Back to Journals » International Journal of General Medicine » Volume 16
A Nomogram-Based Model for Predicting the Risk of Severe Acute Cholangitis Occurrence
Authors Xu J , Xu ZX, Zhuang J , Yang QF , Zhu X , Yao J
Received 6 April 2023
Accepted for publication 16 July 2023
Published 25 July 2023 Volume 2023:16 Pages 3139—3150
DOI https://doi.org/10.2147/IJGM.S416108
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Hyam Leffert
Jian Xu, Zhi-Xiang Xu, Jing Zhuang, Qi-Fan Yang, Xin Zhu, Jun Yao
Department of Gastroenterology, the Affiliated People’s Hospital of Jiangsu University, Zhenjiang, Jiangsu Province, 212000, People’s Republic of China
Correspondence: Jun Yao, Department of Gastroenterology, the Affiliated People’s Hospital of Jiangsu University, Zhenjiang, Jiangsu Province, 212000, People’s Republic of China, Tel +86-13952943749, Email [email protected]; [email protected]
Background: Acute cholangitis is a severe inflammatory disease associated with an infection of the biliary system, which can lead to complications and adverse outcomes. The existing nomogram-based risk assessment methods largely rely on a limited set of clinical features and laboratory indicators, and are mostly constructed using univariable models, which have limitations in predicting the severity. This study aims to develop a nomogram-based model that integrates multiple variables to improve risk prediction for acute cholangitis.
Methods: Data were retrospectively collected from 152 patients with acute cholangitis who attended the People’s Hospital of Jiangsu University between January 2019 and March 2022, and were graded as having mild to moderate versus severe cholangitis according to the 2018 Tokyo guidelines. Univariate and multivariate analyses were employed to discern independent risk factors associated with severe acute cholangitis, which were subsequently integrated into a nomogram model. The efficacy of the model was appraised by leveraging Receiver Operating Characteristic (ROC) curves, calibration curves, and Decision Curve Analysis (DCA).
Results: Aspartate to alanine transaminase ratio (Transaminase ratio or TR), Neutrophil-lymphocyte ratio (NLR), C-reactive protein (CRP), and D-dimer (DD) levels were independent risk factors for severe acute cholangitis. A nomogram model was constructed based on these 4 risk factors. ROC and calibration curves were well differentiated and calibrated. DCA had a high net gain in the range of 7% to 83%. The above model was tested internally. According to the nomogram model when patients using characteristic curve critical values were divided into a low-risk group and a high-risk group, the incidence in the high-risk group was significantly higher than in the low-risk group.
Conclusion: This nomogram model may provide clinicians with an effective tool to predict the potential risk of severe acute cholangitis in patients and guide informed intervention measures and treatment decisions.
Keywords: cholangitis, risk factors, prognosis, nomogram
Introduction
Acute cholangitis is one of the common clinical abdominal conditions, which frequently presents an emergency, due to partial or complete biliary obstruction (by bile duct stones, malignant strictures, etc.), resulting in biliary stasis and biliary tract infection.1–3 The 2018 Tokyo guidelines (TG18) represent the current, globally accepted, criteria for diagnosis of acute cholangitis and for grading its severity. Patients are classified according to their clinical features and laboratory findings, at the time of admission into the hospital, as mild, moderate, and severe (grades I, II, and III) to determine their management.4 Once diagnosed, patients with severe acute cholangitis should be treated immediately with antibiotics and biliary drainage (Endoscopic retrograde cholangiopancreatography, ERCP). Several studies,5,6 have demonstrated that 30-day mortality is significantly higher in patients with severe acute cholangitis compared with mild to moderate disease, but mortality can be significantly reduced in patients with severe acute cholangitis who receive early ERCP drainage.7–9 Therefore, accurate assessment and prediction of the risk of severe acute cholangitis occurrence are crucial for early intervention and effective treatment.
In contemporary clinical practice, there is a discernible limitation in the TG18 guidelines pertaining to the expeditious delineation of acute cholangitis of severe nature, particularly during emergent circumstances. It has been observed that these guidelines are not optimal in terms of convenience.10 Furthermore, existing nomogram-based risk assessment methodologies predominantly rely on clinical indices and radiological examinations. However, these methodologies often fail to encompass the intricate interrelations among various factors and are generally constrained to evaluations based on singular parameters.11–15 Consequently, there is an exigency for a more accurate and comprehensive predictive model to assess the risks associated with the manifestation of severe acute cholangitis.
This study, employing the Nomogram model, aims to develop a predictive model for assessing the risk of severe acute cholangitis. The proposed model not only emphasizes clinical convenience and practicality but also integrates multiple clinical indicators and biomarker variables to enhance the accuracy and reliability of risk assessment. By employing this model, our objective is to provide clinicians with an effective tool for predicting the potential risk of severe acute cholangitis in patients, thereby guiding appropriate intervention strategies and treatment decisions.
Clinical Data and Methods
Study Population and Data Collection
This was a single-center, retrospective, study conducted at a tertiary referral hospital, and data were collected from 152 patients with acute cholangitis who attended the People’s Hospital of Jiangsu University between January 2019 and March 2022. This study was approved by the Ethics Committee of the Affiliated People’s Hospital of Jiangsu University (K-20230037-W), and the requirement for written informed consent was waived due to the retrospective nature of the study. The inclusion criteria included: patients diagnosed with acute biliary cholangitis according to TG18, and patients who were admitted to the hospital for the first time. The exclusion criteria included: 17 cases who were repeatedly admitted for acute biliary cholangitis; 10 cases with recent infections in the pulmonary or urinary tract; 1 case receiving warfarin anticoagulation; and 5 cases with incomplete clinical data. Based on the TG18 classification, all patients with acute cholangitis were stratified into mild-to-moderate (101 cases) and severe (51 cases) groups (Figure 1). All data for this study were from the hospital electronic medical record system collected within 24 hours of patient admission. This included information on age, gender, smoking status, body mass index (BMI), concomitant diseases (hypertension, diabetes, heart disease) obtained from the history taking, temperature taken by the nurse on admission, and routine blood results were obtained from the laboratory; including white blood cell count (WBC), NLR, CRP, and coagulation studies DD, (using the Hysenmachem fully automated hematology analyzer), and biochemical results including TR, total bilirubin (TBil), albumin (using the Beckman Coulter AU biochemical analyzer). Information related to whether the patient died within 30 days of admission was also collected.
 |
Figure 1 Patient Screening and Grouping Flowchart. |
Statistical Methods
SPSS25.0 was used for data analysis. For one-way analysis of variance, the expression of the number of cases (as a percentage) was selected for the count data, and the χ2 test was used. For data, which conformed to a normal distribution, they were expressed as mean ± standard deviation (SD) and the independent sample t-test was used. Data which were not normally distributed were expressed as median (lower–upper quartile), and the nonparametric test for two independent samples (Mann–Whitney U rank sum test) was used. Variables with a significance level of p < 0.05 were selected through the aforementioned tests. Following the assessment of independence using the Spearman correlation test, a backward stepwise binary logistic regression was employed to identify the risk factors associated with severe acute cholangitis. Statistical significance was defined as p < 0.05. Subsequent to the determination of the beta coefficients for the respective variables encompassing multiple factors, a nomogram was employed to substantiate the predictive model. The diagnostic performance of the model was evaluated utilizing ROC curves and an analysis of the area under the curve (AUC). Calibration curves were generated to assess the calibration attributes of the nomogram model. Additionally, DCA was conducted to compute the net benefits of employing this model at varying threshold probabilities.16,17 All curves were plotted using R software (version: 4.2.1).
Results
Etiological Investigation of Acute Cholangitis
Within the aggregate study cohort, an exploration pertaining to the etiology of acute cholangitis was undertaken (Table 1). Of the entire 152 instances assessed, choledocholithiasis was observed in 131 cases, constituting 86.1% of the cases, while benign or malignant strictures in the bile or hepatic ducts accounted for 19 cases, which is equivalent to 12.5%. Additionally, a solitary case, representing 0.7%, was attributed to pancreatic cancer, and a corresponding proportion was ascribed to a stricture in bilioenteric anastomosis. Delving into the subgroup of mild-to-moderate cholangitis, choledocholithiasis emerged as the preeminent etiology, encompassing 89 cases or 88.1%, followed by benign or malignant strictures in the bile or hepatic ducts, tallying 10 cases or 9.9%. In the cohort ascribed to severe cholangitis, choledocholithiasis persevered as the predominant etiology, representing 42 cases or 82.4%, whilst a more substantial fraction concerning benign or malignant strictures of the bile/hepatic ducts, totaling 9 cases, was recorded, accounting for 17.6%.
 |
Table 1 Etiological Investigation of Acute Cholangitis |
Comparison of Mortality in the Mild to Moderate Group and the Severe Group Based on TG18 Severity Grading
According to the TG18 diagnostic criteria, 152 patients with acute cholangitis included in the study were divided into 101 patients in the mild to moderate group and 51 patients in the severe group. The number of deaths in the mild to moderate group was 1, (giving a rate of 0.99%), while the number of deaths in the severe group was 5 (9.80%); the difference was statistically significant (p < 0.01) (Table 2). The severe acute cholangitis patients had a significantly higher mortality rate than patients with mild to moderate acute cholangitis.
 |
Table 2 30-Day Mortality in Severe Acute Cholangitis versus Mild to Moderate Acute Cholangitis |
Baseline Characteristics and Univariate Analysis of Severe Acute Cholangitis Patients
According to the published literature,2,18 age > 70 years is a risk factor for severe acute cholangitis, and 70 years was therefore used as the age cut off for dichotomization in this study. The demographic characteristics and laboratory data of severe acute cholangitis and mild to moderate acute cholangitis patients are shown in Table 3. The risk of developing severe acute cholangitis was positively associated with age, CRP, NLR, DD and TR (all p < 0.05) but not with gender, smoking status, comorbidities (diabetes, hypertension, heart disease), BMI, TBil, albumin, WBC, or body temperature (p > 0.05).
 |
Table 3 Univariate Analysis of the Risk of Developing Severe Acute Biliary Cholangitis |
Correlations Between Risk Factors
The risk factors, screened by univariate analysis, were tested for covariance. Since age was a general characteristic and the remaining four indicators were laboratory data, age was considered relatively independent. From Table 3, it can be seen that the remaining four numerical variables did not obey a normal distribution. Therefore, Spearman correlation analysis was chosen for the examination of covariance between risk factors. In each case for the correlation between TR and CRP, TR and DD, and TR and NLR p > 0.05 indicating that there was no linear correlation between these groups of variables. Furthermore, although there were significant correlations between CRP and NLR (p < 0.01), CRP and DD (p < 0.01), NLR and DD (p < 0.01), with correlation coefficients of 0.343, 0.518, and 0.509, respectively; the correlations were weak (Figure 2). Therefore, the risk factors screened by univariate analysis can be considered independent of each other.
Multivariate Analysis of Risk Factors for Developing Severe Acute Cholangitis
These risk factors: age, CRP, NLR, DD and TR were included in the multivariate analysis, with the results shown in Figure 3. NLR, DD, CRP, and TR were risk factors for severe acute cholangitis.
Establishment and Evaluation of a Nomogram Risk Model for Predicting Severe Acute Cholangitis
Construction of the Nomogram Model
Based on the independent risk factors examined by multivariate analysis, four indicators, TR, CRP, NLR, and DD, were included in the construction of the nomogram risk model for severe acute cholangitis (Figure 4). Each variable was identified as a point on the line segment to obtain the corresponding score, and the sum of the scores of all variables was the total score. The corresponding predicted probability of severe acute cholangitis was based on the total score.
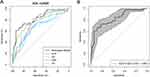
Evaluation of the Nomogram Model by ROC Curves
The ROC curves of the nomogram model and the independent predictors were plotted separately, and the area under the ROC curve (AUC) was used to test discrimination of the predictive efficacy for severe acute cholangitis (Figure 5A). The nomogram model predicted the probability of severe acute cholangitis at 0.48 with an AUC of 0.82, when the specificity was 0.94 and the sensitivity was 0.61; a critical value of TR of 0.93 was associated with an AUC of 0.69, when the specificity was 0.7 and the sensitivity was 0.65; a cut off value of CRP of 45 gave an AUC of 0.67, with a specificity of 0.75 and sensitivity of 0.58; a cut off value of DD of 2.53 gave an AUC of 0.76, with a specificity of 0.75 and a sensitivity of 0.71; NLR at a threshold value of 13.2 gave an AUC of 0.74, a specificity of 0.62 and a sensitivity of 0.82; thus, the nomogram model had a higher AUC in predicting severe acute cholangitis, and outperformed the predictive ability of each independent predictor. Internal validation of the nomogram model using Bootstrap resampling 1000 times gave an AUC of 0.82 (95% CI: 0.75 to 0.89) (Figure 5B).
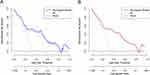
Evaluation of the Nomogram Model by Calibration Curves
The calibration curve is a plot established by the actual probability of occurrence relative to the predicted probability of occurrence; the closer the curve is to ideal line, the more reliable the nomogram model. We used the calibration curve to further evaluate the constructed model. The calibration curve Brier value for this nomogram was 0.152, and the Hosmer-Lemeshow goodness-of-fit test p = 0.545, representing essentially close predicted and actual incidence rates (Figure 6A). In addition, the calibration curve after internal validation of the model, using Bootstrap resampling 1000 times, for this dataset (Figure 6B) showed good agreement with the calibration curve of the nomogram model, demonstrating good performance and repeatability.
DCA Was Conducted Utilizing the Nomogram Model to Assess the Clinical Utility
DCA were plotted based on the nomogram model (Figure 7A). In the threshold range of 7%–83%, the decision curve lies above the None and the All lines. The internal validation of the nomogram model, using the Bootstrap resampling method, validated the high net benefit in the threshold probability range of 4%–83% (Figure 7B), demonstrating clinical utility of the model.
Risk Stratification Based on the Nomogram Model
Risk stratification of all patients with acute cholangitis included in the study was performed according to the threshold value of the optimal ROC curve for the nomogram model. The total points score corresponding to the threshold value of the ROC curve was 62, and therefore we set 62 as the threshold: individuals with a total score of less than 62 were classified as low-risk group, while those with a total score greater than 62 were considered high-risk group. The incidence of severe acute cholangitis was significantly higher in the high-risk group than in the low-risk group (Table 4).
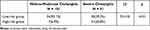 |
Table 4 The Incidence of Severe Acute Cholangitis in Low-Risk and High-Risk Group |
Discussion
In this retrospective study, we collected data on 152 patients admitted to hospital with acute cholangitis. The 30-day mortality rates of patients with severe acute cholangitis were 9.8% compared to 0.99% in patients with mild to moderate acute cholangitis, with a p value < 0.05, indicating a statistically significant difference in mortality rates, consistent with the results of several previous retrospective studies.5,6 It follows, that it is clinically important to identify independent risk factors for severe acute cholangitis for its early recognition. Univariate and multivariate analysis of patient data revealed that four indicators, TR, CRP, DD, and NLR, were independent risk factors for severe acute cholangitis, while age, gender, smoking status, comorbidities (diabetes, hypertension, heart disease), BMI, TBil, albumin, WBC, and body temperature were not.
Aspartate transaminase (AST) and alanine transaminase (ALT) are found mainly in hepatocytes. When the bile duct is obstructed for any reason, biliary pressure is increased and subsequent damage to hepatocytes releases AST and ALT resulting in elevated AST and ALT levels in the blood.19 However, the changes in AST and ALT levels in different conditions are lacking in published studies. Previous authors have concentrated on associating changes in TR levels with chronic liver fibrosis, to good effect.20,21 The relationship between changes in TR and acute cholangitis has not been much reported. In this study, we correlated TR levels with grades of acute cholangitis and used TR to predict the risk of severe acute cholangitis. We found that the higher the TR, the higher the risk of severe acute cholangitis. We speculate that in severe acute cholangitis, more AST is released into the blood due to the destruction of hepatocyte mitochondria while in mild to moderate acute cholangitis, the increase of AST is less marked due to less liver damage.
CRP is a well-recognized acute-phase reactive protein. CRP levels in human serum are generally very low, but in an acute inflammatory setting, CRP levels begin to rise within hours and can increase up to 10,000-fold within 24–72 hours. CRP concentrations directly reflect the severity of underlying inflammatory processes and tissue damage.22,23 Several studies have reported CRP concentrations to be valuable in predicting severe acute cholangitis; furthermore, the occurrence of severe acute cholangitis was positively correlated with CRP concentration.15,24 Our results were consistent with this, as CRP levels were significantly higher in severe compared with mild to moderate acute cholangitis. We found that the threshold value of CRP in predicting severe acute cholangitis was 45 mg/L, with a specificity of 75% and a sensitivity of 58%.
DD is a secondary fibrin degradation product and a biological marker of the activation of the coagulation and fibrinolytic systems in the blood. Due to its molecular stability and easy accessibility, it is now widely used to exclude venous thromboembolism.25,26 Additionally, DD is a marker of the inflammatory response.27,28 In severe acute pancreatitis, patients were found to have more severe coagulation disorders and higher plasma levels of DD compared to those with non-severe acute pancreatitis.29 However, the association between severe acute cholangitis and DD levels is not currently established, and there are few published literature reports. In the present study, plasma DD levels were positively associated with disease severity in patients with an initial presentation of acute cholangitis. We hypothesized that acute cholangitis causing tissue damage, in turn, leads to an increased risk of thrombosis, causing local ischemia and further exacerbating tissue damage.
Zahorec et al30 reported a significant increase in neutrophil counts and a significant decrease in lymphocyte counts in patients with severe sepsis, which led to the proposal of NLR as a new marker of infection. Subsequent studies31,32 have confirmed a correlation between neutrophil-lymphocyte stress factor and the severity of disease. Currently, NLR has been progressively introduced into various fields of research, particularly in infectious diseases. In biliary tract infections, the level of NLR has been suggested12,33 to be higher in severe than in mild to moderate acute cholangitis. Our results are in agreement in demonstrating that NLR is an independent risk factor for severe acute cholangitis and may be a convenient alternative laboratory marker for predicting severe acute cholangitis. We found that NLR >13.2 has 62% specificity and 82% sensitivity for the diagnosis of severe acute cholangitis.
In the annals of prior scholarly endeavors, an assortment of predictive models has been posited for forecasting the incidence of severe acute cholangitis, leveraging a heterogeneous spectrum of prognostic elements encompassing non-alcoholic fatty liver disease, procalcitonin, Lipocalin-2, IL-7, NLR, among others. Specifically, Mahmud et al13 explicated the sovereign risk attribute of non-alcoholic fatty liver disease in severe acute cholangitis through an exhaustive exploration enveloping 298 instances. Additionally, Umefune et al15 meticulously examined a dataset comprising 213 patients diagnosed with acute cholangitis, of which 29 were demarcated as severe, ultimately inferring that procalcitonin manifests adeptness in prognosticating severe acute cholangitis with a notable AUC of 0.9 and an optimal threshold of 2.2 ng/mL (concomitant with a sensitivity of 0.97 and a specificity of 0.73). In addition, an ancillary retrospective analysis expounded upon the efficacy of serum Lipocalin-2 as a judicious biomarker for risk categorization in acute cholangitis patients, outstripping traditional inflammatory indices in discriminative prowess.11 Additionally, the inquiry conducted by Suwa et al accentuated the nexus between attenuated concentrations of IL-7 and the severity of acute cholangitis.14 Notwithstanding, the diagnostic processes for non-alcoholic fatty liver disease and the quantification of procalcitonin and Lipocalin-2 are frequently encumbered by constraints pertaining to hospital instrumentation, which precludes a plethora of medical establishments from executing such appraisals and evaluations. Moreover, the predictive precision of models that are anchored solely upon discrete parameters, such as IL-7 and NLR, remains circumscribed. This engenders a pressing requisition for an economically viable and ubiquitously implementable criterion, ingrained within the fabric of standard clinical practice, to facilitate highly perspicacious forecasts of acute cholangitis severity.
In this study, the efficacy of four independent risk factors (TR, CRP, DD, and NLR) alone for the diagnosis of severe acute cholangitis was determined to be 69%, 67%, 76%, and 74%, respectively. The nomogram model, which incorporates these four clinical indicators, demonstrates a robust discriminative capacity. Both the calibration curve and clinical decision curve exhibit excellent calibration performance of the model and provide valuable clinical recommendations in practical settings. Additionally, risk stratification was performed based on the optimal cutoff value of the ROC curve, enabling individualized risk assessment of patients. The high-risk group showed a significantly higher likelihood of severe acute cholangitis occurrence compared to the low-risk group. In future clinical practice, the established nomogram model can be employed to assign scores to patients. A score exceeding 62 indicates a highly probable diagnosis of severe acute cholangitis. It is crucial to enhance patient management and promptly initiate biliary decompression, particularly in cases where biliary drainage is not feasible in primary healthcare institutions. Timely identification and expedited referral of patients to tertiary hospitals are essential to prevent disease progression and improve patient prognosis.34
The conventional TG18 diagnostic criteria,4 owing to their incorporation of a comprehensive array of intricate standards and indicators, necessitate the comprehensive consideration of diverse facets, encompassing a patient’s clinical presentation, laboratory examination findings, and radiological manifestations. This presents a formidable challenge for medical practitioners and healthcare personnel, demanding heightened time and exertion to appraise and establish a definitive diagnosis. Consequently, applying these criteria for diagnosing severe acute cholangitis in emergency situations is inconvenient.10 Furthermore, the TG18 criteria are population-based and do not provide personalized risk assessment. Each patient’s condition and characteristics may vary, rendering a unified set of standards inadequate for accurately assessing the severity of their individual cases. In light of these limitations, we have developed a nomogram risk model that enables personalized assessment and scoring for each patient, predicting the likelihood of severe acute cholangitis in a visualized manner, thereby facilitating the comprehension and interpretation of risk assessment outcomes by physicians and patients. This intuitive presentation method contributes to effective communication between physicians and patients, fostering the collaborative development of individualized treatment and management plans.
Machine Learning (ML) is an emergent domain in medicine, wherein an amalgamation of computational sciences and statistics is applied to address medical quandaries.35 It harnesses the prowess of classification techniques to enhance the predictive capabilities by categorizing data into predefined classes.36 Relative to traditional binary logistic regression models, ML models may exhibit superior predictive performance under certain circumstances, especially in scenarios involving voluminous data sets and intricate problems. The present study is characterized as a single-center retrospective investigation with a relatively limited sample size. The employment of ML for model construction in this context may be susceptible to overfitting or underfitting, which signifies an avenue for future refinement and augmentation in subsequent research endeavors.
Conclusion
In summary, our study has yielded a highly accurate predictive model harnessing laboratory indicators. This model presents clinicians with a robust instrument to evaluate the prospective jeopardy of severe acute cholangitis in patients, thus facilitating informed interventions and treatment determinations. Notably, its implementation substantially advances patient prognostication while concurrently mitigating mortality rates associated with severe acute cholangitis.
Abbreviations
ALT, alanine transaminase; AST, aspartate transaminase; AUC, area under the curve; BMI, body mass index; CI, confidence interval; CRP, c-reactive protein; DCA, decision curve analysis;DD, d-dimer; ERCP, endoscopic retrograde cholangiopancreatography;ML, machine Learning; NLR, neutrophil-lymphocyte ratio; ROC, receiver operating characteristic; SD, standard deviation; TBil, total bilirubin; TG18, 2018 Tokyo guidelines;TR, aspartate to alanine transaminase ratio or transaminase ratio; WBC, white blood cell.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon request.
Ethical Approval
This study was approved by the Ethics Committee of the Affiliated People’s Hospital of Jiangsu University (K-20230037-W). Due to its retrospective nature, the requirement for written informed consent was waived. Nonetheless, we strictly adhere to the principles of patient data confidentiality and the Declaration of Helsinki.
Acknowledgments
The authors would like to express their gratitude to EditSprings (https://www.editsprings.cn) for the expert linguistic services provided. First author: Jian Xu.
Funding
This research was supported by the “Jinshan Talent” High-level Leading Talent Training Program in Zhenjiang (2021-169XX-22).
Disclosure
The authors declare that they have no competing interests.
References
1. Kiriyama S, Takada T, Hwang TL, et al. Clinical application and verification of the TG13 diagnostic and severity grading criteria for acute cholangitis: an international multicenter observational study. J Hepatobiliary Pancreat Sci. 2017;24(6):329–337. doi:10.1002/jhbp.458
2. Lee JG. Diagnosis and management of acute cholangitis. Nat Rev Gastroenterol Hepatol. 2009;6(9):533–541. doi:10.1038/nrgastro.2009.126
3. Weber A, Schneider J, Wagenpfeil S, et al. Spectrum of pathogens in acute cholangitis in patients with and without biliary endoprosthesis. J Infect. 2013;67(2):111–121. doi:10.1016/j.jinf.2013.04.008
4. Kiriyama S, Kozaka K, Takada T, et al. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25(1):17–30. doi:10.1002/jhbp.512
5. Gomi H, Takada T, Hwang TL, et al. Updated comprehensive epidemiology, microbiology, and outcomes among patients with acute cholangitis. J Hepatobiliary Pancreat Sci. 2017;24(6):310–318. doi:10.1002/jhbp.452
6. Csendes A, Diaz JC, Burdiles P, Maluenda F, Morales E. Risk factors and classification of acute suppurative cholangitis. Br J Surg. 1992;79(7):655–658. doi:10.1002/bjs.1800790720
7. Tan M, Schaffalitzky de Muckadell OB, Laursen SB. Association between early ERCP and mortality in patients with acute cholangitis. Gastrointest Endosc. 2018;87(1):185–192. doi:10.1016/j.gie.2017.04.009
8. Khashab MA, Tariq A, Tariq U, et al. Delayed and unsuccessful endoscopic retrograde cholangiopancreatography are associated with worse outcomes in patients with acute cholangitis. Clin Gastroenterol Hepatol. 2012;10(10):1157–1161. doi:10.1016/j.cgh.2012.03.029
9. Rift CV, Kovacevic B, Toxvaerd A, et al. Response. Gastrointest Endosc. 2020;92(4):983–984. doi:10.1016/j.gie.2020.06.020
10. Kim H, Kong T, Chung SP, et al. Usefulness of the Delta Neutrophil Index as a Promising Prognostic Marker of Acute Cholangitis in Emergency Departments. Shock. 2017;47(3):303–312. doi:10.1097/SHK.0000000000000722
11. Deng X, Wang JW, Wu Q, Pan L, Mou T, Du CY. Lipocalin2 as a useful biomarker for risk stratification in patients with acute cholangitis: a single-center prospective and observational study. Clin Chim Acta. 2022;533:22–30. doi:10.1016/j.cca.2022.05.022
12. Lee SH, Lee TY, Jeong JH, Cheon YK. Clinical Significance of the Neutrophil-Lymphocyte Ratio as an Early Predictive Marker for Adverse Outcomes in Patients with Acute Cholangitis. Medicina. 2022;58(2):56. doi:10.3390/medicina58020255
13. Mahamid M, Fteiha B, Goldin E, Nseir W. Nonalcoholic Fatty Liver Disease as a Risk Factor for Severe Cholangitis. Isr Med Assoc J. 2023;25(3):191–195.
14. Suwa Y, Matsuyama R, Goto K, et al. IL-7 and procalcitonin are useful biomarkers in the comprehensive evaluation of the severity of acute cholangitis. J Hepatobiliary Pancreat Sci. 2017;24(2):81–88. doi:10.1002/jhbp.420
15. Umefune G, Kogure H, Hamada T, et al. Procalcitonin is a useful biomarker to predict severe acute cholangitis: a single-center prospective study. J Gastroenterol. 2017;52(6):734–745. doi:10.1007/s00535-016-1278-x
16. Zhang X, Wang J, Wu B, et al. A nomogram-based model and ultrasonic radiomic features for gallbladder polyp classification. J Gastroenterol Hepatol. 2022;37(7):1380–1388. doi:10.1111/jgh.15841
17. Zhang X, Wang J, Wu B, et al. A Nomogram-based Model to Predict Neoplastic Risk for Patients with Gallbladder Polyps. J Clin Transl Hepatol. 2022;10(2):263–272. doi:10.14218/JCTH.2021.00078
18. Yeom DH, Oh HJ, Son YW, Kim TH. What are the risk factors for acute suppurative cholangitis caused by common bile duct stones? Gut Liver. 2010;4(3):363–367. doi:10.5009/gnl.2010.4.3.363
19. Zhou J, He Z, Ma S, Liu R. AST/ALT ratio as a significant predictor of the incidence risk of prostate cancer. Cancer Med. 2020;9(15):5672–5677. doi:10.1002/cam4.3086
20. Giannini E, Botta F, Testa E, et al. The 1-year and 3-month prognostic utility of the AST/ALT ratio and model for end-stage liver disease score in patients with viral liver cirrhosis. Am J Gastroenterol. 2002;97(11):2855–2860. doi:10.1111/j.1572-0241.2002.07053.x
21. Angulo P, Hui JM, Marchesini G, et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology. 2007;45(4):846–854. doi:10.1002/hep.21496
22. Lobo SM. Sequential C-reactive protein measurements in patients with serious infections: does it help? Crit Care. 2012;16(3):130. doi:10.1186/CC11347
23. Zeller J, Bogner B, McFadyen JD, et al. Transitional changes in the structure of C-reactive protein create highly pro-inflammatory molecules: therapeutic implications for cardiovascular diseases. Pharmacol Ther. 2022;235:108165. doi:10.1016/j.pharmthera.2022.108165
24. Qin Y-S, Q-Y L, Yang F-C, Zheng -S-S. Risk factors and incidence of acute pyogenic cholangitis. Hepatobiliary Pancreat Dis Int. 2012;11(6):650–654. doi:10.1016/s1499-3872(12)60240-9
25. Johnson ED, Schell JC, Rodgers GM. The D-dimer assay. Am J Hematol. 2019;94(7):833–839. doi:10.1002/ajh.25482
26. Health Investigators. Total Hip Arthroplasty or Hemiarthroplasty for Hip Fracture. N Engl J Med. 2020;382(11):1072–1074. doi:10.1056/NEJMc2000062
27. Semeraro F, Ammollo CT, Caironi P, et al. D-dimer corrected for thrombin and plasmin generation is a strong predictor of mortality in patients with sepsis. Blood Transfusion. 2020;18(4):304–311. doi:10.2450/2019.0175-19
28. Franchi L, Patrelli TS, Berretta R, et al. Role of D-dimer testing in severe pelvic inflammatory disease: a new usable marker to assess the need for fertility-impairing surgery? Fertil Steril. 2010;94(6):2372–2375. doi:10.1016/j.fertnstert.2010.03.080
29. Ke L, Ni HB, Tong ZH, Li WQ, Li N, Li JS. D-dimer as a marker of severity in patients with severe acute pancreatitis. J Hepatobiliary Pancreat Sci. 2012;19(3):259–265. doi:10.1007/s00534-011-0414-5
30. Zahorec R. Ratio of neutrophil to lymphocyte counts--rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy. 2001;102(1):456.
31. Liu Z, Li Y, Wang Y, Zhang H, Lian Y, Cheng X. The Neutrophil-to-Lymphocyte and Monocyte-to-Lymphocyte Ratios Are Independently Associated With the Severity of Autoimmune Encephalitis. Front Immunol. 2022;13:911779. doi:10.3389/fimmu.2022.911779
32. Lin H, Bai Z, Wu Q, et al. Inflammatory Indexes for Assessing the Severity and Disease Progression of Ulcerative Colitis: a Single-Center Retrospective Study. Frontiers Public Health. 2022;10:851295. doi:10.3389/fpubh.2022.851295
33. Beliaev AM, Booth M, Rowbotham D, Bergin C. Diagnostic inflammatory markers in acute cholangitis. J Surg Res. 2018;228:35–41. doi:10.1016/j.jss.2018.02.048
34. Buxbaum JL, Buitrago C, Lee A, et al. ASGE guideline on the management of cholangitis. Gastrointest Endosc. 2021;94(2):34.
35. Handelman GS, Kok HK, Chandra RV, Razavi AH, Lee MJ, Asadi H. eDoctor: machine learning and the future of medicine. J Intern Med. 2018;284(6):603–619. doi:10.1111/joim.12822
36. Al-Mallah MH, Ahmed A, Qureshi W, et al. Using Machine Learning to Define the Association between Cardiorespiratory Fitness and All-Cause Mortality: the Fit (Henry Ford Exercise Testing) Project. J Am Coll Cardiol. 2017;69(11). doi:10.1016/s0735-1097(17)35001-5
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.