Back to Journals » Chronic Wound Care Management and Research » Volume 2
Wound pruritus: pathophysiology and management
Authors Paul J
Received 14 March 2015
Accepted for publication 4 June 2015
Published 12 August 2015 Volume 2015:2 Pages 119—127
DOI https://doi.org/10.2147/CWCMR.S70360
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Prof. Dr. Marco Romanelli
Julia C Paul
School of Nursing, Oakland University, Rochester, MI, USA
Purpose: The objective of this article is to review literature on wound pruritus, with a focus on summarizing pathophysiology and management.
Method: Literature related to the physiology of itch was reviewed. PubMed, MEDLINE, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Embase were searched for all research studies written in English which include “wound” (injury/burn) and “pruritus” (itch) in the title or abstract. Articles were accepted if they involved wounds or acute burns. Literature related to options for management of wound pruritus was reviewed.
Results: While all types of wounds can be the source of associated pruritus, most studies have been done concerning pruritus associated with burns. There are treatment options for pruritus which can be considered for management of wound pruritus.
Conclusion: Further research is indicated to gain insights into the problem of wound pruritus. As more is learned about the physiology of wound pruritus, more effective management strategies can be developed and employed.
Keywords: wound, chronic itch, C-fibers, spinothalamic tract, positron emission tomography, pruritogens
Introduction to wound pruritus
The objective of this article is to review literature on wound pruritus, with a focus on summarizing pathophysiology and management. A similar review was completed by Upton et al.1 This review, however, focuses on literature about open wounds with itching (and not closed or healed wounds).
Itch is an irritation of the skin, which can be as distressing as pain. There is no established treatment protocol for itch; and even after nearly a century of investigation, “many mysteries, misconceptions, and controversies still haunt this rather neglected yet clinically important” sensation.2 “Itch is the least understood and researched of the somatosensory modalities”.3 Rapid progress is being made in understanding the mechanisms underlying the itch sensation,4 but more needs to be learned about the physiology of itch before more appropriate treatments can be developed.5 Itch involves multiple body systems, including the integumentary, nervous, endocrine, and immune systems.5,6
In the 1600s, Samuel Hafenreffer, a German physician, defined itch as “an unpleasant sensation that elicits the desire to scratch”.7 Greaves and Khalifa8 described itch as “a complex, multidimensional experience involving a range of different qualities of sensation, such as pleasurable relief by local physical intervention, which leads to itch/scratch cycles and modulation by cognitive and psychological functions from higher centers”. Itch can be defined as “1) an irritation of the skin, 2) an impatient desire: a hankering”.9 Stedman’s Medical Dictionary10 defines itch as “an irritating sensation in the skin that arouses the desire to scratch” and defines pruritus as “itching”. While pruritus has been specified as itch without a particular cause or without apparent skin changes, itch is synonymous with pruritus.5,10–12 Pruritus is generally considered a sensation of the skin, but wound pruritus is related to wounds, which are often through the skin and deeper than the skin.5 Wound itch or wound pruritus is “the irritating sensation or disturbing feeling related to an open wound, including the wound bed and the skin immediately surrounding the open wound”.5
Chronic wounds
The etiology of chronic wounds may be vascular (arterial and venous), neuropathic, traumatic, pressure related, or mixed.5 Pruritus has been found with all of these wound types.5,13 Burn injuries are also a source of pruritus, with as many as 87% of adults with burns reporting pruritus.14 That these wounds are considered “chronic” wounds should not necessarily indicate lengthy duration.5 Chronic wounds “have failed to proceed through an orderly and timely process to produce anatomic and functional integrity, or proceeded through a repair process without sustaining an anatomic and functional result” as indicated by Paul5 and Lazarus et al.15 Chronic wounds become suspended in the inflammatory phase of healing.16 Pruritus can be so annoying that the person with a chronic wound gives in to the urge to scratch, which can traumatize the wound bed and surrounding skin.5 Prevention of wound deterioration and promotion of healing is crucial.
Classification of itch
The classification of itch based on duration or source has proven to be inadequate. Acute itch can last from seconds to a week.17 Chronic itch is generally considered as that itch which lasts longer than 6 weeks.18 Twycross et al19 proposed a classification system for itch based on underlying mechanism; this has been used successfully. In this classification system, itch can be pruritoceptive (peripheral, cutaneous, dermatological), neurogenic (central, caused by systemic disorders), neuropathic (from diseased neurons as in multiple sclerosis), psychogenic (mind-related, as with parasitosis), and mixed (with overlapping causes). Pathophysiological conditions can trigger multiple types of itch.
Theoretical frameworks for itch
Several theories exist related to the processes involved in transmission of the itch sensation from the skin to the brain: the intensity theory, the labeled line or specificity theory, and the selectivity theory.3 The intensity theory regarding neurons which are weakly or strongly activated to produce both painful and itchy stimuli, depending on the intensity, is no longer considered viable.20
The selectivity theory assumes that neurons are selective for itch as well as pain. This model involves neurons that can differentiate nociceptive stimuli from pruritogenic stimuli.3,20
The labeled line (or specificity) theory assumes that there are itch-specific neurons separate from pain-specific neurons.3,20 Itch-specific spinal neurons are recognized, with itch-specific peripheral neurons recently reported.3,20,21
Physiology of pruritus
For many years pruritus was considered a lesser form of pain, with the same physiological pathways as pain.5,13 In 1997, neurons specific for pruritus were identified in humans.5,13,22,23 Pruritus can be induced by analgesics or hindered by painful stimuli.5,10,22 The skin contains afferent C-fibers which are slow-conducting and similar in appearance to, yet functionally different from, pain fibers.5,13,24 The primary neurons (histamine-sensitive and mechano-insensitive) synapse via dorsal root ganglia with second-order neurons in the dorsal horn of the spinal cord.2,5,11,19,24 Unlike pain, itch does not provoke a spinal reflex.25 The secondary neurons cross over to join the contralateral spinothalamic tract (STT) and ascend to the thalamus, where they synapse with third-order neurons for transmission to the somatosensory cortex of the postcentral cingulate gyrus.11,19,25 The C-fibers are sensitive to histamine, growth factors, and other pruritogens, which may be present in open wounds.5,19,25,26
Sun and Chen27 examined thermal, mechanical, inflammatory, and neuropathic pain responses in gastrin-releasing peptide receptor (GRPR)-mutant mice and found that there was no difference in responses when compared to responses of unaltered wild-mice to noxious stimuli. Scratching behavior was induced with injection of compound 48/80 (a mast cell degranulator), a type-2 proteinase-activated receptor (PAR-2) agonist (a mediator of itch in human skin), and chloroquine into both groups of mice. PAR-2 and chloroquine are believed to act independently of histamine, and the reduction in scratching behavior was much more apparent with PAR-2 agonist (P<0.05) and chloroquine (P<0.01) than with compound 48/80. The number of scratches was significantly less in the GRPR mutant mice in response to injection of known pruritogens. Those differences were not found with pain-inducing agents. Intrathecal injection of GRPR agonist induced dose-dependent scratching behavior. Swain28 noted that gastrin-releasing peptide (GRP) participated in transmission of the itch sensation, but not in the pain sensation. GRP was found in a small subset of dorsal root ganglion neurons with expression of its receptor restricted to lamina I of the dorsal spinal cord, consistent with the current model of central processing of itch sensation.
Neuronal pathways for itch
Sensory receptors in the skin include free and corpuscular nerve endings. Corpuscular endings include both nonencapsulated Merkel’s touch spots and encapsulated receptors.29 The free nerve endings of unmyelinated C-fibers and small myelinated A-fibers are the sensory fibers in humans. These free nerve endings are found in the papillary dermis and epidermis.25 Interestingly, itch is not inducible where epidermis has been removed,29 so itch sensed within wounds is difficult to explain. Itch is specific to the skin, mucus membranes, and cornea.30
Schmelz et al22 reported iontophoresis, with histamine inducing the itch sensation.5,13 The itch-sensing neuronal units demonstrated mechanical insensitivity, slow conduction velocities (average of 0.5 m/s), and large innervation territories.5,13,22 Johanek et al31 compared skin reaction to histamine, with skin reaction to cowhage spicules.5,13 The cowhage spicules produced less vasodilation. Additionally, topical capsaicin eliminated cowhage-induced itch but not histamine-induced itch, implicating a separate group of itch-sensitive neurons.5,13,31
Andrew and Craig32 used histamine on the lumbosacral spinal cords of 33 anesthetized cats to categorize neurons into functional categories. They were able to demonstrate a functionally unique subset of histamine-selective lamina I SST neurons in the cats, which match the response of human neurons to the itch sensation. The matched response supports the notion of itch as a specific sensation. The conduction velocities of the histamine-sensitive neurons were significantly slower than the conduction velocities of the other neurons, and their electrical thresholds were higher.
No single “itch center” in the brain has been identified.33 Positron emission tomography (PET) has enabled the study of supraspinal processing of itch.34 The multidimensionality of itch is indicated as multiple areas of the brain are activated when itch is induced. Drzezga et al35 used PET scanning to study the central processing of histamine-induced itch. They noted significant activation of contralateral somatosensory cortex, as well as contralateral and ipsilateral motor areas, but no thalamic activation. Yosipovitch et al34 saw that with histamine skin pricks, the anterior cingulate cortex, supplementary motor area, and inferior parietal lobe are activated. That the limbic and motor areas are activated supports the clinical observation that itch elicits the desire to scratch.
Itch-specific peripheral neurons have recently been reported.3,21 Neurons in the dorsal root ganglia of mice, which exclusively innervated the epidermis, were genetically manipulated and labeled so that response to pruritogens could be determined.21
Studies of scratching have added further to the understanding of pruritus. Scratching is controlled by an area of the medulla.25,30 Scratching has been imitated by repetitively moving a cytology brush over an area with enough force to bend the skin-facing brush bristles (equivalent to 29× g of force on a digital scale).36 Yosipovitch et al36 used functional magnetic resonance imaging (fMRI) on 13 healthy human subjects who received scratching stimuli to the right lower leg. They determined that scratching may mediate inhibition of itch by deactivating the anterior cingulate cortex and posterior cingulate cortex, providing relief by suppressing the emotional components of itch. The cerebellum has been associated with motor and sensory coordination, and activation of this area as was seen in the scratch study may result from its sensory coordination activities.36 Davidson et al37 examined whether responses to histamine in primate (monkey) STT neurons could be inhibited by scratching in the receptive field. They found that scratching provides relief of itch by reduction in the discharge rate of STT neurons, which are responding to an itch-producing stimulus. Yosipovitch et al38 had 21 healthy subjects rate histamine-induced itch sensation with innocuous warmth, innocuous cooling, noxious cold, and noxious heat applied distal to the area of histamine iontophoresis. Scratching, noxious heat, and noxious cold significantly reduced ratings of itch intensity.38
In contrast to pain, pruritus elicits a protective attack and removes response.2,5,13 The itch–scratch cycle is initiated when a person scratches in response to a pruritic stimulus.5,13,25,39 Scratching causes an inflammatory response, so nerve fibers are further stimulated to cause continued itching and scratching. While scratching and rubbing can provide relief, both can also cause scratch marks and further injury.5,13,25,39
Pruritogens
A number of endogenous and exogenous pruritogens (itch triggers) have been identified. These pruritogens may be found in the body of the itching person, in the wound bed, or may be in the environment of the itching person. Itch response to the various pruritogens varies between individuals. The discussion of pruritogens which follows is not exhaustive, as it is possible for any stimulus to trigger itch.
Endogenous pruritogens
Histamine
Histamine is released as degranulation of dermal mast cells occurs and directly stimulates histamine type 1 (H1) receptors on itch-specific C-fibers.19 Histamine is often used to elicit itch as, the reaction to histamine is predictable. The reaction includes an itch which begins 30–45 seconds after histamine application and resolves over 10–15 minutes, a wheal which develops over 8 minutes, and a surrounding flare. The wheal and flare are specifically histamine mediated.
Leknes et al40 used fMRI to compare allergen- and histamine-induced itch in terms of skin blood flow changes and central processing. Responses to skin prick tests done with histamine and allergens on 14 healthy subjects were compared. Both types of itch correlated with activity in the anterior cingulate, striatum, and thalamus. Additionally, itch elicited by allergens resulted in activation of orbitofrontal, supplementary motor, and posterior parietal areas. Histamine-induced itch resulted in activation of the insula bilaterally. Allergen-induced itch was perceived as more intense and enduring (P<0.005), while histamine-induced itch intensity faded more quickly. Perceived itch intensity and blood flow occurred significantly later in response to allergen-induced itch than to histamine-induced itch (P<0.001).
Acetylcholine
Acetylcholine is a neurotransmitter which, via muscarinic and nicotinergic receptors, causes pain in nonatopic persons, but itch in atopic persons.19 Apparently, the activation of itch units by acetylcholine does not provoke itch in nonatopic persons due to simultaneous activation of nonitch receptors that suppress the itch.41 A flare response to intradermal acetylcholine is less than, but similar to, that induced by histamine.
Serotonin
Serotonin induces itch via 5-HT3 receptors.25 Selective serotonin reuptake inhibitors have antipruritic effects.42 Serotonin is a mediator in psychogenic itch.7
Bradykinin
Bradykinin, and its receptors, lowers the receptor threshold and causes pain.42 However, bradykinin induces mast cell degranulation for the release of histamine and enhances histamine responses, so contributes to the itch sensation.25
Prostaglandins
Prostaglandins potentiate histamine-induced itch by lowering the receptor threshold to histamine and papain.25,42
Interleukins
Interleukins (IL-2, IL-4, IL-6, and IL-31) are cytokines which originate in T cells and macrophages.7 Interleukins play a role in the elicitation of itch, similar to histamine, by activating the cutaneous C-fibers.25 IL-31 induces pruritic dermatitis in mice.7 The role of interleukins in itch behavior is still being determined.
Nerve growth factor
The role of nerve growth factor is speculative, but it may lead to sensitization of peripheral nerve fibers.42 A direct correlation between nerve growth factor and pruritus has not been found, but increased plasma levels of nerve growth factor have been found in patients with atopic dermatitis.25 Nerve growth factor is elevated in traumatized tissue.43
Substance P
Substance P (neurokinin1) is a neuropeptide, released from sensory nerve fibers by PAR-2, and appears to potentiate itch by releasing histamine from dermal mast cells.8,19 Topical capsaicin depletes substance P from cutaneous nerve terminals and destroys C-fibers to relieve itch.
Stress
There is some understanding of neurogenic inflammation and the influence of stress on pruritic skin conditions.44 Neurotrophic factors such as nerve growth factor which can modify expression of inflammatory cytokines by mast cells have been found to be stress inducible. Also, there is evidence that, in stress states, keratinocytes influence nonmyelinated nerve fibers in the epidermis through β-endorphin production by proopiomelanocortin.
Exogenous pruritogens
Chemical stimuli
Botanicals including poison ivy, stinging nettles, and cowhage spicules induce itch. Latex, a plant derivative, can cause pruritus. Cosmetics and soaps can cause irritant and allergic reactions. Insect bites and parasite infestations (ie, scabies) are familiar pruritogens. Many drugs, including opiates, aspirin, and β-blockers can induce pruritus without a rash.45
Physical stimuli
In addition to chemical pruritogens, there are numerous physical stimuli that can elicit itch. Light touch, pressure, suction, heat, and electrical stimulation can induce itch.46 Wool fibers, fiberglass, and water (“aquagenic pruritus”) can cause itching in some people.45
Research related to wound pruritus
PubMed, MEDLINE, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Embase were searched for all research studies written in English, which include wound (injury/burn) and pruritus (itch) in the title or abstract. Articles were accepted if they involved wounds or acute burns. Many studies regarding pruritus of healed burns were excluded. Table 1 gives a summary of the studies involving wound pruritus (Table 1).
  | Table 1 Summary of research studies related to wound itch |
Management of wound pruritus
The studies reviewed confirm the presence of wound-related pruritus as a clinical problem requiring intervention. Treatment options are available for chronic pruritus as recently described.47 Pruritus associated with burns was reduced with histamine type 2 (H2) antagonist with antihistamine,26 relaxation exercises,48 paraffin and colloidal bath oil,49 antiepileptic use,50 and antinausea/antivomiting medication,51 indicating usefulness of pharmacologic and nonpharmacologic therapies for burn wounds. Topical therapies are typically used to treat localized itch.52 The management of pruritus must be based on the physiology of the underlying cause of the itch and must be individualized.52 While all methods for preventing and treating itch might not be appropriate for the various itchy wounds, options which might be considered are discussed. Many of the treatment options available for managing itch are only appropriate for use once the wounds have healed.50 The wound base and periwound skin must be considered. As more is understood about wound itch, more appropriate interventions can be made to manage wound itch.
Pharmacological agents
Cooling agents
Menthol, camphor, and icilin (a newly developed substance) activate channels of the TRP (vanilloid) family and induce cold sensation, which temporarily masks the sensation of pruritus.42 Cold relieves pruritus by activating A-delta fibers which inhibit C-fiber activity.53 Icilin is 400–800 times more active in bioassay endpoints than menthol and has proven to be effective against pruritus in a number of cases.53 Cooling of an itchy area provides only short-term relief, and long-term effects of coolant use for itch management are not known.47
Corticosteroids
Topical corticosteroids as used for inflammation would not benefit noninflammatory itch and may have local side effects with prolonged use.52
Anesthetics
Capsaicin acts via vanilloid (TRPV1) receptors to induce burning pain or pruritus.25 With topical application for several days, capsaicin desensitizes nerve fibers for relief of itch.42 Pramoxine and eutectic mixture of lidocaine and prilocaine have been used.42,47,52,54
Antihistamines
Sedating antihistamines including hydroxyzine, doxepin, and diphenhydramine have been used with mixed results.47,52,54
Anticonvulsants
Gabapentin may act by blocking postsynaptic calcium channels or inhibiting neurotransmitter synthesis.42 Pregabalin acts similarly but with more tolerable adverse effects.42
Antidepressants
Several antidepressant drugs have proven to be effective antipruritics. Doxepin has potent antihistamine H1 receptor properties.55 Mirtazapine has noradrenergic and serotonergic as well as H1-antihistaminic properties.55 Paroxetine and sertraline, selective serotonin reuptake inhibitors, target sodium- and calcium-dependent transporters which inhibit uptake of neuromediators (ie, serotonin) into presynaptic cell bodies, so there is increased serotonin acting on postsynaptic receptors, resulting in antipruritic effects.42
Opioid and cannabinoid peptides
Cannabinoids originate from epidermal keratinocytes and neurons and have analgesic and antipruritic effects via cannabinoid receptors.7 Opioids also originate from neurons and keratinocytes and can be antipruritic in the skin. Systemic opioids induce pruritus as already discussed. Naloxone and naltrexone, drugs that block opiate receptors, have been used to treat cholestatic pruritus.8
Chemotherapy
Oral chemotherapy (ie, azathioprine and cyclosporine) and topical immunosuppressants (ie, tacrolimus and pimecrolimus) can be tried in cases of treatment-resistant pruritus.34,42,52 Photochemotherapy and phototherapy (UVB, ultraviolet B radiation) have been effective in some cases.34
Zangrado
This red, blood-like sap is produced by cutting the bark of the Sangre de Grado tree, which is found in the jungles of the upper Amazon.56 The sap can be applied topically or taken orally for antipruritic therapy. It appears to act via vanilloid receptor antagonism54 and has shown unparalleled effectiveness against the itch of insect bites.56
Nonpharmacological measures for treatment of pruritus
Most of the nonpharmacological measures listed in Table 2 are familiar and rather self-explanatory. Chronic rubbing and scratching result in secondary skin lesions including excoriations, lichenification, and scars.42 Rubbing and scratching should be avoided, especially where there is already a wound. Table 2 explains the nonpharmacological measures for controlling itch.
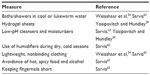  | Table 2 Nonpharmacological measures to control itch |
Transcutaneous electrical nerve stimulation
Transcutaneous electrical nerve stimulation (TENS) involves central inhibition of nerve conduction at the level of the spinal cord. A stimulator generates alternating current through flat rubber electrode plates inducing pressure and vibration. Low-frequency TENS has been found to reduce itch significantly in some cases.57
Cutaneous field stimulation
Cutaneous field stimulation is a newer technique which involves a flexible rubber electrode plate covered with 16 needle-like electrodes. When the plate is pressed gently onto the skin, the electrode tips enter the epidermis and superficial layer of the dermis. A constant current is delivered to each electrode, causing prickling and a slight burning pain so that itch is abolished for up to 2 hours after treatment.57
Broad-band UVB radiation therapy
Radiation therapy has proven to be effective in some cases.8
Psychological treatment approaches
A recent review of psychological treatment options for wound pruritus includes suggestion, relaxation training, massage, habit reversal, and behavioral programs.58
Relaxation
Farahani et al48 found that, compared to controls, itching, pain, and vital signs were significantly reduced postintervention in a group of patients with burns who underwent 20 minutes of muscle relaxation (P<0.5).
Massage
Skin massage including classic effleurage (stroking and gliding), petrissage (kneading), and tapotement (percussion) was applied to 18 persons with partial- or full-thickness burns on the hands or forearms by certified skin rehabilitation nurses for 30 minutes once a week and daily by the primary caregiver at home for 3 months and resulted in reduced pruritus (P=0.006) and depression (P=0.007) compared to controls.59 Massage therapy twice a week for 15 minutes each session reduced pain, itching, and anxiety levels associated with burn injuries in 32 adolescents, with 11%–20% body surface area burns, compared to controls (P<0.001).60
Behavioral programs
Psychological comorbidities frequently accompany chronic pruritus, so behavioral programs including stress training, training in social competence, and relaxation techniques are indicated.42 A nursing program intended to minimize itch and help the person cope with itch is described.61 The program was developed in the Netherlands for an outpatient dermatology department of a hospital. The program consists of educational and cognitive behavioral interventions, including patient education, awareness training and habit reversal, relaxation exercises, and ongoing patient support. A pretest–posttest design was used to examine the effectiveness of the intervention. No changes were found in quality of life, but frequency and intensity of itching and scratching, reduction in catastrophizing and helpless coping, and reduction in skin-related psychosocial morbidity were found.
Summary regarding management of wound pruritus
Pharmacological and nonpharmacological options for itch management are available and can be individualized based on wound-associated symptoms. Topical and systemic therapies are available and have been shown to be effective, particularly with burns. Therapies for pruritus related to other wound types must be studied. Wounds as the source or cause of localized itch pose a dilemma in terms of usual treatment for localized itch, which might include at first, moisturizers, emollients, antihistamine creams, and topical corticosteroids; then systemic therapies; and then combination topical and systemic therapy.52,62 As more is known about itch physiology, advances in itch therapy can be made.
Conclusion
Further research is required to gain insights into the problem of wound pruritus. As more is learned about the physiology of wound pruritus, more effective management strategies can be developed and employed.
Disclosure
The author reports no conflicts of interest in this work.
References
Upton D, Richardson C, Andrews A, Rippon M. Wound pruritus: prevalence, aetiology and treatment. J Wound Care. 2013;22(9):501–508. | |
Paus R, Schmelz M, Biro T, Steinhoff M. Frontiers in pruritus research: scratching the brain for more effective itch therapy. J Clin Invest. 2006;16(5):1174–1185. | |
Garibyan L, Rheingold CG, Lerner EA. Understanding the pathophysiology of itch. Dermatol Ther. 2013;26(2):86–91. | |
Tawa MC. 7th World Congress on Itch. J Dermatol Nurses’ Assoc. 2014;6(2):82–83. | |
Paul J. Characteristics of chronic wounds that itch. Adv Skin Wound Care. 2013;26(7):320–332. | |
Guarneri C, Terranova M, Terranova G, Guarneri F. The future: critical knowledge about anti-itch therapy. Dermatol Ther. 2005;18:363–365. | |
Ikoma A, Steinhoff M, Stander S, Yosipovitch G, Schmelz M. The neurobiology of itch. Nat Rev Neurosci. 2006;7:535–547. | |
Greaves MW, Khalifa N. Itch: more than skin deep. Inter Arch Allergy Immunol. 2004;135(2):166–172. | |
Hawkins JM, Allen R, editors. The Oxford Encyclopedic English Dictionary. Oxford, UK: Clarindon Press; 1991. | |
Stedman TL. Stedman’s Medical Dictionary. 28th ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2006. | |
Waxler B, Dadabhoy ZP, Stojiljkovic L, Rabito SF. Primer of postoperative pruritus for anesthesiologists. Anesthesiology. 2005;103:168–178. | |
Bernhard JD, editor. Itch: Mechanisms and Management of Pruritus. New York, NY: McGraw-Hill, Inc.; 1994. | |
Paul J. A cross-sectional study of chronic wound-related pain and itching. Ostomy Wound Manage. 2013;59(7):28–34. | |
VanLoey NE, Bremmer M, Faber AW, et al. Itching following burns: epidemiology and predictors. Br J Dermatol. 2008;158(1):95–100. | |
Lazarus G S, Cooper DM, Knighton DR, et al. Definitions and guidelines for assessment of wounds and evaluation of healing. Arch Dermatol. 1994;130:489–493. | |
Doughty DB, Sparks-Defries B. Wound-healing physiology. In: Bryant RA, Nix DP, editors. Acute and Chronic Wounds: Current Management Concepts. St Louis, MO: Mosby/Elsevier; 2007:307–336. | |
Yosipovitch G, Greaves MW. Definitions of itch. In: Yosipovitch G, Greaves MW, Fleischer AB Jr, McGlone F, editors. Itch: Basic Mechanisms and Therapy. New York, NY: Marcel Dekker, Inc.; 2004:1–4. | |
Stander S, Weisshaar E, Mettang T, et al. Clinical classification of itch: a position paper of the International Forum for the Study of Itch. Acta Derm Venereol. 2007;87:291–294. | |
Twycross R, Greaves MW, Handwerker H, et al. Itch: scratching more than the surface. QJM. 2003;96(1):7–26. | |
Patel TS, Dong X. An itch to be scratched. Neuron. 2010;68(4):334–339. | |
Han L, Ma C, Liu Q, et al. A subpopulation of nociceptors specifically linked to itch. Nat Neurosci. 2013;16(2):174–182. | |
Schmelz M, Schmidt R, Bickel A, Handwerker HO, Torebjork HE. Specific C-receptors for itch in human skin. J Neurosci. 1997;17(20):8003–8008. | |
Stander S, Schmelz M. Chronic itch and pain – similarities and differences. Eur J Pain. 2006;10(5):473–478. | |
Heymann WR. Itch. J Am Acad Dermatol. 2006;54(4):705–706. | |
Stander S, Steinhoff M, Schmelz M, Weisshaar E, Metze D, Luger T. Neurophysiology of pruritus: cutaneous elicitation of itch. Arch Dermatol. 2003;139:1463–1470. | |
Baker RA, Zeller RA, Klein RL, et al. Burn wound itch control using H1 and H2 antagonists. J Burn Care Rehabil. 2001;22(4):263–268. | |
Sun Y, Chen Z. A gastrin-releasing peptide receptor mediates the itch sensation in the spinal cord. Nature. 2007;448(7154):700–703. | |
Swain MG. Gastrin-releasing peptide and pruritus: more than just scratching the surface. J Hepatol. 2008;48:681–683. | |
Metze D. Skin nerve anatomy: neuropeptide distribution and its relationship to itch. In: Yosipovitch G, Greaves MW, Fleischer AB Jr, McGlone F, editors, Itch: Basic Mechanisms and Therapy. New York, NY: Marcel Dekker, Inc.; 2004:305–314. | |
Yosipovitch G, Papoiu AD. What causes itch in atopic dermatitis? Curr Allergy Asthma Rep. 2008;8:306–311. | |
Johanek LM, Meyer RA, Hartke T, et al. Psychophysical physiological evidence for parallel afferent pathways mediating the sensation of itch. J Neurosci. 2007;27(28):4790–4797. | |
Andrew D, Craig AD. Spinothalamic lamina I neurons selectively sensitive to histamine: a central neural pathway for itch. Nat Neurosci. 2001;4(1):72–77. | |
Darsow U, Drzezga A, Ring J. Central nervous system imaging of itch with PET. In: Yosipovitch G, Greaves MW, Fleischer AB Jr, McGlone F, editors. Itch: Basic Mechanisms and Therapy. New York, NY: Marcel Dekker, Inc.; 2004:63–70. | |
Yosipovitch G, Greaves M, Schmelz M. Itch. Lancet. 2003;362:690–694. | |
Drzezga A, Darsow U, Treede R, et al. Central activation by histamine-induced itch: analogies to pain processing: a correlational analysis of O-15 H2O positron emission tomography studies. Pain. 2001;92:295–305. | |
Yosipovitch G, Ishiuji Y, Patel TS, et al. The brain processing of scratching. J Invest Dermatol. 2008;128:1806–1811. | |
Davidson S, Zhang X, Khasabov SG, Simone DA, Giesler GJ Jr. Relief of scratching: State-dependent inhibition of primate spinothalamic tract neurons. Nat Neurosci. 2009;12(5):544–546. | |
Yosipovitch G, Duque MI, Fast K, Dawn AG, Coghill RC. Scratching and noxious heat stimuli inhibit itch in humans: a psychophysical approach. Br J Dermatol. 2007;156:629–634. | |
Yosipovitch G, Hundley JL. Practical guide lines for the relief of itch. Dermatol Nurs. 2004;16(4):325–328. | |
Leknes SG, Bantick S, Willis CM, Wilkinson JP, Wise RG, Tracey I. Itch and motivation to scratch: an investigation of the central and peripheral correlates of allergen- and histamine-induced itch in humans. J Neurophysiol. 2007;97:415–422. | |
Schmelz M, Handwerker HO. Neurophysiologic basis of itch. In: Yosipovitch G, Greaves MW, Fleischer AB Jr, McGlone F, editors. Itch: Basic Mechanisms and Therapy. New York, NY: Marcel Dekker, Inc.; 2004:5–12. | |
Pogatzki-Zahn E, Marziniak M, Schneider G, Luger TA, Stander S. Chronic pruritus: targets, mechanisms and future therapies. Drug News Perspect. 2008;21(10):541–551. | |
Schmelz M. Modulators of pruritus: peripheral and central sensitization. In: Misery L, Stander S, editors. Pruritus. London, UK: Springer-Verlag; 2010:22–29. | |
Gieler U, Niemeier V, Brosig B, Kupfer J. Psychosomatic aspects of pruritus. Psychosom Dermatol. 2002;3:6–13. | |
Yelverton CB, Yosipovitch G. Exogenous factors in the itch response. Curr Probl Dermatol. 2007;35:146–153. | |
McMahon SB, Koltzenburg M. Itching for an explanation. Trends Neurosci. 1992;15(12):497–501. | |
Yosipovitch G, Bernhard, JD. Chronic pruritus. N Engl J Med. 2013;368:1625–1634. | |
Farahani PV, Hekmatpou D, Khani SS. Effectiveness of muscle relaxation on pain, pruritus and vital signs of patients with burns. Iran J Crit Care Nurs. 2013;6(2):87–94. | |
Matheson J, Clayton J, Muller M. The reduction of itch during burn wound healing. J Burn Care Rehabil. 2001;22(1):76–81. | |
Mendham, JE. Gabapentin for the treatment of itching produced by burns and wound healing in children: a pilot study. Burns. 2004;30:851–853. | |
Gross S, Overbaugh R, Jansen R. Ondansetron for treating itch in healing burns. Internet J Pain Symptom Contr Palliat Care. 2006;5(1):4. | |
Elmariah SB, Lerner EA. Topical therapies for pruritus. Semin Cutan Med Surg. 2011;30(2):118–126. | |
Biró T, Ko MC, Bromm B, et al. How to fight that nasty itch – from new insights into the neuroimmunological, neuroendocrine, and neurophysiological bases of pruritus to novel therapeutic approaches. Exp Dermatol. 2005;14:225–240. | |
Weisshaar E, Kucenic M, Fleischer AB. Pruritus: a review. Acta Derm Venereol. 2003;213:5–32. | |
Greaves MW. Itch in systemic disease: therapeutic options. Dermatol Ther. 2005;18:323–327. | |
Miller MJS, Reuter BK, Wallace JL, Sharkey KA, Bobrowski P. Mechanistic and clinical assessment of Zangrado, an extract of the Amazonian ethnomedicinesangre de grado, for the treatment of itch. In: Yosipovitch G, Greaves MW, Fleischer AB Jr, McGlone F, editors. Itch: Basic Mechanisms and Therapy. New York, NY: Marcel Dekker, Inc.; 2004:305–314. | |
Wallengren J. Cutaneous nerve stimulation in the treatment of localized itch. In: Yosipovitch G, Greaves MW, Fleischer AB Jr, McGlone F, editors. Itch: Basic Mechanisms and Therapy. New York, NY: Marcel Dekker, Inc.; 2004:335–341. | |
Upton D, Penn F, Richardson C, Rippon M. Psychological management of wound pruritus. J Wound Care. 2014;23(6):291–299. | |
Roh YS, Cho H, Oh JO, Yoon CJ. Effects of skin rehabilitation massage therapy on pruritus, skin status and depression in burn survivors. J Korean Acad Nurs. 2007;37(2):221–226. | |
Gurol AP, Polat S, Akcay MN. Itching, pain, and anxiety level are reduced with massage therapy in burned adolescents. J Burn Care Res. 2010;31:429–432. | |
Van Os-medendorp H, Eland-de Kok PC, Ros, WJ, Bruijnzeel- Koomen CA, Grypdonck M. The nursing programme ‘Coping with Itch’: a promising intervention for patients with chronic pruritic skin diseases. J Clin Nurs. 2007;16:1238–1246. | |
Raap U, Stander S, Metz M. Pathophysiology of itch and new treatments. Curr Opin Allergy Clin Immunol. 2011;11:420–427. | |
Sarvis C. Providing relief to patients with malignant burns. Nurs Spectr. 2005;14(23):19–21. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
