Back to Journals » Journal of Pain Research » Volume 10
Xiaozhi decoction reduced posthemorrhoidectomy pain and analgesic medication consumption: a prospective study
Authors Shen JB, Luo XG, Zhou X, Tang CW, Ju HY, Xu YQ, Qin LJ
Received 23 November 2016
Accepted for publication 14 December 2016
Published 17 January 2017 Volume 2017:10 Pages 197—201
DOI https://doi.org/10.2147/JPR.S128500
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Enrica Santarcangelo
Jianbin Shen,1,* Xiagang Luo,2,* Xiao Zhou,3 Chengwu Tang,1 Huanyu Ju,2 Yongqiang Xu,1 Lianjin Qin1
1Department of General Surgery, First People’s Hospital Affiliated to Huzhou Normal College, Huzhou, Zhejiang, 2Department of General Surgery, The Second Affiliated Hospital of Nanjing Medical University, Nanjing, Jiangsu, 3Department of Orthopedics, People’s Hospital of Zhangqiu, Jinan, Shandong, People’s Republic of China
*These authors contributed equally to this work
Objective: The aim of this study was to investigate the effect of Xiaozhi decoction (XZD) on posthemorrhoidectomy pain and analgesic medication consumption.
Methods: From May 2013 to March 2015, 315 patients who underwent open hemorrhoidectomy in our hospital were enrolled in this study, of whom, 160 patients were randomly assigned to accept sitz bath with warm water after hemorrhoidectomy (control group) and 155 patients were randomly assigned to accept sitz bath with XZD (XZD group) after hemorrhoidectomy. Postoperative pain at 12 hours after surgery and on postoperative days (PODs) 1, 2, 7, 14 and 28 was evaluated by Visual Analog Scale (VAS). Pain on defecation on PODs 1, 2, 7, 14 and 28 was also recorded using the VAS. The consumption of analgesics was also analyzed.
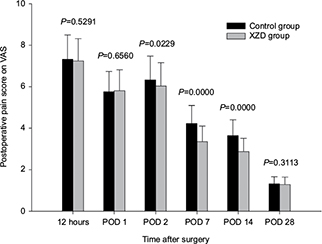
Results: No significant difference was found in baseline characteristics between the two groups. Postoperative pain score of the XZD group was significantly lower on POD 2 (6.04±1.11 vs 6.33±1.14, P=0.0229), POD 7 (3.35±0.75 vs 4.22±0.87, P=0.0000) and POD 14 (2.87±0.64 vs 3.64±0.77, P=0.0000) than that of the control group. Similarly, patients in the XZD group experienced significantly less pain on defecation on POD 2 (5.02±1.34 vs 5.43±1.56, P=0.0130), POD 7 (3.08±1.17 vs 3.52±1.29, P=0.0017) and POD 14 (2.31±0.85 vs 2.68±0.99, P=0.0004). Patients in the XZD group consumed significantly less analgesic medication on POD 2 (P=0.0136), POD 7 (P=0.0074) and POD 14 (P=0.0046) than the control group.
Conclusion: XZD could effectively relieve postoperative pain and reduce analgesic medication consumption after hemorrhoidectomy.
Keywords: hemorrhoids, hemorrhoidectomy, traditional Chinese medicine, posthemorrhoidectomy pain
Introduction
Hemorrhoids as one of the most common chronic anorectal diseases severely affect patients’ quality of life.1–3 Hemorrhoidectomy is utilized to treat severe hemorrhoids (especially for III or IV degree hemorrhoids) or hemorrhoids failing to respond to conservative therapies.4 However, hemorrhoidectomy is always associated with significant postoperative pain, which may make the patient and the surgeon anxious. Moreover, poor wound healing may retard return to work or daily activities.5 During the early period after hemorrhoidectomy, patients usually need analgesics medication to relieve postoperative pain and discomfort.6
Sitz bath with warm water was well accepted as a safe postoperative care after anal surgery and routinely utilized to relieve postoperative pain and promote wound healing during the posthemorrhoidectomy period.7,8 However, recent studies have revealed that warm sitz bath did not relieve pain, promote wound healing or reduce consumption of analgesics after anal surgery but offered only a significant relief in anal burning and a marginally higher satisfaction score.9,10 Traditional Chinese medicine (TCM) has been used to treat hemorrhoids for centuries in our country.11 Therefore, Chinese herbal decoction, Xiaozhi decoction (XZD), was added into sitz bath as posthemorrhoidectomy care in our clinical practice due to its positive effect on pain relief. The aim of the current prospective study was to clarify the efficacy of sitz bath with XZD as postoperative care for patients who underwent hemorrhoidectomy.
Methods
Patients
Between May 2013 and March 2015, 315 patients who underwent open hemorrhoidectomy in the First People’s Hospital affiliated to Huzhou Normal College were included in this prospective study. According to the computer-based sequential method, 160 patients were randomly assigned to accept sitz bath with warm water after hemorrhoidectomy (control group) and 155 patients were randomly assigned to accept sitz bath with XZD (XZD group) after hemorrhoidectomy.
Inclusion criteria were as follows: 1) age between 18 and 75 years and 2) indication for hemorrhoidectomy: symptomatic III and IV degree hemorrhoids. Patients who had associated fistula, anal fissure, inflammatory bowel disease, perineal skin inflammation, proctitis, pregnancy, previous anorectal surgery or allergy to the decoction were excluded from this study.
This study was approved by the ethics committee for medical research of the First People’s Hospital affiliated to Huzhou Normal College and was performed on the basis of the Declaration of Helsinki and “Good Clinical Practice” guidelines. All participants signed the written informed consent.
Treatment
All patients underwent a standard Milligan–Morgan hemorrhoidectomy by the same surgeon under standard general anesthesia. After surgery, metronidazole tablets were administrated at a dose of 250 mg, twice a day for 1 week. Analgesic tablets containing a combination of tramadol hydrochloride 37.5 mg and paracetamol 325 mg (Ultracet; Xian Janssen Pharmaceutical Ltd., Xian, People’s Republic of China) were prescribed as needed but not more than four tablets each day.
Sitz bath was begun on postoperative day (POD) 1 and lasted for 7 days. Patients accepted sitz bath for 15 min each time, twice a day, once in the morning after defecation and another just before bedtime. Patients in the control group accepted sitz bath with warm water alone, while in the XZD group 100 mL of XZD was added into the warm water.
The composition of XZD (Table 1) consisted of Flos Chrysanthemi Indici 10.0 g, Radix Sophorae Flavescentis 10.0 g, Herba Taraxaci 10.0 g, Mirabilitum 10.0 g, Rhizoma Corydalis 10.0 g, Olibanum 10.0 g, Myrrha 10.0 g, Galla Chinensis 10.0 g, Radix et Rhizoma Rhei 7.5 g, Flos Carthami 5.0 g and Radix Glycyrrhizae 3.0 g. All the herbs were decocted in 1000 mL of water and finally condensed into 100 mL of decoction.
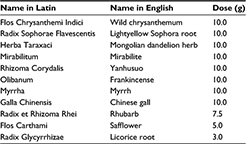  | Table 1 Components of XZD with Latin and English names Abbreviation: XZD, Xiaozhi decoction. |
Outcome measurements and follow-up
Patients were monitored and discharged within 72 hours after surgery. All patients were followed up after discharge from the hospital via phone. Postoperative pain at 12 hours after surgery and on PODs 1, 2, 7, 14 and 28 was evaluated by Visual Analog Scale (VAS) scored 0 (no pain) to 10 (very severe pain). Pain on defecation on PODs 1, 2, 7, 14 and 28 was also recorded using the VAS. The number of analgesic tablets consumed by each patient per day was also recorded and analyzed.
Statistical analysis
The measurement data were represented as mean ± SD and were compared using two-sample t-test. Enumeration data were analyzed using adjusted c2-test. Ridit analysis was used to compare the distributions of ranked data, such as the degree of hemorrhoids, posthemorrhoidectomy and analgesic consumption of the two groups. SPSS 21.0 (IBM China Investment Co. Ltd., Beijing, People’s Republic of China) statistical software was adopted for data analyzing. A P-value of <0.05 was considered statistically significant.
Results
Baseline characteristics
No statistical difference was found in baseline characteristics between the two groups, in terms of age, gender, body mass index (BMI), hemorrhoidal disease duration, operation duration or degree of hemorrhoids (Table 2).
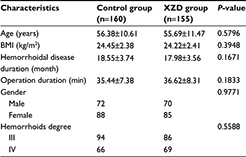  | Table 2 Baseline characteristics Abbreviations: BMI, body mass index; XZD, Xiaozhi decoction. |
Posthemorrhoidectomy pain
Postoperative pain did not differ between the two groups at 12 hours after surgery (XZD group: 7.24±1.08 vs control group: 7.32±1.17, P=0.5291) or on POD 1 (XZD group: 5.80±1.01 vs control group: 5.75±0.98, P=0.6560). Moreover, no significance was found in pain on defecation on POD 1 between the two groups (XZD group: 4.19±1.04 vs control group: 4.22±1.12, P=0.8057). After initiation of sitz bath with XZD, postoperative pain score of the XZD group decreased and was significantly lower on POD 2 (6.04±1.11 vs 6.33±1.14, P=0.0229), POD 7 (3.35±0.75 vs 4.22±0.87, P=0.0000) and POD 14 (2.87±0.64 vs 3.64±0.77, P=0.0000) than that of the control group (Figure 1). Similarly, patients in the XZD group experienced significantly less pain on defecation on POD 2 (5.02±1.34 vs 5.43±1.56, P=0.0130), POD 7 (3.08±1.17 vs 3.52±1.29, P=0.0017) and POD 14 (2.31±0.85 vs 2.68±0.99, P=0.0004) than those of the control group (Figure 2). As a result of reduced posthemorrhoidectomy pain by the XZD, patients in the XZD group consumed significantly less analgesic medication on POD 2 (P=0.0136), POD 7 (P=0.0074) and POD 14 (P=0.0046) than the control group (Table 3).
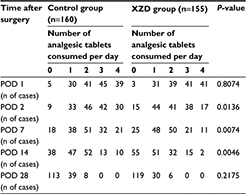  | Table 3 Posthemorrhoidectomy analgesic consumption Abbreviations: n, number; POD, postoperative day; XZD, Xiaozhi decoction. |
Discussion
Hemorrhoidectomy is a standard treatment for extensive hemorrhoids and usually causes significant postoperative pain which would harm postoperative quality of life.12 Posthemorrhoidectomy pain is mainly caused by surgical incision per se and tissue inflammation related to bacterial infiltration of the wound.13 In the first few hours after hemorrhoidectomy, wound inflammation is the primary cause of pain, while during the days after hemorrhoidectomy bacterial infiltration mainly causes the posthemorrhoidectomy pain. Another factor of posthemorrhoidectomy pain could be spasm of the internal sphincter which is always aggravated by wound inflammation, swelling and infection during the PODs.14
In our clinical practice, sitz bath with XZD was routinely performed after hemorrhoidectomy and was found effective for pain relief and wound healing. In its composition, Flos Chrysanthemi Indici primarily diminishes tissue swelling, complemented by Mirabilitum. Rhizoma Corydalis and Flos Carthami remove blood stasis and relief pain. Galla Chinensis and Herba Taraxaci help to clear wound infection. Olibanum and Myrrha promote wound healing. Radix Sophorae Flavescentis and Radix Glycyrrhizae have antiphlogistic effect. Radix et Rhizoma Rhei promotes defecation. Theoretically, the XZD could not only directly relieve postoperative pain but also diminish the major adverse factors such as wound inflammation, swelling and infection which cause postoperative pain after hemorrhoidectomy.
In the current study, we found that patients in the XZD group experienced significantly less postoperative pain and pain on defecation and consumed less analgesic medication than those in the control group on PODs 2, 7 and 14.
Conclusion
The Chinese herbal decoction, XZD, could effectively relieve postoperative pain and reduce analgesic medication after hemorrhoidectomy. Because of the open-label nature and small sample size of this study, further double-blind, placebo-controlled studies with larger sample size are required to verify our results. In addition, more investigation is needed to figure out the potential mechanisms of therapeutic effects of XZD.
Author contributions
Jianbin Shen, Chengwu Tang, Xiagang Luo and Lianjin Qin designed the study and wrote the manuscript. Yongqiang Xu and Chengwu Tang performed management and monitoring of patients. Xiao Zhou, Lianjin Qin and Huanyu Ju collected and analyzed the data. All authors contributed toward data analysis, drafting and revising the article and agreed to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Sneider EB, Maykel JA. Diagnosis and management of symptomatic hemorrhoids. Surg Clin North Am. 2010;90(1):17–32. Table of Contents. | ||
Lorenzo-Rivero S. Hemorrhoids: diagnosis and current management. Am Surg. 2009;75(8):635–642. | ||
Hollingshead JR, Phillips RK. Haemorrhoids: modern diagnosis and treatment. Postgrad Med J. 2016;92(1083):4–8. | ||
Moult HP, Aubert M, De Parades V. Classical treatment of hemorrhoids. J Visc Surg. 2015;152(2 suppl):S3–S9. | ||
Karanlik H, Akturk R, Camlica H, Asoglu O. The effect of glyceryl trinitrate ointment on posthemorrhoidectomy pain and wound healing: results of a randomized, double-blind, placebo-controlled study. Dis Colon Rectum. 2009;52(2):280–285. | ||
Khubchandani IT. Internal sphincterotomy with hemorrhoidectomy does not relieve pain: a prospective, randomized study. Dis Colon Rectum. 2002;45(11):1452–1457. | ||
Ramler D, Roberts J. A comparison of cold and warm sitz baths for relief of postpartum perineal pain. J Obstet Gynecol Neonatal Nurs. 1986;15(6):471–474. | ||
Janicke DM, Pundt MR. Anorectal disorders. Emerg Med Clin North Am. 1996;14(4):757–788. | ||
Gupta PJ. Effects of warm water sitz bath on symptoms in post-anal sphincterotomy in chronic anal fissure--a randomized and controlled study. World J Surg. 2007;31(7):1480–1484. | ||
Gupta PJ. Warm sitz bath does not reduce symptoms in posthaemorrhoidectomy period: a randomized, controlled study. ANZ J Surg. 2008;78(5):398–401. | ||
Wang YJ, Hua GH. Observation of curative effect of hemorrhoids lotion on pain, edema and bleeding after anorectal surgery. Zhongguo Zhong Yao Za Zhi. 2015;40(22):4497–4500. | ||
Hsu KF, Chia JS, Jao SW, et al. Comparison of clinical effects between warm water spray and sitz bath in post-hemorrhoidectomy period. J Gastrointest Surg. 2009;13(7):1274–1278. | ||
Ala S, Saeedi M, Eshghi F, Mirzabeygi P. Topical metronidazole can reduce pain after surgery and pain on defecation in postoperative hemorrhoidectomy. Dis Colon Rectum. 2008;51(2):235–238. | ||
Eshghi F, Hosseinimehr SJ, Rahmani N, Khademloo M, Norozi MS, Hojati O. Effects of Aloe vera cream on posthemorrhoidectomy pain and wound healing: results of a randomized, blind, placebo-control study. J Altern Complement Med. 2010;16(6):647–650. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.