muscle Nerve. 2004;29(6):768–781. doi:10.1002/mus.20060
3. Aarabi B, Koltz M, Ibrahimi D. Hyperextension cervical spine injuries and traumatic central cord syndrome. Neurosurgical Focus. 2008;25(5):E9. doi:10.3171/FOC.2008.25.11.E9
4. Avila MJ, Hurlbert RJ. Central cord syndrome redefined. Neurosurg Clin N Am. 2021;32(3):353–363. doi:10.1016/j.nec.2021.03.007
5. Henninger B, Kaser V, Ostermann S, et al. Cervical disc and ligamentous injury in hyperextension trauma: MRI and intraoperative correlation. J Neuroimaging. 2020;30(1):104–109. doi:10.1111/jon.12663
6. Rao SK, Wasyliw C, Nunez DB Jr. Spectrum of imaging findings in hyperextension injuries of the neck. Radiographics. 2005;25(5):1239–1254. doi:10.1148/rg.255045162
7. Schneider RC, Cherry G, Pantek H. The syndrome of acute central cervical spinal cord injury; with special reference to the mechanisms involved in hyperextension injuries of cervical spine. J Neurosurg. 1954;11(6):546–577. doi:10.3171/jns.1954.11.6.0546
8. Siegmund GP, Myers BS, Davis MB, Bohnet HF, Winkelstein BA. Mechanical evidence of cervical facet capsule injury during whiplash: a cadaveric study using combined shear, compression, and extension loading. Spine. 2001;26(19):2095–2101. doi:10.1097/00007632-200110010-00010
9. Benedetti PF, Fahr LM, Kuhns LR, Hayman LA. MR imaging findings in spinal ligamentous injury. AJR Am J Roentgenol. 2000;175(3):661–665. doi:10.2214/ajr.175.3.1750661
10. Malham GM, Ackland HM, Varma DK, Williamson OD. Traumatic cervical discoligamentous injuries: correlation of magnetic resonance imaging and operative findings. Spine. 2009;34(25):2754–2759. doi:10.1097/BRS.0b013e3181b6170b
11. Katzberg RW, Benedetti PF, Drake CM, et al. Acute cervical spine injuries: prospective MR imaging assessment at a level 1 trauma center. Radiology. 1999;213(1):203–212. doi:10.1148/radiology.213.1.r99oc40203
12. Maeda T, Ueta T, Mori E, et al. Soft-tissue damage and segmental instability in adult patients with cervical spinal cord injury without major bone injury. Spine. 2012;37(25):E1560–E1566. doi:10.1097/BRS.0b013e318272f345
13. Vaccaro AR, Madigan L, Schweitzer ME, Flanders AE, Hilibrand AS, Albert TJ. Magnetic resonance imaging analysis of soft tissue disruption after flexion-distraction injuries of the subaxial cervical spine. Spine. 2001;26(17):1866–1872. doi:10.1097/00007632-200109010-00009
14. Martínez-Pérez R, Cepeda S, Paredes I, Alen JF, Lagares A. MRI prognostication factors in the setting of cervical spinal cord injury secondary to trauma. World Neurosurg. 2017;101:623–632. doi:10.1016/j.wneu.2017.02.034
15. Awad BI, Carmody MA, Lubelski D, et al. Adjacent level ligamentous injury associated with traumatic cervical spine fractures: indications for imaging and implications for treatment. World Neurosurg. 2015;84(1):69–75. doi:10.1016/j.wneu.2015.02.029
16. Choi SJ, Shin MJ, Kim SM, Bae SJ. Non-contiguous spinal injury in cervical spinal trauma: evaluation with cervical spine MRI. Korean J Radiol. 2004;5(4):219–224. doi:10.3348/kjr.2004.5.4.219
17. Holmes JF, Mirvis SE, Panacek EA, et al.. Variability in computed tomography and magnetic resonance imaging in patients with cervical spine injuries. J Trauma. 2002;53(3):524–529; discussion 530. doi:10.1097/00005373-200209000-00021
18. Haris AM, Vasu C, Kanthila M, Ravichandra G, Acharya KD, Hussain MM. Assessment of MRI as a modality for evaluation of soft tissue injuries of the spine as compared to intraoperative assessment. J Clin Diagn Res. 2016;10(3):TC01–TC05. doi:10.7860/JCDR/2016/17427.7377
19. Goradia D, Linnau KF, Cohen WA, Mirza S, Hallam DK, Blackmore CC. Correlation of MR imaging findings with intraoperative findings after cervical spine trauma. AJNR Am J Neuroradiol. 2007;28(2):209–215.
20. Maynard FM Jr, Bracken MB, Creasey G, et al. international standards for neurological and functional classification of spinal cord injury. American spinal injury association. Spinal Cord. 1997;35(5):266–274.
21. Yonenobu K, Abumi K, Nagata K, Taketomi E, Ueyama K. Interobserver and intraobserver reliability of the Japanese orthopaedic association scoring system for evaluation of cervical compression myelopathy. Spine. 2001;26(17):1890–1894. doi:10.1097/00007632-200109010-00014
22. Shateri H, Cronin DS. Out-of-position rear impact tissue-level investigation using detailed finite element neck model. Traffic Inj Prev. 2015;16(7):698–708. doi:10.1080/15389588.2014.1003551
23. Krappinger D, Lindtner RA, Zegg MJ, et al. Spondylotic traumatic central cord syndrome: a hidden discoligamentous injury?. Eur Spine J. 2019;28(2):434–441. doi:10.1007/s00586-018-5796-5
24. Martinez-Perez R, Paredes I, Cepeda S, et al. Spinal cord injury after blunt cervical spine trauma: correlation of soft-tissue damage and extension of lesion. AJNR Am J Neuroradiol. 2014;35(5):1029–1034. doi:10.3174/ajnr.A3812
25. Thompson C, Gonsalves JF, Welsh D. Hyperextension injury of the cervical spine with central cord syndrome. Eur Spine J. 2015;24(1):195–202. doi:10.1007/s00586-014-3432-6
26. Shiau JP, Chin CC, Yeh CN, et al. Does the ratio and thickness of prevertebral soft tissue provide benefit in blunt cervical spine injury?. Eur J Trauma Emerg Surg. 2013;39(3):297–303. doi:10.1007/s00068-013-0270-x
27. Song K-J, Kim G-H, Lee K-B. The efficacy of the modified classification system of soft tissue injury in extension injury of the lower cervical spine. Spine. 2008;33(15):E488–493. doi:10.1097/BRS.0b013e31817b6191
28. Alhilali LM, Fakhran S. Evaluation of the intervertebral disk angle for the assessment of anterior cervical diskoligamentous injury. AJNR Am J Neuroradiol. 2013;34(12):2399–2404. doi:10.3174/ajnr.A3585
29. Kliewer MA, Gray L, Paver J, et al. Acute spinal ligament disruption: MR imaging with anatomic correlation. J Magn Reson Imaging. 1993;3(6):855–861. doi:10.1002/jmri.1880030611
30. Kumar Y, Hayashi D. Role of magnetic resonance imaging in acute spinal trauma: a pictorial review. BMC Musculoskelet Disord. 2016;17(1):310. doi:10.1186/s12891-016-1169-6
31. Saifuddin A, Green R, White J. Magnetic resonance imaging of the cervical ligaments in the absence of trauma. Spine. 2003;28(15):1686–1691; discussion 1691–1682. doi:10.1097/01.BRS.0000083166.22254.BA
32. Jonas R, Demmelmaier R, Wilke H-J. Influences of functional structures on the kinematic behavior of the cervical spine. Spine J. 2020;20(12):2014–2024. doi:10.1016/j.spinee.2020.07.017
33. Johnson RM, Crelin ES, White AA, Panjabi MM, Southwick WO. Some new observations on the functional anatomy of the lower cervical spine. Clin Orthop Relat Res. 1975;111(111):192–200. doi:10.1097/00003086-197509000-00027
34. Samartzis D, Wein SM, Shen FH, Beazell J, Francke EI, Anderson DG. A revisitation of distractive-extension injuries of the subaxial cervical spine: a cadaveric and radiographic soft tissue analysis. Spine. 2010;35(4):395–402. doi:10.1097/BRS.0b013e3181c9fa35
35. Tanishima S, Mihara T, Ogawa S, Takeda C, Fujiwara S, Nagashima H. Bilateral facet effusion is a risk factor for segmental instability with cervical injury without vertebral fracture. Sci Rep. 2021;11(1):12531. doi:10.1038/s41598-021-91981-y
36. Geck MJ, Yoo S, Wang JC. Assessment of cervical ligamentous injury in trauma patients using MRI. J Spinal Disord. 2001;14(5):371–377. doi:10.1097/00002517-200110000-00001
37. Wang JC, Hatch JD, Sandhu HS, Delamarter RB. Cervical flexion and extension radiographs in acutely injured patients. Clin Orthop Relat Res. 1999;365(365):111–116. doi:10.1097/00003086-199908000-00015
38. Giuliano V, Giuliano C, Pinto F, Scaglione M. Soft tissue injury protocol (STIP) using motion MRI for cervical spine trauma assessment. Emerg Radiol. 2004;10(5):241–245. doi:10.1007/s10140-004-0327-6
39. Lee HM, Kim HS, Kim DJ, Suk KS, Park JO, Kim NH. Reliability of magnetic resonance imaging in detecting posterior ligament complex injury in thoracolumbar spinal fractures. Spine. 2000;25(16):2079–2084. doi:10.1097/00007632-200008150-00012
40. Moliere S, Zaragori-Benedetti C, Ehlinger M, Le Minor JM, Kremer S, Bierry G. Evaluation of paraspinal fat pad as an indicator of posterior ligamentous complex injury in cervical spine trauma. Radiology. 2017;282(3):790–797. doi:10.1148/radiol.2016160330
41. Pollack CV Jr, Hendey GW, Martin DR, Hoffman JR, Mower WR, Group N. Use of flexion-extension radiographs of the cervical spine in blunt trauma. Ann Emerg Med. 2001;38(1):8–11. doi:10.1067/mem.2001.116810
42. Onoue K, Farris C, Burley H, et al. Role of cervical spine MRI in the setting of negative cervical spine CT in blunt trauma: critical additional information in the setting of clinical findings suggestive of occult injury. J Neuroradiol. 2021;48(3):164–169. doi:10.1016/j.neurad.2019.05.001
43. Schoenfeld AJ, Bono CM, McGuire KJ, Warholic N, Harris MB. Computed tomography alone versus computed tomography and magnetic resonance imaging in the identification of occult injuries to the cervical spine: a meta-analysis. J Trauma. 2010;68(1):109–113; discussion 113–104. doi:10.1097/TA.0b013e3181c0b67a
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




