Back to Journals » Nature and Science of Sleep » Volume 15
A First Glimpse at the Latent Structure of Sleep Valuation Using a Sleep Valuation Item Bank
Authors Kay DB, Simmons Z, Nielson SA, Braithwaite SR, Esplin C
Received 23 August 2022
Accepted for publication 30 January 2023
Published 21 March 2023 Volume 2023:15 Pages 127—137
DOI https://doi.org/10.2147/NSS.S386838
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ahmed BaHammam
Daniel B Kay,1 Zach Simmons,1 Spencer A Nielson,2 Scott R Braithwaite,1 Charlotte Esplin1
1Department of Psychology, Brigham Young University, Provo, UT, USA; 2Department of Psychology, Virginia Commonwealth University, Richmond, VA, USA
Correspondence: Daniel B Kay, Department of Psychology, Brigham Young University, UT 1090 KMBL, Provo, UT, 84602, USA, Tel +1 801 422-7949, Email [email protected]
Introduction: Sleep valuation is the relative worth individuals place on sleep. Our prior study using a Sleep Valuation Item Bank (SVIB) showed that sleep valuation relates to age, gender, and health status. In this study, the psychometric properties of the SVIB and its latent factor structure were explored. We also investigated how sleep valuation factors relate to demographic, psychological, and sleep features.
Methods: Participants (N = 854) were recruited through TurkPRIME and completed a survey consisting of demographic, psychological, and sleep-related questions. The distributional properties of the SVIB items were quantified. Cronbach’s alpha and correlation analyses were used to assess the internal consistency and test-retest reliability of SVIB items. Iterated principal factoring with a Promax rotation was used on the SVIB to explore its latent factor structure. Multiple regression analyses were used to investigate the variables associated with each factor.
Results: The factor analysis identified 29 items with factor loadings ≥ 0.4 on four major factors, tentatively called (1) sleep wanting, (2) sleep prioritizing, (3) sleep onset preference, and (4) sleep devaluation. While women had higher sleep wanting and lower sleep devaluation scores than men, they had lower sleep prioritizing. Older individuals tended to value sleep less but also devalued it less than younger participants. Finally, although both individuals with insomnia and depression devalued sleep, depressed individuals prioritized it more than those who were less depressed, while individuals with insomnia symptoms wanted sleep and preferred sleep onset more than those with less insomnia symptoms.
Discussion: The current SVIB captures broad dimensions of sleep valuation (wanting, prioritizing, preferring) and sleep devaluation. These broad dimensions had distinct patterns across person-level factors. Recognition of individual differences in sleep valuation may help target sleep health advocacy efforts and individualized treatment approaches, including for those with depression or insomnia.
Keywords: sleep valuation, sleep health, sleep quality, insomnia, depression
Sleep valuation is the relative worth placed on sleep. The active part of this concept, valuation is defined herein broadly as the degree of value (ie, importance, desire, wanting, preference, liking, or satisfaction) placed on objects, activities, and experiences. As the valued “object”, sleep is conceptualized as a set of reversible, naturally reoccurring states involving reduced conscious awareness. Many types of values have been proposed including those values held by an individual (ie, individual values) and those values held by societies, institutions, and organizations (ie, societal values).1 This paper focuses more specifically on sleep valuation held at the individual level, which has long been known to contribute to thoughts, feelings, and behaviors about its object.2 As such, sleep valuation has major implications for sleep health behavior and sleep disorder prevention and treatment efforts. Indeed, valuing sleep was recently highlighted as the first of 5 Principles of good sleep health: value, prioritize, personalize, trust, and protect sleep.3
At the individual level, valuation can be broken down into intrinsic and extrinsic forms. Intrinsic value has been described as the value an individual places on objects, activities, and experiences for their own sake, while extrinsic value refers to values held for their ends. Sleep can be thought of as both an end in itself (intrinsic value) and a means to an end (extrinsic value). Sleep psychologists have framed sleep in instrumental conditioning theory as having intrinsic value, proposing that sleep is a self-reinforcing consequence of sleep onset and associated behaviors.4 Survey results support the view that sleep has intrinsic value, in that 33% of Americans said they like or love sleep, feel good/great/OK about sleep, or felt grateful for sleep, 14% reported sleep as their favorite part of the day, and 6% reported sleep was a personal indulgence.5 Some people view sleep as a reprieve or escape from the pains and cares of wakefulness and may, likewise, value sleep for these intrinsic benefits. These observations support the view that sleep can serve as a positive or negative reinforcer with intrinsic value. Sleep psychologists have also framed sleep as a complex behavior with its own set of instrumental consequences.6 Sleep researchers have argued variously that sleep is the price we pay for wakefulness, plasticity, or life and have long wondered why mammals invest so much time in sleep.7–9 Sleep is associated with a host of health outcomes that may be deemed rewarding, such as rejuvenation of cognitive, affective, and physical functioning. Conversely, poor sleep has been linked to impairments in these domains.10 As such, many people may come to extrinsically value sleep for its secondary gains or avoidance of the negative consequences of its neglect. Indeed, in the aforementioned survey, 62% of respondents reported that sleep is necessary to recharge/restore/refresh.5 Whether intrinsic or extrinsic, sleep valuation is reflected in the large amount of money spent on sleep promotion each year, including on sleep treatments, over-the-counter remedies for sleep problems, beds and bedding, sleep-related apps, sleep tracking devices, and other devices designed to promote sleep quality.11–14 There is evidence that sleep is valued by many individuals as a valid currency that is used transactionally with other objects, activities, and experiences. One of the earliest human writings, dating over 3000 years ago, describes this transaction process in the Epic of Gilgamesh whose hero weighed his accomplishments during wakefulness against his sacrificed sleep, “Of my slumber sweet my face had too little, I have scourged myself by going sleepless, I have filled my sinew with sorrow, and what have I achieved by my toil?”15 This ancient reference highlights how two ends, sleep and wakefulness, having supreme status commonly come in conflict in this transaction. Modern economists have sought to estimate the opportunity cost of an hour of sleep,16 and currently terms such as sleep debt and sleep deficit reflect the analogy of monetary value placed on sleep, often bargained against waking activities.17,18 Collectively, these findings support the view that because sleep is a valued state of being and a state that has value-laden consequences on health and daytime functioning, it also carries the potential for high individual value.
We recently introduced a novel Sleep Valuation Item Bank (SVIB), the first measure designed specifically to study the construct of sleep valuation.19 That study provided reliability estimates for each item of the item bank and found concurrent validity for the total score with several demographic, sleep, and health variables.19 Consistent with a national survey,20 we showed that women value sleep more than men and that greater sleep valuation was associated with poorer mental and physical health. These latter associations were explained by the shared relationship of sleep valuation and health with poorer sleep. However, the sample was relatively small and had limited diversity, preventing us from conducting an exploratory factor analysis to determine the latent structure of sleep valuation captured by the SVIB. In the present study, we sought to further develop the construct of sleep valuation in a larger, nationally stratified adult sample using the SVIB. We quantified the internal consistency reliability and test-retest reliability of items. As a preliminary step to investigate the latent structure of sleep valuation, we used exploratory factor analysis. Additionally, we investigated associations between the SVIB factors and individual differences in demographic, psychological, and sleep features.
Methods
The SVIB is a list of 43 items generated by Dr. Kay and his research team to capture attitudes and behaviors that might reflect sleep valuation.19 These items were sent to 17 of Dr. Kay’s peers who had an advanced degree (Ph.D. or M.D.) and prior publications in sleep research. Evaluators were offered $20 for sharing their time and insights. To help the evaluators provide feedback from respondents’ perspective, they were instructed to first respond to each item as a respondent. Next, they were asked to rate how essential each item was on a 3-point rating scale of necessity (ie, Essential = 2, Useful but Not Essential = 1, Not Necessary = 0). In total, 9 individuals scored each item. Several evaluators left insightful comments on individual items. Overall, evaluators felt that the items were useful or essential, with an average rating of 1.42/2 (Supplemental Table 1). There was general agreement that items 15, 16, 30, and 32 were not necessary. Items 13, 25, and 37 met criteria for being essential using Lawshe’s equation for determining the content validity ratio (CVR), (ne - N/2)/(N/2) where ne is the number of panelists who rated an item as “essential”, N is the total number of evaluators, and CRV = 0.78 is the threshold for significance at p < 0.05.21 Evaluators were also encouraged to make comments about each item and reasons for their ratings. A few evaluators noted that some items (ie, 2, 9, 15, 17, 26, 30, 32) may reflect depression rather than sleep valuation.
Based largely on peer evaluation, the sleep valuation items were modified for clarity before being administered as part of a Qualtrics survey study to a sample of individuals recruited through TurkPrime. A stratified sample was sought based on age (18–99), race (50% White, 17% Black, and 8.33% for each American Indian, Asian, Pacific Islander, and other), gender (50/50 female/male), and employment status (50% employed full time and 8.33% for each part-time, homemaker, retired, student, temp worker, unemployed, and disabled). This survey study complied with the Declaration of Helsinki and the study protocol was approved by the Institutional Review Board at Brigham Young University.
Participant informed consent was obtained electronically by clicking on a button that indicated that they understood the purpose of the study, accepted the minimal risk associated with the study, and qualified for the study. Upon providing consent, participants completed a Qualtrics survey that assessed basic demographic information including gender, race/ethnicity, age, state residence, marital status, level of education, employment status, living arrangements, number of dependents, age of children, annual income, general health estimate on a scale from 0 (extremely unhealthy) to 100 (extremely healthy), caffeine consumption, drug use, and medications. Following the demographics questions, participants answered the items from the SVIB. Participants rated agreement with each item on a scale from 0 (strongly disagree) − 100 (strongly agree). They then completed questionnaires on sleep and mood including the Pittsburgh Sleep Quality Index (PSQI), a valid and reliable measure of sleep quality over the prior month,22 the Insomnia Severity Index, a 7-item reliable and valid assessment of insomnia severity,23 the Patient-Reported Outcomes Measurement Information System (PROMIS) Depression Item Bank, a 24-item validated assessment of depression severity,24 the PROMIS Sleep-Related Impairment (PROMIS-SRI) Item Bank a 16-item validated assessment of impairment related to sleep difficulty,25 and the PROMIS Sleep Disturbance (PROMIS-SD) Item Bank, a validated 27-item measure of sleep disturbance severity.25 At the end of the survey participants again completed the sleep valuation items. Participants were debriefed electronically after completing the survey.
Analyses
Of the 1110 individuals in the original sample pool provided by TurkPrime, 164 participants were excluded due to failure to complete at least 95% of the survey and/or completing the survey in less than 7 minutes. An additional 92 participants were excluded following a visual inspection of response set patterns. Individuals who responded consistently high or consistently low, despite negative or positive wording of items on the SVIB, were excluded. Analyses were conducted on the remaining 854 participants. Psychometric properties including distributional properties, normality, central tendency, and variance were assessed for each item of the SVIB. Agreeing with peer evaluators, items 17, 30, and 32 were removed prior to analyses due to poor face validity (ie, reflected depression). Cronbach’s alpha and Pearson’s correlation coefficient were used to help identify SVIB items with poor internal and test-retest reliability. Negatively worded items were reverse scored to compute the total score prior to its use in analyses (note that these items were not reverse scored in the factor analysis described below). Supplemental Table 1 shows the full list of original questionnaire items and psychometric properties. Item-level correlations with the total score showed that 12 items (3, 14, 16, 20, 21, 22, 29, 31, 33, 34, and 42) had negligible to low correlations (>-0.3 to <0.3) with the total score, perhaps suggesting lesser relevance in their ability to discern overall sleep valuation. Most of these items were negatively worded. Alpha levels of the items all exceeded 0.92 with an average of 0.92, indicating acceptable internal consistency.
We performed iterated principal factoring with a Promax rotation on the remaining 40 items to explore the latent factor structure of the SVIB. Factor loadings <0.40 were suppressed. The scree plot method was used to identify the appropriate number of factors to extract, and we used Bartlett’s method to compute the factor scores used in subsequent analyses.
Multiple regression analyses were used to determine the variables most strongly associated with each SVIB factor. The independent variables in the multiple regression analyses were gender referenced to “male”, race/ethnicity referenced to “White”, marital status referenced to “married”, education referenced to “graduated 4-year college”, occupation referenced to “employed full-time”, general health estimate, age, income referenced to “$10,000-$40,000”, depression severity, and insomnia severity.
To investigate whether the sleep valuation factors were more or less associated with extrinsic or intrinsic valuation, we conceptualized the PROMIS-SRI, a measure of sleep-related impairment as an instrumental valuation marker. We used Pearson correlations to quantify the association between PROMIS-SRI and each factor and then used Fisher’s Z test to compare the strength of the correlations. Analyses were performed with STATA 16 (StataCorp. 2019. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC). With the exception of the test-retest correlations, all analyses were conducted on the first administration of the SVIB.
Results
Table 1 shows the demographic features of the sample. In summary, the sample was stratified across gender (49%/50%/1% female/male/transgender), age (range 18–79), race (53% White, 18% Black, 12% Asian, 9% Latino, 5% other, 4% mixed), and employment status (36% employed full-time, 21% retired, 11% employed part-time, 9% unemployed, seeking work, 8% disabled, 6% caregiving/house-keeping full-time, 4% full-time student/training, 3% unemployed, not seeking work, and 1% other).
 |
Table 1 Demographic Features |
In the exploratory factor analysis, we found support for four factors based on the scree plot method (Figure 1). All 4 factors had eigenvalues greater than 1 (Table 2). Item loadings are reported in Table 3. Eleven items had poor factor loadings (<0.4) or double factor loadings and were suppressed. We tentatively labeled the factors sleep wanting, sleep prioritizing, sleep onset preference, and devaluation. On the sleep wanting factor, 13 items had an average factor loading of 0.59. Most of the items on this factor suggest a desire to obtain more sleep, to sleep longer, and to obtain the benefits of sleep: “I generally desire more sleep”, “I would want to sleep more if my sleep were more restful”, “I want to sleep more because I feel sleepy”, and “I want to sleep more because I enjoy it so much” (italics added for emphasis). Several items suggest a preference to sleeping longer as opposed to getting up in the morning. On the sleep prioritizing factor, 6 items had an average factor loading of 0.64. Most of the items on this factor suggest a proactive intention to obtaining sleep on principle, which seems decoupled from the instrumental value of sleep, as reflected by item 26: “I want to sleep even when I am not sleepy”. On the sleep onset preference factor, the 3 items had an average factor loading of 0.75. Most of the items on this factor reflect an emphasis on the preference of going to sleep over other activities. On the sleep devaluation factor, 7 items had an average factor loading of 0.55. Factor correlations were medium strong among the 3 sleep valuation factors, but the sleep devaluation factor was only weakly correlated with the other factors (Table 4).
 |
Table 2 Factor Eigenvalues |
 |
Table 3 Exploratory Factor Analysis with a Promax Rotation of the Sleep Valuation Item Bank |
 |
Table 4 Factor Correlations |
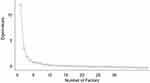 |
Figure 1 Scree plot with inflection point suggesting 4 factors are captured by the Sleep Valuation Item Bank. |
To help determine whether each factor related more or less to extrinsic valuation, we conducted follow up correlations between sleep-related impairments and each sleep valuation/devaluation factor. Using Fisher’s Z, we found that the sleep wanting factor correlated most strongly with sleep-related impairments (r = 0.60), as compared to the sleep prioritizing (r = 0.28), sleep onset preference (r = 0.23), and sleep devaluation (r = −0.26) factors, p < 0.001 for all comparisons.
Table 5 displays the results of the multiple regression analyses investigating the associations of each sleep valuation factor with demographic, psychological, and sleep features. In adjusted models, women had higher sleep wanting scores, lower sleep prioritizing scores, and lower sleep devaluation scores than men. Race/ethnicity, marital status, and education were largely unrelated to sleep valuation with a few exceptions. Compared to married individuals, separated individuals had lower devaluation scores, and those cohabiting had lower sleep prioritizing scores. Compared to individuals with a college education, those with 7–12 years of education had lower sleep preference scores and those with a professional degree had lower sleep devaluation scores. Age, household income, occupational status, depression severity, and insomnia severity showed nuanced patterns of significance. Older individuals had lower sleep wanting scores and lower sleep prioritizing scores but lower sleep devaluation scores. Compared to those with household income of $10,001-$40,000, individuals who endorsed $90,001-$190,000 yearly income had higher sleep prioritizing scores but higher sleep devaluation scores as well. Individuals with greater depression symptoms had higher sleep prioritizing and sleep onset preference scores, but also higher sleep devaluation scores. Individuals with more severe insomnia had higher sleep wanting and sleep preference scores, but again higher sleep devaluation scores.
 |
Table 5 Results of the Multiple Regression Predictors of Sleep Valuation Item Bank Factor Scores |
Discussion
A primary aim of this study was to explore the latent factor structure of the SVIB, a novel instrument designed to study sleep valuation. Using factor analysis, we found evidence for four factors, which we tentatively labeled sleep wanting, sleep prioritizing, sleep onset preference, and sleep devaluation. Conceptually, factors 1 (wanting) and 3 (preference) include items that signify preference for sleep. However, the preference tends to be for different aspects of sleep, the former staying asleep and the latter going to sleep. The distinction between these factors may relate to the concept of diminishing marginal utility in which each unit of gain is associated with a smaller increase in valuation. From this perspective, sleep onset preference may gain relative value due to its primacy in satisfying the sleep need and the value of waking activities diminishes across the day. In contrast, the sleep wanting factor appears to be more relative to the enjoyment, satisfaction, benefits, or satiation the individual obtains from sleep relative to the wake state. The finding of a stronger correlation between daytime sleep-related impairment and the sleep wanting factor supports the interpretation that it is more related to the utility of sleep. A seemingly odd loading was a “desire” item in the sleep prioritizing factor: “I want to sleep even when I am not sleepy”. However, as with the other items that loaded on this factor, it seems to be more suggestive of commitment to sleep regardless of sleep need, rather than a desire for sleep because of sleep need. The fourth factor, sleep devaluation, was unique in several ways. Its items tended to correlate poorly with the sleep valuation total score and its factor score was only weakly correlated with the other sleep valuation factors. The positive correlations found for sleep devaluation with the sleep wanting and sleep prioritizing factors were somewhat surprising but highlight that many people are ambivalent about sleep. A previous national survey supports a common ambivalence towards sleep’s value, in that 82% of Americans reported that an extra hour of sleep at night would be somewhat or extremely valuable to them, yet only 26% of respondents said they would choose sleep over other activities if they were given an extra hour in the day.5 Despite clear intrinsic and extrinsic value, as much as 15% of respondents in that survey had negative feelings about sleep or felt that sleep is a waste of 1/3 of their lives.5 More broadly, many people are willing to sacrifice sleep health for other activities, including academic study, social engagement, media use, and entertainment.26–28 Collectively, these findings suggest that sleep devaluation and sleep valuation may be separate constructs, as opposed to opposite ends of the same dimension. Collectively, we found evidence for 3 sleep valuation factors and a devaluation factor. As outlined in the introduction, valuation is often broken down into intrinsic and extrinsic types. Our factors did not map cleanly onto this conceptualization. The identified factors appear to reflect broad dimensions of sleep valuation rather than explanatory mechanisms (ie, extrinsic vs intrinsic).
Another major aim of this study was to explore how sleep valuation factors related to individual differences in demographic, psychological, and sleep features. We found several interesting patterns in relation to prior studies. First, while prior evidence suggested that women tend to value sleep more than men, our results suggest that sleep valuation between men and women is more nuanced.19,20 Compared to men, women had higher sleep wanting scores and lower sleep devaluation scores, but men tended to have higher sleep prioritizing scores than women. These findings support high levels of ambivalence about sleep’s value among both men and women. Second, consistent with a previous national survey,5,20 we found a clear pattern of decreased sleep valuation with age across 3 of the sleep valuation factors. Yet, older individuals tended to devalue sleep less than younger participants. Third, prior evidence has linked employment to sleep behavior. We found that individuals working full-time tended to value sleep more than individuals with other types of work status, but again patterns of associations were nuanced. Interestingly, students tended to have lower sleep prioritizing scores than full-time workers, suggesting they value sleep but are less preoccupied with prioritizing it. The finding that unemployed individuals had lower wanting scores than full-time works was unexpected, as prior studies showed that unemployed individuals tend to have poorer sleep,29 and poor sleep has been linked to greater sleep valuation.19 Fifth, congruent with our previous study, we found that those with poorer mental health as indexed by greater depression or greater insomnia tended to have higher sleep valuation.19 For depression, this was limited to the prioritizing and preference factors. We found no evidence that those with more depressive symptoms wanted sleep more, but they did have higher devaluation. For insomnia, the nuanced pattern across factors was intriguing. Those with more insomnia symptom severity wanted sleep more and valued sleep onset but had greater sleep devaluation. Surprisingly, there was only a trend for sleep prioritizing associated with insomnia severity. A common clinical observation is that individuals with insomnia desire sleep greatly, potentially maladaptively; this, coupled with a high valuation for sleep onset preference and devaluation of sleep, may contribute to the clinical presentation of insomnia. In combination with our previous study, these results suggest that sleep valuation relates to many person-level factors.
This study has notable limitations. Because the study was conducted online, participants may have rushed through the questions, particularly while doing the relatively long SVIB. At least 10% of respondents appeared to not take notice of the negative wording of several items, responding in a consistent pattern regardless of the direction of the questions. We were able to remove many of the more egregious patterns of response sets through visual inspection of the data, but many of the remaining participants may have missed the need to respond differently on the sleep devaluation items. This may explain, in part, the poor correlation between devaluation items and sleep valuation total score. Separating out the devaluation items from the SVIB may be advisable to explore how a response set may have influenced the results. The current item bank is by no means comprehensive, and development of additional sleep valuation items is warranted. We did not find factors that reflect cleanly, other broad aspects of valuation such as sleep liking, sleep enjoyment, sleep importance, or sleep satisfaction. The lack of a significant loading of item 41 “I enjoy sleeping” may suggest that more items are needed to capture pleasure-based components of sleep valuation such as “liking” or “enjoying” sleep. To capture a distinction between intrinsic and extrinsic valuation, items that more explicitly ask about secondary benefits of sleep are warranted.
The importance of values on attitudes and behavior is well recognized in social science research and in clinical practice more broadly. A rich literature on valuation theory and research has relevance to the field of sleep and sleep medicine. In this study, we focused on sleep valuation at the individual level. Future studies on the antecedents and consequences of sleep valuation are needed. Studies on the relationships between sleep valuation and treatment seeking for sleep problems, willingness to pay for sleep therapy, and adherence to treatment recommendations may inform efforts to promote sleep health and may help to predict treatment outcomes. For example, in cognitive-behavioral therapy for insomnia (CBTI), a major component of treatment is changing dysfunctional beliefs and attitudes about sleep. Research is needed to test if sleep valuation can be used to determine whether treatment effectively replaced maladaptive beliefs and attitudes about sleep with more adaptive ones. Value interventions in the context of sleep medicine may be one interesting untapped adjunct to CBTI and other psychological approaches to insomnia (e.g., Acceptance and Commitment Therapy for Insomnia). Sleep valuation is a novel concept and many questions about it remain. Supplemental Table 2 lists several future directions and questions to facilitate research on this topic.
Conclusion
Sleep valuation is a novel concept with implications on sleep health. Ours is the first study to investigate the latent structure of sleep valuation and how sleep valuation subfactors relate to person-level variables including demographic, psychological, and sleep features. The latent structure found using the SVIB taps into broad domains of valuation including wanting, prioritizing, preferring, and devaluation of sleep. We found wide individual differences in these sleep valuation factors that related to age, gender, employment status, income, depression, and insomnia. Additional work is required to refine the SVIB and eventually validate a brief sleep valuation questionnaire. This line of research may help identify the influence of sleep valuation on sleep health disparities and sleep-related decision-making.
Acknowledgments
We would like to acknowledge the TurkPrime Project Manager, Tommy Roggina for recruiting this sample. We also acknowledge student researchers’ including McKaella Swenson and Josh Mason for input on survey items and entering the items into Qualtrics, respectively. We thank Matthew R. Cribbet, Ph.D., Natalie D. Dautovich, Ph.D., Joseph M. Dzierzewski, Ph.D., Eric R. Eide, Ph.D., Brant P. Hasler, Ph.D., S. Justin Thomas, Ph.D., Kristine A. Wilckens, Ph.D., and 2 anonymous colleagues who provided peer evaluation of the SVIB. We thank Carter Chugg for his editorial review and comments.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Rokeach M. The Nature of Human Values. The Free Press. A Division of Macmillan. London: Collier Macmillan; 1973.
2. Rokeach M. Understanding Human Values: Individual and Societal. New York, N.Y: Free Press. A Division of Macmillan; 1979.
3. Espie CA. The ‘5 principles’ of good sleep health. J Sleep Res. 2022;31(3):e13502. doi:10.1111/jsr.13502
4. Bootzin RR . Stimulus control treatment for insomnia, in Proceedings of the American Psychological Association. Washington, DC: American Psychological Association; 1972. 395396.395396.
5. Better Sleep Council. Survey: Americans don’t value sleep: Americans see sleep as a hero – and a villain. Available from: https://bettersleep.org/research/survey-americans-dont-value-sleep/.
6. Spielman AJ, Caruso LS, Glovinsky PB. A behavioral perspective on insomnia treatment. Psychiatr Clin North Am. 1987;10(4):541–553. doi:10.1016/S0193-953X(18)30532-X
7. Tononi G, Cirelli C. Sleep and the price of plasticity: from synaptic and cellular homeostasis to memory consolidation and integration. Neuron. 2014;81(1):12–34. doi:10.1016/j.neuron.2013.12.025
8. Van Dongen HP, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26(2):117–126. doi:10.1093/sleep/26.2.117
9. Rechtschafen A. Allan Rechtschaffen, Ph.D. In: Eastman C, editor. Conversations with Our Founders. Sleep Research Society; 2010. Available from: https://sleepresearchsociety.org/about/conversations-our-founders/.
10. Killgore WD. Effects of sleep deprivation on cognition. Prog Brain Res. 2010;185:105–129. doi:10.1016/B978-0-444-53702-7.00007-5
11. Daley M, Morin CM, LeBlanc M, Grégoire JP, Savard J. The economic burden of insomnia: direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms, and good sleepers. Sleep. 2009;32(1):55–64 doi:doi:10.5665/sleep/32.1.55.
12. Shelgikar AV, Anderson PF, Stephens MR. Sleep tracking, wearable technology, and opportunities for research and clinical care. Chest. 2016;150(3):732–743. doi:10.1016/j.chest.2016.04.016
13. Leger D, Bayon V. Societal costs of insomnia. Sleep Med Rev. 2010;14(6):379–389. doi:10.1016/j.smrv.2010.01.003
14. Ko PR, Kientz JA, Choe EK, Kay M, Landis CA, Watson NF. Consumer sleep technologies: a review of the landscape. J Clin Sleep Med. 2015;11(12):1455–1461. doi:10.5664/jcsm.5288
15. George AR. The Epic of Gilgamesh: The Babylonian Epic Poem and Other Texts in Akkadian and Sumerian. Oxford University Press; 2020.
16. Cardon JH, Eide ER, Phillips KL, Showalter MH, Wijnen H. Interacting circadian and homeostatic processes with opportunity cost: a mathematical model of sleep with application to two mammalian species. PLoS One. 2018;13(12):e0208043. doi:10.1371/journal.pone.0208043
17. Fischgold H, Lavernhe J, Blanc C. [Sleep, insomnia and sleep debt in aeronautic medicine] Sommeil, insomnie et dette de sommeil dans la médecine aéronautique. Presse Med. 1967;75(8):391–395. French.
18. Foret J, Benoit O. [Study of sleep of shift workers with alternating schedules: adaptation and recovery in case of rapid shift rotation (3–4 days) (author’s transl)] étude du sommeil de travailleurs à horaires alternants: adaptation et récupération dans le cas de rotation rapide de poste (3–4 jours). Eur J Appl Physiol Occup Physiol. 1978;38(1):71–82. French. doi:10.1007/bf00436754
19. Nielson SA, Taylor J, Simmons Z, Decker AN, Kay DB, Cribbet MR. Sleep valuation is associated with components of sleep health and daytime functioning in a college sample: a survey study. Int J Environ Res Public Health. 2021;18(11):5644. doi:10.3390/ijerph18115644
20. Better Sleep Council. Survey: starving for sleep: in the battle to get more sleep, Americans are their own worst enemy. Available from: https://bettersleep.org/research/survey-starving-for-sleep/.
21. Lawshe CH. A quantitative approach to content validity. Pers Psychol. 1975;28(4):563–575. doi:10.1111/j.1744-6570.1975.tb01393.x
22. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi:10.1016/0165-1781(89)90047-4
23. Bastien CH, Vallieres A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. doi:10.1016/S1389-9457(00)00065-4
24. Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D. Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): depression, anxiety, and anger. Assessment. 2011;18(3):263–283. doi:10.1177/1073191111411667
25. Yu L, Buysse DJ, Germain A, et al. Development of short forms from the PROMIS™ sleep disturbance and sleep-related impairment item banks. Behav Sleep Med. 2011;10(1):6–24. doi:10.1080/15402002.2012.636266
26. Hershner SD, Chervin RD. Causes and consequences of sleepiness among college students. Nat Sci Sleep. 2014;6:73–84. doi:10.2147/nss.S62907
27. Okano K, Kaczmarzyk JR, Dave N, Gabrieli JDE, Grossman JC. Sleep quality, duration, and consistency are associated with better academic performance in college students. NPJ Sci Learn. 2019;4:16. doi:10.1038/s41539-019-0055-z
28. Mohammadbeigi A, Absari R, Valizadeh F, et al. Sleep quality in medical students; the impact of over-use of mobile cell-phone and social networks. J Res Health Sci. 2016;16(1):46–50.
29. Blanchflower DG, Bryson A. Unemployment and sleep: evidence from the United States and Europe. Econ Hum Biol. 2021;43:101042. doi:10.1016/j.ehb.2021.101042
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
