Back to Journals » OncoTargets and Therapy » Volume 11
A new apatinib microcrystal formulation enhances the effect of radiofrequency ablation treatment on hepatocellular carcinoma
Authors Xie H , Tian S , Yu H , Yang X, Liu J, Wang H, Feng F , Guo Z
Received 8 February 2018
Accepted for publication 20 March 2018
Published 31 May 2018 Volume 2018:11 Pages 3257—3265
DOI https://doi.org/10.2147/OTT.S165000
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr William C. Cho

Hui Xie,1,2 Shengtao Tian,2 Haipeng Yu,1 Xueling Yang,1 Jia Liu,3 Huaming Wang,2 Fan Feng,2 Zhi Guo1
1Department of Interventional Therapy, Tianjin Medical University Cancer Institute and Hospital, National Clinical Research Center for Cancer, Key Laboratory of Cancer Prevention and Therapy, Tianjin’s Clinical Research Center for Cancer, Tianjin, People’s Republic of China; 2Department of Interventional Therapy, 302nd Hospital of People’s Liberation Army, Beijing, People’s Republic of China; 3Department of Blood Transfusion, 302nd Hospital of People’s Liberation Army, Beijing, People’s Republic of China
Introduction: Radiofrequency ablation (RFA) is the foremost treatment option for advanced hepatocellular carcinoma (HCC), however, rapid and aggressive recurrence of HCC often occurs after RFA due to epithelial–mesenchymal transition process. Although combination of RFA with sorafenib, a molecular targeted agent, could attenuate the recurrence of HCC, application of this molecular targeted agent poses a heavy medical burden and oral administration of sorafenib also brings severe side effects.
Materials and methods: In this study, we prepared an apatinib microcrystal formulation (Apa-MS) that sustainably releases apatinib, a novel molecular targeted agent, for advanced HCC treatment. We injected apatinib solution or Apa-MS into subcutaneous HCC tumors.
Results: It was found that Apa-MS exhibited slow apatinib release in vivo and in turn inhibited the epithelial–mesenchymal transition of HCC cells for extended time. Moreover, in rodent HCC model, Apa-MS enhanced the antitumor effect of RFA treatment.
Conclusion: Based on these results, we conclude that Apa-MS, a slow releasing system of apatinib, allows apatinib to remain effective in tumor tissues for a long time and could enhance the antitumor effect of RFA on HCC.
Keywords: apatinib microcrystals, radiofrequency ablation, sustained releasing behavior, long-acting efficiency, epithelial–mesenchymal transition, interventional therapy
Introduction
HCC poses a heavy medical burden worldwide, especially in the People’s Republic of China, due to the high infection rate of hepatitis viruses (hepatitis B or C virus).1,2 Patients often suffer from advanced HCC due to lack of early diagnostic techniques.3,4 RFA can selectively destroy HCC tissues, and hence, it is believed to be a suitable treatment option for advanced HCC patients with cirrhosis and compromised liver function.5–7 However, rapid/aggressive recurrence of HCC after RFA treatment is a major drawback of this approach.8,9 It has been reported that the EMT induced by RFA would be a major reason of HCC recurrence post-RFA, and combination of RFA and molecular targeted agent sorafenib could help to inhibit this process.10,11 However, there are some obstacles for sorafenib application: 1) advanced HCC patients often have compromised gastrointestinal digestive function that attenuates the absorption of orally administered sorafenib;12–14 2) oral administration of sorafenib will result in systemic distribution, making local drug concentration insufficient;15 and 3) the high daily dose (over 800 mg) imposes a heavy financial burden.15 Therefore, it is valuable to develop novel and more effective strategies to enhance the antitumor effect of RFA on HCC.
Apatinib is a newly approved molecular targeting drug for the treatment of advanced HCC.16,17 However, apatinib is insoluble in water, and the daily dose of apatinib-mesylate tablets is very high (over 850 mg).18,19 Microcrystallization is a pharmaceutical process that converts drug powder into microcrystals with a diameter of 30–50 μm.20 Microcrystals have been used to improve the absorption of orally administered drugs due to the fact that microcrystals can fully contact and mix with digestive fluid.20 Here, for the first time, we report the preparation of a microcrystal formulation that extends the release time of apatinib in vivo. By preparing Apa-MS and studying its antitumor effect in tumor models, we found apatinib was slowly released from Apa-MS in vivo. This approach could overcome the limitation of solubility of apatinib and condense drug concentration in tumor without affecting the surrounding tissue. We also examined whether single-dose administration of Apa-MS could achieve accurate apatinib delivery and enhance the antitumor effect of RFA on HCC cells. Figure 1 presents the workflow of the study.
Materials and methods
Cell line and agents
MHCC97-H cells (a highly aggressive HCC cell line) was purchased from the Type Culture Collection of the Chinese Academy of Sciences and maintained under conditions described in our previous work.21,22 Apatinib was a gift from Jiangsu Hengrui Medicine Co., Ltd., Lianyungang, People’s Republic of China. Sodium dodecyl sulfate, dimethyl sulfoxide, polyethylene glycol 400 and Tween 80 were purchased from Sigma-Aldrich Corporation, St Louis, MO, USA.
Preparation of apatinib formulations
For preparing Apa-Sol, apatinib was dissolved in DMSO, PEG400 and Tween 80. Then, the solution was carefully and slowly diluted with physiological saline, accompanied by ultrasonic treatment or churning. The ultimate concentrations of DMSO, PEG400 and Tween 80 in solution were 1%, 4% and 4%, respectively, and the concentration of apatinib was almost 1 mg/mL. For preparing apatinib microcrystals,23 1.5 g apatinib was dispersed into 50 mL aqueous solution with 6.25% Tween 80 and mixed by magnetic stirring to obtain a relatively uniform coarse suspension. The microcrystals were prepared using a MiniZeta (NETZSCH Machinery and Instruments Co., Ltd., Burlington, MA, USA) machine equipped with the grinding media of yttrium-stabilized zirconium oxide beads (0.6 mm in diameter). The coarse suspension was transferred to the milling bowl, and the agitator speed was set at 3,000 rpm. The apatinib concentration in Apa-MS was almost 30 mg/mL.
Subcutaneous tumor
All the animal experiments were reviewed and approved by the Institutional Animal Care and Use Committee of the 302nd Hospital of People’s Liberation Army, Beijing, People’s Republic of China. Nude SCID mice aged 4–6 weeks were purchased from Si-Bei-Fu Biotechnology Corporation, Beijing, People’s Republic of China. All animal studies were performed in accordance with the UK Animals (Scientific Procedures) Act 1986 and associated guidelines. To produce a subcutaneous tumor model,24 MHCC97-H cells were injected into nude SCID mice (1 × 106 cells per animal). After 2–3 weeks, the tumoral volume reached almost 1,200 mm3.
Pharmacokinetic experiments of apatinib formulations
For in vitro release experiments, the release behavior of Apa-MS was identified by vortex shock method. Apa-MS was added to 10 mL physiological saline with 0.1% Tween 80 and 0.9% NaCl. At different time points, 1 mL solution was sucked out for analysis, and the volume was made up to 10 mL. The release of apatinib into physiological saline at each time point was identified. For in vivo release experiments, 50 μL Apa-Sol or Apa-MS was intratumorally injected into subcutaneous tumor formed by MHCC97-H cells. At indicated time points, tumor tissues were harvested, and apatinib was extracted using acetonitrile. The amount of apatinib was identified by liquid chromatography–tandem mass spectrometry following the methods described by Allard et al25 and He et al.26
RFA treatment
MHCC97-H cells were injected into nude mice (1 × 106 cells per animal). After 4–6 weeks, the tumoral volume reached almost 1,200 mm3. RFA of the subcutaneous tumors was performed using a thyroid ablation needle (cat. no UniBlate 700-103587 17G; RITA Company, Crystal Lake, IL, USA). The ablation time was 3–5 minutes, and the temperature was 65°C–70°C. After 2–3 weeks of RFA treatment, the tumoral volume was calculated using the following formula: width2 × length/2. Tumors were harvested 16 days after RFA treatment, and their weights were measured.
qPCR experiments
Total RNA of cells or clinical specimens was extracted using a PARIS™ kit (Applied Biosystems; Thermo Fisher Scientific Corporation, Waltham, MA, USA) and reverse transcribed by MultiScribe™ Reverse Transcriptase (Applied Biosystems; Thermo Fisher Scientific Corporation). The qPCR experiments were performed as described previously.27 The level of β-actin mRNA was measured as an internal control. Primers used in qPCR are listed in Table 1.
  | Table 1 Primers used in this work |
Intrahepatic tumor model
To produce an in situ liver tumor model,28,29 HCC cells were separated from subcutaneous tumors formed by MHCC97-H cells and directly inoculated into the right lobe of the liver of mice (1 × 105 cells per animal). After 4–8 weeks, nude mice were injected intravenously with 100 μCi of 18F-FDG, and the animals were examined using a PET/CT scanner (Philips Corp., Amsterdam, the Netherlands). Two-minute CT and 10-minute PET scans were performed 45 minutes after the 18F-FDG injection. A NaI (Tl) well counter (China Atom Corp., Beijing, People’s Republic of China) was used to measure the radioactivity of organs (liver) and blood.29,30 The liver organ photographs were analyzed using ImageJ Software (version 1.51j8; National Institutes of Health, Bethesda, MD, USA). The percentage of red areas indicated the relative HCC amount.29,30
Statistical analysis
All statistical analyses were performed using SPSS 16.0 statistical software (SPSS Inc., Chicago, IL, USA). Statistical significance was analyzed by two-way ANOVA with Bonferroni correction. Differences between groups were examined by paired-sample t-test.
Results
Characterization of Apa-MS
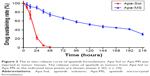
Apa-MS was prepared as described in the Materials and methods section. As shown in Figure 2A, Apa-MS contained irregularly shaped crystals with a particle diameter of 30–50 μm. Apa-MS released apatinib at a slow speed, and almost 60% (40.24%±3.52%) of apatinib remained after 9 days in vitro (Figure 2B). Next, the in vivo release of apatinib was examined. We prepared Apa-Sol as a control. Apa-Sol or Apa-MS was intratumorally injected into subcutaneous MHCC97-H tumors. Tumor tissues were harvested at indicated time points, and apatinib concentration was tested. As shown in Figure 3, following single-dose administration of Apa-Sol, apatinib was completely cleared from tumor tissues at 48 hours, whereas clearance of Apa-MS was much slower: almost 30% (30.2%±2.00%) of Apa-MS remained in tumors at 216 hours (9 days).
Apa-MS enhanced RFA-induced inhibition of the growth of HCC cells in vivo
Apa-Sol or Apa-MS was injected intratumorally into RFA-treated subcutaneous HCC tumor model. As shown in Figure 4, Apa-MS administration reduced the tumor growth and enhanced the effect of RFA treatment. It has been previously reported that RFA induced the EMT of HCC cells by decreasing the expression of E-cadherin and increasing the expression of N-cadherin and vimentin.31 Therefore, we examined the transcriptional level of these proteins in tumor tissues after the subcutaneous HCC tumor growth experiments. As shown in Figure 5, an increase in the mRNA expression of E-cadherin and decrease in the mRNA expression of N-cadherin and vimentin were observed. Apa-MS also attenuated the EMT process of HCC cells induced by RFA at mRNA level. Moreover, the protein levels of E-cadherin, N-cadherin and vimentin were examined (Figure 6). Single-dose administration of Apa-MS was found to inhibit the RFA-induced EMT at protein level (Figure 6). Thus, we found that single-dose administration of Apa-MS inhibited the RFA-induced EMT in HCC.
We also tested the effect of Apa-MS on intrahepatic HCC model, using PET/CT imaging of whole animals and liver organ photographs. As shown in Figure 7A, PET/CT images of whole animals indicated that RFA treatment decreased the intrahepatic growth of HCC cells and Apa-MS enhanced the effect of RFA. Moreover, HCC cells formed multifocal nodules in liver. RFA treatment decreased the nodules formation of HCC cells, and Apa-MS enhanced the antitumor effect of RFA (Figure 7B). Quantitative results including radioactivity ratio of liver to blood (Figure 7C) and relative nodule number (percentage of nodules in liver) (Figure 7D) confirmed the findings of PET images of whole animal (Figure 7A) and liver organ images (Figure 7B). These in vivo data support our hypothesis that Apa-MS enhances the effect of RFA treatment on HCC.
Discussion
Currently, RFA is the prime treatment option for late-stage HCC, particularly for patients with cirrhosis or for those whose liver functional reserve precludes radiotherapy.32 However, HCC can aggressively and rapidly recur after RFA.32 To protect nontumor liver tissue, we cannot indefinitely increase the ablation temperature or power during RFA treatment. On the other hand, RFA may induce cellular stress and pathological changes in HCC cells.33,34 Several studies suggested that the elevated EMT may account for post-RFA recurrence.33–35 Therefore, inhibiting the EMT process during RFA treatment may be a useful strategy to overcome the recurrence of HCC after RFA treatment. Apatinib is a novel and effective molecular targeted agent for advanced HCC treatment; it may enhance the effect of RFA treatment and suppress EMT process.36 However, apatinib is insoluble in water, making treatment combination difficult to be applied. To overcome this obstacle, this work aimed to prepare a novel formulation of apatinib that is easily administrated and has elongated effect. This work, for the first time, established a slow releasing system for apatinib based on its insoluble features. The average size of the apatinib microcrystals in the formulation was 30–50 μm. Apatinib microcrystals could not beidentical; however, in our work, the diameter of the particles was relatively uniform. Due to restrictions in the current pharmaceutical techniques, there were many smaller particles. The size of the particle would affect its release, and hence, it is necessary to prepare apatinib microcrystals with different diameters to reveal the relationship between diameter and release behavior. Moreover, our results showed that Apa-MS extended the releasing duration of apatinib as compared with the control formulation. Single-dose administration of Apa-MS enhanced the effect of RFA and had a long-acting effect of inhibiting the EMT process of HCC cells induced by RFA. Apa-MS had several advantages compared with other formulations: 1) Apa-Sol was cleared from tumor tissues within 48 hours, but Apa-MS remained in the tissues for a longer period; 2) only drugs that are soluble could be loaded into microspheres, and Apa-MS exhibited excellent solubility; 3) microcrystals were more tolerant to high temperatures during RFA compared to gelatin sponge particles or liposomes; and 4) Apa-MS released a very high concentration (30–50 mg/mL) of apatinib and permitted injecting a large amount of drug within a small volume. Thus, this work extended our knowledge on apatinib, and injection of Apa-MS into HCC tissues of patients guided by CT or digital subtraction angiography would be a promising combination strategy to enhance the effect of RFA.37
Conclusion
We conclude that the new apatinib formulation Apa-MS allows single-dose apatinib to be slowly released in tumor tissues for up to 9 days and enhances the antitumor effect of RFA on HCC.
Abbreviations
18F-FDG, 18F-radiolabeled fluorodeoxyglucose; Apa-MS, apatinib microcrystal formulation; Apa-Sol, apatinib solution; CT, computed tomography; EMT, epithelial–mesenchymal transition; HCC, hepatocellular carcinoma; PET, positron emission tomography; qRT-PCR, quantitive real-time polymerase chain reaction; RFA, radiofrequency ablation; SCID, severe combined immune deficiency.
Acknowledgments
This study was supported in part by the National Natural Science Foundation of China (No 81471761 and No 81501568) and Tianjin Program to Support Science and Technology Research (No 15ZCZDSY00890).
Author contributions
All authors made substantial contributions to the design and conception of the study, and acquisition, analysis and interpretation of data, and took part in either drafting or revising the manuscript. All authors gave final approval of the version to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosure
The authors report no conflicts of interest in this work.
References
Wang FS, Fan JG, Zhang Z, Gao B, Wang HY. The global burden of liver disease: the major impact of China. Hepatology. 2014;60(6):2099–2108. | ||
Bruix J, Qin S, Merle P, et al; RESORCE Investigators. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;389(10064):56–66. | ||
Liu ZC, Ning F, Wang HF, et al. Epidermal growth factor and tumor necrosis factor α cooperatively promote the motility of hepatocellular carcinoma cell lines via synergistic induction of fibronectin by NF-κB/p65. Biochim Biophys Acta. 2017;1861(11 Pt A):2568–2582. | ||
Jia H, Yang Q, Wang T, et al. Rhamnetin induces sensitization of hepatocellular carcinoma cells to a small molecular kinase inhibitor or chemotherapeutic agents. Biochim Biophys Acta. 2016;1860(7):1417–1430. | ||
Lee MW, Raman SS, Asvadi NH, et al. Radiofrequency ablation of hepatocellular carcinoma as bridge therapy to liver transplantation: a 10-year intention-to-treat analysis. Hepatology. 2017;65(6):1979–1990. | ||
Wang C, Wang H, Yang W, et al. Multicenter randomized controlled trial of percutaneous cryoablation versus radiofrequency ablation in hepatocellular carcinoma. Hepatology. 2015;61(5):1579–1590. | ||
Xie H, Yu H, Tian S, et al. What is the best combination treatment with transarterial chemoembolization of unresectable hepatocellular carcinoma? A systematic review and network meta-analysis. Oncotarget. 2017;8(59):100508–100523. | ||
Ikemoto T, Shimada M, Yamada S. Pathophysiology of recurrent hepatocellular carcinoma after radiofrequency ablation. Hepatol Res. 2017;47(1):23–30. | ||
Iwahashi S, Shimada M, Utsunomiya T, et al. Epithelial-mesenchymal transition-related genes are linked to aggressive local recurrence of hepatocellular carcinoma after radiofrequency ablation. Cancer Lett. 2016;375(1):47–50. | ||
Tang Z, Kang M, Zhang B, et al. Advantage of sorafenib combined with radiofrequency ablation for treatment of hepatocellular carcinoma. Tumori. 2017;103(3):286–291. | ||
Dong S, Kong J, Kong F, et al. Sorafenib suppresses the epithelial-mesenchymal transition of hepatocellular carcinoma cells after insufficient radiofrequency ablation. BMC Cancer. 2015;15:939. | ||
Roskoski R Jr. The role of small molecule platelet-derived growth factor receptor (PDGFR) inhibitors in the treatment of neoplastic disorders. Pharmacol Res. 2018;129:65–83. | ||
Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391(10127):1301–1314. | ||
Kim HA, Kim KA, Choi JI, et al. Comparison of biannual ultrasonography and annual non-contrast liver magnetic resonance imaging as surveillance tools for hepatocellular carcinoma in patients with liver cirrhosis (MAGNUS-HCC): a study protocol. BMC Cancer. 2017;17(1):877. | ||
Rimola J, Díaz-González Á, Darnell A, et al. Complete response under sorafenib in patients with hepatocellular carcinoma: relationship with dermatologic adverse events. Hepatology. Epub 2017 Sep 12. | ||
Kong Y, Sun L, Hou Z, et al. Apatinib is effective for treatment of advanced hepatocellular carcinoma. Oncotarget. 2017;8(62):105596–105605. | ||
Kou P, Zhang Y, Shao W, et al. Significant efficacy and well safety of apatinib in an advanced liver cancer patient: a case report and literature review. Oncotarget. 2017;8(12):20510–20515. | ||
Lee JE, Kim KL, Kim D, et al. Apatinib-loaded nanoparticles suppress vascular endothelial growth factor-induced angiogenesis and experimental corneal neovascularization. Int J Nanomedicine. 2017;12:4813–4822. | ||
Jeong JH, Nguyen HK, Lee JE, Suh W. Therapeutic effect of apatinib-loaded nanoparticles on diabetes-induced retinal vascular leakage. Int J Nanomedicine. 2016;11:3101–3109. | ||
Barnes CO, Kovaleva EG, Fu X, et al. Assessment of microcrystal quality by transmission electron microscopy for efficient serial femtosecond crystallography. Arch Biochem Biophys. 2016;602:61–68. | ||
Chen Y, Feng F, Gao X, et al. MiRNA153 reduces effects of chemotherapeutic agents or small molecular kinase inhibitor in HCC cells. Curr Cancer Drug Targets. 2015;15(3):176–187. | ||
Hou J, Hong Z, Feng F, et al. A novel chemotherapeutic sensitivity-testing system based on collagen gel droplet embedded 3D-culture methods for hepatocellular carcinoma. BMC Cancer. 2017;17(1):729. | ||
Hu LD, Kong DQ, Hu QF, et al. Preparation, characterization and in vivo evaluation of injectable long-acting curcumin microcrystal. Particul Sci Technol. Epub 2017 Mar 10. | ||
Li L, Kang L, Zhao W, et al. miR-30a-5p suppresses breast tumor growth and metastasis through inhibition of LDHA-mediated Warburg effect. Cancer Lett. 2017;400:89–98. | ||
Allard M, Khoudour N, Rousseau B, et al. Simultaneous analysis of regorafenib and sorafenib and three of their metabolites in human plasma using LC-MS/MS. J Pharm Biomed Anal. 2017;142:42–48. | ||
He Y, Zhou L, Gao S, et al. Development and validation of a sensitive LC-MS/MS method for simultaneous determination of eight tyrosine kinase inhibitors and its application in mice pharmacokinetic studies. J Pharm Biomed Anal. 2017;148:65–72. | ||
Zhao J, Bai Z, Feng F, et al. Cross-talk between EPAS-1/HIF-2α and PXR signaling pathway regulates multi-drug resistance of stomach cancer cell. Int J Biochem Cell Biol. 2016;72:73–88. | ||
Chao TI, Tai WT, Hung MH, et al. A combination of sorafenib and SC-43 is a synergistic SHP-1 agonist duo to advance hepatocellular carcinoma therapy. Cancer Lett. 2016;371(2):205–213. | ||
Xu X, Fan Z, Liang C, et al. A signature motif in LIM proteins mediates binding to checkpoint proteins and increases tumour radiosensitivity. Nat Commun. 2017;8:14059. | ||
Feng F, Jiang Q, Cao S, et al. Pregnane X receptor mediates Sorafenib resistance in advanced hepatocellular carcinoma. Biochim Biophys Acta. 2018;1862(4):1017–1030. | ||
Fei Y, Xiong Y, Shen X, et al. Cathepsin L promotes ionizing radiation-induced U251 glioma cell migration and invasion through regulating the GSK-3β/CUX1 pathway. Cell Signal. 2018;44:62–71. | ||
Lee HW, Park WJ, Heo YR, Park TI, Park SY, Lee JH. TERT-CLPTM1 locus polymorphism (rs401681) is associated with the prognosis of hepatocellular carcinoma. Onco Targets Ther. 2017;10:4853–4858. | ||
Muaddi H, Al-Adra DP, Beecroft R, et al. Liver transplantation is equally effective as a salvage therapy for patients with hepatocellular carcinoma recurrence following radiofrequency ablation or liver resection with curative intent. Ann Surg Oncol. 2018;25(4):991–999. | ||
Tong Y, Yang H, Xu X, et al. Effect of a hypoxic microenvironment after radiofrequency ablation on residual hepatocellular cell migration and invasion. Cancer Sci. 2017;108(4):753–762. | ||
Jiangzheng Z, Cai X, Hao X, et al. LncRNA FUNDC2P4 down-regulation promotes epithelial-mesenchymal transition by reducing E-cadherin expression in residual hepatocellular carcinoma after insufficient radiofrequency ablation. Int J Hyperthermia. 2018:1–10. | ||
Vallese F, Mishra NM, Pagliari M, et al. Helicobacter pylori antigenic Lpp20 is a structural homologue of Tipα and promotes epithelial-mesenchymal transition. Biochim Biophys Acta. 2017;1861(12):3263–3271. | ||
Agiba AM, Nasr M, Abdel-Hamid S, Eldin AB, Geneidi AS. Enhancing the intestinal permeation of the chondroprotective nutraceuticals glucosamine sulphate and chondroitin sulphate using conventional and modified liposomes. Curr Drug Deliv. Epub 2018 Jan 22. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.