Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 17
A Comprehensive Analysis of Immunoglobulin E Levels, Allergen-Specific Sensitivities, and Clinical Manifestations in Allergic Dermatological Conditions: A Multicenter Retrospective Study in China
Authors Zhao J, Liang S, Zhou B, Li M, Li L
Received 21 November 2023
Accepted for publication 8 February 2024
Published 1 March 2024 Volume 2024:17 Pages 499—512
DOI https://doi.org/10.2147/CCID.S451117
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Jian Zhao,1 Surong Liang,2 Boyang Zhou,1 Min Li,3 Linfeng Li1
1Department of Dermatology, Beijing Friendship Hospital, Capital Medical University, Beijing, People’s Republic of China; 2Beijing Luhe Hospital, Capital Medical University, Beijing, People’s Republic of China; 3Clinical Epidemiology and Evidence Based Medicine Unit, Beijing Friendship Hospital, Capital Medical University, Beijing, People’s Republic of China
Correspondence: Linfeng Li, Department of Dermatology, Beijing Friendship Hospital, Capital Medical University, No. 95 Yong’an Road, Beijing, 100050, People’s Republic of China, Tel +86-10-63139108, Email [email protected]
Objective: To assess the correlations between Immunoglobulin E (IgE) levels, pruritus, and lesion severity in patients with eczema, atopic dermatitis, or urticaria.
Methods: A retrospective study was conducted and data of 814 patients who visited the dermatology or allergy clinics of multiple hospitals, from December 2019 to December 2021, were collected. Patients were divided into children group (< 18 years, 325 cases), adult group (18– 60 years, 435 cases), and older population group (> 60 years, 54 cases) based on the age. Baseline information, pruritus severity, severity of skin lesions, total IgE level, and specific IgE level were recorded to analyze the complex relationship between them.
Results: The prevalence of allergic conjunctivitis and allergic rhinitis in the children group was significantly higher than that in the adult and older population group (P < 0.01 or P < 0.05). The positive rate of specific IgE in children group was significantly higher than that in the adult and older population group (P < 0.01). The IgE levels in children with moderate pruritus were significantly lower than those of severe pruritus (63.39vs 114.42 IU/mL, P < 0.05). The IgE levels in children with mild and moderate skin lesions were significantly lower than those in children with severe skin lesions (58.95 vs 72.88 vs 169.15 IU/mL, P < 0.001 or P < 0.01, respectively).
Conclusion: Relationships among age, severity of skin pruritus and lesions, and allergen-specific IgE response are complex and subtle, displaying dynamic patterns.
Keywords: multi-center analysis, immunoglobulin E, pruritus severity, lesion severity
Introduction
Allergic skin diseases, including eczema, atopic dermatitis (AD), and urticaria, are prevalent dermatological conditions often intertwined with allergic sensitization.1 Global prevalence and incidence of cases of atopic dermatitis have continued to rise, leading to significant morbidity worldwide.2 Allergic skin diseases frequently prompt allergen-specific blood testing to ascertain the causal allergens and guide patient management.3 Eczema is a chronic, relapsing skin disease with rashes and itching.4 Atopic dermatitis, a chronic inflammatory skin condition, is often considered a manifestation of atopy and is frequently associated with elevated Immunoglobulin E (IgE) levels.5,6 Urticaria, characterized by itchy welts or hives, can be triggered by allergic reactions, and allergen testing can be instrumental in identifying causative allergens.7 However, there is a potential impact of baseline IgE levels on treatment resistance in atopic dermatitis, particularly concerning JAK inhibitors like baricitinib.8
IgE is a specialized class of antibodies that plays a pivotal role in the adaptive immune system, and detection of allergen-specific immunoglobulin E (IgE) antibodies in serum can screen for allergens in allergic patients.9 IgE antibodies are highly specific and are responsible for mediating immediate hypersensitivity reactions upon exposure to allergens. These reactions can manifest as allergic rhinitis, asthma, skin allergies, and even life-threatening anaphylactic shock.10 The binding of IgE to mast cells and basophils sensitizes these cells to allergen exposure, triggering the release of inflammatory mediators, such as histamine, which underlie the hallmark symptoms of allergy-itching, redness, swelling, and mucus production.11,12 However, IgE may not always serve as a reliable biomarker for treatment responsiveness in atopic dermatitis, particularly with JAK inhibitor therapy.13,14
Allergen testing is a cornerstone in the diagnosis and management of allergic diseases. Its primary objective is to identify specific allergens responsible for a patient’s allergic reactions, enabling targeted therapeutic interventions and allergen avoidance strategies. Various methods are employed for allergen testing, including blood tests, skin prick tests, patch tests, and intradermal tests.1,15–17 In China, blood testing, specifically measuring specific IgE antibody levels, is widely employed in clinical practice due to its relative immunity to interference from medications and its objectivity.18 These tests encompass total IgE and a panel of 20 common allergens, including inhalants and food allergens.
Although there are many studies on allergic diseases and IgE, there are relatively few studies on different age groups. We supposed that there may be some relationships among age, the severity of skin pruritus and lesions, and allergen-specific IgE response. Herein, this study aimed to comprehensively analyze the clinical characteristics of IgE in children, adults, and older population patients in China. By exploring the patterns of IgE sensitization and their associations with allergic skin diseases in different age cohorts, we aim to contribute valuable insights into the diagnostic and therapeutic approaches for allergic skin conditions, ultimately enhancing patient care and quality of life.
Materials and Methods
Patients and Methods
A retrospective study was conducted to collect data from 814 patients who attended dermatology or allergy clinics from December 2019 to December 2021 (the patient cohort was drawn from 17 hospitals located across diverse geographical regions within China, as detailed in Supplementary A). Patients were divided into three groups according to their age, children group (<18 years), adult group (18–60 years), and older population group (>60 years). The patient’s age, gender, geographical regional distribution, geographical and economic regional distribution, geographical and economic regional distribution, age of onset, comorbid allergic conditions, pruritus severity, severity of skin lesions, presence of food triggers, effective in avoidance of IgE-positive food allergens, exacerbation of symptoms after the consumption of IgE-positive foods, serum total IgE levels, serum-specific IgE levels were analyzed.
This study was approved by the ethics committee of the Beijing Friendship Hospital, Capital Medical University (NO.2019-P2-108-01), and the retrospective study has applied for exemption of patient informed consent because the review of the patient data was anonymous, and all aspects of the study comply with the Declaration of Helsinki.
Inclusion and Exclusion Criteria
Inclusion criteria: ① patients were diagnosed with skin diseases, including eczema, atopic dermatitis, or urticaria, and some patients were complicated with allergic manifestations such as allergic rhinitis, allergic conjunctivitis, or allergic asthma; ② patients underwent comprehensive allergen testing as part of the protocol.
Exclusion criteria: ① Physicians assessed patients who were unable to complete follow-up; ② Patients with mental disorders; ③ Pregnant woman.
Indicator Detection
IgE Detection
In this study, venous blood samples were collected from the patients and subsequently centrifuged to obtain serum. HOB® Quantitative Allergen Specific IgE Antibody REAST Kit (HOB Biotech Group Corp., Ltd, 96 Tests/Kit, sample undiluted) was used to quantitatively detect serum-specific IgE levels with method of reversed enzyme allegro-sorbent test (REAST). The specific procedural steps followed the manufacturer’s instructions.
The test results were interpreted as follows: serum total IgE levels (IU/mL) ≥60 IU/mL were considered positive, while allergen-specific IgE levels ≥0.35 IU/mL were also classified as positive. The 20 items of allergen-specific IgE (sIgE) detection include inhaled allergens and food allergens. Inhalation allergens include Dermatophagoides pteronyssinus, Dermatophagoides farina, Ambrosia artemisiifolia, Salix babylonica, dander of dog, Alternaria, cockroach, Artemisia argyi, dander of cat and house dust, food allergens include milk, hen’s egg, mutton, cod, peanut, beef, soybean, shrimp, crab, and wheat.
Evaluation of Pruritus Severity and Skin Lesion Severity
The degree of pruritus and severity of skin lesions were assessed by two dermatologists. Pruritus is a common symptom in dermatological disorders, and its severity can significantly impact the quality of life of affected individuals. In this study, we classified the degree of pruritus into three categories: (1) Mild Pruritus: Itching that does not require scratching; (2) Moderate Pruritus: Itching necessitating scratching but not affecting sleep or overall quality of life; (3) Severe Pruritus: Itching requiring scratching, which adversely affects both sleep and daily life. The severity of cutaneous manifestations is a pivotal aspect of our investigation into dermatological disorders. In our classification, we categorized the severity of cutaneous manifestations into three grades (the severity of cutaneous manifestations can be categorized as mild, moderate, or severe, as referenced) as follows: (1) Mild: cutaneous involvement affecting less than 5% of the total body surface area; (2) Moderate: cutaneous involvement affecting 5% to 10% of the total body surface area; and (3) Severe: cutaneous involvement affecting more than 10% of the total body surface area.19
Criteria for Geographical Division
China’s geographical divisions, including the boundary between southern and northern China, were classically defined by the Qinling-Huaihe Line. Regions south of this demarcation fall within the subtropical climate zone, while those to the north reside in the temperate climate zone. Additionally, China’s categorization into eastern, central, and western regions is typically based on a combination of geographical and economic factors. The eastern region encompasses the coastal areas and represents an economically developed sector, while the central region functions as an industrial hub with relatively robust economic development. Conversely, the western region is characterized by economic underdevelopment.20
Data Analysis
All analyses were performed using SAS software version 9.4. Heat maps of IgE values were made using GraphPad Prism software. Normally distributed measurement data were expressed as mean ± standard deviation (SD), while non-normally distributed measurement data were expressed as median (interquartile range), and the comparisons were examined by Student-t-test and Mann–Whitney test (non-parametric distribution). The categorical data were expressed as n (%), and the differences between the two groups were examined by chi-square analysis or Fisher’s exact test. A two-sided P < 0.05 was considered statistically significant.21
Results
Demographic Data and Baseline Characteristics: The Prevalence of Specific IgE Sensitization Differs Significantly Among Age Groups
The proportion of males in adults was lower than that in children and the elderly, respectively, and the differences were statistically significant (both P < 0.01). In the western region, the proportion of adult patients was significantly higher than that of children and elderly patients (both P < 0.01).
The prevalence of allergic conjunctivitis and allergic rhinitis in children group was significantly higher than that in the adult and older population group (P < 0.01 or P < 0.05).
Compared with the adult group, the children group and the older population group showed more severe skin pruritus and skin lesions, and the difference was statistically significant (P < 0.01).
The rate of symptom aggravation in older population group after eating IgE positive food was significantly higher than that in children group and adult group (P < 0.05). There were no significant group differences in other study variables (P > 0.05). Results are shown in Table 1.
 |
Table 1 Demographic Characteristics and Basics |
Qualitative IgE Results Across Age Groups: The Variations in Specific IgE Sensitization Profiles Among Different Age Groups are Striking
No significant differences in total IgE positivity rates were found across the age groups (P > 0.05).
The positive rate of specific IgE in children group was significantly higher than that in the adult and older population group (P < 0.01).
The positive rate of IgE in adult group exposed to Dermatophagoides farinae, cockroach, and Artemisia argyi was significantly higher than that in children and the elderly (P < 0.05 or P < 0.01). The positive rate of IgE in children exposed to Alternaria, house dust, milk, wheat, and eggs was significantly higher than that in adult group (P < 0.05) and older population group (P < 0.01).
No significant differences were noted for other specific IgEs (P > 0.05). Results are shown in Table 2.
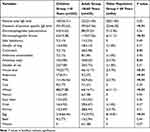 |
Table 2 Qualitative Results of Positive Total IgE and Positive Specific IgE Levels Among Different Age Groups, n (%) |
Qualitative IgE Findings by Pruritus Severity Across Age Groups: Distinct Patterns of Allergen Characteristics Associated with Pruritus Severity Among Different Age Groups
In the children group, the positive rate of IgE induced by cod and peanut in the severe pruritus group was significantly higher than that in the mild pruritus and moderate pruritus (P < 0.05). The positive rate of IgE caused by beef in children with mild pruritus was significantly higher than that of moderate pruritus and severe pruritus (P < 0.05). There was no significant difference between the degree of pruritus and qualitative IgE level in other age groups (P > 0.05). Results are shown in Table 3.
 |
Table 3 Qualitative Results of Positive Total IgE and Positive Specific IgE Levels for Different Pruritus Degrees Among Different Age Groups, n (%) |
Qualitative IgE Findings by Lesion Severity Across Age Groups: Varying IgE Positivity Rates Among Different Age Groups Based on the Severity of Cutaneous Manifestations
In children, the positive rate of total IgE in patients with severe skin lesions was significantly higher than that of mild and moderate skin lesions (P < 0.05). The positive rate of IgE caused by cod and peanut in patients with severe lesion was significantly higher than that of mild lesion and moderate lesion (P < 0.05). The positive rate of IgE caused by egg in patients with moderate and severe skin lesions was significantly higher than that of mill lesion (P < 0.05), and the positive rate of IgE caused by Artemisia argyi in patients with moderate skin lesion was significantly higher than that of mill lesion and severe lesion (P < 0.05).
In the elderly, the positive rate of at least one specific IgE in patients with mild skin lesion was higher than that of moderate and severe skin lesions (P < 0.05).
In adult group, there was no significant difference in the positive rate of total IgE and specific IgE among patients with different severity of the disease (P > 0.05). Results are shown in Table 4.
 |
Table 4 Qualitative Results of Positive Total IgE and Positive Specific IgE Levels for Different Lesion Severities Among Different Age Groups, n(%) |
Quantitative Levels of Total IgE by Pruritus Severity Across Age Groups: Distinct Patterns Emerged Concerning Itch Severity and Total IgE Levels Across Different Age Groups
Our analysis assessed total IgE across age groups with varying pruritus intensities, excluding 20 patients with IgE >1000 IU/mL (Figure 1).
 |
Figure 1 Quantitative levels of total IgE for different pruritus degrees among different age groups (excluding 20 patients with IgE >1000 IU/mL). |
In children, the IgE levels in children with moderate pruritus were significantly lower than those of severe pruritus (63.39 vs 114.42 IU/mL, P < 0.05). There was no significant difference in quantitative IgE levels among different pruritus severity in other age groups (P > 0.05).
Quantitative Levels of Total IgE by Lesion Severity Across Age Groups: Intriguing Disparities in Total IgE Distributions Concerning the Severity of Skin Lesions Across Different Age Groups
Our analysis assessed total IgE across age groups with varying pruritus intensities, excluding 20 patients with IgE >1000 IU/mL (Figure 2).
 |
Figure 2 Quantitative levels of total IgE for different lesion severities among different age groups (excluding 20 patients with IgE >1000 IU/mL). |
In children, the IgE levels in children with mild and moderate skin lesions were significantly lower than those of severe skin lesions (58.95 vs 72.88 vs 169.15 IU/mL, P < 0.001 or P < 0.01, respectively). There was no significant difference in quantitative IgE levels among different lesions severity in other age groups (P > 0.05).
Quantitatively Specific IgE Profiles by Pruritus Severity Across Age Groups: Distinct Allergen-Specific IgE Patterns Among Patients of Different Age Groups Experiencing Varying Levels of Itch Severity
Our investigation mapped the IgE profiles to 20 allergens across age demographics correlated with pruritus severity (Figure 3). The heatmap’s rows (A-T) represent allergens like house dust mites, pollens, foods, and animal danders, with columns denoting individual patient data.
In children, allergen-specific IgE varied with pruritus intensity. Mild pruritus was associated with higher IgE to Dermatophagoides farinae and Alternaria, while moderate pruritus correlated with increased IgE to a broader range of allergens including Dermatophagoides pteronyssinus, Dermatophagoides farinae, egg, Artemisia argyi, dander of cat, and Alternaria. Severe pruritus in children showed significant IgE elevations to Dermatophagoides pteronyssinus, Dermatophagoides farinae, milk, wheat, crab, shrimp, egg, dander of dog, and Artemisia argyi.
For adult group, the IgE profile was less uniform. Mild pruritus was linked to higher IgE levels to Dermatophagoides farinae, Artemisia argyi, dander of cat, and house dust. Moderate pruritus did not show distinct IgE elevations, suggesting varied underlying factors. Severe pruritus was marked by increased IgE to dog dander.
Elderly subjects presented unique allergen sensitivities. Mild pruritus was associated with higher IgE to milk and wheat, moderate pruritus to Dermatophagoides pteronyssinus, Dermatophagoides farinae, and egg, and severe pruritus to milk and Artemisia argyi.
Quantitatively Specific IgE Profiles by Lesion Severity Across Age Groups: Diverse Allergen-Specific IgE Patterns Were Observed Among Different Age Groups Experiencing Varying Degrees of Skin Lesion Severity
Our analysis delineated specific IgE reactivity to 20 allergens across age groups, correlating with skin lesion severity (Figure 4). The heatmap aligns individual patient data with allergens including dust mites, pollens, foods, and animal danders.
Children with mild lesions showed increased IgE to Dermatophagoides farinae, milk, egg, and dander of dog, while moderate lesions correlated with higher IgE to a broader allergen spectrum including Dermatophagoides pteronyssinus, Dermatophagoides farinae, Artemisia argyi, dander of cat, and Alternaria. Severe lesions in children were marked by elevated IgE to Dermatophagoides farinae, wheat, crab, shrimp, and egg.
In adult group, mild lesions were associated with higher IgE to Dermatophagoides farinae. Moderate lesions showed increased IgE to dog dander, and severe lesions correlated with higher IgE to Dermatophagoides pteronyssinus, Dermatophagoides farinae, and Artemisia argyi.
Elderly individuals with mild lesions had elevated IgE to Dermatophagoides pteronyssinus, Dermatophagoides farinae, and shrimp. Those with moderate lesions showed higher IgE to wheat and eggs, while severe lesions were associated with increased IgE to milk.
Discussion
Allergic diseases encompass a spectrum of conditions, among the most prevalent being eczema, atopic dermatitis, urticaria, allergic conjunctivitis, allergic rhinitis, and asthma. In the contemporary context, marked by robust economic growth, there has been a notable upsurge in the prevalence of allergic diseases within the global populace.22 The implications of these allergic conditions are multifaceted, profoundly affecting individuals’ social engagements, sleep patterns, and often imposing substantial economic burdens.23
Allergic reactions are mediated by IgE antibodies produced by the immune system in response to environmental proteins (allergens) such as pollen, animal dander or dust mites, which play a pivotal role in the initiation and progression of allergic diseases.24 An oft-utilized diagnostic approach for discerning the etiological factors underlying allergic diseases involves the assessment of specific IgE antibodies through serological analysis-a widely adopted clinical methodology.9 The identification and subsequent avoidance of allergens to which patients demonstrate sensitivity frequently led to the amelioration or prevention of symptoms associated with allergic diseases.
Our results demonstrate diverse patterns of allergen-specific IgE among different age groups with varying degrees of skin lesion severity. Among children, a wide range of allergens showed significantly elevated IgE values across different severity levels, particularly in cases of moderate and severe skin lesions. In contrast, young and elderly adults exhibited a reduced variety of allergens with significantly elevated IgE values, with only one predominant allergen observed in cases of mild and moderate skin lesions in the adult group and severe skin lesions in the elderly. Furthermore, elderly individuals with moderate skin lesions displayed elevated IgE values for only two specific allergens. These findings underscore the association between IgE levels and the severity of skin lesions.
Our study reveals that the prevalence of specific IgE sensitization differs significantly among age groups. Notably, the children group exhibits the highest prevalence of sensitization. Among food allergens, milk, egg, and wheat allergens were significantly higher in the children’s group than in other age groups; among respiratory allergens, house dust allergens were significantly higher in the children’s group than in other age groups. This observation aligns with existing literature,18 which underscores the higher susceptibility of children to allergen sensitization due to their developing immune systems and increased exposure to common allergens; moreover, genetic predispositions and early-life environmental factors play a significant role in shaping allergen sensitization patterns in children.25
The variations in specific IgE sensitization profiles among different age groups are striking. Notably, specific allergens such as dust mites, milk, wheat, eggs, house dust, alternata, cockroach, and Artemisia pollen exhibit statistically significant differences in sensitization rates. Understanding the allergen profiles associated with specific age groups is of paramount importance for tailoring diagnostic and therapeutic interventionsYoung and middle-aged adults, representing the “productive” age groups, exhibit unique allergen sensitization profiles, which can significantly impact an individual’s quality of life and productivity. Allergen-specific IgE testing is vital for precise diagnosis and management strategies in this age group. In contrast, the elderly population often shows sensitization to indoor allergens such as house dust mites and cockroaches.26 Identifying sensitization to these allergens through specific IgE testing is vital for optimizing clinical management in older patients.
In our study, we observed distinct patterns of allergen characteristics associated with pruritus severity among different age groups, providing valuable insights into the complex interplay between allergic sensitization and itching. Our analysis revealed notable variations in the specific allergens associated with pruritus severity across different age groups. Specifically, in the children group, we observed significant differences in the IgE sensitization profiles to various allergens among children experiencing different degrees of pruritus. Codfish (cod) and peanuts exhibited higher IgE positivity rates in children with severe pruritus. Conversely, beef-specific IgE showed a higher positivity rate in children with mild pruritus. This suggests that these particular food allergens may contribute to exacerbated pruritus in children with severe symptoms, while beef might be more likely to induce mild pruritus. Intriguingly, all the allergens exhibiting statistical differences were food allergens. This highlights the significant impact of dietary factors, especially in children's populations, on the severity of pruritus.
The observed variation in allergen profiles associated with pruritus severity raises several important questions and warrants further investigation. Firstly, it prompts consideration of whether previous literature has explored the propensity for different age groups, particularly children, to exhibit varying degrees of pruritus in connection with allergies. Secondly, the relationship between pruritus severity and IgE sensitization patterns, especially in the context of different allergens, requires more in-depth exploration. These aspects merit comprehensive investigation in future research endeavors. Understanding the intricate relationship between pruritus severity, age, and specific allergens can have profound implications for clinical practice. Tailored management strategies that account for age-related differences in allergic sensitization and dietary factors may be essential for effectively alleviating itching in individuals with allergic dermatological conditions.
Our results reveal varying IgE positivity rates among different age groups based on the severity of cutaneous manifestations. Notably, in the children group, individuals with severe cutaneous involvement exhibited higher total IgE positivity rates; conversely, within the older population group, individuals with mild cutaneous involvement displayed the highest IgE positivity rates for any specific allergen. Children may have a higher prevalence of atopic dermatitis and a higher IgE response to allergens than adults. Similarly, older adults may have a lower IgE response to allergens due to age-related changes in immune function. Therefore, it is important to consider age when interpreting the correlation between IgE levels and skin condition severity.
These findings underscore the complex interplay between the severity of cutaneous manifestations and IgE sensitization across different age groups. In particular, among children, the allergen-specific IgE profiles differed based on the severity of cutaneous manifestations. Codfish and peanuts displayed higher IgE positivity rates in children with severe cutaneous involvement, while eggs exhibited higher IgE positivity rates in children with moderate and severe cutaneous involvement. Moreover, Artemisia argyi-specific IgE had a higher positivity rate in children with moderate cutaneous involvement. These observations suggest that certain dietary elements, such as codfish, peanuts, eggs, and Artemisia argyi, could potentially exacerbate the severity of cutaneous manifestations in children. Consequently, diet appears to exert a significant influence on the extent of cutaneous involvement in children’s populations.
The relationship between the severity of cutaneous manifestations, age, and IgE sensitization has not been extensively explored in existing literature. Therefore, our findings contribute valuable insights into the intricate connections between age-related variations in cutaneous severity, IgE responses, and specific allergens. Future research endeavors should delve deeper into these associations to elucidate the underlying mechanisms driving the observed patterns. This may involve investigating the role of immune system development and aging in shaping IgE sensitization patterns and their correlation with the severity of cutaneous manifestations. Furthermore, exploring potential therapeutic interventions, including dietary modifications, for individuals with dermatological conditions across different age groups could prove beneficial. As allergic skin disorders continue to impact a substantial portion of the population, a comprehensive understanding of these multifaceted relationships is imperative for devising more effective diagnostic and management strategies.
In our results, distinct patterns emerged concerning itch severity and total IgE levels across different age groups. Interestingly, we observed a similar distribution of total IgE levels concerning mild to severe itch severity among adult group and the elderly. However, the children group exhibited notable differences in the distribution of total IgE levels, specifically concerning moderate itch. In this group, only the distribution of total IgE levels corresponding to moderate and severe itch showed statistically significant differences, indicating varying levels of itch severity among children and a corresponding divergence in total IgE distribution. Notably, our findings underscore the significant impact of total IgE levels on itch severity within the children population. Our study not only adds to this body of knowledge but also highlights the need for targeted interventions, especially among children’s patients, where the correlation between total IgE levels and itch severity is notably pronounced.
Our results shed light on intriguing disparities in total IgE distributions concerning the severity of skin lesions across different age groups. Notably, a uniform pattern emerged among adult group and the elderly, indicating similar total IgE distributions in the presence of varying degrees of skin lesions. However, the children group exhibited distinctive patterns. In this cohort, significant differences were observed in total IgE distributions between children with mild skin lesions and those with severe skin lesions. Moreover, the distribution of total IgE levels in children with moderate skin lesions significantly differed from those with severe skin lesions. These findings underscore the nuanced relationship between skin lesion severity and total IgE levels, particularly within the children's population.
In our study, we observed distinct allergen-specific IgE patterns among patients of different age groups experiencing varying levels of itch severity. Specifically, among children, moderate and severe itch conditions were associated with significantly elevated IgE values for a wider array of allergens. Conversely, among adult group, mild itch correlated with higher IgE values for a broader range of allergens compared to moderate and severe itch. In the elderly, moderate itch was linked to higher IgE values for multiple allergens. These findings underscore the association between IgE levels and itch severity.
The strength of this study is that it adopted a multicenter study, and the study included patients of all ages from different geographical and climatic environments in the east, west, north, and south of China, which included a relatively comprehensive range of patients. Qualitative and quantitative studies of IgE in patients with skin diseases of different ages, as well as in patients with different levels of pruritus and disease severity, are relatively comprehensive in scope. Of course, this study also has some shortcomings. First of all, although this study is a multi-center study, as a retrospective study, it has considerable limitations, and the results also need to be further verified by prospective studies. Secondly, this study was only a phenomenal-level study, without further discussion of its internal causes and mechanisms. Further longitudinal studies and clinical trials are needed to elucidate the underlying mechanisms and explore potential therapeutic approaches to alleviate the severity of pruritus and improve the quality of life of patients. Finally, the sample size of this study was small; although more than 800 patients were included, it was relatively small in the whole of China.
Conclusion
This study sheds light on the subtle dynamic relationships among age, severity of skin pruritus and lesions, and allergen-specific IgE response.
Acknowledgment
Thanks to the research units and corresponding medical staff in the Supplementary Document.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wang X, Zhou L, Wei G, Zhang H, Yang B. Prevalence of allergen-specific IgE in southern China: a multicenter research. Aging. 2021;13(14):18894–18911. doi:10.18632/aging.203341
2. Shin YH, Hwang J, Kwon R, Lee SW, Kim MS; GBD 2019 Allergic Disorders Collaborators, et al. Global, regional, and national burden of allergic disorders and their risk factors in 204 countries and territories, from 1990 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. Allergy. 2023;78(8):2232–2254. doi:10.1111/all.15807
3. Özdoğru EE, Gönülal M. Atopic dermatitis, inhalant allergy and food allergy: a paediatric approach. Dermatol Ther. 2021;34(1):e14542. doi:10.1111/dth.14542
4. Guo Y, Dou X, Chen XF, Huang C, Zheng YJ, Yu B. Association between nasal colonization of staphylococcus aureus and eczema of multiple body sites. Allergy Asthma Immunol Res. 2023;15(5):659–672. doi:10.4168/aair.2023.15.5.659
5. Wollenberg A, Werfel T, Ring J, Ott H, Gieler U, Weidinger S. Atopic dermatitis in children and adults—diagnosis and treatment. Dtsch Arzteblatt Int. 2023;120(13):224–234.
6. Tokura Y, Hayano S. Subtypes of atopic dermatitis: from phenotype to endotype. Allergol Int off J Jpn Soc Allergol. 2022;71(1):14–24. doi:10.1016/j.alit.2021.07.003
7. Zuberbier T, Aberer W, Asero R, et al. The EAACI/GA2LEN/EDF/WAO guideline for the definition, classification, diagnosis and management of urticaria. Allergy. 2018;73(7):1393–1414. doi:10.1111/all.13397
8. Hagino T, Saeki H, Fujimoto E, Kanda N. Efficacy and safety of baricitinib treatment for moderate to severe atopic dermatitis in real-world practice in Japan. J Dermatol. 2023;50(7):869–879. doi:10.1111/1346-8138.16763
9. Koga Y, Ishii S, Yokooji T, et al. A novel test for type-I allergy based on crosslink formation of immunoglobulin-E receptors by allergen-specific immunoglobulin-E antibodies and an allergen. Sci Rep. 2023;13(1):19676. doi:10.1038/s41598-023-46730-8
10. Justiz Vaillant AA, Modi P, Jan A. Atopy. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023. Available from http://www.ncbi.nlm.nih.gov/books/NBK542187/.
11. Gould HJ, Sutton BJ. IgE in allergy and asthma today. Nat Rev Immunol. 2008;8(3):205–217. doi:10.1038/nri2273
12. Stone KD, Prussin C, Metcalfe DD. IgE, mast cells, basophils, and eosinophils. J Allergy Clin Immunol. 2010;125(2 Suppl 2):S73–80. doi:10.1016/j.jaci.2009.11.017
13. Hagino T, Yoshida M, Hamada R, Saeki H, Fujimoto E, Kanda N. Effectiveness of switching from baricitinib 4 mg to upadacitinib 30 mg in patients with moderate-to-severe atopic dermatitis: a real-world clinical practice in Japan. J Dermatol Treat. 2023;34(1):2276043. doi:10.1080/09546634.2023.2276043
14. Hagino T, Hamada R, Yoshida M, Fujimoto E, Saeki H, Kanda N. Effectiveness and safety of upadacitinib in combination with topical corticosteroids in adolescent patients with moderate-to-severe atopic dermatitis. Clin Cosmet Invest Dermatol. 2023;16:3201–3212. doi:10.2147/CCID.S439053
15. Ruëff F, Bergmann KC, Brockow K, et al. Hauttests zur Diagnostik von allergischen Soforttyp-Reaktionen1 Leitlinie der Deutschen Gesellschaft für Allergologie und klinischen Immunologie (DGAKI) [Skin tests for diagnostics of allergic immediate-type reactions. Guideline of the German Society for Allergology and Clinical Immunology]. Pneumol Stuttg Ger. 2011;65(8):484–495. German. doi:10.1055/s-0030-1256476
16. Uyesugi BA, Sheehan MP. Patch testing pearls. Clin Rev Allergy Immunol. 2019;56(1):110–118. doi:10.1007/s12016-018-8715-y
17. Larrabee YC, Reisacher W. Intradermal testing after negative skin prick testing for patients with high suspicion of allergy. Int Forum Allergy Rhinol. 2015;5(6):547–550. doi:10.1002/alr.21512
18. Ying X, Qi X, Yin Y, et al. Allergens sensitization among children with allergic diseases in Shanghai, China: age and sex difference. Respir Res. 2022;23(1):95. doi:10.1186/s12931-022-02008-7
19. Matsuoka H, Maki N, Yoshida S, et al. A mouse model of the atopic eczema/dermatitis syndrome by repeated application of a crude extract of house-dust mite Dermatophagoides farinae. Allergy. 2003;58(2):139–145. doi:10.1034/j.1398-9995.2003.23790.x
20. Xiong X, Wang Y, Liu B, He W, Yu X. The impact of green finance on the optimization of industrial structure: evidence from China. PLoS One. 2023;18(8):e0289844. doi:10.1371/journal.pone.0289844
21. Lee S. Methods for testing statistical differences between groups in medical research: statistical standard and guideline of Life Cycle Committee. Life Cycle. 2022;24:2.
22. Asher MI, Montefort S, Björkstén B, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC phases one and three repeat multicountry cross-sectional surveys. Lancet Lond Engl. 2006;368(9537):733–743. doi:10.1016/S0140-6736(06)69283-0
23. Dierick BJH, van der Molen T, Flokstra-de Blok BMJ, et al. Burden and socioeconomics of asthma, allergic rhinitis, atopic dermatitis and food allergy. Expert Rev Pharmacoecon Outcomes Res. 2020;20(5):437–453. doi:10.1080/14737167.2020.1819793
24. Justiz Vaillant AA, Vashisht R, Zito PM. Immediate Hypersensitivity Reactions. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023. Available from http://www.ncbi.nlm.nih.gov/books/NBK513315/.
25. Yang IV, Lozupone CA, Schwartz DA. The environment, epigenome, and asthma. J Allergy Clin Immunol. 2017;140(1):14–23. doi:10.1016/j.jaci.2017.05.011
26. Li J, Huang Y, Lin X, et al. Influence of degree of specific allergic sensitivity on severity of rhinitis and asthma in Chinese allergic patients. Respir Res. 2011;12(1):95. doi:10.1186/1465-9921-12-95
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


