Back to Journals » Neuropsychiatric Disease and Treatment » Volume 11
A cross-sectional study on anxiety and stress in pregnant women with chronic HBV infection in the People’s Republic of China
Authors Zhou F, Li J, Lin K, Ji P, Sun Y
Received 14 May 2015
Accepted for publication 14 July 2015
Published 25 August 2015 Volume 2015:11 Pages 2225—2232
DOI https://doi.org/10.2147/NDT.S88602
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Wai Kwong Tang
Fen Zhou,1 Jianju Li,2 Keke Lin,1 Ping Ji,1 Yumei Sun1
1School of Nursing, Peking University, 2Infection Control Department, Beijing Ditan Hospital, Capital Medical University, Beijing, People’s Republic of China
Purpose: To investigate the anxiety and pregnancy-associated stress of pregnant women with chronic hepatitis B virus (HBV) infection in the People’s Republic of China and analyze the relationship between anxiety and pregnancy-associated stress in the hope of finding ways to reduce the stress or improve the coping skills for these mothers-to-be during pregnancy.
Methods: A cross-sectional study was conducted. One hundred and sixty chronic HBV-infected pregnant women (HBV group) and 160 healthy pregnant women (control group) selected from three Peking University-affiliated hospitals participated in the study, and completed the State-Trait Anxiety Inventory (STAI) and Pregnancy Stress Rating Scale (PSRS) survey.
Results: The mean scores of STAI and PSRS for the HBV group were higher than for the control group. Factor 2 of PSRS (stress caused by worrying about mother and child’s health and safety) was the highest, and was significantly higher in the HBV group than in the control group. Correlation analysis showed STAI scores were significantly correlated with economic status and diagnosis, as well as the total score, factor 1 (stress about identifying with the role of mother), and factor 2 of PSRS, but not significantly correlated with factor 3 of PSRS (stress caused by the changes of body shape and physical activity).
Conclusion: Pregnant women with chronic HBV infection experienced higher levels of anxiety and stress than healthy pregnant women. Their major stress came from concerns for the health and safety of the mother and the child.
Keywords: anxiety, pregnancy-associated stress, chronic HBV infection, State-Trait Anxiety Inventory, Pregnancy Stress Rating Scale
Introduction
Childbirth is a monumental moment for a mother. The moment a woman becomes pregnant, a miraculous journey to motherhood begins. This period is characterized by waves of physiological and psychological changes; understandably, many expecting mothers experience anxiety and stress in the process,1–3 and anxiety appears to occur very commonly during pregnancy.3
Over the years, researchers have examined how anxiety affects pregnancy and its outcomes. It has been shown that antenatal anxiety is a major predictor of postpartum depression4,5 and parenting stress6 for the mother, as well as adverse obstetric, fetal, and neonatal outcomes.7,8 When the expecting mother experiences high anxiety levels during pregnancy, the child is more likely to have intrauterine growth restriction, to be born prematurely, or to have low birth weight;9–12 even if the child is born at term with no complications, the child will still have a high risk of having non-optimal neuromotor development13 and less perceptual/social competency.14 There is a study showing that higher levels of antenatal anxiety worsen the quality of maternal–fetal attachment and induce negative attitudes toward motherhood and self-image as a mother,15 hence further endangering the already delicate mother–child relation. Pregnancy-related anxiety, therefore, is a serious issue.
Women of childbearing age in the People’s Republic of China (PRC) seem to have even more to worry about when it comes to pregnancy. Diseases, especially the diseases that can be transmitted vertically to the child from the mother, such as hepatitis B virus (HBV) infection, are of particular concern to pregnant women. The PRC is a country with a high epidemic rate of HBV infection. According to a nationwide HBV epidemiological survey in 2006,16 the hepatitis B surface antigen (HBsAg) carrier rate was 7.18% among the population aged 1–59 years and 8.57% among ages 15–59 years. These data indicate that approximately 93 million people in the PRC are infected with HBV. While the country has devoted efforts to educate the public about HBV, the disease remains a stigma in the society. Hence, when a chronic HBV-infected woman becomes pregnant in the PRC, it is expected that her anxiety level will rise significantly.
Studies reveal that pregnant women who are HBsAg carriers have increased risks of hepatitis flares,17,18 and their fetuses are more likely to develop congenital malformations, have low birth weight, and have other adverse perinatal outcomes.19,20 Vertical transmission of the virus from mother to child is also highly possible. Thus, most studies about pregnant women with chronic HBV infection focus on ways to block mother-to-child transmission, “such as administrating standard passive-active immunoprophylaxis with hepatitis B immunoglobulin and hepatitis B vaccine”,21 and findings suggest that the prophylaxis failure rate can be as high as 10%–15%.21,22 Infection with HBV in infancy or early childhood may lead to a high rate of persistent infection (25%–90%).23 It is speculated that high anxiety levels might play a role in prophylaxis failure and persistent infection. Therefore, pregnant women with chronic HBV infection not only have to adjust themselves to progressive weight gain and physiological changes, but they also have heavy psychological burdens to carry. However, there are few studies focused on exploring the sources of concerns and the anxiety levels in these women. Hence, it is critical to direct attention to pregnant women with chronic HBV infection and examine their anxiety sources in the hopes of achieving a desirable pregnancy outcome.
The objective of this study was to investigate anxiety and stress experienced by pregnant women with chronic HBV infection in the PRC with the State-Trait Anxiety Inventory (STAI) and Pregnancy Stress Rating Scale (PSRS) survey. STAI is a widely used tool to assess anxiety in pregnant women at a particular time point, and is a validated and straightforward way for research subjects to participate with ease.14,24–27 It was introduced into the PRC in 1988,28 and acceptable validity and reliability has been reported in various populations in the PRC.28 However, STAI cannot reveal what pregnant women are anxious about. Fortunately, PSRS is able to fill this gap. PSRS was developed in Taiwan by Chen et al in 1983,29 and has been recently revised and revalidated.30 It aims to rate incidences and severity of stressors associated with pregnancy.31 PSRS was introduced to Mainland PRC by Pan et al in 2003,32 and it has been shown to have high reliability and validity.32,33 Since then, the scale has been used in various studies to measure pregnancy-associated stress.34,35
Methods
Design and participants
A cross-sectional survey was conducted in two groups of pregnant women, an HBV group carrying chronic HBV infection and a control group of healthy pregnant women. Participants in both groups were selected through a convenience sampling method. The HBV group included 160 pregnant women with chronic HBV infection from the outpatient unit of the Department of Obstetrics at Beijing Ditan Hospital, PRC (180 patients were initially assessed for eligibility, but only 160 finished the study), and the control group included 160 pregnant women without HBV infection or other illnesses from the outpatient units of the Departments of Obstetrics at Peking University First Hospital and Peking University Third Hospital in Beijing, PRC (173 patients were initially assessed for eligibility, but only 160 finished the study). Please refer to Figure 1 for details regarding the study design and a flow diagram of the study process.
  | Figure 1 Flow diagram of the study design. |
The inclusion criteria for the HBV group were: 1) clinically diagnosed with chronic HBV infection for at least 6 weeks; 2) suitable for pregnancy (health status after the pregnancy will not be deteriorated due to burden on liver) and decided to proceed with pregnancy at the discretion of their physician; and 3) no communication barrier and willing to participate in the study. The exclusion criterion was a history of multiple pregnancies.
The inclusion criteria for the control group were: 1) tested negative with HBsAg and hepatitis B e antigen (HBeAg); 2) healthy; 3) suitable for pregnancy and decided to proceed with pregnancy on the advice of their physician; and 4) no communication barrier and willing to participate in the study. The exclusion criterion was a history of multiple pregnancies.
Questionnaires
The questionnaires included the Chinese-version STAI and PSRS. STAI consists of 20 items. Each item is scored from 1–4. The total scores range from 20–80. STAI Cronbach’s α was 0.93 in this study. PSRS was used to measure the incidence and severity of stressors associated with pregnancy. The scale consists of 30 items and can be divided into three factors: factor 1 is about the stress about identifying with the role of mother (15 items); factor 2 is about the stress caused by worrying about mother and child’s health and safety (eight items); and factor 3 is about the stress caused by the changes of body shape and physical activity (four items). The remaining three items contribute to the total score and cannot be classified in any factor. Each item scores from 0–3. The average score measures the severity of stress: 0 means the mother experiences no stress; 0.001–1 means the mother experiences a mild level of stress; 1.001–2 means the mother experiences a moderate level of stress; and 2.001–3 means the mother experiences a severe level of stress. The Cronbach’s α for the PSRS total score was 0.89 and for each factor was 0.70–0.88.
Sociodemographic data (age, educational level, economic status) and pregnancy data (planned pregnancy or not, gestational period) were collected from all participants. Medical diagnosis (carrier or chronic hepatitis B) and the latest HBV viral load were obtained from each HBV group participant’s medical record.
Procedure
This study was approved by the Ethics Committee of Beijing Ditan Hospital, Capital Medical University. After reviewing the medical records of desirable candidates for the study, the subjects who met the criteria and were eligible and willing to participate in the study were invited to fill out the questionnaires. The researchers explained the aims and the content of the study and ensured confidentiality for each participant. After participants agreed to volunteer and signed the written consent forms to join the study, they proceeded to complete the questionnaires.
Data analysis
The raw data were analyzed using SPSS 13.0. Independent Student’s t-tests and chi-square tests were used to compare sociodemographic and pregnancy data and STAI scores between the HBV group and the control group. The Mann–Whitney U-test was used to compare PSRS scores between the HBV group and the control group. For the HBV group, Spearman’s correlation was used to examine the relationships between STAI and sociodemographic, pregnancy, and infection characteristics and pregnancy-associated stress. All tests were two-tailed, with P<0.05 considered to be significant.
Results
Description of participants
The ages of the 160 chronic HBV-infected pregnant women were from 21–37 years, and the mean age was 28.13 (SD 3.40) years. The ages of the 160 healthy pregnant women were from 21–38 years, and the mean age was 28.36 (SD 3.62) years. There was no significant difference in age between the HBV group and control group (t=0.589, P=0.556). There were also no significant differences in education level, economic status, gestational period, and desired pregnancy or not between the HBV group and control group (Table 1).
  | Table 1 Characteristics of pregnant women in the HBV group and control group |
Of the 160 chronic HBV-infected pregnant women, 121 were HBV carriers and 39 had chronic hepatitis B; 110 of them were HBeAg-positive. The geometric mean of HBV viral load was 1.5×104 (SD 7×102; range from undetectable to 5.0×108).
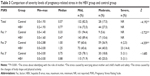
Comparison of the pregnancy-associated stress between the two groups
The total and factor scores of PSRS in the two groups are shown in Table 2. For the two groups, the score of factor 2, the stress caused by worrying about mother and child’s health and safety, was the highest, and next came factor 3, the stress caused by the changes of body shape and physical activity. The score of factor 1, the stress about identifying with the role of mother, was the lowest (Table 2).
  | Table 2 Comparison of PSRS scores between the HBV group and control group |
The Mann–Whitney test showed the total score and the scores of factor 1 and factor 2 of PSRS for the HBV group were significantly higher than those of the control group, whereas there was no statistically significant difference (P>0.05) in factor 3 between the two groups (Table 2).
The HBV group had more women with moderate and severe stress than the control group. The Mann–Whitney test showed that there were significant differences in the total score and the scores of factor 1 and factor 2 of PSRS between the two groups (P<0.05), while there was no statistically significant difference (P>0.05) in factor 3 between the two groups (Table 3).
Comparison of the anxiety between the two groups
The mean STAI score of the pregnant women in the HBV group was 44.42 (SD 10.70), while that of the pregnant women in the control group was 36.52 (SD 9.62). The two independent samples Student’s t-test showed that there was a significant difference in the state anxiety score between the two groups (t=6.943, P<0.001).
Correlation analysis
For the HBV group, Spearman’s correlation analysis was conducted to examine the relationships of STAI with sociodemographic, pregnancy, and infection variables. The results showed that STAI was positively correlated with economic status (r=0.226, P<0.01) and diagnosis (r=0.216, P<0.01). No significant relationships were found between STAI and other sociodemographic, pregnancy, or infection variables (P>0.05).
For the HBV group, Spearman’s correlation analysis also showed that STAI was positively correlated with the total (r=0.427, P<0.001), factor 1 (r=0.340, P<0.001), and factor 2 (r=0.439, P<0.001) scores of PSRS, but not significantly correlated with the factor 3 score of PSRS (r=0.140, P=0.077). For the control group, Spearman’s correlation analysis showed similar findings: STAI was significantly positively correlated with the total (r=0.350, P<0.001), factor 1 (r=0.294, P<0.001), and factor 2 (r=0.358, P<0.001) scores of PSRS, but not significantly correlated with the factor 3 score of PSRS (r=0.136, P=0.087).
Discussion
Pregnancy-associated stress in women with chronic HBV infection needs attention
The results of this study show that the total, factor 1 (stress about identifying with the role of mother), and factor 2 (stress caused by worrying about mother and child’s health and safety) scores of PSRS were significantly higher in the HBV group than in the control group. Moreover, the study found that the HBV group reported a higher level of anxiety than the control group (P<0.01), which is consistent with the results of a study using the Hamilton Anxiety Scale for late-pregnancy women with positive HBsAg.36 Our present study indicated that women with chronic HBV infection experience greater psychological stress than healthy women during pregnancy. It has been shown that a high level of stress during pregnancy is strongly correlated with adverse pregnancy outcomes. For example, it has been shown that maternal stress had detrimental consequences on pregnancy and birth outcomes – in particular, shortened gestation and increased risk of preterm birth. On the contrary, maternal positive affect during pregnancy is associated with beneficial consequences in terms of increased length of gestation and reduced risk of preterm birth.37 The anxiety of pregnant women during pregnancy has been shown to weaken the newborn’s response to pain and to have negative effects on the development of newborns’ nervous systems.38 Prenatal anxiety in pregnant women has also been shown to alter adaptive immunity in the infant.39 It is therefore critical for medical professionals to be aware of psychological stress for pregnant women with chronic HBV infection.
Characteristics of the psychological stress in pregnant women with chronic HBV infection
Worries about the health and safety of the mother and the child
This study revealed that the health and safety of the mother and the child was the primary concern for pregnant women in both the HBV group and the control group. Women in both groups scored highest in issues related to health concerns of the mother or the child (factor 2), and especially for the child (Table 2). There were more than 50% of women in the HBV group who expressed a “moderate” or even “severe” stress level (Table 3). This finding supports that worrying about the health and safety of mother and child is one of the most important psychological stressors for pregnant women. Although pregnancy and delivery is a physiological process, it is rare but possible to have some adverse pregnancy outcomes that threaten mother–child health, such as preterm birth, stillbirth, postpartum hemorrhage. However, women in the HBV group expressed even more concerns with the health issues, especially in items like “afraid baby will not be normal”, “worry about safe labor for her child”, and “worry about safe labor for herself”.
For pregnant women with chronic HBV infection, knowing the chance of vertical transmission of HBV, which will make her child be a chronic carrier of the virus, and the possibility of various adverse pregnancy outcomes, are all proven reasons for them to be concerned. Through our clinical observation, those women always repetitively seek counseling, on whether or not and when they are suitable for pregnancy, before planning for pregnancy or after an undesired pregnancy, as well as on effective methods to block mother-to-child transmission before becoming pregnant; they would also monitor the pregnancy more closely, and are more likely to volunteer to be hospitalized when they feel a change in their bodies. Furthermore, exam results (liver functional test and relevant tests in the fetus) are also a contributing stressor: some get insomnia; some of them even ask family members to check the result.
Worries about changes in body shape and in physical activities
Worries about changes in body shape and physical activities appeared to be the second greatest concern of women from both the HBV group and the control group. Women in both groups expressed anxieties about having permanent stretch marks that may alter their body images or gaining too much weight that may turn daily activities into a burden. But since both these items scored low in the PSRS, their significance should not be overestimated.
These results reflect the aesthetic desire in every woman, and that feeling unattractive was a stress factor in the pregnancy journey. It could be speculated that making pregnant women feel attractive, perhaps by means of cosmetic makeup or compliments from husbands or other family members, could lower the stress level.
Worries about identifying with the role of a mother
Whether the pregnancy is planned or not, once a mother has decided to proceed with it, she is prepared to enter parenthood. Hence, the stress about identifying with the role of mother came last in the concern list. Nevertheless, women from the HBV group still showed more concerns than women from the control group; they expressed most concerns in issues like “difficulty deciding the type of infant feeding”, and so on.
This study shows that the average score of the issue about “difficulty deciding the type of infant feeding” was 1.01 (SD 0.94) in the HBV group, while it was 0.25 (SD 0.46) in the control group (P<0.01). Breastfeeding is proven to be beneficial for the mother’s health and the baby’s development. However, HBV can be detected in breast milk from HBV carriers, making breastfeeding a problem for women with HBV infection. Fortunately, a study has shown that immunotherapy prior to delivery is an effective way to block virus from passing through breast milk;40 hence informing women with chronic HBV infection about a prophylactic immunotherapy option could be a solution to reduce stress.
Public education on HBV is a pressing issue. Having identified worries concerning women with chronic HBV infection, it is a medical practitioner’s responsibility to separate incorrect health beliefs from valid health concerns and educate the public with accurate information on HBV, so that women with chronic HBV infection can enjoy a joyful and safe journey to motherhood and the whole family can welcome the arrival of the new baby to the household.
The unsatisfied level of predominant need may be most closely related with anxiety
The greater the stress, and the longer it continues, the higher the level of anxiety which the individual will experience. Both anxiety and psychological stress are subjective feelings. In a stressful situation, anxiety is the most direct response. The results of this study show pregnancy-associated stress was positively correlated with anxiety, which is similar to the results by Zhou et al, who used STAI and PSRS in non-HBV infected pregnant women.35
However, this study also shows that, among the three factors of PSRS, factor 1 and factor 2 were positively correlated with anxiety, while the second highest stress, factor 3, was not. According to Maslow’s needs hierarchy theory,41–44 humans have five basic needs, which are arranged in a hierarchy of prepotency as a pyramid. Unmet needs result in a state of tension or anxiety.44 The physiological needs are filled first. Once these are nearing complete satisfaction, effort is allocated to the next level of the hierarchy, safety, and so on for each of the higher needs. In this study, the stress caused by worrying about mother and child’s health and safety was the highest, and more than 50% of women experienced a moderate or severe level of stress in this factor. This suggests that, for the majority of chronic HBV-infected pregnant women, their physiological and safety needs were not well gratified and remained predominant needs. The stress caused by the changes of body shape and physical activity reflect the need for self-esteem and the esteem of others. The need for self-esteem and the esteem of others is a higher level need. Although the need for self-esteem and the esteem of others was the second highest stress in this study, it was not a predominant need for pregnant women during pregnancy. This study finding suggests that the unsatisfied level of predominant need may be most closely related with anxiety.
Further studies are required to explore the effects of anxiety and psychological stress on pregnancy outcomes through longitudinal studies. Additionally, qualitative studies may be helpful for evaluating the characteristics of the psychological stress.
Conclusion
In this study, we investigated the anxiety and pregnancy-associated stress in women with chronic HBV infection in the PRC compared with healthy pregnant women. The findings show that worrying about the health and safety of mother and child was one of the most important psychological stressors for pregnant women and was positively correlated with anxiety. It may imply that the unsatisfied level of predominant need was most closely related with anxiety. The study also shows chronic HBV-infected pregnant women had higher levels of anxiety and stress than healthy pregnant women. Giving appropriate information and social support may be an effective way to reduce their anxiety about mother and child’s health and safety.
Acknowledgments
The authors thank Dr Yuying Yang and Dr Min Liu at Beijing Ditan Hospital for their help in conducting this study. The authors also thank the nurse managers, Mrs Shiping Su at Peking University First Hospital, and Mrs Luyan Liu at Peking University Third Hospital, for their help with subject recruitment. Most importantly, we thank the pregnant women who participated in the study.
Disclosure
The authors report no conflicts of interest in this work.
References
Lee AM, Lam SK, Sze Mun Lau SM, Chong CS, Chui HW, Fong DY. Prevalence, course, and risk factors for antenatal anxiety and depression. Obstet Gynecol. 2007;110(5):1102–1112. | ||
Faisal-Cury A, Rossi Menezes P. Prevalence of anxiety and depression during pregnancy in a private setting sample. Arch Womens Ment Health. 2007;10(1):25–32. | ||
Andersson L, Sundström-Poromaa I, Wulff M, Aström M, Bixo M. Depression and anxiety during pregnancy and six months postpartum: a follow-up study. Acta Obstet Gynecol Scand. 2006;85(8):937–944. | ||
Austin MP, Tully L, Parker G. Examining the relationship between antenatal anxiety and postnatal depression. J Affect Disord. 2007; 101(1–3):169–174. | ||
Milgrom J, Gemmill AW, Bilszta JL, et al. Antenatal risk factors for postnatal depression: a large prospective study. J Affect Disord. 2008;108(1–2):147–157. | ||
Misri S, Kendrick K, Oberlander TF, et al. Antenatal depression and anxiety affect postpartum parenting stress: a longitudinal, prospective study. Can J Psychiatry. 2010;55(4):222–228. | ||
Alder J, Fink N, Bitzer J, Hösli I, Holzgreve W. Depression and anxiety during pregnancy: a risk factor for obstetric, fetal and neonatal outcome? A critical review of the literature. J Matern Fetal Neonatal Med. 2007;20(3):189–209. | ||
Wang WJ, Cui YY, Wang DP, He P. Probe into the correlativity between abnormal psychological status in pregnant women and their perinatal outcomes. Maternal and Child Health Care of China. 2006;21(16):2214–2216. | ||
Field T, Diego M, Hernandez-Reif M, et al. Chronic prenatal depression and neonatal outcome. Int J Neurosci. 2008;118(1):95–103. | ||
Hosseini SM, Biglan MW, Larkby C, Brooks MM, Gorin MB, Day NL. Trait anxiety in pregnant women predicts offspring birth outcomes. Paediatr Perinat Epidemiol. 2009;23(6):557–566. | ||
Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012–1024. | ||
Rahman A, Bunn J, Lovel H, Creed F. Association between antenatal depression and low birthweight in a developing country. Acta Psychiatr Scand. 2007;115(6):481–486. | ||
van Batenburg-Eddes T, de Groot L, Huizink AC, et al. Maternal symptoms of anxiety during pregnancy affect infant neuromotor development: the generation R study. Dev Neuropsychol. 2009;34(4):476–493. | ||
Figueiredo B, Pacheco A, Costa R, Conde A, Teixeira C. Mother’s anxiety and depression during the third pregnancy trimester and neonate’s mother versus stranger’s face/voice visual preference. Early Hum Dev. 2010;86(8):479–485. | ||
Hart R, McMahon CA. Mood state and psychological adjustment to pregnancy. Arch Womens Ment Health. 2006;9(6):329–337. | ||
Chinese Center for Disease Control and Prevention [homepage on the Internet]. Available at http://www.chinacdc.cn/dcbg/200804/t20080423_34870.htm. Accessed May 14, 2015. | ||
ter Borg MJ, Leemans WF, de Man RA, Janssen HL. Exacerbation of chronic hepatitis B infection after delivery. J Viral Hepat. 2008;15(1):37–41. | ||
Tan HH, Lui HF, Chow WC. Chronic hepatitis B virus (HBV) infection in pregnancy. Hepatol Int. 2008;2(3):370–375. | ||
Safir A, Levy A, Sikuler E, Sheiner E. Maternal hepatitis B virus or hepatitis C virus carrier status as an independent risk factor for adverse perinatal outcome. Liver Int. 2010;30(5):765–770. | ||
Tse KY, Ho LF, Lao T. The impact of maternal HBsAg carrier status on pregnancy outcomes: a case-control study. J Hepatol. 2005;43(5):771–775. | ||
Buchanan C, Tran TT. Management of chronic hepatitis B in pregnancy. Clin Liver Dis. 2010;14(3):495–504. | ||
Borgia G, Carleo MA, Gaeta GB, Gentile I. Hepatitis B in pregnancy. World J Gastroenterol. 2012;18(34):4677–4683. | ||
Chang MH. Hepatitis B virus infection. Semin Fetal Neonatal Med. 2007;12(3):160–167. | ||
Teixeira J, Martin D, Prendiville O, Glover V. The effects of acute relaxation on indices of anxiety during pregnancy. J Psychosom Obstet Gynaecol. 2005;26(4):271–276. | ||
Teixeira C, Figueiredo B, Conde A, Pacheco A, Costa R. Anxiety and depression during pregnancy in women and men. J Affect Disord. 2009;119(1–3):142–148. | ||
Dayan J, Creveuil C, Marks MN, et al. Prenatal depression, prenatal anxiety, and spontaneous preterm birth: a prospective cohort study among women with early and regular care. Psychosom Med. 2006;68(6):938–946. | ||
Petersen JJ, Paulitsch MA, Guethlin C, Gensichen J, Jahn A. A survey on worries of pregnant women – testing the German version of the Cambridge worry scale. BMC Public Health. 2009;9:490. | ||
Wang XD, Wang XL, Ma H, editors. The Manual Of Mental Health Scales. Revised ed. Beijing: Chinese Mental Health magazine; 1999. | ||
Chen CH, Yu YM, Hwang KK. [Psychological stressors perceived by pregnant women during their third trimester]. Formosan Journal of Public Health. 1983;10(1):88Y98. Chinese. | ||
Chen CH. Revision and validation of a scale to assess pregnancy stress. J Nurs Res. 2015;23(1):25–32. | ||
Chen CH, Chen HM, Huang TH. Stressors associated with pregnancy as perceived by pregnant women during three trimesters. Gaoxiong Yi Xue Ke Xue Za Zhi. 1989;5(9):505–509. | ||
Pan Y-L, Wang H-J, Hu M. Study on the stress of pregnant women. Journal of Nursing Science. 2003;18(12):891–893. | ||
Pan Y-L, Yang Y, Wu Y. A correlative investigation on the stress and psychological health of pregnant women’s spouses. Zhonghua Hu Li Za Zhi. 2004;39(8):565–567. | ||
Liu Y-S, Guo M, Yuan X-Z. Study on psychological press of pregnant women and analysis of correlative factors. Modern Nursing. 2006;12(30):2852–2854. | ||
Zhou X, Li L, Zhou Y. Study on the correlation between psychological stress and anxiety in pregnant women. China Journal of Modern Medicine. 2010;20(7):1079–1082. | ||
Zou YL, Fan FL, Yue YF, Gou WL, Zhang PH, Zong L. Relationship between psychological status survey and cortisol and sex hormones in pregnant women with positive HBsAg. Maternal and Child Health Care of China. 2010;25(21):2944–2948. | ||
Voellmin A, Entringer S, Moog N, Wadhwa PD, Buss C. Maternal positive affect over the course of pregnancy is associated with the length of gestation and reduced risk of preterm delivery. J Psychosom Res. 2013;75(4):336–340. | ||
Sahebari M, Nabavi N, Salehi M. Correlation between serum 25(OH)D values and lupus disease activity: an original article and a systematic review with meta-analysis focusing on serum VitD confounders. Lupus. 2014;23(11):1164–1177. | ||
O’Connor TG, Winter MA, Hunn J, et al. Prenatal maternal anxiety predicts reduced adaptive immunity in infants. Brain Behav Immun. 2013;32:21–28. | ||
Petrova M, Kamburov V. Breastfeeding and chronic HBV infection: clinical and social implications. World J Gastroenterol. 2010;16(40):5042–5046. | ||
Majercsik E. Hierachy of needs of geriatric patients. Gerontology. 2005;51(3):170–173. | ||
Nydén K, Petersson M, Nyström M. Unsatisfied basic needs of older patients in emergency care environments – obstacles to an active role in decision making. J Clin Nurs. 2003;12(2):268–274. | ||
Ishikura R, Tashiro N. Frustration and fulfillment of needs in dissociative and conversion disorders. Psychiatry Clin Neurosci. 2002;56(4):381–390. | ||
Wiklund I, Glise H. Patient in focus: the way forward to promote wellbeing and delivery of health care in patients with gastro-oesophageal reflux disease. Eur J Surg Suppl. 2002;(587):82–88. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.