Back to Journals » ClinicoEconomics and Outcomes Research » Volume 15
A Cost-Utility Analysis of SQ® Tree SLIT-Tablet versus Placebo in the Treatment of Birch Pollen Allergic Rhinitis from a Swedish Societal Perspective
Authors Pollock RF , Slættanes AK, Brandi H , Grand TS
Received 26 June 2022
Accepted for publication 7 December 2022
Published 3 February 2023 Volume 2023:15 Pages 69—86
DOI https://doi.org/10.2147/CEOR.S377399
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Dean Smith
Richard F Pollock,1 Andreas K Slættanes,2 Henrik Brandi,2 Tobias Sydendal Grand2
1Covalence Research Ltd, Harpenden, UK; 2ALK-Abelló A/S, Hørsholm, Denmark
Correspondence: Andreas K Slættanes, ALK-Abelló A/S, Bøge Allé 1, Hørsholm, DK-2970, Denmark, Tel +45 53638813, Email [email protected]
Background and Aims: Allergic rhinitis (AR) is an immunoglobulin E antibody-mediated inflammatory condition that arises in response to inhaled allergens such as pollen. Pollens from trees in the birch homologous group are the most common allergenic tree pollens in Northern and Central Europe and North America. SQ® Tree SLIT-Tablet (ITULAZAX®) is a sublingual immunotherapy tablet indicated for moderate-to-severe AR and/or conjunctivitis induced by pollen from the birch homologous group. The present analysis evaluated the cost-utility of treating adults with AR with SQ Tree SLIT-Tablet versus placebo, both in combination with symptom-relieving medications, from a Swedish societal perspective.
Methods: A model was developed to evaluate changes in cost and quality of life associated with using SQ Tree SLIT-Tablet relative to placebo in an adult population of individuals with AR. The model captured costs associated with symptom-relieving medications, healthcare professional interactions, SQ Tree SLIT-Tablet, and indirect costs arising from absenteeism and reduced workplace productivity. The analysis was conducted over 10 years with costs captured in 2021 Swedish Krona (SEK) and future costs and effects discounted at 3% per annum. One-way and probabilistic sensitivity analyses were conducted.
Results: Treatment with SQ Tree SLIT-Tablet resulted in an improvement of 0.041 quality-adjusted life years (QALYs) over 10 years versus placebo. From a Swedish societal perspective, costs increased by SEK 9077 over the same period, resulting in an incremental cost-utility ratio of SEK 223,445 per QALY gained. One-way sensitivity analysis showed that the model was most sensitive to assumptions around the disease-modifying effect of SQ Tree SLIT-Tablet.
Conclusion: SQ Tree SLIT-Tablet improved quality of life in moderate-to-severe AR and/or conjunctivitis induced by pollen from the birch homologous group in Sweden, with only a modest increase in societal costs over a medium-term time horizon, representing good value for money at a willingness-to-pay threshold of SEK 700,000 per QALY.
Keywords: rhinitis, allergic, desensitization, immunologic, administration, oral, costs and cost analysis, quality of life, Sweden
Introduction
Allergic rhinitis (AR) is an inflammatory condition caused by an immunoglobulin E (IgE)-mediated immunological response to inhaled allergens such as pollen.1 Local symptoms that arise from the immune cascade in the nasal mucosa can include nasal congestion or obstruction, rhinorrhea, an itchy nose, sneezing, and conjunctivitis. Conjunctivitis manifests as ocular symptoms such as hyperemia, chemosis, periorbital edema, and itchy or watery eyes. In addition to these localized symptoms, individuals with AR also commonly suffer from systemic symptoms such as fatigue, reduced productivity, sleep impairment, and impaired concentration.1,2 AR also shares elements of pathology and pathophysiology with allergic asthma, which often co-exists with AR in the same individual;3,4 up to 30% of patients with AR have concomitant asthma, and more than 70% of patients with asthma have concomitant AR.5,6 The incidence of comorbid AR and asthma likely arises from the common systemic IgE-mediated response to inhaled allergens,2,7 and AR has been identified as a key risk factor for developing asthma.8–10
AR is most commonly caused by inhaled molds, dust mites, insects, dander, and pollens from weeds, grasses, and trees.1,11 Of the tree pollens, birch is the most common allergenic pollen in Northern and Central Europe, and among the key pollen allergens in North America.11–13 In Sweden specifically, the self-reported prevalence of AR was 28.0% according to a 2012 study by Eriksson et al with the highest prevalence of 33.6% reported amongst people aged 30–40.14 The primary allergenic component of birch pollen is the allergen Bet v 1, a homolog of allergens from other trees in the Fagales order. Based on a 2008 proposal for allergen homologous groups put forward by Lorenz et al, the European Medicines Agency (EMA) has defined the birch homologous group as including birch, alder, beech, hazel, hop/hornbeam, oak, and chestnut.15,16 The cross-reactive nature of allergens in the birch homologous group combined with the sequential flowering of trees in the group can result in individuals with birch pollen-induced AR experiencing symptoms for a prolonged period, extending beyond the birch pollen season.17 The geographical area in which an allergic reaction may be triggered may also be substantially widened thanks to the cross-reactivity between allergens in the group.
The long duration of exposure to pollen from the birch homologous group (birch and cross-reactive allergens) and the diverse range of AR symptoms combine to make birch pollen-induced AR a serious disease that can have a substantial negative effect on patient quality of life. The exact duration of the birch homologous group pollen season varies by year, but a 2019 randomized controlled trial reported the birch pollen season to last for 24 days (range: 10–42 days), while the full tree pollen season (including birch, alder, and hazel) was reported to last for 50 days (range: 14–68 days).18,19
The symptoms of AR can be reduced either by allergen avoidance or by one of the two forms of AR treatment recommended by clinical guidelines: symptom-relieving medications or allergy immunotherapy (AIT). Since allergen avoidance is difficult to achieve for tree pollen allergies, the Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines recommend the use of second-generation (non-sedating) oral or intranasal H1-antihistamines to treat the symptoms of pollen-induced AR, in combination with an intranasal corticosteroid or leukotriene receptor antagonist in cases where the symptoms are moderate/severe.20 AIT is then recommended in patients with moderate/severe AR who have a diagnosis of IgE-mediated allergy and have symptoms despite the use of symptom-relieving medications.20
SQ® Tree SLIT-Tablet (ITULAZAX®; ALK-Abelló, Hørsholm, Denmark) is a sublingual immunotherapy (SLIT) tablet indicated for the treatment of moderate-to-severe AR and/or conjunctivitis (with or without asthma) induced by pollen from the birch homologous group, indicated in adults with a clinical history of symptoms despite use of allergy pharmacotherapy and a positive test of sensitization to a member of the birch homologous group (skin prick test and/or specific IgE).21 The SQ Tree SLIT-Tablet is a standardized allergen extract of pollen from white birch (Betula verrucosa) per oral lyophilisate and has been investigated in a pan-European clinical development program comprising four randomized controlled trials (RCTs) in patients with AR due to birch pollen. The TT-04 trial was a Phase III, randomized, parallel-group, double-blind, placebo-controlled, multi-site study investigating the efficacy and safety of SQ Tree SLIT-Tablet in 634 subjects with moderate-to-severe allergic rhinitis and/or conjunctivitis induced by pollen from the birch homologous group.18,19 The primary endpoint was the average daily allergic rhinoconjunctivitis total combined score—a sum of the daily symptom score and the allergic rhinoconjunctivitis daily medication score—during the birch pollen season. TT-04 showed that the SQ Tree SLIT-Tablet reduced AR symptoms and symptom-relieving medication use by 39.6% during the birch pollen season and by 36.5% throughout the long tree pollen season (TPS; alder, hazel and birch) (p < 0.0001 versus placebo) while significantly improving quality of life versus placebo during both the birch and the long TPS (p < 0.05).18,19
In 2016, a systematic review of costs arising from AR in five European countries (Sweden, France, Germany, Italy, and Denmark) concluded that AR is associated with a considerable economic burden, driven primarily by indirect costs arising from high levels of absenteeism and reduced workplace productivity.22,23 Given this economic burden and the increasing pressure to optimize healthcare expenditure, the objective of the present study was to evaluate the cost-utility of the SQ Tree SLIT-Tablet and symptom-relieving medications relative to placebo and symptom-relieving medications, based on a combination of local data from the Swedish setting and the findings of the TT-04 trial.
Methods
Cost-Utility Analysis and Model
A cost-utility analysis was considered to be the most appropriate health economic analysis modality based on the findings of the TT-04 RCT, which, through mapping of Rhinoconjunctivitis Quality of Life Questionnaire (RQLQ) data to the EQ-5D health state utility values, provided evidence of a significant improvement in quality of life with the SQ Tree SLIT-Tablet relative to placebo.24,25 A discrete-time, cohort-level, cost-utility model was developed in Microsoft Excel 2016 to evaluate the cost and quality of life outcomes associated with the SQ Tree SLIT-Tablet versus placebo, both in combination with symptom-relieving medications, capturing changes in health-related quality of life, all relevant costs associated with treatment, and indirect costs arising from absenteeism and reduced workplace productivity. The model captured survival using two states: alive with AR, and dead, with time-dependent transitions governed by annual probabilities (to align with the annual cycle length) derived from Swedish life tables. All modeling of costs and quality-adjusted life expectancy, including differences between the SQ Tree SLIT-Tablet and placebo occurred within the “alive with AR” state.
Patient Population
The simulated patient population was in line with the approved indication for the SQ Tree SLIT-Tablet, consisting of individuals ≥18 years of age with moderate-to-severe allergic rhinoconjunctivitis (with or without asthma) induced by birch pollen, with a clinical history of symptoms despite use of symptom-relieving medications and a positive test of sensitization to a member of the birch homologous group (skin prick test and/or specific immunoglobulin E). The cost-utility analysis was conducted in individuals initiating treatment with AIT in the SQ Tree SLIT-Tablet arm (with access to symptom-relieving medications as required) or starting to take symptom-relieving medications only in the placebo arm. Population characteristics were derived from the TT-04 trial population, which was 47% male with a mean baseline age of 36.1 years (standard deviation 13.6 years).19 As the present study was based exclusively on computer simulation modeling, no human or animal subjects or samples were involved and no Institutional Review Board/Ethics Committee review was sought.
Life Expectancy and Quality of Life
In the base case analysis, age and sex-indexed all-cause mortality was captured based on Swedish life tables using cohort characteristics from the TT-04 trial.
The effect of the SQ Tree SLIT-Tablet on quality of life was evaluated as a secondary endpoint in the TT-04 RCT; using the RQLQ, the SQ Tree SLIT-Tablet significantly reduced the overall RQLQ score by 31.7% relative to placebo during the birch pollen season (24 days) and by 28.0% during the TPS (50 days), reflecting significantly improved quality of life. The RQLQ scores showed that quality of life was better with the SQ Tree SLIT-Tablet versus placebo at all time points assessed during the birch pollen season and the TPS (p < 0.05 for all time points except for week 10 [p = 0.2] during the TPS).
A utility increase of 0.0047 was modeled with the SQ Tree SLIT-Tablet in year 1 in line with a mapping analysis that estimated EQ-5D health state utility values directly from the TT-04 symptom and medication score data, and RQLQ scores.25 The quality of life difference was assumed to be maintained over the whole model time horizon. As the mapping analysis only evaluated the difference between the SQ Tree SLIT-Tablet and placebo, the baseline quality of life health state utility was assumed to be 0.92 based on reference values for patients with hay fever (n = 416) from Ara and Brazier.26 No change in quality of life from this baseline value was modeled in the placebo arm.
Perspective, Time Horizon, and Discounting
The analysis was conducted from a societal perspective, capturing the direct costs borne by the Swedish healthcare system, and indirect costs borne by Swedish society associated with absenteeism and reduced workplace productivity. The base case analysis was conducted over a 10-year time horizon, representing a one-year extension relative to a number of previous cost-utility analyses of AIT in Europe.27–30 The time horizon was selected based on the assumed duration of a disease-modifying effect with the SQ Tree SLIT-Tablet. In line with the European Academy of Allergy and Clinical Immunology (EAACI) recommendation of 3 years of AIT treatment, sustained treatment effects have been demonstrated over 6–7 years after treatment cessation with subcutaneous immunotherapy (SCIT).31,32 A structured review of the literature on disease modification arising from the use of AIT in the treatment of AR identified 14 relevant studies. All but one of the studies reported either a measurable improvement in AR symptoms versus control 1 to 10 years after cessation of AIT or no significant difference in AR symptom scores between treatment cessation and end of study, across grass, house dust mite-induced AR (Table 1).32–45
 |
Table 1 Evidence on the Disease-Modifying Effect of Allergy Immunotherapy Products for Allergic Rhinitis |
A 3% annual discount rate was applied to all future cost and effectiveness outcomes in line with recommendations from the Swedish Dental and Pharmaceutical Benefits Agency.46 A maximum willingness-to-pay (WTP) threshold of SEK 700,000 per quality-adjusted life year (QALY) gained was adopted using a “revealed preferences” approach as the highest acceptable incremental cost-utility ratio (ICUR) from the Swedish societal perspective based on the lowest cost per QALY of a declined reimbursement submission in Sweden in the period 2005–2011, as reported in a study by Svensson et al.47 The same study reported a median WTP threshold of SEK 350,000 across 86 reimbursement decisions in the same period. An alternative WTP threshold of the Swedish per capita gross domestic product (GDP) of SEK 523,000 was also used for comparison, with Swedish GDP obtained from the 2021 Statistiska centralbyrån.48
Direct Costs and Resource Use
The base case analysis captured direct costs associated with AIT, healthcare professional (HCP) interactions, and symptom-relieving medications. AIT costs were only captured in the SQ Tree SLIT-Tablet arm, based on a pack price of SEK 2948.81 for 90 SQ Tree SLIT-Tablets. It was assumed that the SQ Tree SLIT-Tablet would be taken perennially, taking one tablet per day for the first three years of the analysis covering the first three pollen seasons falling in the analysis period.31 On cessation of SQ Tree SLIT-Tablet treatment, no further AIT or HCP interaction costs were captured, but the effect of treatment was assumed to persist based on the established disease-modifying effect of AIT.
It was assumed that patients in the placebo arm would not attend any HCP appointments for AR, while two allergist visits were modeled in the first year of SQ Tree SLIT-Tablet treatment, followed by one allergist visit in subsequent years in line with AIT practice parameters published by the Joint Task Force on Practice Parameters from the American Academy of Allergy, Asthma & Immunology (AAAAI), the American College of Allergy, Asthma & Immunology (ACAAI), and the Joint Council of Allergy, Asthma & Immunology. The general AIT guidelines recommend patients “should have follow-up visits at least every 6 to 12 months”.49 The 2017 SLIT-specific practice parameter update made no more specific recommendations in terms of routine follow-up for patients using SLIT.50 A cost of SEK 1878 was assumed for each HCP interaction based on the “Sjv beh Lung och Allergi exkl lungmott (LAPSS1)” (medical treatment for lung and allergy excluding pulmonary embolism) price from the 2021 Prislista Västra Sjukvårdsregionen.
In the base case analysis, the costs of antihistamine tablets (desloratadine), eyedrops (olopatadine), and corticosteroid nasal spray (mometasone) were captured. Symptom-relieving medication resource use was based on data from the TT-04 trial (Table 2), and costs of symptom-relieving medications were taken from fass.se in November 2021 (Table 3). It was assumed that the cost of the nearest integer multiple of symptom-relieving medication packs sufficient to cover the required dose would be incurred in each modeled allergy season.
 |
Table 2 Symptom-Relieving Medication Resource Use Based on the TT-04 Trial |
 |
Table 3 Symptom-Relieving Medication Costs |
Indirect Costs
Indirect costs were modeled using a human capital approach based on absenteeism and reduced workplace productivity data from the TT-04 trial. In the base case analysis, the levels of absenteeism and reduced workplace productivity were based on data covering the TPS, with a duration of 50 days in line with the TPS duration in the TT-04 trial. In TT-04, 1.29% of days were taken as sick days with placebo, with the SQ Tree SLIT-Tablet reducing the risk of needing a sick day by 42% (corresponding to a relative risk of 0.58). Mean productivity with placebo in the TT-04 trial was 89.3%, which increased by 3.39%-points (in absolute terms) with the SQ Tree SLIT-Tablet. Reductions in productivity loss were captured for the TPS duration only. Workforce characteristics were derived from a combination of the TT-04 trial population (age and proportion male) and Sweden-specific data from the Statistiska centralbyrån and Eurostat (Table 4).
 |
Table 4 Workforce Characteristics Utilized in the Human Capital Approach to Modeling Costs of Absenteeism and Reduced Workplace Productivity |
In addition to the TT-04 based productivity losses, the base case analysis associated one hour of absenteeism with each HCP interaction in the SQ Tree SLIT-Tablet arm. Based on the assumption of no AR-related HCP interactions in the placebo arm, no excess absenteeism (beyond that based on the rates of absence in the TT-04 trial) was captured in the placebo arm.
One-Way Sensitivity Analyses
A series of one-way sensitivity analyses were conducted to establish the magnitude of the effect of changing various model parameters on outcomes. Annual discount rates were varied from 3% in the base case to 0% per annum (undiscounted) and 5% per annum to reflect different valuations of costs incurred and QALYs gained in the future. The time horizon was changed from 10 years in the base case analysis to 5 years and 15 years to establish if the cost-utility of the SQ Tree SLIT-Tablet increases or decreases over different time periods. An analysis was conducted in which no mortality was captured over the model time horizon. While no mortality differences were assumed in the base case analysis, the “no mortality” sensitivity analysis quantified the effect of 100% of patients surviving for the analysis time horizon in both arms of the analysis. Given that the assumption of individuals in the placebo arm not attending any allergy-related HCP appointments was likely to underestimate costs in the placebo arm, this was explored in two analyses. In the first, HCP interactions were set to be identical in both arms, and in the second, the HCP interaction frequency was set to be identical but individuals in the placebo arm were assumed to attend an appointment with a general practitioner (GP) rather than an allergy specialist.
A series of six analyses were then conducted in which key model options were changed from the base case settings. Productivity loss was modeled over the birch pollen season (24 days) rather than the TPS (50 days) in the base case, resulting in higher productivity loss but over a shorter time period. Indirect costs were excluded from the analysis, no productivity loss was associated with HCP interactions, symptom-relieving medication costs were omitted from the analysis, and the disease-modifying effect of the SQ Tree SLIT-Tablet was omitted using two different modeling assumptions.
In considering the disease-modifying effect, one analysis was conducted in which SQ Tree SLIT-Tablet treatment was continued over 10 years; costs were captured over the full 10-year time horizon (rather than 3 years in the base case analysis), while no changes were made to the effects of treatment relative to the base case analysis. A second analysis was conducted in which the effects of SQ Tree SLIT-Tablet on absenteeism, productivity loss, symptom-relieving medication use, and quality of life were abolished after 3 years to coincide with completion of a 3-year course of treatment. Notably, in the analysis in which SLIT treatment is continued for 10 years, the treatment duration far exceeds the SLIT treatment duration specified in the EAACI Guidelines, which note that “for patients with AR a minimum of three years of AIT is recommended in order to achieve long-term efficacy after treatment discontinuation”.31
Finally, an analysis was conducted around the rates of persistence with AIT treatment. Persistence rates were aligned with those reported for SLIT tablet use in Allam et al at 41% in year 2 and 31% in year 3.53 Costs, quality of life improvements, changes in absenteeism and productivity loss, and reductions in the use of symptom-relieving medications were assumed to decline proportionately with the rate of non-persistence across the cohort. After the end of SLIT treatment in year 3, all further cost and effectiveness outcomes were modeled at 30% of those modeled in the base case, in line with the proportion of patients ultimately deemed to be persistent in Allam et al.53
Probabilistic Sensitivity Analyses
In addition to the one-way sensitivity analyses, a probabilistic sensitivity analysis (PSA) was conducted in which uncertainty around multiple parameters was captured. In the analysis, 1000 Monte Carlo simulations were conducted, simultaneously drawing from seven distributions around key model parameters. The modeled estimates of cost and quality of life were recorded for each iteration and used to generate a cost-effectiveness scatterplot, cost-effectiveness acceptability curve (CEAC), and an estimate of the expected value of perfect information (EVPI) over a range of WTP thresholds.
EVPI is a theoretical measure commonly used in cost-utility analyses to quantify the value associated with eliminating uncertainty around model parameters. If the actual cost of obtaining that “perfect” information (eg, by means of conducting a larger clinical trial) were higher than the EVPI, then the additional data collection would not be worthwhile. Conversely, if the expected cost of obtaining the additional information were lower than the EVPI, additional research might be warranted. In all cases, the EVPI (and hence the decision to conduct additional research) is dependent on WTP. In the present analysis, the EVPI represents the value to the healthcare decision-maker of removing all uncertainty from the cost-effectiveness analysis. The value can therefore be thought of as the maximum acceptable cost of conducting additional research to obtain perfect information on all model parameters included in the PSA, which would thereby guarantee that the decision on the cost-effectiveness of the SQ Tree SLIT-Tablet versus placebo would be correct in the target population and at the specified WTP threshold.
Results
In the base case analysis, the SQ Tree SLIT-Tablet was associated with an improvement in quality-adjusted life expectancy of 0.041 QALYs relative to placebo over a 10-year time horizon, from 7.951 QALYs to 7.992 QALYs. The increase in quality-adjusted life expectancy was accompanied by an increase in costs of SEK 9077 per patient, from SEK 103,981 to SEK 113,057 over 10 years (Figure 1). The increases in costs and quality-adjusted life expectancy resulted in an ICUR of SEK 223,445 per QALY gained (Table 5).
 |
Table 5 Summary of Results from the Base Case Analysis of the Cost-Utility of SQ the Tree SLIT-Tablet Relative to Placebo Over a 10-Year Time Horizon from a Swedish Societal Perspective |
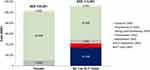 |
Figure 1 Cost breakdown in the deterministic base case analysis. |
One-way sensitivity analyses showed that incremental model outcomes were insensitive to changes in many of the model’s individual input parameters, with the notable exceptions of the disease-modifying effect of the SQ Tree SLIT-Tablet, the inclusion of indirect costs (absenteeism and reduced workplace productivity), and assumptions around HCP interactions in individuals in the placebo arm (Table 6). Excluding the disease-modifying effect of the SQ Tree SLIT-Tablet (thereby incurring AIT costs in every year of the analysis) increased the ICUR to SEK 2,210,793 per QALY gained, falling over the WTP threshold. Excluding all indirect costs from the analysis increased the incremental costs of the SQ Tree SLIT-Tablet relative to placebo to SEK 41,371 (from SEK 9077 in the base case), increasing the ICUR to 1,018,468 per QALY gained, which was similarly above the WTP threshold. Including the same frequency and nature of HCP interaction costs in the placebo arm as in the SQ Tree SLIT-Tablet arm resulted in SQ Tree SLIT-Tablet dominating placebo, with improved life expectancy and cost savings of SEK 11,489 per patient over 10 years. Assuming the same frequency of HCP interactions in the placebo arm but with a GP rather than an allergy specialist reduced the ICUR to SEK 77,461 per QALY gained. The analysis in which cost and effectiveness outcomes were reduced proportionately with a modeled rate of persistence to SQ Tree SLIT-Tablet treatment showed reductions in the incremental cost and QALY outcomes relative to the base case, but the assumption of proportionality resulted in an ICUR identical to that in the base case analysis.
 |
Table 6 One-Way Sensitivity Analysis Results |
Running 1000 PSA iterations showed that the SQ Tree SLIT-Tablet would be more costly than placebo in 84.7% of iterations, and more effective than placebo in 56.6% of iterations (Figure 2). The mean incremental quality-adjusted life expectancy was 0.047 QALYs higher (median 0.039 QALYs) with the SQ Tree SLIT-Tablet than placebo, in agreement with the increase of 0.041 QALYs in the deterministic base case analysis. The mean incremental cost was SEK 9518 higher with the SQ Tree SLIT-Tablet compared to SEK 9077 higher in the deterministic base case (ie, a difference of SEK 441 or 4.8% indicating that parameter uncertainty in the model had a relatively small effect on mean incremental outcomes).
 |
Figure 2 Cost-utility scatterplot based on 1000 probabilistic sensitivity analysis iterations. |
The incremental outcomes from the PSA were then used to plot a cost-effectiveness acceptability curve over a range of WTP thresholds from SEK 0 per QALY gained to SEK 700,000 per QALY gained (Figure 3). At a WTP threshold of SEK 350,000 per QALY gained, there would be a 52.1% likelihood that the SQ Tree SLIT-Tablet would be cost-effective relative to placebo (Figure 3); this increased to 53.4% at a WTP threshold of SEK 523,000 per QALY corresponding to Swedish GDP per capita in 2021 and to 53.6% at a WTP threshold of SEK 700,000 per QALY.
 |
Figure 3 Cost-utility acceptability curve generated from 1000 probabilistic sensitivity analysis iterations. |
Finally, an EVPI curve was generated from the PSA iteration data, showing that, at a WTP threshold of SEK 350,000 per QALY gained, the EVPI would be SEK 52,657 (Figure 4), increasing to SEK 77,436 at a WTP threshold of SEK 523,000 per QALY gained, and to SEK 102,277 at a WTP threshold of SEK 700,000 per QALY gained. Investment in the collection of additional information to reduce uncertainty in the decision-making around adoption of the SQ Tree SLIT-Tablet should therefore only be considered if the cost of the research fell below SEK 102,277 per patient (assuming a WTP threshold of SEK 700,000).
 |
Figure 4 Expected value of perfect information curve based on 1000 probabilistic sensitivity analysis iterations. |
Discussion
The present analysis showed that the SQ Tree SLIT-Tablet is likely to be cost-effective relative to placebo in the treatment of individuals ≥18 years of age with moderate-to-severe allergic rhinitis and/or conjunctivitis induced by pollen from the birch homologous group in Sweden. Over a 10-year time horizon, the SQ Tree SLIT-Tablet was projected to increase quality-adjusted life expectancy by 0.041 QALYs relative to placebo, and incur an additional SEK 9077 in costs, translating to an ICUR of SEK 223,445 per QALY gained. This falls well below the SEK 700,000 per QALY maximum WTP threshold identified using a “revealed preferences” approach in Sweden, and below the median value of SEK 350,000 per QALY across 86 Swedish reimbursement decisions evaluated by Svensson et al.47
The key drivers of cost-effectiveness identified through one-way sensitivity analyses were the analysis time horizon, the disease-modifying effect of the SQ Tree SLIT-Tablet and the inclusion of indirect costs borne by Swedish society in addition to direct medical costs. The inclusion of the disease-modifying effect in the base case analysis was based on the recommendation from the EAACI Guidelines, which note that “for patients with AR a minimum of three years of AIT is recommended in order to achieve long-term efficacy after treatment discontinuation”.31 Notably, in sensitivity analysis, when the cost of the SQ Tree SLIT-Tablet treatment was captured over the full 10-year duration of the analysis, the ICUR increased to SEK 2,210,793 per QALY gained, illustrating that continuous AIT treatment over 10 years would not be cost-effective relative to placebo.
Indirect costs were the biggest driver of cost offsets in the analysis, with the direct cost savings for symptom-relieving medications contributing only SEK 548 to the total SEK 32,882 of cost offsets brought about by the use of the SQ Tree SLIT-Tablet. The remaining cost offsets of SEK 3632 and SEK 28,702 were associated with reduced absenteeism and increased workplace productivity brought about by the SQ Tree SLIT-Tablet, respectively. Excluding these costs resulted in an ICUR of SEK 1,018,468 per QALY gained, which would not be considered cost-effective, but this analysis highlights the conservatism of the base case, particularly the exclusion of HCP interactions for individuals using symptom-relieving medications only; total costs in the placebo arm were only SEK 2550 over 10 years when indirect costs were excluded.
The analysis included numerous assumptions that may have underestimated the costs of placebo and overestimated the costs of SQ Tree SLIT-Tablet, for instance, assuming that individuals receiving no AIT would not have any allergy-related interactions with HCPs over the duration of the analysis. Given the moderate-to-severe nature of the allergic rhinitis and/or conjunctivitis experienced in the target population, this would be unlikely over a period of 10 years. Conversely, the analysis captured the fullest possible costs of HCP interactions with SQ Tree SLIT-Tablet, assuming an allergy specialist would be seen at every appointment and that each appointment would be associated with 1 hour of absenteeism and 10 km of travel. Furthermore, in the base case analysis, it was assumed that individuals would be 100% adherent to the prescribed treatment with SQ Tree SLIT-Tablet, with the likely effect of increasing both cost and efficacy relative to routine clinical practice.
Considering the duration of the AIT treatment course, persistence and adherence are worthy of some further consideration; a 2018 analysis of 2429 patients receiving SLIT and 2109 patients receiving SCIT in Germany reported 3-year persistence rates of 30% and 31% for SLIT tablet and SCIT patients, respectively.53 Within the persistent patients, adherence rates of 81% and 83%, respectively, were observed in patients treated with SLIT tablet and SCIT, again respectively.53 While these persistence rates are substantially lower than 100%, the balance of cost and utility (and hence the ICUR) would only be affected substantively if the relationship between adherence/persistence and cost was meaningfully different from the relationship between adherence/persistence and quality-adjusted life expectancy.
The analysis omitted comorbid conditions that commonly occur concomitantly with AR. For instance, the Bet v 1 allergen is cross-reactive with the major allergens of certain foods, which can result in individuals experiencing pollen-food syndrome (PFS). PFS symptoms include itching of the lips, tongue and throat, sometimes accompanied by swelling.54 The prevalence of PFS in individuals with AR is high, with 73.3% of individuals with birch-related AR experiencing symptoms associated with eating certain types of food, 86% of whom experienced PFS perennially.54 Costs of asthma were also not captured in the present analysis. Although the asthma symptom scores recorded in the TT-04 RCT were low (~1 on a scale from 0 to 12) in subjects with a medical history of asthma and in general for all subjects, an analysis of the average asthma daily symptom scores showed a reduction in asthma symptoms in the SQ Tree SLIT-Tablet group compared to placebo during both the birch pollen season (p = 0.0089) and the full TPS (p = 0.0239). However, an analysis of the proportion of days on which individuals required asthma medication showed no differences between the SQ Tree SLIT-Tablet and placebo during either the birch or tree pollen seasons.
One final potential limitation of the study pertains to the assumptions around the extent and duration of disease modification with the SQ Tree SLIT-Tablet. The assumption of 3 years of treatment with the SQ Tree SLIT-Tablet resulting in modification of the underlying disease is consistent with AIT treatment recommendations made by the EAACI, but the duration and extent of disease modification has not yet been demonstrated in individuals taking the SQ Tree SLIT-Tablet.31 The disease-modifying effect has been conclusively demonstrated in SQ SLIT tablets indicated for grass pollen-induced allergic rhinitis. Given that the mechanism of action for the birch homologous group is driven by the same immunological processes, it is likely that disease modification would also be observed in this patient group.
To our knowledge, the present study presents the first cost-utility analysis comparing SLIT tablets with placebo in patients with moderate-to-severe allergic rhinitis and/or conjunctivitis induced by pollen from the birch homologous group in Sweden; however, a 2008 analysis evaluated the cost-utility of the SQ Grass SLIT-Tablet (SLIT tablets for the treatment of allergic rhinitis induced by polled from Timothy grass) versus symptom-relieving medication over a 9-year time horizon in seven European countries including Sweden.55 The most notable difference from the present analysis was the use of health state utility values elicited directly from a clinical trial using the EQ-5D, which yielded an estimated 0.0287 QALY improvement per season with the SQ Grass SLIT-Tablet versus symptom-relieving medication. This compares with an estimate of 0.0047 QALY improvement per season in the present analysis, based on mapping symptom and medication score and RQLQ data from the TT-04 trial to health state utility values. Despite this substantial difference in the estimated difference in quality of life with SLIT versus placebo, the 2008 analysis reported a range of ICURs from approximately EUR 23,000 to EUR 50,000 per QALY gained depending on the assumed annual cost of the SQ Grass SLIT-Tablet. While there are numerous methodological differences between these studies which focus on different allergens, the lower end of the estimate from the 2008 study is closely aligned with the ICUR of EUR 21,330 per QALY gained in the present analysis (based on a 90-day trailing average EUR: SEK exchange rate as of May 2022).
Conclusion
The TT-04 RCT demonstrated that SQ Tree SLIT-Tablet is a safe and efficacious AIT product, with a simple mode of administration, and resulting in marked improvements in quality of life in individuals with moderate-to-severe allergic rhinitis and/or conjunctivitis induced by pollen from the birch homologous group. The present analysis showed that these quality of life benefits would be associated with only a modest increase in societal costs over a 10-year time horizon, therefore representing a cost-effective treatment option from the Swedish societal perspective based on a WTP threshold of SEK 700,000 per QALY gained.
Ethics Approval and Informed Consent
As the present study was based exclusively on computer simulation modeling, no human or animal subjects or samples were involved and no Institutional Review Board/Ethics Committee review was sought.
Data Sharing Statement
Additional data are available upon reasonable request to the corresponding author.
Funding
Development of the cost-utility model, formulation and execution of the Swedish analyses, and preparation of the manuscript were funded by ALK-Abelló A/S.
Disclosure
RFP is a director, shareholder, and full-time employee of Covalence Research Ltd, which received consultancy fees from ALK-Abelló A/S to develop the cost-utility model, formulate and execute the Swedish analyses, and prepare the manuscript draft. AKS, HB, and TSG were full-time employees of ALK-Abelló A/S at the time of the study. The authors report no other conflicts of interest in this work.
References
1. European Academy of Allergy and Clinical Immunology (EAACI). Global atlas of allergic rhinitis and chronic rhinosinusitis; 2015.
2. Léger D, Annesi-Maesano I, Carat F, et al. Allergic rhinitis and its consequences on quality of sleep: an unexplored area. Arch Intern Med. 2006;166(16):1744–1748. doi:10.1001/archinte.166.16.1744
3. Feng CH, Miller MD, Simon RA. The united allergic airway: connections between allergic rhinitis, asthma, and chronic sinusitis. Am J Rhinol Allergy. 2012;26(3):187–190. doi:10.2500/ajra.2012.26.3762
4. Khan DA. Allergic rhinitis and asthma: epidemiology and common pathophysiology. Allergy Asthma Proc. 2014;35(5):357–361. doi:10.2500/aap.2014.35.3794
5. Leynaert B, Neukirch C, Kony S, et al. Association between asthma and rhinitis according to atopic sensitization in a population-based study. J Allergy Clin Immunol. 2004;113(1):86–93. doi:10.1016/j.jaci.2003.10.010
6. Linneberg A, Henrik Nielsen N, Frølund L, Madsen F, Dirksen A, Jørgensen T; Copenhagen Allergy Study. The link between allergic rhinitis and allergic asthma: a prospective population-based study. The Copenhagen Allergy Study. Allergy. 2002;57(11):1048–1052. doi:10.1034/j.1398-9995.2002.23664.x
7. Fiocchi A, Fox AT. Preventing progression of allergic rhinitis: the role of specific immunotherapy. Arch Dis Child Educ Pract Ed. 2011;96(3):91–100. doi:10.1136/adc.2010.183095
8. Guerra S, Sherrill DL, Martinez FD, Barbee RA. Rhinitis as an independent risk factor for adult-onset asthma. J Allergy Clin Immunol. 2002;109(3):419–425. doi:10.1067/mai.2002.121701
9. Polosa R, Al-Delaimy WK, Russo C, Piccillo G, Sarvà M. Greater risk of incident asthma cases in adults with allergic rhinitis and effect of allergen immunotherapy: a retrospective cohort study. Respir Res. 2005;6:153. doi:10.1186/1465-9921-6-153
10. Shaaban R, Zureik M, Soussan D, et al. Rhinitis and onset of asthma: a longitudinal population-based study. Lancet. 2008;372(9643):1049–1057. doi:10.1016/S0140-6736(08)61446-4
11. World Allergy Organization. WAO white book on allergy. Milwaukee, WI, USA: World Allergy Organization; 2013. Available from: https://www.worldallergy.org/UserFiles/file/WhiteBook2-2013-v8.pdf.
12. Biedermann T, Winther L, Till SJ, Panzner P, Knulst A, Valovirta E. Birch pollen allergy in Europe. Allergy. 2019;74(7):1237–1248. doi:10.1111/all.13758
13. Morjaria JB, Caruso M, Emma R, Russo C, Polosa R. Treatment of Allergic rhinitis as a strategy for preventing asthma. Curr Allergy Asthma Rep. 2018;18(4):23. doi:10.1007/s11882-018-0781-y
14. Eriksson J, Ekerljung L, Rönmark E, et al. Update of prevalence of self-reported allergic rhinitis and chronic nasal symptoms among adults in Sweden. Clin Respir J. 2012;6(3):159–168. doi:10.1111/j.1752-699X.2011.00269.x
15. Lorenz AR, Lüttkopf D, May S, Scheurer S, Vieths S. The principle of homologous groups in regulatory affairs of allergen products – a proposal. Int Arch Allergy Immunol. 2008;148(1):1–17. doi:10.1159/000151243
16. European Medicines Agency. Guideline on allergen products: production and quality issues. EMEA/CHMP/BWP/304831/2007. London, UK; 2008. Available from: https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-allergen-products-production-quality-issues_en.pdf.
17. D’Amato G, Cecchi L, Bonini S, et al. Allergenic pollen and pollen allergy in Europe. Allergy. 2007;62(9):976–990. doi:10.1111/j.1398-9995.2007.01393.x
18. Integrated Clinical Trial Report. Efficacy and safety of the SQ tree SLIT-tablet in subjects with moderate to severe allergic rhinitis and/or conjunctivitis induced by pollen from the birch group. Trial ID: TT-04, 16 January 2018; 2018.
19. Biedermann T, Kuna P, Panzner P, et al. The SQ tree SLIT-tablet is highly effective and well tolerated: results from a randomized, double-blind, placebo-controlled Phase III trial. J Allergy Clin Immunol. 2019;143(3):1058–1066.e6. doi:10.1016/j.jaci.2018.12.1001
20. Bousquet J, Khaltaev N, Cruz AA, et al. World Health Organization; GA(2)LEN; AllerGen. allergic rhinitis and its impact on asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy. 2008;63(Suppl 86):8–160. doi:10.1111/j.1398-9995.2007.01620.x
21. Farmaceutiska Specialiteter i Sverige. ITULAZAX Summary of product characteristics. Available from: https://www.fass.se/LIF/product?userType=2&nplId=20180727000034&docType=6.
22. Linneberg A, Dam Petersen K, Hahn-Pedersen J, Hammerby E, Serup-Hansen N, Boxall N. Burden of allergic respiratory disease: a systematic review. Clin Mol Allergy. 2016;14:12. doi:10.1186/s12948-016-0049-9
23. Cardell LO, Olsson P, Andersson M, et al. TOTALL: high cost of allergic rhinitis-a national Swedish population-based questionnaire study. NPJ Prim Care Respir Med. 2016;26:15082. doi:10.1038/npjpcrm.2015.82
24. Juniper EF, Guyatt GH. Development and testing of a new measure of health status for clinical trials in rhinoconjunctivitis. Clin Exper Allergy. 1991;21:77–83. doi:10.1111/j.1365-2222.1991.tb00807.x
25. Dick K, Briggs A, Ohsfeldt R, Sydendal Grand T, Buchs S. A quality-of-life mapping function developed from a grass pollen sublingual immunotherapy trial to a tree pollen sublingual immunotherapy trial. J Med Econ. 2020;23(1):64–69. doi:10.1080/13696998.2019.1649268
26. Ara R, Brazier JE. Using health state utility values from the general population to approximate baselines in decision analytic models when condition-specific data are not available. Value Health. 2011;14:539–545. doi:10.1016/j.jval.2010.10.029
27. Hahn-Pedersen J, Worm M, Green W, Nørgaard Andreasen J, Taylor M. Cost utility analysis of the SQ® HDM SLIT-tablet in house dust mite allergic asthma patients in a German setting. Clin Transl Allergy. 2016;6:35. doi:10.1186/s13601-016-0127-6
28. Verheggen BG, Westerhout KY, Schreder CH, Augustin M. Health economic comparison of SLIT allergen and SCIT allergoid immunotherapy in patients with seasonal grass-allergic rhinoconjunctivitis in Germany. Clin Transl Allergy. 2015;5:1. doi:10.1186/s13601-015-0045-z
29. Nasser S, Vestenbaek U, Beriot-Mathiot A, Poulsen PB. Cost-effectiveness of specific immunotherapy with Grazax in allergic rhinitis co-existing with asthma. Allergy. 2008;63(12):1624–1629. doi:10.1111/j.1398-9995.2008.01743.x
30. Ronaldson S, Taylor M, Bech PG, Shenton R, Bufe A. Economic evaluation of SQ-standardized grass allergy immunotherapy tablet (Grazax) in children. Clinicoeconom Outcomes Res. 2014;6(1):187–196.
31. European Academy of Allergy and Clinical Immunology (EAACI). Allergen Immunotherapy guidelines. Part 2: recommendations. Available from: https://medialibrary.eaaci.org/mediatheque/media.aspx?mediaId=60223&channel=8518.
32. Jacobsen L, Niggemann B, Dreborg S, et al.; The PAT investigator group. Specific immunotherapy has long-term preventive effect of seasonal and perennial asthma: 10-year follow-up on the PAT study. Allergy. 2007;62:943–948. doi:10.1111/j.1398-9995.2007.01451.x
33. Mosbech H, Osterballe O. Does the effect of immunotherapy last after termination of treatment? Follow-up study in patients with grass pollen rhinitis. Allergy. 1988;43(7):523–529. doi:10.1111/j.1398-9995.1988.tb01631.x
34. Des Roches A, Paradis L, Knani J, et al. Immunotherapy with a standardized Dermatophagoides pteronyssinus extract. V. Duration of the efficacy of immunotherapy after its cessation. Allergy. 1996;51(6):430–433. doi:10.1111/j.1398-9995.1996.tb04643.x
35. Durham SR, Walker SM, Varga EM, et al. Long-term clinical efficacy of grass-pollen immunotherapy. N Engl J Med. 1999;341(7):468–475. doi:10.1056/NEJM199908123410702
36. Ott H, Sieber J, Brehler R, et al. Efficacy of grass pollen sublingual immunotherapy for three consecutive seasons and after cessation of treatment: the ECRIT study. Allergy. 2009;64(1):179–186. doi:10.1111/j.1398-9995.2008.01875.x
37. Marogna M, Spadolini I, Massolo A, Canonica GW, Passalacqua G. Long-lasting effects of sublingual immunotherapy according to its duration: a 15-year prospective study. J Allergy Clin Immunol. 2010;126(5):969–975. doi:10.1016/j.jaci.2010.08.030
38. Tabar AI, Arroabarren E, Echechipía S, García BE, Martin S, Alvarez-Puebla MJ. Three years of specific immunotherapy may be sufficient in house dust mite respiratory allergy. J Allergy Clin Immunol. 2011;127(1):57–63. doi:10.1016/j.jaci.2010.10.025
39. Durham SR, Emminger W, Kapp A, et al. SQ-standardized sublingual grass immunotherapy: confirmation of disease modification 2 years after 3 years of treatment in a randomized trial. J Allergy Clin Immunol. 2012;129(3):717–725.e5. doi:10.1016/j.jaci.2011.12.973
40. Bergmann KC, Demoly P, Worm M, et al. Efficacy and safety of sublingual tablets of house dust mite allergen extracts in adults with allergic rhinitis. J Allergy Clin Immunol. 2014;133(6):1608–1614. doi:10.1016/j.jaci.2013.11.012
41. Didier A, Malling HJ, Worm M, Horak F, Sussman GL. Prolonged efficacy of the 300IR 5-grass pollen tablet up to 2 years after treatment cessation, as measured by a recommended daily combined score. Clin Transl Allergy. 2015;5:12. doi:10.1186/s13601-015-0057-8
42. Scadding GW, Calderon MA, Shamji MH, et al.; Immune Tolerance Network GRASS Study Team. Effect of 2 years of treatment with sublingual grass pollen immunotherapy on nasal response to allergen challenge at 3 years among patients with moderate to severe seasonal allergic rhinitis: the GRASS randomized clinical trial. JAMA. 2017;317(6):615–625. doi:10.1001/jama.2016.21040
43. Bozek A, Starczewska-Dymek L, Jarzab J. Prolonged effect of allergen sublingual immunotherapy for house dust mites in elderly patients. Ann Allergy Asthma Immunol. 2017;119(1):77–82. doi:10.1016/j.anai.2017.05.012
44. Valovirta E, Petersen TH, Piotrowska T, et al.; GAP investigators. Results from the 5-year SQ grass sublingual immunotherapy tablet asthma prevention (GAP) trial in children with grass pollen allergy. J Allergy Clin Immunol. 2018;141(2):529–538. doi:10.1016/j.jaci.2017.06.014
45. Yonekura S, Gotoh M, Kaneko S, Maekawa Y, Okubo K, Okamoto Y. Disease-modifying effect of Japanese cedar pollen sublingual immunotherapy tablets. J Allergy Clin Immunol Pract. 2021;9(11):4103–4116.e14. doi:10.1016/j.jaip.2021.06.060
46. Dental and Pharmaceutical Benefits Board. Ändring i Tandvårds- och läkemedelsförmånsverkets allmänna råd (TLVAR 2003:2) om ekonomiska utvärderingar. Available from: https://www.tlv.se/download/18.467926b615d084471ac3230c/1510316374332/TLVAR_2017_1.pdf.
47. Svensson M, Nilsson FO, Arnberg K. Reimbursement decisions for pharmaceuticals in Sweden: the Impact of disease severity and cost effectiveness. Pharmacoeconomics. 2015;33(11):1229–1236. doi:10.1007/s40273-015-0307-6
48. Statistiska centralbyrån. National Accounts, quarterly and annual estimates; 2021. Available from: https://www.scb.se/en/finding-statistics/statistics-by-subject-area/national-accounts/national-accounts/national-accounts-quarterly-and-annual-estimates/.
49. Cox L, Nelson H, Lockey R, et al. Allergen immunotherapy: a practice parameter third update. J Allergy Clin Immunol. 2011;127(1 Suppl):S1–55. doi:10.1016/j.jaci.2010.09.034
50. Greenhawt M, Oppenheimer J, Nelson M, et al. Sublingual immunotherapy: a focused allergen immunotherapy practice parameter update. Ann Allergy Asthma Immunol. 2017;118(3):276–282.e2. doi:10.1016/j.anai.2016.12.009
51. Eurostat. Unemployment by sex and age - monthly average. Sweden; 2021. Available from: http://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=une_rt_m&lang=en.
52. Statistiska centralbyrån. Short-term statistics, wages and salaries, private sector (KLP); 2022. Available from: http://www.scb.se/am0101-en.
53. Allam JP, Andreasen JN, Mette J, Serup-Hansen N, Wüstenberg EG. Comparison of allergy immunotherapy medication persistence with a sublingual immunotherapy tablet versus subcutaneous immunotherapy in Germany. J Allergy Clin Immunol. 2018;141(5):1898–1901.e5. doi:10.1016/j.jaci.2017.12.999
54. Geroldinger-Simic M, Zelniker T, Aberer W, et al. Birch pollen-related food allergy: clinical aspects and the role of allergen-specific IgE and IgG4 antibodies. J Allergy Clin Immunol. 2011;127(3):616–22.e1. doi:10.1016/j.jaci.2010.10.027
55. Bachert C, Vestenbaek U, Christensen J, Griffiths UK, Poulsen PB. Cost-effectiveness of grass allergen tablet (GRAZAX) for the prevention of seasonal grass pollen induced rhinoconjunctivitis - a Northern European perspective. Clin Exp Allergy. 2007;37(5):772–779. doi:10.1111/j.1365-2222.2007.02706.x
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
