Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
A Meta-Analysis on the Efficacy of Acupuncture as an Adjuvant Therapy for Schizophrenia
Authors Huang C , Zhang P , Dong Y, Chang R , Lao J, Li Z, Lan D
Received 27 July 2023
Accepted for publication 20 October 2023
Published 7 November 2023 Volume 2023:19 Pages 2381—2400
DOI https://doi.org/10.2147/NDT.S428518
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yuping Ning
Cheng Huang,1 Peiming Zhang,2 Yu Dong,1 Ruchun Chang,2 Jinxiong Lao,2,3 Ziyong Li,2,3 Danchun Lan2
1Acupuncture and Rehabilitation Clinical School of Medicine, Guangzhou University of Chinese Medicine, Guangzhou, People’s Republic of China; 2Department of Acupuncture and Moxibustion, Foshan Hospital of Traditional Chinese Medicine, Foshan, People’s Republic of China; 3The Eighth Clinical School of Medicine, Guangzhou University of Chinese Medicine, Foshan, People’s Republic of China
Correspondence: Danchun Lan, Email [email protected]
Objective: To systematically evaluate the efficacy of acupuncture in the treatment of schizophrenia.
Methods: We searched China National Knowledge Infrastructure (CNKI), Wanfang Database, Chongqing VIP Chinese Science and Technology Periodical Database (VIP), China Biology Medicine Database (CBM), PubMed, Embase, Web of Science, Cochrane Library for relevant literature on the acupuncture treatment of schizophrenia published from database inception to May 17, 2023. The evaluation criteria included total effective rate, incidence of adverse reactions, TESS scale, PANSS scale, BPRS scale, SANA scale, SAPS scale. Two researchers independently screened the literature, extracted data, and assessed the risk of bias of the included studies. The RevMan 5.4 software was used for meta-analysis, risk of bias (ROB) evaluation tool was used to evaluate the risk of bias of the studies, and the GRADE evaluation tool was used to evaluate the quality of evidence. The study was registered on PROSPERO, CRD42023416438.
Results: A total of 38 RCTs involving 3143 patients were included in the meta-analysis. The results showed that acupuncture can improve the total effective rate [OR=3.43 (95% CI: 2.71, 4.35), moderate credibility], reduce the incidence of adverse reactions [OR=0.45 (95% CI: 0.32, 0.63), moderate credibility], reduce the TESS score (side effect scale) [MD=− 1.83 (95% CI: − 2.94, − 0.71), very low credibility]. Acupuncture also reduced the PANSS total score [MD=− 5.75 (95% CI: − 8.08, − 3.42), very low credibility], SANA score [MD=− 2.66 (95% CI: − 6.84, 1.51), very low credibility], SAPS score [MD=− 1.26 (95% CI: − 2.55, − 0.02), very low credibility], and BPRS score [MD=− 7.02 (95% CI: − 10.59, − 3.46), very low credibility].
Conclusion: Existing evidence indicates that acupuncture as an adjunctive therapy can improve the total effective rate of SZ patients, reduce the incidence of adverse reactions, improve clinical symptoms, and alleviate depression and anxiety in SZ patients. However, more high-quality clinical research evidence is still needed to support these findings.
Keywords: acupuncture, meta-analysis, schizophrenia
Introduction
Schizophrenia (SZ) is a chronic mental illness characterized by changes in personality, cognitive, thinking, emotional, and behavioral disorders, as well as a lack of coordination between mental activity and the environment. Its main clinical manifestations are delusions, hallucinations, disordered thinking (speech), obvious disordered or abnormal movements and behaviors, and other symptoms. It affects approximately 20 million people worldwide,1 and the global prevalence of schizophrenia is estimated to be between 0.33% and 0.75%.1 The disease is more common in young adults or adults.2 At the same time, schizophrenia seriously affects the daily life of patients, and maintaining daily activities is very difficult for schizophrenia patients.
In terms of mechanisms, the etiology of SZ remains elusive to date. Researchers have been searching for biomarkers to aid in the diagnosis and understanding of the pathogenesis of this disease. In recent years, exosomes as a prominent biomarker have garnered widespread attention in this research field. Studies have shown that metabolites derived from exosomes have significant potential to provide diagnostic information for SZ, highlighting the role of exosomal miRNA dysregulation in the pathophysiology of SZ.3
In clinical practice, drug therapy and psychotherapy are the main treatments for SZ, but their adverse reactions are obvious. Studies have found that second-generation or “atypical” antipsychotics (SGA) can lead to weight gain and significant metabolic changes in patients, indirectly increasing their risk of developing diabetes and increasing circulating cholesterol levels.4 In addition, the recurrence rate of this disease is as high as 78–82%.
Acupuncture, as a green therapy, provides another option for SZ without significant side effects. The research findings indicate that acupuncture, by modulating functionally opposing brain networks, enhances the behavior of SZ patients, and this effect is contingent upon psychophysiological responses.5 While the effectiveness of acupuncture in treating SZ has been confirmed by several Cochrane systematic reviews,6,7 there are limitations in the methodological quality of some included studies, leading to a lack of high-quality evidence. Furthermore, the potential impact factors underlying acupuncture’s therapeutic effects in SZ remain a subject of debate. This study aims to bridge these research gaps, offering more systematic evidence and applying meta-regression to investigate potential factors influencing the efficacy of acupuncture in SZ treatment.
Materials and Methods
The study was registered on PROSPERO (CRD42023416438).
Inclusion and Exclusion Criteria
Inclusion Criteria
(1) Randomized controlled trials (RCTs) of acupuncture treatment(Intervention definition can be found in Appendix 1) for schizophrenia were included in this meta-analysis. (2) Patients with a clinical diagnosis of schizophrenia according to diagnostic criteria such as Chinese Classification of Mental Disorders (CCMD-2,8 CCMD-39), International Classification of Diseases (ICD-1010), or Diagnostic and Statistical Manual of Mental Disorders (DSM-V11). (3) The intervention group received acupuncture or acupuncture combined with other therapies, and the control group received other therapies except for acupuncture (when the intervention group received acupuncture combined with other adjunct therapies, the control group should receive the same adjunct therapies). (4) The outcome measures must be one of the following, such as total effective rate, incidence of adverse reactions, score on the Treatment Emergent Symptom Scale (TESS), Positive and Negative Syndrome Scale (PANSS), Brief Psychiatric Rating Scale (BPRS), Scale for the Assessment of Negative Symptoms (SANS), and Scale for the Assessment of Positive Symptoms (SAPS).
Exclusion Criteria
(1) Unclear diagnostic criteria or no diagnostic criteria; (2) Studies that did not include outcome measures; (3) Studies with unextractable data or inaccessible full text; (4) Duplicate publications; (5) Reviews, conference abstracts, before-and-after comparison studies, case reports, cohort studies, and other non-randomized studies.
Search Strategy
We searched the China National Knowledge Infrastructure (CNKI), Wanfang Database, Chongqing VIP Chinese Scientific Journal Full-text Database (VIP), China Biology Medicine disc (CBM), PubMed, Embase, Web of Science, and Cochrane Library for relevant literature on acupuncture treatment for schizophrenia. The search time limit was from the establishment of the databases until May 17, 2023. The search terms used included “acupuncture”, “acup*” “moxibustion”, “electroacupuncture”, “schizophrenia”, “schizo*” “psychos*” and other relevant terms. Language restrictions were not applied. The specific search formula can be found in Appendix 2
Literature Screening and Data Extraction
Firstly, two researchers independently screened the retrieved literature based on the inclusion and exclusion criteria. In case of any disputes, a third reviewer cross-checked the articles to reach a consensus. The two researchers extracted relevant information from the included literature, including study identification (first author and year of publication), general characteristics of patients (gender, age, and sample size), intervention measures, treatment process, and outcome indicators.
Risk of Bias Assessment of Included Studies
The Cochrane risk of bias assessment tool (version 5.4.0) was used to evaluate the risk of bias in the included RCTs. It includes seven items: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases. The risk of bias for each item was classified into three categories: low risk of bias, high risk of bias, or unclear risk of bias. Two reviewers independently assessed the risk of bias of the studies. In case of inconsistent results, a third reviewer made the final decision.
Outcomes and Measures
Primary Outcome
The primary outcome was the total effective rate, which was assessed using the Positive and Negative Syndrome Scale (PANSS), Scale for the Assessment of Positive Symptoms (SAPS), Scale for the Assessment of Negative Symptoms (SANS), Brief Psychiatric Rating Scale (BPRS), Global Assessment of Functioning (GAF), and Pittsburgh Sleep Quality Index (PSQI). In the study, a reduction rate of ≥30% in PANSS score, ≥20% in BPRS score, ≥25% in SAPS excitation score, ≥25% in SANS score, an increase rate of ≥20% in GAF score, and a reduction rate of ≥25% in PSQI score were considered as effective. The evaluation time points included before and after treatment (usually 1–12 weeks).
Secondary Outcomes
The secondary outcome was the PANSS score, which is a scale for evaluating the positive symptoms, negative symptoms, and general psychological symptoms of patients with schizophrenia. The total score ranges from 30 to 210, and includes subscales such as positive symptoms, negative symptoms, and general psychopathology. A threshold of 60 points was used, with higher scores indicating more severe symptoms. The evaluation time points included before and after treatment (usually 1–12 weeks).
BRPS score: The BRPS score was used to evaluate the severity of illness and treatment efficacy in patients with mental illness, with a range of 1–7 points. A score of 1 indicated extremely worsening condition, while a score of 7 indicates complete remission of symptoms. The evaluation time points included before and after treatment (usually 1–12 weeks).
SAPS score: The SAPS score was used to assess the severity and changes in symptoms of mental illness. The scale was consisted of 4 dimensions, including hallucinations, delusions, thought disorders, and affective flattening. The total score ranged from 0–176, with higher scores indicating more severe symptoms. The evaluation time points included before and after treatment (usually 1–12 weeks).
SANS score: The SANS score was used to assess the severity and changes in symptoms of mental illness. The scale was consisted of 5 dimensions, including hallucinations, delusions, thought disorders, affective flattening, and behavioral symptoms, each with multiple scoring indicators. The score range was 0–95, with higher scores indicating more severe symptoms. The evaluation time points included before and after treatment (usually 1–12 weeks).
Effect Size and Heterogeneity Assessment
Meta-analysis was performed using RevMan 5.4 software. With 95% confidence interval (CI), the odds ratio (OR) was used as the effect size (ES) considering the the total effective rate was a dichotomous variable, and the mean difference (MD) was applied for the continuous variables, involving all secondary outcomes.
Effect model: Fixed or random effect models were chosen based on the heterogeneity test results of the studies. Statistical heterogeneity was assessed using I2 statistic, Cochran’s Q test (reporting its between-study variance component τ2 and corresponding P-value based on the significance level α=0.1), and forest plots. If P > 0.1 and I2 ≤ 50%, heterogeneity was considered acceptable, and a fixed effect model was used for the pooled effect size. If P< 0.1 or I2 ≥ 50%, statistical heterogeneity was considered unacceptable When the random effects model still could not explain the heterogeneity well, we attempted to explore the sources of heterogeneity using subgroup analysis, sensitivity analysis, or comparing the specific content of the literature.
Publication Bias
Funnel plots were used to assess potential publication bias when the number of included studies exceeded 10.
Evidence Certainty Assessment
To assess the evidence certainty, we used the GRADEpro online tool (http://gdt.gradepro.org/app#projects) to perform the evaluation and followed the recommended procedures for grading (high, moderate, low, very low).
Results
Literature Search Results
A total of 1761 relevant articles were obtained in the initial screening, and after a series of selection processes, 38 RCTs12–49 were finally included. The flowchart of literature screening process and results are shown in Figure 1.
 |
Figure 1 Flowchart of literature search and selection results. |
Characteristics of Included Studies
A total of 38 randomized controlled trials (RCTs) were included in this review, comprising of 3143 participants. Of these, 1595 were in the treatment group and 1548 were in the control group. The trials were conducted in different countries, including China (37 trials12–48 with 3112 participants) and Tunisia (1 trial49 with 31 participants). 36 studies12–47 were published in Chinese, 148 in English, and 149 in French. Sample sizes ranged from 31 to 200 participants, with treatment durations ranging from 1 to 12 weeks. The age of participants ranged from 18 to 65 years. The main interventions in the treatment group included electroacupuncture, manual acupuncture, and scalp acupuncture. The control group included sham acupuncture, psychological health education, clozapine, quetiapine, risperidone, aripiprazole, dextropropoxyphene tablets, paliperidone, haloperidol, olanzapine, sulpiride, chlorpromazine, team psychological intervention, cognitive behavior therapy, and sertraline hydrochloride tablets. The main outcome measures included the total effective rate, and secondary outcome measures included PANSS score, BRPS score, SAPS score, and SANS score (Table 1).
 |
Table 1 Basic Characteristics of the Included Studies |
Diagnostic Criteria
Among the 38 studies, three34,37,46 did not mention the specific version of the diagnostic criteria, while 35 studies had clear versions of the diagnostic criteria. One study27 used the Chinese Classification of Mental Disorders 2nd edition (CCMD-2), 18 studies12,13,15,16,18,21–26,28–30,36,43,44,47 used CCMD-3, 9 studies14,17,31,33,35,39–42 used the International Classification of Diseases 10th edition (ICD-10), and 7 studies19,20,32,38,45,48,49 used DSM-V.
3.4 Among the 38 studies included in this study, 17 provided sufficient information on randomization and were assessed as having a low risk of selection bias. The randomization methods included random number tables (13),14,17–19,23–25,29,30,32,36,39,42 digit tables (1),40 drawing lots (1),12 random allocation tables (1),26 and computer-generated random number sequences (1).48 One study48 mentioned allocation concealment using sealed opaque envelopes. Two studies48,49 mentioned blinding of patients and evaluators. Regarding completeness, two studies24,29 out of the 38 did not address the handling of missing data, and we did not find any sources of selective reporting or other bias in all included studies (Figure 2A and B).
Meta-Analysis Results
Primary Results
Overall Effectiveness
A total of 27 RCTs12,13,15,17–30,34,36,37,39,42,44–48 with 2367 patients were included. Heterogeneity testing was conducted on the results of the 27 studies. Based on a fixed-effect model, the Meta-analysis showed a statistically significant advantage in total effectiveness of acupuncture compared to the control group (OR=3.43, 95% CI (2.71, 4.35), P<0.00001), with low statistical heterogeneity (Chi2=26.71, df=26, P=0.42>0.1, I2=3%<50%) (Figure 3).
 |
Figure 3 Forest Plot for Overall Response Rate. |
Subgroup Analysis
Different Assessment Measures for Overall Response Rate
PANSS
12 studies12,13,21,22,26,34,36,39,42,45,47,48 utilized the PANSS scale to evaluate the overall response to acupuncture. The analysis revealed that acupuncture had a significantly greater influence on PANSS scores in comparison to the control group [MD=2.77 (95% CI: 1.93, 3.98), P<0.00001, I²=34%]. (Figure 4)
 |
Figure 4 Forest Plot of Total Effective Rate Subgroup Analysis Meta-Regression. |
BPRS
8 studies18,24,25,27,29,30,37,46 used the BPRS scale to assess the overall response rate of acupuncture. The analysis showed that acupuncture had a greater impact on BPRS scores compared to the control group [MD=3.57 (95% CI: 2.32, 5.51), P<0.00001, I²=0%]. (Figure 4)
SAPS
3 studies19,20,44 employed the SAPS scale to evaluate the overall response to acupuncture. The analysis demonstrated that acupuncture had a greater effect on SAPS scores compared to the control group [MD=5.59 (95% CI: 3.05, 10.26), P<0.00001, I²=0%]. (Figure 4)
SANS
2 studies15,23 used the SANS scale to assess the overall response rate to acupuncture. The analysis revealed that acupuncture had a more pronounced effect on SANS scores when compared to the control group [MD=3.05 (95% CI: 1.21, 7.70), P=0.02, I²=0%]. (Figure 4)
One study28 reported the use of GAF to assess the overall response rate (OR: 6.46, 95% CI: 1.18–35.26), and one study17 mentioned the use of PSQI to assess the overall response rate (OR: 2.14, 95% CI: 0.37–12.32).
Subgroup difference test showed no heterogeneity among different comparison groups (P=0.45, I²=0%).
Meta-Regression
In this study, we used meta-regression analysis to explore the relationship between treatment duration and treatment effectiveness. In a meta-analysis that included 27 studies, we found a negative correlation between treatment duration and treatment effectiveness, but this relationship did not reach statistical significance (P = 0.052) (Table 2). Specifically, for every one-day increase in treatment duration, the index level of treatment effectiveness decreased to 0.987. This result was validated in the meta-regression modified by Knapp-Hartung (b = 5.56, 95% CI [3.14, 9.84]) (Table 2). The results indicate that for the treatment of schizophrenia, prolonged treatment may not be beneficial to patients’ recovery, and further optimization of treatment plans is needed. (Figure 5).
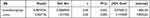 |
Table 2 Regression Table of Total Effective Rate and Treatment Time |
 |
Figure 5 Total response rate and treatment duration regression plot. |
Secondary Outcomes
PANSS has broad applicability and high reliability, which can accurately assess the symptoms of SZ patients. BPRS is a simple and easy-to-use tool that evaluates positive symptoms, negative symptoms, affective symptoms, and cognitive symptoms. SANS and SAPS can accurately evaluate the core symptoms of schizophrenia but may not fully reflect the patient’s comprehensive symptoms.
PANSS
PANSS evaluates the severity and changes of patients’ psychotic symptoms before and after treatment to determine the effectiveness of acupuncture. A total of 21 RCTs12–14,17,22,26,31,33–36,38,40–43,45–49 with 1566 patients were included in the random effects model meta-analysis. The results showed that compared with the control group, acupuncture treatment for schizophrenia patients had a significant treatment advantage, with MD=−5.75 (95% CI: −8.08, −3.42) and Z=4.84 (P<0.00001). The heterogeneity test showed significant heterogeneity among the included studies (I²=88%, P<0.00001), indicating significant differences among the included studies (Figure 6).
 |
Figure 6 Forest plot of PANSS scores. |
BPRS
The Brief Psychiatric Rating Scale (BPRS) is mainly used to assess the psychopathological symptoms of psychiatric patients to observe the effect of acupuncture on psychiatric symptoms. A total of 10 RCTs16,18,23,27,29,32,33,43,46 were included with a total of 698 patients. The random-effects model meta-analysis showed that compared with the control group, acupuncture had a greater impact on BPRS with a MD of −7.02 (95% CI: −10.59, −3.46). The heterogeneity test showed significant heterogeneity among the included studies (I²=94%, P=0.0001) (Figure 7).
 |
Figure 7 Forest plot of BPRS scores. |
SANS
The SANS scale is used to evaluate negative symptoms in patients and assess the effectiveness of acupuncture. A total of 15 RCTs13–17,22,23,31,34,38,42,43,47–49 with 1106 patients were included. The random-effects model meta-analysis showed that the effect of acupuncture on SANS was not greater than that of the control group, with no significant difference [MD=−2.66 (95% CI: −6.84, 1.51), P=0.21, I²=99%] (Figure 8).
 |
Figure 8 Forest Plot of SANS Scores. |
Subgroup Analysis
Different Intervention Measures
Manual Acupuncture Vs Control
7 studies15,17,31,38,42,43,49 conducted a comparison between manual acupuncture and a control group using SANS assessment. The analysis revealed that acupuncture did not have a significantly greater impact on SANS scores when compared to the control group [MD: −0.86 (−8.53, 6.80), P=0.82, I²=99%] (Figure 9).
 |
Figure 9 Forest plot of subgroup analysis for SANS. |
Electroacupuncture VS Control
8 studies13,14,16,22,23,34,47,48 compared the effectiveness of electroacupuncture with a control group using SANS assessment. The analysis showed that acupuncture had a greater impact on SANS scores compared to the control group [MD: −3.52 (−6.22, −0.82), P=0.01, I²=90%] (Figure 9).
After the primary meta-analysis, the result of SANS score showed P=0.21, which is greater than 0.05. However, during the subgroup analysis, we divided acupuncture into two groups: electroacupuncture and manual acupuncture. The result revealed that the electroacupuncture group had a P-value of 0.01, which is less than 0.05. Therefore, we can infer that electroacupuncture treatment may be more effective than manual acupuncture in terms of SANS score.
SAPS
The SAPS scale is used to assess positive symptoms and measure symptom changes in patients, aiming to evaluate the effectiveness of acupuncture. A total of 11 RCTs13,14,16,17,22,31,34,38,42,48,49 with 828 patients were included in the random-effects model Meta-analysis. The results demonstrated that acupuncture had a greater impact on SAPS compared to the control group, and the difference was statistically significant [MD=−1.26 (95% CI: −2.55, −0.02), P=0.05, I²=86%]. Please refer to Figure 10 for details.
 |
Figure 10 Forest plot of SAPS score. |
Sensitivity Analysis
To determine the robustness of the summary data for the main outcome measures, we performed a sensitivity analysis by removing each study one by one. The results of the sensitivity analysis showed no significant changes in the combined results, which supports the statistical advantage of acupuncture in overall efficacy (P < 0.0001).
Adverse Events
A total of 15 RCTs12,13,17,21,22,24,30,33–35,37,42,45–47 were included, including 1344 patients. 1 study35 reported both count data and continuous data. 9 RCTs12,24,30,34,35,37,42,46,47 reported count data and were analyzed using the odds ratio (OR) and its 95% confidence interval (CI). Based on the fixed-effect model, the results of the heterogeneity test of the 9 studies showed statistical advantage of acupuncture over the control group in terms of adverse events (OR=0.55, 95% CI (0.42, 0.71), P<0.00001), with moderate statistical heterogeneity (Chi2=13.01, df=8, P=0.11>0.1, I2=39%) (Figure 11).
 |
Figure 11 Forest plot of adverse events for binary variables. |
7 RCTs13,17,21,22,33,35,45 reported continuous data and were analyzed using the mean difference (MD) and its 95% CI. Based on the random-effects model, the results of the heterogeneity test of the 7 studies showed statistical advantage of acupuncture over the control group in terms of adverse events (MD=−1.82, 95% CI (−2.94, −0.71), P=0.0001), with high statistical heterogeneity (Chi2=50.06, df=6, P<0.00001<0.1, I2=88%) (Figure 12).
 |
Figure 12 Forest plot of adverse events for continuous variables. |
As can be seen, acupuncture as an adjunctive therapy can effectively reduce adverse reactions in clinical practice.
Publication Bias of Included Literature
Funnel plot and Egger’s test were used to evaluate the publication bias of the overall effective rate. The funnel plot and Egger’s test (t=1.00, P=0.329) showed no evidence of publication bias. As shown in Figure 13 and Table 3.
 |
Table 3 Egger’s Test for Publication Bias in Overall Effectiveness |
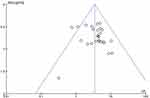 |
Figure 13 The Funnel plot for publication bias of overall effectiveness. |
GRADE Evidence Quality Assessment
For the adverse reaction incidence rate, we divided it into two outcome indicators based on the different types of variables: incidence rate of adverse reactions for binary variables and TESS score for continuous variables. There were a total of 7 outcome indicators, including Effective rate, incidence rate of adverse reactions, PANSS score, BRPS score, SANS score, SAPS score, and TESS score. The results showed that the quality of Total Effective rate and incidence rate of adverse reactions was Moderate, while the quality of PANSS score, BRPS score, SANS score, SAPS score, and TESS score was very low. Details can be found in Table 4.
 |
Table 4 GRADE Evidence Quality Assessment |
Discussion
Overview
This meta-analysis included 38 randomized controlled trials with a total of 3143 patients, comparing the efficacy and safety of acupuncture combined with another therapy versus the use of the therapy alone. The results indicated that acupuncture, as an adjunctive therapy in conjunction with Western medicine or other therapies, could improve the overall effective rate of SZ patients (P<0.00001) while reducing the adverse reactions caused by medication. We conducted subgroup analyses on the overall effective rate, comparing different outcome measures, and the results showed no heterogeneity among the different measures (P=0.45, I²=0%), indicating the stability of acupuncture treatment across various outcome measures and its reliability as a treatment option.
Regarding the mechanism of acupuncture in the treatment of schizophrenia, some studies have suggested50,51 that structural changes occur in the default mode network (DMN) brain regions of schizophrenia patients, and the dysfunction between the frontoparietal control system and the DMN may be one of the causes of schizophrenia. Acupuncture acts by regulating and normalizing the lateral parietal-occipital network (LPNN), including the default mode network (DMN), thereby balancing bodily functions and improving clinical symptoms in Schizophrenia patients5,52
Comparison with Previous Studies
Compared with previous studies, we have also concluded the effectiveness of acupuncture in the treatment of schizophrenia. In a meta-analysis6 published in 2018, researchers found that when comparing acupuncture combined with conventional antipsychotic medication to the use of antipsychotic medication alone, acupuncture combined with antipsychotic medication showed significantly better efficacy in treating SZ. In our study, we focused on the primary outcome measure of overall effectiveness rate and selected PANSS, BPRS, SANS, and SAPS as secondary outcome measures, providing a more comprehensive reflection of the effectiveness of acupuncture treatment.
In published network meta-analyses,7 researchers compared the efficacy of acupuncture combined with Western medicine to the use of Western medicine alone and found that acupuncture had the best efficacy when combined with body acupuncture. In contrast, our meta-analysis has several unique features. Firstly, we performed GRADE evidence grading for each outcome to ensure the reliability of the research findings. Secondly, we conducted subgroup analyses for the overall effectiveness rate to explore differences among different subgroups. Additionally, we performed a meta-regression specifically for the primary outcome measure (overall effectiveness rate) and found that prolonged treatment may not be beneficial for patient recovery.
Clinical Implementation
The findings suggest that acupuncture treatment is an effective adjunctive therapy for schizophrenia and can be used as a supplement or alternative to traditional medication, providing clinicians with a new treatment option.
The Inspiration for Future Directions
Although the meta-analysis results demonstrate the effectiveness of acupuncture, further exploration is needed regarding the treatment mechanisms and long-term effects of acupuncture. Additionally, considering the methodological limitations and quality issues in the studies, more high-quality, large-sample, multicenter clinical trials are required to validate and strengthen these findings. A more comprehensive evaluation of acupuncture’s clinical applications in patients with SZ will provide healthcare professionals and patients with more reliable treatment evidence and decision-making support.
Strengths and Limitations
Based on our understanding, this is the first systematic review to evaluate the efficacy and safety of acupuncture as an adjunctive therapy for improving clinical symptoms in patients with schizophrenia.
Our strengths lie in several aspects. First, we selected the total effective rate as the primary outcome measure and conducting subgroup analysis on the primary outcome measure, which allows for a more accurate evaluation of the effect size between different subgroups and further confirms the effectiveness of acupuncture. Second, we performed a meta-regression on the effective rate and found a negative correlation trend between treatment duration and treatment effect, suggesting that longer treatment duration may not be beneficial for patient recovery. Third, we conducted a GRADE assessment on the outcome measures, enhancing the credibility of the results.
We also analyzed the acupoints mentioned in the literature and found that the most frequently mentioned acupoints were Baihui (GV20) (26 times), Neiguan (PC6) (15 times), Yintang (EX-HN3) (13 times), Zusanli (ST36) (13 times), Taichong (LR3) (13 times), Fenglong (ST40) (13 times), Sanyinjiao (SP6) (12 times), Hegu (LI4) (12 times), Shenmen (HT7) (12 times), and Sishencong (EX-HN1) (8 times). Clinical practitioners can use these findings to selectively choose these acupuncture points for acupuncture treatment, aiming to enhance treatment effectiveness. Furthermore, the discovery of these high-frequency acupuncture points provides valuable clues for further exploring the mechanisms of acupuncture treatment and contributes to a deeper understanding of the specific role and pathways of acupuncture in the treatment of SZ.
This study has several limitations: (1) Most of the included studies did not mention the implementation of allocation concealment and blinding, which may introduce selection bias. (2) The interventions included in the studies, such as the types of adjunctive medication, forms of acupuncture, duration of treatment, and techniques used, varied, which could affect the accuracy of the results.
Conclusion
Existing evidence suggests that acupuncture, as an adjunctive therapy used in conjunction with Western medicine or other treatments, can improve the overall effectiveness in patients with SZ, reduce adverse reactions, and improve the mental condition, alleviating the severity of symptoms in SZ patients. However, due to limitations in the quality of the included studies, further high-quality research is needed to validate the above conclusions.
Data Sharing Statement
All data relevant to the study are included in the article or uploaded as Online Supplemental Information. The data used in this review was collected from the thirty-eight eligible studies and therefore available in the public domain.
Author Contributions
All authors have made significant contributions to the work reported, whether in the conception, study design, execution, data acquisition, analysis and interpretation, or in all of these areas. They have all been involved in drafting, revising, or critically reviewing the article, and have given final approval for the version to be published. They have also agreed on the journal to which the article has been submitted and committed to being accountable for all aspects of the work.
Funding
The authors received no financial support for the research, authorship, and/or potential publication of this article.
Disclosure
The authors have no conflicts of interest to declare for this work.
References
1. World Health Organization. Factsheet on Schizophrenia. World Health Organization Newsroom; 2019.
2. Moreno-Küstner B, Martín C, Pastor L. Prevalence of psychotic disorders and its association with methodological issues. A systematic review and meta-analyses. PLoS One. 2018;13(4):e0195687. doi:10.1371/journal.pone.0195687
3. Du Y, Yu Y, Hu Y, et al. Genome-Wide, integrative analysis implicates exosome-derived MicroRNA dysregulation in schizophrenia. Schizophr Bull. 2019;45(6):1257–1266. doi:10.1093/schbul/sby191
4. Rognoni C, Bertolani A, Jommi C. Second-generation antipsychotic drugs for patients with schizophrenia: systematic literature review and meta-analysis of metabolic and cardiovascular side effects. Clin Drug Investig. 2021;41(4):303–319. doi:10.1007/s40261-021-01000-1
5. Hui KK, Marina O, Liu J, Rosen BR, Kwong KK. Acupuncture, the limbic system, and the anticorrelated networks of the brain. Auton Neurosci. 2010;157(1–2):81–90. doi:10.1016/j.autneu.2010.03.022
6. Zhao J-Q, Ma T-M. Meta-analysis of acupuncture treatment for schizophrenia. Acupunct Res. 2018;43(12):806–812. doi:10.13702/j.1000-0607.170716
7. Zhaohan H, Yuan F, Xiaolu W, Yue H, Qi YU, Tong W. Effectiveness of acupuncture-related therapies on schizophrenia: a Bayesian network Meta-analysis. J Tradit Chin Med. 2023;43(2):239–251. doi:10.19852/j.cnki.jtcm.20221226.001
8. Chinese Society of Psychiatry, Chinese Medical Association. Chinese Classification and Diagnostic Criteria of Mental Disorders. Vol. 35. Nanjing: Southeast University Press; 1995:64.
9. Chen YF. Chinese classification of mental disorders (CCMD-3): towards integration in international classification. Psychopathology. 2002;35:171–175. doi:10.1159/000065140
10. World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. World Health Organization; 1992.
11. Edition F. Diagnostic and statistical manual of mental disorders. Am Psychiatric Assoc. 2013;21:591–643.
12. Feng-Ju Y, Fu-Gen S, Zhi-Hua Z. Short-term curative effect of electroacupuncture as an adju nctive treatment on schizophrenia. Chin J Integ Tradit West Med. 2006;26(3):253–255.
13. Jiang P-R, Xiao Q, Dai L-Y, et al. Exploring the adjunctive effect of electroacupuncture in the treatment of schizophrenia. Psychol Doc. 2011;7:529.
14. Fan H. Influence of risperidone combined with electro-acupuncture on the curative effect and P300 of schizophrenic patients. J Psych. 2015;28(01):43–45.
15. Gong S, Qu Y, Ai C. Effects of acupuncture and moxibustion on living ability in patients with schizophrenia. J Hubei Univer Chin Med. 2015;17(04):79–81.
16. Liu X-C, Su X-L, Zhao L-Z. Observation on the therapeutic efficacy of electroacupuncture combined with medication in the treatment of schizophrenia. J Mod Integ Trad Chin West Med. 2011;20(12):1483–1484.
17. Huang Y, Zheng Y. Sleep disorder of schizophrenia treated with shallow needling: a randomized controlled trial. Chin Acupun Moxibust. 2015;35(09):869–873.
18. Gao L, Wang T-L, Yuan Y-T. Clinical study of intelligent electroacupuncture combined with drug treatment for auditory hallucinations. Med J Chin People’s Health. 2014;26(12):39–40.
19. Chen M-M, Xu Y. Comparative study on the treatment of agitated state in schizophrenia with electroacupuncture combined with olanzapine. Pract Clin J Integ Tradit Chin West Med. 2015;15(09):32–34.
20. Chen J, Zhou C-M, Chen X-X. Comparative study on the therapeutic effects of risperidone combined with fluphenazine and electroacupuncture in the treatment of agitated state in schizophrenia. Stra Pharmaceut J. 2016;28(08):213–214.
21. Zhao L, Zhang N, An Y-M, et al. Clinical observation of acupuncture combined with olanzapine in the treatment of 40 cases of schizophrenia. Hebei J Tradit Chin Med. 2013;35(10):1533–1534.
22. Xiong D-Z, Liu L-L, Liu Y-Y. Observation on the therapeutic effect of electroacupuncture combined with small dose of clozapine in clinical treatment of refractory schizophrenia. Acupunct Res. 2010;35(2):134–137.
23. Du Y-J. Efficacy of acupuncture combined with sulpiride in the treatment of schizophrenia dominated by negative symptoms. Pract Clin Med. 2011;12(05):19–21.
24. Li G-H, Yan M. Scalp acupuncture with treatment for refractory auditory hallucination in schizophrenia patients-A report of curative effect observation of 60 cases. Liaoning J Tradit Chin Med. 2012;39(07):1396–1398.
25. Li G-H, Hu Y-H, Yan M. Clinical efficacy observation of electroacupuncture in the treatment of refractory auditory hallucinations. Chin J Behav Med Brain Sci. 2006;2006:(11):1015.
26. Xu T-C, Su J, Wang W-N. Effect of three-step acupuncture combined with small dosage antipsychotic in treating incipient schizophrenia. Chin J Integ Tradit West Med. 2010;30(11):1138–1141.
27. Cui G-M, Wang P. Clinical study on the treatment of schizophrenia with electroacupuncture combined with chlorpromazine. J Mod Integ Trad Chin West Med. 2000; 16:1536–1537.
28. Ou Y-Y, Zhang X-F, Ouyang H-L, Huang Y, Ouyang Q. Therapeutic observation of acupuncture plus moxibustion at shenque(GV 8) for schizophrenia. Shangh J Acupunct Moxib. 2014;33(09):795–797.
29. Liu X. Acupuncture treatment for refractory auditory hallucination in schizophrenia patients——a report of 50 cases. J Tradit Chin Med. 2010;51(07):621–624.
30. Zhao L-J. Clinical efficacy of traditional Chinese medicine syndrome differentiation acupoint selection acupuncture combined with low-dose risperidone in the treatment of schizophrenia. Henan Med Res. 2018;27(24):4553–4554.
31. Chen J. Analysis of the effects of acupuncture combined with aripiprazole on executive function and quality of life in patients with post-schizophrenic depression. Chin J Pract Med. 2017;12(03):139–140.
32. Dang Y-M, Cai J-Y, Cui J, et al. Efficacy of acupuncture in treating patients with treatment-resistant auditory hallucinations in schizophrenia and observations on social functioning. Chin J Clin Res. 2017;9(19):25–27.
33. Qin L, Chen Z, Wang Y, Nie H, CHen L. Study on acupuncture combined Clozapine in treatment of refractory schizophrenia. Med J Chin People’s Health. 2017;29(14):7–10.
34. Li H. Effect of electric needle combined with clozapine in refractory schizophrenia. Contemp Med. 2022;28(6):55–57.
35. Ji Y, Li X, Hong Q. Effect of clozapine combined with electroacupuncture in the treatment of refractory schizophrenia. Tibetan Med. 2022;43(2):67–69.
36. Yang J, Yang C, Zhang J. Impact of acupuncture combined with medication on cognitive function and serum hcy and nrg-1 in patients with schizophrenia. Shangh J Acupunct Moxib. 2022;41(09):883–888.
37. Li H. Clinical observation on the treatment of first-episode schizophrenia with electroacupuncture of Baihui Yintang and antipsychotics. Contemp Med. 2021;27(26):23–25.
38. Shen H, Zhao H, Chen J, Lu Y, Pan L. Curative effect of integrated traditional Chinese acupuncture and western medicine on patients with phlegm dampness block schizophrenia. J Guizhou Med Univer. 2021;46(11):1338–1342.
39. Zhon L-L, Lin W-Y. Clinical study on the therapeutic effect of acupuncture combined western medicine in patients with schizophrenia of remission. J Nongken Med. 2021;43(06):481–483.
40. Zheng W, Zhang L-M, Huang H-X, Lin X-D, Sun Q-Y. The influence of acupuncture therapy on cognitive function in patients with chronic schizophrenia. Mod Pract Med. 2020;32(01):75–77.
41. Li Q, Tian Y. The effect of scalp acupuncture combined with electroacupuncture on cognitive function in paranoid schizophrenia patients. Chin J Mod Drug Applic. 2020;14(03):104–106.
42. Pan L, Shen H-B, Zhang J, Lu Y, Zhao H. Effect of acupuncture on quality of life of patients with schizophrenia of remission. World J Integ Tradit West Med. 2020;15(04):593–596.
43. Li H, Li X. Exploring the effectiveness of acupuncture in the treatment of schizophrenia. J Contemp Med. 2020;18(11):196–197.
44. Cheng L, Kang C. Observation and analysis of efficacy and safety of electroacupuncture combined with fluphenazine and risperidone in the treatment of excited state of schizophrenia. J Integ Tradit Chin West Med Cardio Cerebrov Dis. 2020;8(29):62–63.
45. Li J, Li X, Liu C, Xu L, Yang P. Clinical observation on the effect of acupuncture with brain-heart concurrent regulation therapy with risperidone on aggressive behavior and cognitive function of schizophrenia. J Hunan Univer Chin Med. 2020;40(10):1244–1248.
46. Liao Y. Effect of acupuncture and moxibustion combined with clozapine in the treatment of refractory schizophrenia. Heilongjiang Sci. 2019;10(06):50–51.
47. Lin F, Chen M. Clinical analysis of olanzapine combined with electroacupuncture in the treatment of negative symptoms of male schizophrenia: a clinical analysis of 30 cases. Chin Health Stand Manag. 2018;9(02):97–99.
48. Cheng J, Wang G, Xiao L, Wang H, Wang X, Li C. Electro-acupuncture versus sham electro-acupuncture for auditory hallucinations in patients with schizophrenia: a randomized controlled trial. Clin Rehabil. 2009;23(7):579–588. doi:10.1177/0269215508096172
49. Bouhlel S, El-Hechmi S, Ghanmi L. Apport de l’acupuncture dans le traitement de la schizophrénie: etude randomisée en double-aveugle portant sur 31 patients [Effectiveness of acupuncture in treating schizophrenia: a clinical randomized trial of 31 patients]. Tunis Med. 2011;89(10):774–778. French.
50. Camchong J, MacDonald AW, Bell C, Mueller BA, Lim KO. Altered functional and anatomical connectivity in schizophrenia. Schizophr Bull. 2011;37(3):640–650. doi:10.1093/schbul/sbp131
51. Pomarol‐Clotet E, Canales‐Rodríguez EJ, Salvador R, et al. Medial prefrontal cortex pathology in schizophrenia as revealed by convergent findings from multimodal imaging. Mol Psychiatry. 2010;15(8):823–830. doi:10.1038/mp.2009.146
52. Fang J, Zhen J, Li K, et al. The salient characteristics of the central effects of acupuncture needling: limbic–paralimbic–neocortical network modulation. Hum Brain Mapp. 2009;30(4):1196–1206. doi:10.1002/hbm.20583
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

