Back to Journals » Clinical Ophthalmology » Volume 17
0.2% Betamethasone Sodium Phosphate: A Multicenter, Randomized, Double-Masked Study to Compare Its Ocular Safety, Tolerability, and Efficacy to Vehicle in Cataract Surgery Subjects
Authors Hosseini K, Gollamudi S , Reiser H, Walters T , Lindstrom RL
Received 17 May 2023
Accepted for publication 25 July 2023
Published 5 August 2023 Volume 2023:17 Pages 2219—2230
DOI https://doi.org/10.2147/OPTH.S419857
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Kamran Hosseini,1 Subba Gollamudi,2 Harvey Reiser,3 Tom Walters,4 Richard L Lindstrom5
1Surface Ophthalmics, Pleasanton, CA, USA; 2VRF Eye Specialty Group, Memphis, TN, USA; 3Eye Care Specialists, Kingston, PA, USA; 4Texan Eye, PA — Keystone Research, Austin, TX, USA; 5Minnesota Eye Consultants, Bloomington, MN, USA
Correspondence: Kamran Hosseini, Surface Ophthalmics, Inc, 5000 Hopyard Road, Ste. 402, Pleasanton, CA, 94588, USA, Email [email protected]
Purpose: To compare the preservative-free corticosteroid 0.2% betamethasone sodium phosphate BID (SURF-201) to vehicle BID in patients undergoing routine cataract surgery.
Methods: Phase 2, multicenter, randomized (1:1 ratio), double-masked, vehicle-controlled, parallel-group study in patients scheduled for uncomplicated cataract surgery without the aid of a femtosecond laser. Subjects instilled topical medications for 16 days beginning the day before cataract surgery (Day − 1), 1 dose administered at least 1 hour prior to cataract surgery (on Day 0) and 1 dose on the evening after cataract surgery, and then 2 doses administered each day through Day 15; patients were re-evaluated on Days 22 and 32 to ensure no rebound inflammation. Primary outcome was the difference in the proportion of subjects with anterior chamber cell (ACC) grade 0 between the two groups at Day 15. Secondary outcomes included pain scores and overall safety.
Results: There was a statistically significant difference (P=0.004) in the proportion of subjects in the SURF-201 treatment group with an ACC grade of 0 at Day 15 (n=22/39 [56.4%]) compared to subjects in the vehicle treatment group (n=9/43 [20.9%]). There was no statistically significant difference (P=0.528) in the proportion of subjects in the SURF-201 treatment group who had a visual analog scale pain score of 0 at Day 15 (n=35/38 [89.7%]) compared to subjects in the vehicle group (n=33/40 [82.5%]). A slightly higher incidence of adverse events occurred in subjects in the SURF-201 treatment group (n=27/40 [67.5%]) compared to the vehicle treatment group (n=23/43 [53.5%]).
Conclusion: SURF-201 is an effective topical, preservative-free corticosteroid when dosed BID for the treatment of postoperative inflammation and prevention of pain in a post-cataract population.
Keywords: cataract, postoperative inflammation, corticosteroid, betamethasone sodium phosphate, preservative-free
Introduction
Age-related cataract is a leading cause of visual impairment worldwide, with numbers expected to increase as the aging population increases1–3 Globally, 17 million people are blind and 94 million have vision impairment because of cataract;1,2 the number of cataract surgeries is expected to reach 50 million by 2050.4,5 With millions of surgeries performed yearly worldwide, cataract surgery is generally deemed one of the safest surgical procedures, with very few serious postoperative complications.6
Both ocular inflammation and pain are common post-cataract surgery.7 These are accepted and expected postoperatively, yet if left untreated they can lead to impaired vision and decreased patient satisfaction.3,7,8 Walters et al showed that in the early postoperative period, 70% to 85% of patients had anterior chamber cells, 50% to 65% of patients had anterior chamber flare, and 40% to 60% of patients reported ocular pain.9 The most common treatments for these complaints include both nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids.3,7,8,10–16 Steroids provide some advantages over NSAIDs-steroids produce a wider anti-inflammatory response than NSAIDs and are less expensive; however, they also produce an increased risk of intraocular pressure (IOP) elevation and their frequent dosing schedule may result in poor patient compliance and adherence. NSAID use alone, however, has been associated with corneal melts and ocular discomfort.11,17–19 In the US, it is common practice for ophthalmologists to use a combination of NSAIDs and corticosteroids, although the American Academy of Ophthalmology states NSAID use in postoperative cataract patients remains controversial5 and the increased positive effect of adding NSAIDs to topical corticosteroids may simply be the result of additional dosing.20 Corticosteroids, on the other hand, are a well-accepted effective treatment for ocular inflammation3,17,21 The mechanism of action is similar among all corticosteroids: anti-inflammatory effects achieved through suppression of vascular endothelial cell adhesion molecules, cyclooxygenase I or II, and through cytokine expression.22
There are several topical corticosteroids commonly used in the US to treat postoperative pain and inflammation after ocular surgery: Topical difluprednate 0.05% is approved for use but dosed 4 times daily; topical dexamethasone 0.1%, prednisolone acetate 1.0%, and loteprednol 1.0% have been used off-label to manage postoperative inflammation.21 Loteprednol 1%23 is currently approved as a twice-daily suspension; loteprednol 0.38% is approved as a 3-times-daily medication.24,25 Difluprednate ophthalmic emulsion 0.05% is approved for 4-times-daily use.26 Dexamethasone is approved as an insert; therefore, there is no additional dosing.9,27
There is currently no topical ophthalmic corticosteroid approved specifically to treat both postoperative inflammation and prevention of pain after cataract surgery in the US; all the approved indications are for a more generalized “ocular surgery”.28–31
SURF-201 is a novel, topical ophthalmic formulation of the corticosteroid betamethasone sodium phosphate (BSP) 0.2% that is delivered in a buffered, isotonic, aqueous, non-preserved proprietary solution intended for the treatment of postoperative inflammation and prevention of ocular pain in patients who are undergoing cataract surgery.32 Betamethasone has been used worldwide since the early 1960s, albeit not in ophthalmic form. Studies from the 1990s suggest BSP might be an effective ophthalmic medication.33,34
The vehicle used in SURF-201 comprises chondroitin sulfate (a glycosaminoglycan); this vehicle was co-developed in the 1990s by one of our authors (RLL) and has been shown to be able to stabilize cell membranes and reduce corneal edema.35
The use of preservatives in topical ophthalmic medications is common, as is knowledge of their detractors—including cytotoxic and inflammatory effects that may lead to or exacerbate dry eye.8,16,36–40 Betamethasone has been approved for use in the United States since 1961, although only the injectable suspension remains on the market; Celestone Soluspan (betamethasone acetate and BSP) is marketed and approved for use in various inflammatory indications.41 In Europe, however, BSP is approved as topical formulation, with dosing regimen of 4–8 times a day (and at a lower concentration, 0.1%, than SURF-201).42 SURF-201 comprises a higher concentration (0.2%) than other formulations, a reduced frequency of dosing (BID), and has a similar potency to dexamethasone43–46 but a potentially better safety profile. However, dexamethasone is a suspension41,47 whereas BSP is an aqueous solution, with the latter eliminating patient errors with mixing suspensions. BSP acts within hours; suspensions are designed to work over a longer time frame (days or weeks).48
The purpose of this study was to compare SURF-201 BID to vehicle BID in patients undergoing routine cataract surgery. The primary efficacy outcome was the difference in the proportion of subjects with anterior chamber cell (ACC) grade 0 in the SURF-201 active treatment group versus the vehicle group only at Day 15. Secondary outcomes included pain scores and overall safety. The study was registered on ClinicalTrials.gov: NCT04324359.
Methods
This was a phase 2, multicenter, randomized (1:1 ratio), double-masked, vehicle-controlled, parallel-group study undertaken in adult subjects 18 years of age and older who were scheduled to undergo uncomplicated cataract surgery without the aid of a femto (femtosecond) laser. The study consisted of a 16-day dosing phase (Day -1 from surgery through Day 15 postoperatively), followed by a 2‑week evaluation phase (Days 22 and 32). Subjects were provided with a study drug kit per their randomized treatment assignment and given instruction on both dosing at home and on how to complete a dosing and pain assessment diary. Subjects scheduled for cataract surgery were instructed to instill a dose of their assigned treatment BID, preferably 8‑12 hours apart, for 16 days beginning the day before cataract surgery (Day -1), 1 dose administered at least 1 hour prior to cataract surgery (on Day 0) and 1 dose on the evening after cataract surgery, and then 2 doses administered each day for through Day 15; patients were re-evaluated on Days 22 and 32 to ensure no rebound inflammation (included in the safety analysis).
Some of the key inclusion criteria for subjects: Assigned uncomplicated unilateral cataract surgery (either phacoemulsification or extracapsular extraction; the planned use of a femtosecond laser served as an exclusionary criterion); a best-corrected visual acuity (BCVA) of at least +1.0 log of the minimum angle of resolution (logMAR) (Snellen equivalent of 20/200) in the non-study eye (fellow eye); an intraocular pressure (IOP) of >8 mmHg and ≤ 22 mmHg in the study eye, and the ability to self-instill or have a caregiver would could instill the medications. Some of the key exclusion criteria included: intraocular inflammation or ocular pain above a score of 0 in either eye prior to surgery; any extraocular inflammation in the study eye prior to surgery (blepharitis was allowed if only scurf was present without any concurrent conjunctivitis or lid erythema/edema) or ongoing uveitis, or signs of iritis or scleritis; history of diabetic retinopathy and/or previous vitrectomy in the study eye within the last 2 years prior to screening; a diagnosis of severe dry eye, Fuchs’ dystrophy, guttata, or chalazion in the study eye; a history of glaucoma or retinal surgery; previous refractive surgery; planned additional ocular surgery (eg, femtosecond laser-assisted cataract surgery, limbal relaxing incisions, mechanical pupillary expanders, minimally invasive glaucoma surgery); a history of herpes simplex infection in either eye; active corneal, conjunctival or canalicular pathology (including ocular infection [bacterial, viral, or fungal]) in the study eye. Specifically, active viral diseases of the cornea and conjunctiva including epithelial herpes simplex keratitis (dendritic keratitis), vaccinia, and varicella, and also in mycobacterial infection of the eye and fungal diseases of the ocular structures (such as fungal keratitis).
Subjects were randomized in a 1:1 ratio to receive SURF-201 or vehicle for 16 days BID. The proprietary vehicle is a buffered, isotonic, aqueous, non-preserved solution that has shown promise in studies on dry eye (data on file, Surface Ophthalmics).
Assessments
Evaluations of efficacy included biomicroscopic examinations for anterior chamber cells and flare and a Visual Analog Scale (VAS) of ocular pain as recorded in the subject diary. The primary efficacy endpoint was the proportion of subjects who had cleared ocular inflammation (anterior chamber cell score of 0) at Day 15. The VAS was used to evaluate eye pain/discomfort at screening Visit 1 (Day -14 to Day -2) and at Visit 3 through Visit 7 (Day 1 through Day 32); scoring from 0 to 100 using a mark on a 100 mm line (0 = absent; 100 = maximum). Pain was evaluated before each study drug dose using a pain scale that subjects completed at home. In addition to the VAS, subjects were asked to assess their study eye pain level prior to each study drug dose via a diary at home. For this, VAS descriptive FACES were combined with the dosing diary. Table 1 shows the grading scales for inflammation, while Table 2 and Figure 1 show the VAS and grading scale used to analyze ocular pain.
 |
Table 1 Anterior Chamber Cell and Flare Grading |
 |
Table 2 Ocular Pain Scale |
 |
Figure 1 VAS descriptive faces. |
A worsening of 3 lines or more in logMAR score in the study eye from baseline or any prior visit was deemed an adverse event (AE) and noted as such. An increase from baseline or any prior study visit of 10 mmHg or more in IOP in the study eye was also considered an AE. An IOP of 30 mmHg or higher were reported as a serious AE (SAE).
Safety Analyses
The safety endpoints of the study were AEs, BCVA, IOP, and biomicroscopic and ophthalmoscopic findings. Objective signs of ocular inflammation, including chemosis, bulbar conjunctival injection, ciliary injection, corneal edema, and keratic precipitates, were evaluated according to a 0–3 grading scale.
The protocol was in compliance with Good Clinical Practices (GCP) and the Declaration of Helsinki (1996) and in accordance with applicable Institutional Review Board (IRB) regulations [United States 21 Code of Federal Regulations (US 21 CFR) part 56.103]; Advarra IRB (6100 Merriweather Dr, Ste. 600, Columbia, MD) granted IRB approval. Study participants gave informed consent prior to initiation of any study-related procedures. The study was performed in compliance with informed consent regulations (US 21 CFR part 50).
Statistical Analysis
The Intent-to-Treat (ITT) population included all randomized subjects who underwent routine uncomplicated unilateral cataract surgery. Subjects in the ITT population were analyzed in the treatment group to which they were assigned by the randomization scheme, regardless of which study drug they received. The safety population included all randomized subjects who received at least 1 dose of the study drug. All data processing, summarization, and analyses were performed using the CRO’s SAS Environment/Version 9.4 (or later) of the SAS statistical software package.
The primary efficacy analysis tested for a difference in the proportion of subjects with ACC grade 0 in the SURF-201 active treatment group versus the vehicle group at Day 15. An ACC grade of 0 was considered a success, and an ACC grade > 0 or the use of rescue medication prior to Day 15 was considered a failure. Missing data was imputed using last observation-carried-forward (LOCF).
The secondary efficacy endpoint for the study was the proportion of subjects who achieved a pain score of 0 at each post-surgical VAS (0–100 mm scale) assessment (Days 1, 8, 15, 22, and 32).
Results
Patient Demographics and Characteristics
A total of 91 patients were screened and enrolled: 45 subjects were randomized to the SURF-201 treatment group, and 46 subjects were randomized to the vehicle treatment group. All but 5 (11.1%) subjects in the SURF-201 treatment group and 3 (6.5%) subjects in the vehicle treatment group who were randomized were treated. A total of 83 subjects (40/45 [88.9%] in the SURF-201 group and 43/46 [93.5%] subjects in the vehicle group) were randomized, treated, and underwent cataract surgery; these subjects were included in the safety population. A total of 82/91 (90.1%) subjects were included in the ITT population, including 39/45 (86.7%) and 43/46 (93.5%) subjects in the SURF-201 and the vehicle treatment groups, respectively. There were no statistically significant differences in baseline demographics or characteristics between the two groups. The median age at screening for those in the SURF-201 group was 68 years (range 52 to 83 years), and the majority (27/39, 69.2%) were female (ITT population). Subjects in the vehicle treatment group had a median age of 69 years at screening (range 50 to 90 years), and the majority (25/43, 58.1%) were female (ITT population). Baseline characteristics are listed in Table 3, and Supplemental Figure 1 provides the full subject disposition.
 |
Table 3 Summary of Demographic Characteristics, Intent-to-Treat Population |
Efficacy
Cell and Flare
The primary efficacy outcome was the number/percentage of patients with an ACC grade 0 at Day 15. In the ITT population, a higher proportion of subjects in the SURF-201 treatment group had an ACC grade of 0 at Day 15 (n=22/39 [56.4%]) compared to subjects in the vehicle treatment group (n=9/43 [20.9%]). The difference was statistically significant (P<0.001). These differences were noted as early as Day 8, when 13/39 (33.3%) of patients in the SURF-201 group and 4/41 (9.8%) of patients in the vehicle group had an ACC grade of 0. The difference observed was statistically significant (P=0.010 based on the Barnard’s exact test). There were no statistically significant differences between groups at Day 22 or Day 32.
These outcomes were similar in the per protocol (PP) population as well, with 25/38 (65.8%) of patients in the SURF-201 group and 16/39 (41%) in the vehicle group achieving an ACC grade of 0 at Day 15 (P=0.032). There were statistically significant differences first noted at Day 8 that continued through Day 15 between the two groups; there were no statistically significant differences at Day 22 or Day 32.
Additionally, a similar proportion of subjects in each ITT treatment group achieved an anterior chamber flare (ACF) grade of 0 at each of the time points assessed (on Days 1, 8, 15, 22 and 32); there was only a statistical difference on Day 15 (P=0.031) that favored the SURF-201 group. There were no statistical differences between the PP groups at any time point. Table 4 shows the percentage of patients an ACC and ACF grade of 0 at each study visit in the ITT population.
 |
Table 4 Anterior Chamber Cell and Flare Outcomes at Each Study Visit, Intent-to-Treat Population |
Pain Scores
There was no statistical significance between the groups in the proportion of subjects who achieved a VAS pain score of 0 at any post-surgical assessment. Although not statistically significant, at Day 1 there was a 20% difference in the VAS pain score of 0 between the SURF-201 group (69.2%) and the vehicle group (48.8%) in the ITT population, while there was a 20.9% difference in the VAS pain score of 0 between the two groups in the PP population (data on file). Table 5 shows the proportion of patients with a pain score of 0 at each study visit in the ITT population.
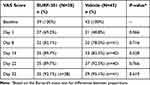 |
Table 5 Proportion of Patients with a Visual Analog Scale Pain Score of 0 at Each Study Visit, Intent-to-Treat Population |
Patients were asked to self-report pain via a subject diary, using a scale of 1 (no pain) to 5 (extreme pain). The proportion of subjects reporting an absence of eye pain occurred similarly on Day 0 in both treatment groups (n=38/39 [97.4%] prior to the morning dose and n=18/39 [46.2%] prior to the evening dose with SURF-201, versus n=40/42 [95.2%] prior to the morning dose and n=20/41 [48.8%] prior to the evening dose with vehicle). Regardless of treatment group, the median eye pain level assessed prior to the morning and evening dose from Day 1 to 14 did not worsen over time. A consistently higher proportion of patients in the SURF-201 group reported a “no pain” score before each dose than the vehicle group through Day 8, after which more than 90% of patients in each group reported “no pain” at both dosing time points.
Safety
A total of 50/83 (60.2%) subjects reported at least 1 AE, with a slightly higher incidence of AEs occurring in subjects in the SURF-201 treatment group (n=27/40 [67.5%]) compared to the vehicle treatment group (n=23/43 [53.5%]).
AEs were treatment emergent in 26/40 (65.0%) and 23/43 (53.5%) subjects in the SURF-201 and vehicle groups, respectively. The majority of AEs that occurred were ocular events, occurring in 26/40 (65.0%) and 22/43 (51.2%) subjects in the SURF-201 and vehicle groups, respectively. All ocular AEs were considered treatment emergent, with the exception of 1 ongoing event of posterior capsule opacification in the fellow eye, which was first reported during the screening period in 1 subject in the SURF-201 treatment group.
Six patients in the SURF-201 group and 14 patients in the vehicle group discontinued treatment early, primarily because of a lack of efficacy in the vehicle group and for treatment-emergent AE (TEAE) in the SURF-201 group. However, one patient in the SURF-201 group was reported by an investigator as having a TEAE (conjunctival hyperemia) related to the study drug; none of the TEAEs in the vehicle group were considered to be related to the treatment.
The majority of AEs that occurred during the study were mild (occurring in 25 [30.1%] subjects, overall) to moderate (occurring in 21 [25.3%] subjects, overall) in severity. Moderate severity AEs occurred in 12/40 (30.0%) subjects treated with SURF-201 and in 9/43 (20.9%) subjects treated with vehicle. All other AEs were considered by the investigator to be mild. Severe TEAEs were only reported in the vehicle treatment group, occurring in 4/43 (9.3%) subjects.
Severe ocular TEAEs included corneal edema, symblepharon, and eye inflammation. All severe ocular TEAEs recovered and were considered by the investigator to be unrelated to study drug. In the vehicle treatment group, Subject 003–005 had a severe ocular TEAE of corneal edema on Day 1 that resolved by Day 15 with no intervention and did not lead to study discontinuation. A severe TEAE of symblepharon on Day 7 resulted in the early discontinuation of study drug in 1 subject (Subject 003–011) in the vehicle treatment group. Treatment was also discontinued early due to a severe TEAE of eye inflammation that occurred on Day 6 in 1 subject (Subject 052–001) in the vehicle treatment group and resulted in administration of rescue medication and required anterior chamber washout.
There were no statistically significant differences in reported AEs between the two groups. There were, however, three ocular SAEs, which were believed to be unrelated to the study drug. One patient discontinued treatment, another withdrew from the study, and the third developed cystoid macular edema, which occurred on Day 33. There were no non-ocular SAEs. Table 6 lists any AE, SAE, or TEAE that occurred in more than 5% of either group in the safety population.
 |
Table 6 Adverse Events, Safety Population |
Rescue Medications
The administration of rescue medication occurred in half of the subjects in the ITT population (n=41/82 [50.0%]). Rescue medications were administered to treat a higher proportion of subjects in the vehicle group (n=25/43 [58.1%]) compared to subjects in the SURF-201 group (n=16/39 [41.0%]). All patients who discontinued the study drug/vehicle received rescue medication (predominantly prednisolone, nepafenac, difluprednate, ketorolac, bromfenac, or sodium chloride).
IOP
The mean IOP mmHg value at baseline was similar in both treatment groups (16.1±2.80 mmHg in the SURF‑201 treatment group and 15.9±2.84 mmHg in the vehicle treatment group).
Clinically significant increases in IOP of 10 mmHg or more from baseline or prior visit occurred in the SURF-201 treatment group at Day 1 (n=2/40 [5.0%]), Day 8 (n=2/39 [5.1%]), and Day 15 (n=1/39), and in 1 subject in the vehicle treatment group only at Day 22. There were no subjects with clinically significant increases in IOP at the Day 32 assessment. In the SURF-201 group, the greatest increases in IOP (18 mmHg and 17 mmHg) were seen in 2 subjects at Day 1; both subjects were treated with IOP-lowering medication, and the events resolved. The other 3 occurrences of increased IOP were transient, considered mild and were not treated. Table 7 presents the mean IOP in each safety group at each follow-up point.
 |
Table 7 Mean Intraocular Pressure at Each Study Visit, Safety Population |
BCVA
At baseline, BCVA was 0.355 logMAR in the SURF-201 group and 0.358 logMAR in the vehicle group. Throughout the study period, BCVA remained similar between the two groups. At Day 15, 18/39 eyes in the SURF-201 group (46.2%) and 14/40 eyes in the vehicle group (35%) gained 3 or more lines, and 8/39 eyes in the SURF-201 group (20.5%) and 11/40 eyes in the vehicle group (27.5%) lost at least one line. At the final study visit on Day 32, gains of ≥3 lines were observed in 21/40 in the SURF-201 group (55.3%) and 24/43 in the vehicle group (58.5%). Differences in BCVA logMAR score were not statistically significantly different between groups.
Discussion
This phase 2, randomized, vehicle-controlled study evaluating the efficacy and safety of SURF-201 dosed BID for 1 day prior to cataract surgery, the day of cataract surgery, and 14 days post-cataract surgery, found the study drug produced a statistically significant proportion of patients achieved an ACC score of 0 on Day 15 compared to patients in the vehicle group: 66.7% to 40% (P=0.019). Further, a higher percentage of patients in the SURF-201 group were pain-free at Day 1 compared to those in the vehicle group, and the proportion of patients in the SURF-201 group who remained pain-free throughout the study period was consistently higher than the proportion of patients in the vehicle group who remained pain-free. By Day 8, 94.3% of patients in the SURF-201 group and 80.6% of those in the vehicle group were pain free before the morning dose, and 91.2% of patients in the SURF-201 group and 93.8% of those in the vehicle group were pain free before the evening dose.
Overall, the study drug was well tolerated, with no new safety signals identified. A higher incidence of AEs occurred in patients in the SURF-201 group (67.5%) compared to the vehicle group (53.5%), but the incidence of TEAEs was similar: 5% and 7% in the SURF-201 and vehicle groups, respectively.
To the authors’ knowledge, this is the first study to report on 0.2% BSP in a proprietary vehicle for the treatment of postoperative inflammation and prevention of pain after cataract surgery. There is a multitude of studies in the literature on the use of corticosteroids (dropless, submicron suspension, or topical) and NSAIDs post-cataract surgery,7,8,10,11,13,16,19,25,49–56 with topical corticosteroid use much more common than other forms. Topical corticosteroid therapy in the postoperative period remains the standard of care, despite concerns about patient adherence/compliance and potential bottle tip contamination.18,19 However, no statistically significant differences have been found when comparing “dropless surgery”—where the surgeon is responsible for delivering postoperative medications at the end of the cataract procedure—to topical steroid use in the postoperative period.57,58
Although we did not conduct any head-to-head studies between SURF-201 and another topical corticosteroid, our findings are similar to other published studies on postoperative corticosteroid use. Donnenfeld et al found intracameral dexamethasone suspension in two different doses cleared inflammation at a much higher rate than placebo at Day 8 postop (63.1% and 66% compared to 25%),52 which was also a higher rate than in this study at Day 8 (33.3% in the study drug eye). In a separate study on the same formulation of dexamethasone, at Day 8, 51.6% had an ACC grade of 0.3 These findings are in alignment with a real-world observational study on the dexamethasone intraocular suspension 9%, where an ACC grade of 0 was achieved by 49/71 patients (69%) at Day 8 and 30/32 patients (93.7%) at Day 14 for patients who received intraocular dexamethasone only.59
Lee et al evaluated a different formulation of dexamethasone (an intracanalicular plug) and found more patients with complete ACC clearance at Day 8 (22.4%) and at Day 14 (42.7%) than placebo;60 our study had a much higher percentage at Day 8 (33.3%) and at Day 15 (66.7%). Pain scores fared similarly: at Day 8, 79.2% and at Day 14, 80.6% were pain free with the insert60 (in our study, 82.1% at Day 8 and 89.7% at Day 15 were pain-free). The plug is designed for a tapered release over 28 days,60 however, while our topical formulation is under evaluation to be used for 14 days post-surgery, although our study results suggest treatment may not be necessary beyond Day 8 postoperatively.
A European study on a combination of dexamethasone 0.1%/netilmicin 0.3% (the latter is an antibiotic) ophthalmic gel BID found 88.2% of patients had an ACC score of 0 at Day 7 in the ITT group (89.7% in the PP group), but that study did not address the prevention of pain.61
Another corticosteroid, loteprednol etabonate (LE) ophthalmic suspension 1%23–25 is approved for the more generic “ophthalmic surgery”, but results from Kim et al on postoperative cataract surgery showed patient ranges from 20.7% to 31.2% of complete ACC resolution at Day 8 that was maintained through Day 15; 53.6% to 57.1% of patients had complete resolution of pain at Day 8 that was maintained through Day 15.23 Fong et al compared a twice-daily submicron LE gel formulation (n=133) to 3-times daily gel (n=139) and found complete ACC resolution on Day 8 of 26.9% and 28.7%, respectively, and 73.7% and 73.1%, respectively, with grade 0 pain on Day 8.25 Fong et al conducted a subsequent study that pooled data from two Phase 3 studies (n=742 ITT population) and found more patients in the LE gel 0.38% TID group compared with the vehicle group had complete resolution of AC cells (29.6% vs 15.1%) and grade 0 pain (74.4% vs 48.8%) at day 8 (P<0.0001 for both).24
Korenfeld et al evaluated difluprednate to vehicle and found 33/110 (30%) in the BID group and 36/103 (34.9%) in the QID group achieved ACC grade of 0 at Day 8, increasing to 55.5% in the BID group and 63.1% in the QID group.26 Similarly, a higher percentage of patients were pain-free at Day 8 and 15 in the QID group compared to the BID group.26 Garg et al62 reported similar findings (but dosing was 6 times daily): at week 1, 50% (n=25) had ACC grade of 0; at week 2, 82% had ACC score of 0 at week 1, 86% (n=43) had pain score of grade 1; at week 2, 90% had pain score of grade 1.
Still others have investigated betamethasone in particular: Dieleman et al showed single subconjunctival betamethasone acetate injection (5.7 mg/mL) appears to be a useful alternative to prolonged postoperative administration of dexamethasone eyedrops in controlling intraocular inflammation and development of macular edema after phacoemulsification.58 [It is important to note BSP—the formulation we evaluated—acts within hours, whereas betamethasone acetate is a suspension that is slowly absorbed over approximately 2 weeks].48
As with most other corticosteroid formulations, the most frequently reported ocular AEs in our study (namely, increased IOP and anterior segment inflammation) are consistent with the type of events typically observed after cataract surgery.
It is well accepted that older patients have difficulty instilling topical medications properly,11,18,63 and the reduced dosing schedule (twice daily) of our formulation may be able to help alleviate those obstacles to proper dosing.
There are few limitations to this study, one of which is the length of the study period. Other studies evaluating topical corticosteroids have had a longer postoperative evaluation,3,11 but the authors of this study believe our findings would remain the same even with a longer follow-up. At the last visit (Day 32) in our current study, 91.9% of those in the SURF-201 group and 95% of those in the vehicle group were pain-free, and 86.5% of those in the SURF-201 group and 95% of those in the vehicle group had an ACC score of 0.
This limitation is more than overcome by the rapid clearance of ACC and ACF, as well as the diminution of pain in the SURF-201 group.
Conclusion
SURF-201 is an effective topical, preservative-free corticosteroid (dosed BID) for the treatment of postoperative inflammation and prevention of pain in a post-cataract population.
Data Sharing Statement
All reasonable requests for the data used in this study will be made available upon request to the corresponding author.
Acknowledgments
The abstract has been presented in part at AECOS 2021 Deer Valley, Utah. Michelle Dalton, ELS, Dalton & Associates, Inc., provided medical writing; this was funded by Surface Ophthalmics, Inc.
Funding
Surface Ophthalmics, Inc. funded this study.
Disclosure
KH is an employee of Surface Ophthalmics; RLL and KH are members of the board of Surface Ophthalmics, Inc. RLL also reports personal fees from Alcon and Allegro during the conduct of the study. SG, HR, TW are paid investigators for Surface Ophthalmics, Inc. The authors report no other conflicts of interest in this work.
References
1. Burton MJ, Ramke J, Marques AP, et al. The lancet global health commission on global eye health: vision beyond 2020. Lancet Glob Health. 2021;9(4):e489–e551. doi:10.1016/S2214-109X(20)30488-5
2. GBD Blindness and Vision Impairment Collaborators, Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the right to sight: an analysis for the global burden of disease study. Lancet Glob Health. 2021;9(2):e144–e160. doi:10.1016/S2214-109X(20)30489-7
3. Donnenfeld ED, Solomon KD, Matossian C. Safety of IBI-10090 for inflammation associated with cataract surgery: phase 3 multicenter study. J Cataract Refract Surg. 2018;44(10):1236–1246. doi:10.1016/j.jcrs.2018.07.015
4. National Eye Institute. NEI charts a clearer future for cataract prevention and treatment; 2017. Available from: https://www.nei.nih.gov/about/news-and-events/news/nei-charts-clearer-future-cataract-prevention-and-treatment.
5. American Academy of Ophthalmology Cataract and Anterior Segment Panel. Preferred practice pattern guidelines: cataract in the adult eye; 2021.
6. Rossi T, Romano MR, Iannetta D, et al. Cataract surgery practice patterns worldwide: a survey. BMJ Open Ophthalmol. 2021;6(1):e000464. doi:10.1136/bmjophth-2020-000464
7. Donnenfeld E. Current use of non-steroidal anti-inflammatory drugs in the treatment of ocular inflammation related to cataract surgery. Eur Ophthal Rev. 2012;6(3):173–177.
8. Hovanesian JA, Donnenfeld ED. Intracameral dexamethasone 9% vs prednisolone acetate 1% in controlling postoperative pain and inflammation in patients undergoing cataract surgery. J Cataract Refract Surg. 2022;48(8):906–911. doi:10.1097/j.jcrs.0000000000000887
9. Walters T, Bafna S, Vold S, et al. Efficacy and safety of sustained release dexamethasone for the treatment of ocular pain and inflammation after cataract surgery: results from two Phase 3 studies. J Clin Exp Ophthalmol. 2016;7(4):1.
10. Shorstein NH, Myers WG. Drop-free approaches for cataract surgery. Curr Opin Ophthalmol. 2020;31(1):67–73. doi:10.1097/ICU.0000000000000625
11. Erichsen JH, Forman JL, Holm LM, Kessel L. Effect of anti-inflammatory regimen on early postoperative inflammation after cataract surgery. J Cataract Refract Surg. 2021;47(3):323–330. doi:10.1097/j.jcrs.0000000000000455
12. Flach AJ. Topical nonsteroidal antiinflammatory drugs in ophthalmology. Int Ophthalmol Clin. 2002;42(1):1–11.
13. Flach AJ. Treatment of postoperative inflammation in ophthalmology. J Toxicol Cutaneous Ocul Toxicol. 2008;10(4):253–277. doi:10.3109/15569529109052135
14. Schalnus R. Topical nonsteroidal anti-inflammatory therapy in ophthalmology. Ophthalmologica. 2003;217(2):89–98. doi:10.1159/000068563
15. Simone JN, Whitacre MM. Effects of anti-inflammatory drugs following cataract extraction. Curr Opin Ophthalmol. 2001;12(1):63–67.
16. Donnenfeld ED, Holland EJ, Solomon KD. Safety and efficacy of nepafenac punctal plug delivery system in controlling postoperative ocular pain and inflammation after cataract surgery. J Cataract Refract Surg. 2021;47(2):158–164. doi:10.1097/j.jcrs.0000000000000414
17. van Rensburg EJ, Meyer D. Astute and safe use of topical ocular corticosteroids in general practice: practical guidelines. Afr J Online. 2013;31(4):127–129.
18. An JA, Kasner O, Samek DA, Levesque V. Evaluation of eyedrop administration by inexperienced patients after cataract surgery. J Cataract Refract Surg. 2014;40(11):1857–1861. doi:10.1016/j.jcrs.2014.02.037
19. Shah TJ, Conway MD, Peyman GA. Intracameral dexamethasone injection in the treatment of cataract surgery induced inflammation: design, development, and place in therapy. Clin Ophthalmol. 2018;12:2223–2235. doi:10.2147/OPTH.S165722
20. Kim SJ, Schoenberger SD, Thorne JE, Ehlers JP, Yeh S, Bakri SJ. Topical nonsteroidal anti-inflammatory drugs and cataract surgery: a report by the American Academy of Ophthalmology. Ophthalmology. 2015;122(11):2159–2168. doi:10.1016/j.ophtha.2015.05.014
21. Grob SR, Gonzalez-Gonzalez LA, Daly MK. Management of mydriasis and pain in cataract and intraocular lens surgery: review of current medications and future directions. Clin Ophthalmol. 2014;8:1281–1289. doi:10.2147/OPTH.S47569
22. Rizzo S, Gambini G, De Vico U, Rizzo C, Kilian R. A one-week course of levofloxacin/dexamethasone eye drops: a review on a new approach in managing patients after cataract surgery. Ophthalmol Ther. 2022;11(1):101–111. doi:10.1007/s40123-021-00435-1
23. Kim T, Sall K, Holland EJ, Brazzell RK, Coultas S, Gupta PK. Safety and efficacy of twice daily administration of KPI-121 1% for ocular inflammation and pain following cataract surgery. Clin Ophthalmol. 2019;13:69–86. doi:10.2147/OPTH.S185800
24. Fong R, Cavet ME, DeCory HH, Vittitow JL. Loteprednol etabonate (submicron) ophthalmic gel 0.38% dosed three times daily following cataract surgery: integrated analysis of two Phase III clinical studies. Clin Ophthalmol. 2019;13:1427–1438. doi:10.2147/OPTH.S210597
25. Fong R, Silverstein BE, Peace JH, Williams JI, Vittitow JL. Submicron loteprednol etabonate ophthalmic gel 0.38% for the treatment of inflammation and pain after cataract surgery. J Cataract Refract Surg. 2018;44(10):1220–1229. doi:10.1016/j.jcrs.2018.06.056
26. Korenfeld MS, Silverstein SM, Cooke DL, Vogel R, Crockett RS; Difluprednate Ophthalmic Emulsion 0.05% Study Group. Difluprednate ophthalmic emulsion 0.05% for postoperative inflammation and pain. J Cataract Refract Surg. 2009;35(1):26–34. doi:10.1016/j.jcrs.2008.09.024
27. Tyson SL, Bafna S, Gira JP, et al. Multicenter randomized phase 3 study of a sustained-release intracanalicular dexamethasone insert for treatment of ocular inflammation and pain after cataract surgery. J Cataract Refract Surg. 2019;45(2):204–212. doi:10.1016/j.jcrs.2018.09.023
28. Lotemax [package insert]. (Bausch & Lomb Incorporated); 2013.
29. Durezol [package insert] (Alcon Laboratories, Inc.); 2016.
30. Lotemax [package insert] (Bausch & Lomb, Inc.); 2016.
31. Inveltys [package insert] (Kala Pharmaceuticals); 2018.
32. Surface Ophthalmics. Surface ophthalmics announces positive top-line results from Phase II Trial for SURF-201 (Betamethasone 0.2% in Klarity® vehicle) for the treatment of post-cataract surgery pain and inflammation; 2021. Available from: https://www.prnewswire.com/news-releases/surface-ophthalmics-announces-positive-top-line-results-from-phase-ii-trial-for-surf-201-betamethasone-0-2-in-klarity-vehicle-for-the-treatment-of-post-cataract-surgery-pain-and-inflammation-301212617.html.
33. Corbett MC, Hingorani M, Boultom JE, Shilling JS. Subconjunctival betamethasone is of benefit after cataract surgery. Eye. 1993;7:744–748.
34. Shah SM, McHugh JD, Spalton DJ. The effects of subconjunctival betamethasone on the blood aqueous barrier following cataract surgery: a double-blind randomised prospective study. Br J Ophthalmol. 1992;76(8):475–478. doi:10.1136/bjo.76.8.475
35. Lindstrom RL, Kaufman HE, Skelnik DL, et al. Optisol corneal storage medium. Am J Ophthalmol. 1992;114(3):345–356. doi:10.1016/s0002-9394(14)71803-3
36. Trattler WB, Majmudar PA, Donnenfeld ED, McDonald MB, Stonecipher KG, Goldberg DF. The Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO) study: the effect of dry eye. Poster. Clin Ophthalmol. 2017;11:1423–1430. doi:10.2147/OPTH.S120159
37. Kasetsuwan N, Satitpitakul V, Changul T, Jariyakosol S. Incidence and pattern of dry eye after cataract surgery. PLoS One. 2013;8(11):e78657. doi:10.1371/journal.pone.0078657
38. Kwon JW, Chung YW, Choi JA, La TY, Jee DH, Cho YK. Comparison of postoperative corneal changes between dry eye and non-dry eye in a murine cataract surgery model. Int J Ophthalmol. 2016;9(2):218–224. doi:10.18240/ijo.2016.02.06
39. Yu Y, Hua H, Wu M, et al. Evaluation of dry eye after femtosecond laser-assisted cataract surgery. J Cataract Refract Surg. 2015;41(12):2614–2623. doi:10.1016/j.jcrs.2015.06.036
40. Porela-Tiihonen S, Kaarniranta K, Kokki M, Purhonen S, Kokki H. A prospective study on postoperative pain after cataract surgery. Clin Ophthalmol. 2013;7:1429–1435. doi:10.2147/OPTH.S47576
41. Celestone Soluspan [package insert] (Merck Sharp & Dohme Corp.); 2018.
42. Betnesol eye, ear and nose drops solution 0.1% [package insert]. (RPH Pharmaceuticals); 2017.
43. Arthur KE, Wolff JC, Carrier DJ. Analysis of betamethasone, dexamethasone and related compounds by liquid chromatography/electrospray mass spectrometry. Rapid Commun Mass Spectrom. 2004;18(6):678–684. doi:10.1002/rcm.1386
44. Fung AT, Tran T, Lim LL, et al. Local delivery of corticosteroids in clinical ophthalmology: a review. Clin Exp Ophthalmol. 2020;48(3):366–401. doi:10.1111/ceo.13702
45. National Health Service. Corticosteroids; 2023. Available from: https://southwest.devonformularyguidance.nhs.uk/formulary/chapters/11.-eye/11-1-2-inflammatory-eye-conditions/11-4-1-corticosteroids.
46. Corticosteroids and the Eye; 2023. Available from: https://www.formularywkccgmtw.co.uk/therapeutic-sections/eye/inflammatory-eye-conditions/corticosteroids-and-the-eye/.
47. Maxidex [package insert] (Alcon Laboratories, Inc.); 2017.
48. Dreyer SJ, Beckworth WJ. Commonly used medications in procedures. In: Lennard TA, Walkowski S, Singla AK, Vivian DG, editors. Pain Procedures in Clinical Practice.
49. Aragona P, Postorino EI, Aragona E. Post-surgical management of cataract: light and dark in the 2020s. Eur J Ophthalmol. 2021;31(2):287–290. doi:10.1177/1120672120963458
50. Schechter BA. Use of topical bromfenac for treating ocular pain and inflammation beyond cataract surgery: a review of published studies. Clin Ophthalmol. 2019;13:1439–1460. doi:10.2147/OPTH.S208700
51. Cho H, Wolf KJ, Wolf EJ. Management of ocular inflammation and pain following cataract surgery: focus on bromfenac ophthalmic solution. Clin Ophthalmol. 2009;3:199–210.
52. Donnenfeld E, Holland E. Dexamethasone intracameral drug-delivery suspension for inflammation associated with cataract surgery: a randomized, placebo-controlled, Phase III trial. Ophthalmology. 2018;125(6):799–806. doi:10.1016/j.ophtha.2017.12.029
53. Foster B. Same-day versus next-day dexamethasone intracanalicular insert administration for inflammation and pain control following cataract surgery: a retrospective analysis. Clin Ophthalmol. 2021;15:4091–4096. doi:10.2147/OPTH.S335764
54. Fram N, Alsetri H, Shiler O, Paterno PJ, Cabang J. Retrospective study of a sustained-release intracanalicular dexamethasone insert for treatment of ocular inflammation after cataract and corneal surgery. Clin Ophthalmol. 2022;16:4065–4074. doi:10.2147/OPTH.S386702
55. Saenz B, Ferguson TJ, Abraham N, Mueller BH, Parkhurst GD. Evaluation of same-day versus next-day implantation of intracanalicular dexamethasone for the control of postoperative inflammation and pain following cataract surgery. Clin Ophthalmol. 2021;15:4615–4620. doi:10.2147/OPTH.S334297
56. Kim SJ, Patel SN, Sternberg P
57. Lindholm JM, Taipale C, Ylinen P, Tuuminen R. Perioperative subconjunctival triamcinolone acetonide injection for prevention of inflammation and macular oedema after cataract surgery. Acta Ophthalmol. 2020;98(1):36–42. doi:10.1111/aos.14175
58. Dieleman M, Wubbels RJ, van Kooten-Noordzij M, de Waard PW. Single perioperative subconjunctival steroid depot versus postoperative steroid eyedrops to prevent intraocular inflammation and macular edema after cataract surgery. J Cataract Refract Surg. 2011;37(9):1589–1597. doi:10.1016/j.jcrs.2011.03.049
59. Bacharach J, McCabe C, Jackson M, et al. First real-world, multicenter, post-marketing, retrospective study of dexamethasone intraocular suspension for inflammation after cataract surgery. Clin Ophthalmol. 2022;16:1783–1794. doi:10.2147/OPTH.S357267
60. Lee A, Blair HA. Dexamethasone intracanalicular insert: a review in treating post-surgical ocular pain and inflammation. Drugs. 2020;80(11):1101–1108. doi:10.1007/s40265-020-01344-6
61. Mencucci R, Ach T, Liekfeld A, et al. Reduced posology of an ophthalmic hydrogel containing dexamethasone/netilmicin to prevent and treat ocular inflammation after cataract surgery: efficacy and tolerability. Adv Ther. 2022;39(12):5474–5486. doi:10.1007/s12325-022-02295-y
62. Garg P, Tuteja N, Qayum S. To study the efficacy of difluprednate ophthalmic emulsion and prednisolone acetate ophthalmic suspension on post-operative inflammation in cataract surgery. J Clin Diagn Res. 2016;10(12):NC05–NC08. doi:10.7860/JCDR/2016/21690.9035
63. Schwartz GF, Hollander DA, Williams JM. Evaluation of eye drop administration technique in patients with glaucoma or ocular hypertension. Curr Med Res Opin. 2013;29(11):1515–1522. doi:10.1185/03007995.2013.833898
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
