Back to Journals » International Journal of General Medicine » Volume 15
A Decrease in Hb and Hypoproteinemia: Possible Predictors of Complications in Neonates with Late-Onset Sepsis in a Developing Country
Authors Cai N, Liao W, Chen Z, Tao M, Chen S
Received 5 April 2022
Accepted for publication 28 July 2022
Published 13 August 2022 Volume 2022:15 Pages 6583—6589
DOI https://doi.org/10.2147/IJGM.S369550
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Na Cai, Wei Liao, Zhiqiang Chen, Min Tao, Sheng Chen
Department of Pediatrics, The First Hospital Affiliated to Army Medical University, Chongqing, 400038, People’s Republic of China
Correspondence: Min Tao; Sheng Chen, Department of Pediatrics, The First Hospital Affiliated to Army Medical University, Chongqing, 400038, People’s Republic of China, Tel +86-23-68766215 ; +86-23-68766213, Email [email protected]; [email protected]
Objective: The main purpose of our study was to determine the predictors of complications in neonates with late-onset sepsis (LOS).
Materials and methods: This was a retrospective cohort study conducted in a neonatal intensive care unit between June 2016 and February 2020. Neonates with LOS were enrolled in this study. According to whether complications were merged after LOS, neonates were divided into a complicated group and a noncomplicated group. The demographic data, perinatal conditions, blood cell count analysis, blood cultures, hypoproteinemia within 1 week after the onset of sepsis and treatment measures were compared between the groups.
Results: A total of 87 neonates with LOS were enrolled in this study. Significant differences were observed between the complicated and noncomplicated groups with regard to hemoglobin (Hb), a decrease in Hb, hypoproteinemia and red blood cell transfusions (P < 0.05). Further comparison found that neonates with LOS who had moderate or severe anemia at the time of sepsis onset were more likely to have complications than those with mild or no anemia. The results of binomial stepwise logistic regression suggested that a decrease in Hb (OR=0.045, P=0.025 < 0.05) and hypoproteinemia (OR=0.266, P=0.007 < 0.05) were independent predictors of complications in neonates with LOS. A receiver operating characteristic analysis showed that the area under the curve was 0.807 for a decrease in Hb.
Conclusion: A decrease in Hb and hypoproteinemia were independent predictors of complications and may help to predict the occurrence of complications in neonates with LOS in the early stage.
Keywords: sepsis, complications, hemoglobin, anemia, decrease in Hb, hypoalbuminemia
Introduction
Neonatal sepsis (NS) is one of the most common infectious diseases with high morbidity and mortality in newborns and remains the third major cause of neonatal death, especially in developing countries.1,2 Sepsis can cause many diseases, such as septic shock, neonatal necrotizing enterocolitis (NEC), meningitis, and osteomyelitis.3 The occurrence of these diseases not only increases the mortality of newborns but also causes short-term and long-term sequelae, such as intestinal stenosis, short bowel syndrome, and neurological and skeletal system sequelae,4–6 seriously affecting the quality of newborns’ lives. Therefore, exploring the predictors of complications of NS will help to develop targeted prevention measures to reduce the incidence of complications and mortality. To date, there are many studies on the severity and prognosis of sepsis all over the world, but very few studies on the predictors of complications of NS, especially quantitative indicators, have been conducted. Hence, we hoped that through this study, we could obtain quantitative indicators that are easy to obtain in clinical practice to predict the occurrence of complications, with a view of reducing the incidence of complications and providing new clues for optimizing treatment strategies in the early clinical stage.
Methods
Study Subjects
This was a retrospective cohort study conducted in the neonatal intensive care unit (NICU). Neonates with LOS (age > 3 days) diagnosed by a neonatal specialist at the First Hospital Affiliated to Army Medical University, China between June 2016 and February 2020 were included. According to whether complications occurred after LOS, neonates were divided into complicated and noncomplicated groups. The exclusion criteria were as follows: (1) intrauterine infection leading to early-onset sepsis (neonates aged ≤ 3 days);7 (2) genetic metabolic diseases (newborns screened for genetic metabolism 3 days after birth);8 (3) Hb reduction caused by intracranial hemorrhage, gastrointestinal hemorrhage, or pulmonary hemorrhage; and (4) a decrease in Hb caused by iatrogenic blood drawing.
This study was approved by the Ethics Committee of the First Hospital Affiliated of Army Medical University (KY2020065). All procedures were carried out according to the Declaration of Helsinki.
Clinical Definitions
The diagnostic criteria for LOS referred to the guidelines for the expert consensus on the diagnosis and management of neonatal sepsis (version 2019) revised by the Chinese Medical Association.7 The diagnostic criteria for LOS were as follows: infants with fever or a low body temperature; infants with less crying; infants with a poor response and feeding; and infants with other clinical manifestations of sepsis. Additionally, the blood cultures or sterile body cavities of infants with LOS showed cultured pathogenic bacteria. Alternatively, infants diagnosed with LOS had the above clinical manifestations and at least two of the following: ① Blood cell count analysis showing a white blood cell (WBC) count < 5 × 109/L, or an increased WBC count (for infants aged ≤ 3 d, a WBC count > 25 × 109/L; for infants aged > 3 d, a WBC > 20 × 109/L); ② Cell classification showing immature neutrophils/total neutrophils (I/T) ≥ 0.16; ③ A platelet count (PLT) < 100 × 109/L; or ④ A C-reactive protein (CRP) level ≥ 8 mg/L. Complications caused by LOS include septic shock, NEC, meningitis, osteomyelitis, and diffuse intravascular coagulation (DIC). For the diagnosis of complications, refer to the fourth edition of Practical Neonatology.3 A hemoglobin (Hb) level < 145 g/L in the neonatal period is considered anemia; 144–120 g/L is considered mild anemia; - 90 g/L is considered moderate anemia; - 60 g/L is considered severe anemia, and < 60 g/L is considered extremely severe anemia.9 The diagnostic criterion for hypoproteinemia was a serum albumin (Alb) level < 25 g/L.10
Data Collection
Demographic data were obtained from electronic medical records and included the mother’s prenatal condition, such as whether there was premature rupture of membranes, amniotic fluid meconium contamination, maternal hypertension or diabetes. Additionally, the information of neonates, such as sex, gestational age, birth weight, age of onset, comorbidities, blood cell count analysis, blood cultures, a decrease in albumin within 1 week after the onset of LOS and treatment measures (after the occurrence of LOS and before the occurrence of complications), was also recorded. When patients first showed symptoms of LOS (such as fever, poor response and poor feeding), the blood samples were collected for the first time and were examined. Laboratory parameters such as WBCs, PLTs, Hb, a decrease in Hb, red blood cell distribution width (RDW), blood culture and albumin were measured. The decrease in Hb was calculated as follows: the most recent Hb level before LOS - The Hb level at the early stage of LOS.
Statistical Analysis
SPSS 20.0 was used for statistical analysis. Continuous variables with a nonnormal distribution are reported as median interquartile range (IQR) percentiles and were compared using Mann–Whitney U-tests. Categorical variables are presented as absolute numbers and percentages. Differences in categorical variables were assessed for significance using the chi-square test and Fisher’s exact test. Multivariate logistic regression analysis was used to assess the independent predictors of complications in neonates with LOS. The receiver operating characteristic (ROC) method was used. The sensitivity and specificity were compared by analyzing the area under the ROC curve. P < 0.05 was considered significant.
Results
Comparison of General Data Between the Two Groups
A total of 87 neonates with LOS were included, with 56 in the noncomplicated group and 31 in the complicated group, including 14 cases of NEC, 6 cases of septic shock, 8 cases of meningitis, 2 cases of osteomyelitis, and 1 case of DIC. The demographic characteristics of the two groups are presented in Table 1, including the sex, gestational age, birth weight, age of onset, perinatal situation, comorbidities, etc. The results showed that there were no significant differences in these data between the complicated and noncomplicated groups (P > 0.05).
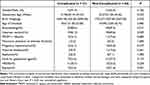 |
Table 1 The Baseline Clinical Characteristics of the Complicated and Non-Complicated Group |
Significant Differences in Hb Levels, Decreases in Hb, Hypoproteinemia and Red Blood Cell Transfusions
We collected the most recent Hb level before LOS and the interval between two Hb collections (the most recent Hb level before LOS and the Hb level at the early stage of LOS). There were no differences in the most recent Hb level before LOS or the sample collection interval between the two groups. Additionally, we calculated the amount of venous blood collection in the early stage of LOS in the two groups to avoid decreases in Hb caused by iatrogenic blood collection. There was no significant difference in venous blood collection between the two groups. The decrease in Hb was calculated as follows: the most recent Hb level before LOS – the Hb level at the early stage of LOS. Significant differences were observed between the complicated and noncomplicated groups with regard to Hb, decreases in Hb, hypoproteinemia within 1 week after the onset of sepsis and red blood cell transfusions (P < 0.05, Table 2). Further analysis of the impact of different degrees of anemia on the incidence of complications suggested that neonates with moderate or severe anemia were more likely to have complications than those with mild or no anemia (P < 0.05, Table 3).
 |
Table 2 Comparison of Laboratory Indicators and Treatment Measures Between the Two Groups |
 |
Table 3 Comparison of the Severity of Anemia Between the Two Groups |
A Decrease in Hb and Hypoproteinemia Were Independent Predictors of Complications in Neonates with LOS
Binomial stepwise logistic regression was used with the occurrence of complications as the dependent variable, and the above statistically significant indicators, including Hb, a decrease in Hb, hypoproteinemia and red blood cell transfusions, were used as independent variables to test whether each factor had a significant effect on the occurrence of complications. The results suggested that a decrease in Hb (OR=0.045, P=0.025<0.05) and hypoproteinemia (OR=0.266, P=0.007<0.05) were independent predictors of complications in neonates with LOS (Table 4).
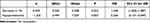 |
Table 4 Logistic Regression Analysis Results |
The High Predictive Value of a Decrease in Hb for Complications in Neonates with LOS
The receiver operating characteristic (ROC) analysis of LOS showed that the area under the curve (AUC) was 0.807, suggesting that a decrease in Hb may help to predict the occurrence of complications in neonates with LOS (Table 5, Figure 1).
 |
Table 5 The ROC Curve of the Decrease in Hb for Predicting Complication in Sepsis |
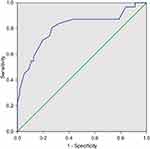 |
Figure 1 The ROC curve of a decrease in Hb for predicting complications in neonates with LOS. Abbreviations: ROC, receiver operating characteristic; Hb, hemoglobin; LOS, late-onset sepsis. |
Discussion
The neonatal immune system is immature, highly susceptible to many microorganisms and prone to sepsis, especially in premature infants and low birth weight infants. Long-term use of invasive procedures and intravenous nutrition increases the incidence of sepsis. Due to the low immunity and weak resistance of newborns, sepsis often develops rapidly from subclinical symptoms to severe systemic infection symptoms, causing damage to systemic organs and the occurrence of diseases such as NEC, meningitis, septic shock, and DIC, making sepsis an important cause of neonatal death.11 Therefore, it is of great significance to analyze the specific risk factors for complications and death from sepsis, taking active control measures to reduce the incidence of complications and mortality.
Our study found that there were significant differences in Hb levels, decreases in Hb, hypoproteinemia within 1 week after the onset of LOS and red blood cell transfusions between the complicated group and the noncomplicated group. Further logistic regression showed that a decrease in Hb and hypoproteinemia were independent predictors of complications in neonates with LOS. Regrettably, no study has focused on the relationship between decreases in Hb and hypoproteinemia and complications in neonates with LOS. As such, our current study is unique in that it mainly focused on a predictive approach to complications in neonates with LOS, which may be a possible predictor of complications.
The Effect of a Decrease in Hb on the Complications and Prognosis of Neonates with LOS
Our study found that sepsis is often accompanied by a decrease in Hb. Some patients may develop anemia, while others only have a decrease in Hb, which does not meet the diagnostic criteria for anemia. Many causes can lead to a decrease in Hb, such as iatrogenic blood loss, reduced serum iron levels, and shortened red blood cell life span and increased destruction.12–14 In addition, vascular endothelial glycocalyx shedding and intravenous fluid administration lead to blood thinning,15–17 which is also manifested by a decrease in Hb. After the occurrence of sepsis, the body may have microcirculation disturbances, leading to tissue ischemia and hypoxia. When severe infection occurs, a large amount of inflammatory factors are secreted in the body, which leads to a decrease in Hb through various mechanisms. The significant reduction in Hb further causes ischemia and hypoxia and the redistribution of blood in the body, causing or aggravating microcirculation disorders. Eventually, sepsis and significantly reduced Hb complement each other and cause adverse effects on tissue organs. We speculate that the decrease in Hb may reflect the level of inflammation in the body. Jung SM18 found that low hemoglobin levels (< 9.0 g/dL) were observed in approximately 20% of patients with septic shock, and the severity of the decrease in these levels correlated with mortality; the lower the Hb level was, the higher the mortality rate. In addition, this study found that the incidence of complications in neonates with LOS was closely related to the severity of anemia caused by a decrease in Hb. Patients with moderate or severe anemia caused by a decrease in Hb were more likely to have complications. Additionally, this study found that after the occurrence of sepsis and before the occurrence of complications, the transfusion of red blood cells may increase the incidence of complications. Many studies have also shown that the transfusion of red blood cells can lead to the occurrence of NEC,19,20 increase the chance of surgery in children with NEC and reduce the survival rate.21 A foreign study on blood transfusion after sepsis onset in children showed that after sepsis-related anemia, compared to the restrictive strategy group, there was a significantly higher incidence of acute respiratory distress syndrome and acute lung injury in the liberal transfusion group. Moreover, mortality was significantly higher, and liberal transfusion might be associated with a worse outcome.22 In addition, other studies found that the transfusion of red blood cells may increase the mortality of critically ill patients.23,24 It should be pointed out that the decrease in Hb may sometimes be caused by blood dilution related to fluid load.17,25 Therefore, after the occurrence of sepsis, even if Hb is reduced, it is necessary to strictly grasp the blood transfusion pointer and carefully infuse red blood cells.
Further logistic regression showed that a decrease in Hb was an independent predictor of complications in neonates with LOS. By comparing the ROC curves of decreases in Hb, the results showed that the AUC was 0.807 for decreases in Hb, which suggests that a decrease in Hb (cutoff value: 14.5) may help to predict the occurrence of complications in neonates with LOS.
The Effect of Hypoproteinemia on the Complications and Prognosis of Neonates with LOS
This study found that the incidence of hypoproteinemia in the complicated group was significantly higher than that in the noncomplicated group. Logistic regression showed that hypoproteinemia was an independent predictor of complications in neonates with LOS. Albumin can be reduced by approximately 10–15 g/L within 1 week after sepsis. After infection, a large number of inflammatory mediators, such as interleukin-1 (IL-1), IL-6 and tumor necrosis factor-α, are released, which can inhibit albumin synthesis. In addition, when children have sepsis, they will have fever, stress and inflammation. These symptoms will accelerate metabolism, and a large amount of albumin in the body will quickly synthesize acute-phase protein, causing the albumin level to drop.26 Additionally, increased permeability and the destruction of vascular endothelial integrity can also lead to hypoalbuminemia.10 Hypoproteinemia can cause the plasma colloid osmotic pressure to drop, and a large amount of fluid remains in the tissue gap, which reduces the effective blood volume of the body and causes damage to multiple organ functions. In addition, albumin can clear free radicals in the body and inhibit the production of oxygen free radicals by multinuclear cells. However, when sepsis occurs, a large number of inflammatory factors are secreted, leading to proinflammatory and anti-inflammatory imbalances in the body; the activity of free radicals is uncontrolled, and a large number of free radicals are produced. The occurrence of hypoalbuminemia leads to a weakening of the body’s ability to scavenge free radicals and promotes the development of sepsis. Therefore, it is necessary to pay attention to children with hypoalbuminemia after the occurrence of infection. For those with sepsis complicated with hypoalbuminemia, hypoalbuminemia should be actively corrected to reduce the incidence of complications.
Limitations
This study has some limitations. First, this study was retrospective, and the data were not available for all variables and were reliant on what was captured by the treating physician. Second, there was a limitation in using the logistic regression model to explore associations since the relationship between covariates can be nonlinear, and the limitations of the current study in adjusting for confounding factors may have had an impact on the results.
Conclusion
A careful analysis of decreases in Hb and hypoproteinemia within 1 week after LOS, which is an easily accessible and affordable tool, may help to predict the occurrence of complications in neonates with LOS in the early stage.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (Grant/Award Number: 82170565).
Disclosure
The authors declare that there are no conflicts of interest.
References
1. Shane AL, Sánchez PJ, Stoll BJ. Neonatal sepsis. Lancet. 2017;390:1770–1780. doi:10.1016/S0140-6736(17)31002-4
2. Zea-Vera A, Ochoa TJ. Challenges in the diagnosis and management of neonatal sepsis. J Trop Pediatr. 2015;61:1–13. doi:10.1093/tropej/fmu079
3. Shao XM, Ye HM, Qiu XS. Practical Neonatology.
4. Neu J, Pammi M. Pathogenesis of NEC: impact of an altered intestinal microbiome. Semin Perinatol. 2017;41:29–35. doi:10.1053/j.semperi.2016.09.015
5. Frost BL, Modi BP, Jaksic T, Caplan MS. New medical and surgical insights into neonatal necrotizing enterocolitis: a review. JAMA Pediatr. 2017;171:83–88. doi:10.1001/jamapediatrics.2016.2708
6. Wadhawan R, Oh W, Hintz SR, et al. Neurodevelopmental outcomes of extremely low birth weight infants with spontaneous intestinal perforation or surgical necrotizing enterocolitis. J Perinatol. 2014;34:64–70. doi:10.1038/jp.2013.128
7. Subspecialty Group of Neonatology, the Society of Pediatric, Chinese Medical Association; Professional Committee of Infectious Diseases, Neonatology Society, Chinese Medical Doctor Association. Expert consensus on the diagnosis and management of neonatal sepsis (version 2019). Zhong hua Er Ke Za Zhi. 2019;57(4):252–257.
8. Zhao YH, Zhang WY, Wang T, Zhao Q, Wang Y. Values of procalcitionin and red blood cell distribution width in evaluating severity and prognosis of septicemia in preterm infants. Chin J Perinat Med. 2019;22(9):641–647.
9. Wang WP. Pediatrics.
10. Gatta A, Verardo A, Bolognesi M. Hypoalbuminemia. Intern Emerg Med. 2012;7(Suppl 3):S193–199. doi:10.1007/s11739-012-0802-0
11. Reyes A. Ending the culture of culture-negative sepsis in the neonatal ICU. Rev Chilena Infectol. 2018;35:216–217. doi:10.4067/s0716-10182018000200216
12. Keel SB, Abkowitz JL. The microcytic red cell and the anemia of inflammation. Br Med J. 2009;2(2296):1773–1774.
13. Kempe DS, Akel A, Lang PA, et al. Suicidal erythrocyte death in sepsis. J Mol Med. 2007;85(3):273–281. doi:10.1007/s00109-006-0123-8
14. van Eijk L, Kroot J, Tromp M, van der Hoeven J, Swinkels D, Pickkers P. Inflammation-induced hepcidin-25 is associated with the development of anemia in septic patients: an observational study. Crit Care. 2011;15(1):R9. doi:10.1186/cc9408
15. Steppan J, Hofer S, Funke B, et al. Sepsis and major abdominal surgery lead to flaking of the endothelial glycocalix. J Surg Res. 2011;165:136–141. doi:10.1016/j.jss.2009.04.034
16. Marechal X, Favory R, Joulin O, et al. Endothelial glycocalyx damage during endotoxemia coincides with microcirculatory dysfunction and vascular oxidative stress. Shock. 2008;29:572–576. doi:10.1097/SHK.0b013e318157e926
17. Jansma G, de Lange F, Kingma WP, et al. ‘Sepsis-related anemia’ is absent at hospital presentation: aretrospective cohort analysis. BMC Anesthesiol. 2015;15:55. doi:10.1186/s12871-015-0035-7
18. Jung SM, Kim YJ, Ryoo SM, Kim WY. Relationship between low hemoglobin levels and mortality in patients with septic shock. Acute Crit Care. 2019;34:141–147. doi:10.4266/acc.2019.00465
19. Teišerskas J, Bartašienė R, Tamelienė R. Associations between red blood cell transfusions and necrotizing enterocolitis in very low birth weight infants: ten-year data of a tertiary neonatal unit. Medicina. 2019;55:16. doi:10.3390/medicina55010016
20. Cunningham KE, Okolo FC, Baker R, Mollen KP, Good M. Red blood cell transfusion in red blood cell transfusion in premature infants leads to worse necrotizing enterocolitis outcomes. J Surg Res. 2017;213:158–165. doi:10.1016/j.jss.2017.02.029
21. Sayari AJ, Tashiro J, Sola JE, Perez EA. Blood transfusions, increased rates of surgical NEC, and lower survival: a propensity score-matched analysis. J Pediatr Surg. 2016;51:927–931. doi:10.1016/j.jpedsurg.2016.02.052
22. Elshinawy M, Kamal M, Nazir H. Sepsis-related anemia in a pediatric intensive care unit: transfusion‐associated outcomes. Transfusion. 2020;60(Suppl 1):S4–S9. doi:10.1111/trf.15688
23. Chacko J, Brar G. Red blood cell transfusion thresholds in critically ill patients. Indian J Crit Care Med. 2019;23(Suppl 3):S181–S184. doi:10.5005/jp-journals-10071-23248
24. Cable CA, Razavi SA, Roback JD, Murphy DJ. RBC transfusion strategies in the ICU: a concise review. Crit Care Med. 2019;47:1637–1644. doi:10.1097/CCM.0000000000003985
25. Weiss G, Ganz T, Goodnough LT. Anemia of inflammation. Blood. 2019;133:40–50. doi:10.1182/blood-2018-06-856500
26. Yang CY, Li BY, Xu P, Yang YJ, Yang QZ. Correlation of serum albumin with the clinical features and prognosis of preterm neonates in the neonatal intensive care unit. Clin Exp Obstet Gynecol. 2016;43:149–153. doi:10.12891/ceog2044.2016
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
