Back to Journals » Research and Reports in Urology » Volume 15
Women as Urologists in Saudi Arabia: Career Choice and Practice Challenges: A Comparative Cross-Sectional Study
Authors Alzahrani MA , Almhmd A, Khan MA , Badriq F, Salman B , Aljaziri ZY , Alotaibi N, Alkhamees M , Almutairi S, Ahmad MS , Alkhateeb S
Received 15 March 2023
Accepted for publication 14 June 2023
Published 27 June 2023 Volume 2023:15 Pages 273—289
DOI https://doi.org/10.2147/RRU.S412713
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Guglielmo Mantica
Meshari A Alzahrani,1 Abdalah Almhmd,2 Muhammad A Khan,3,4 Feras Badriq,5 Budoor Salman,6 Zainab Y Aljaziri,7 Naif Alotaibi,8 Mohammad Alkhamees,1 Sulaiman Almutairi,1 Mohammad Shakil Ahmad,9 Sultan Alkhateeb10,11
1Department of Urology, College of Medicine, Majmaah University, Al-Majmaah, Saudi Arabia; 2College of Medicine, Majmaah University, Al-Majmaah, Saudi Arabia; 3College of Medicine, King Saud bin Abdulaziz University for Health Sciences (KSAU-HS), Jeddah, Saudi Arabia; 4King Abdullah International Medical Research Centre (KAIMRC), Jeddah, Saudi Arabia; 5Division of Urology, Department of Surgery, East Jeddah General Hospital, Ministry of Health, Jeddah, Saudi Arabia; 6Department of Urology, King Abdulaziz Medical City, Ministry of National Guard - Health Affairs, Jeddah, Saudi Arabia; 7Department of Family Medicine, Al Ahsa Health Cluster, Ministry of Health, Al Ahsa, Saudi Arabia; 8King Salman Bin Abdulaziz Hospital, Ministry of Health, Riyadh, Saudi Arabia; 9Department of Family & Community Medicine, College of Medicine, Majmaah University, Al Majmaah, Saudi Arabia; 10Department of Urology, King Faisal Specialist Hospital & Research Center, Riyadh, Saudi Arabia; 11College of Medicine, Alfaisal University, Riyadh, Saudi Arabia
Correspondence: Meshari A Alzahrani, Department of Urology, College of Medicine, Majmaah University, Al-Majmaah, 11952, Saudi Arabia, Tel +966569990693, Fax +966164042500, Email [email protected]
Background: There is limited research on whether women choose urology as a future career. Therefore, we aimed in this study to assess the influencing and challenging factors among female physicians in Saudi Arabia.
Methods: We approached 552 female physicians, including 29 (5.2%) urologists and 523 (94.7%) non-urologists. A cross-sectional survey was carried out, which included five sections and 46 items to assess and compare the perspectives of (urologists and non-urologists regarding influencing factors to choose urology, challenges toward applying to urology, and challenges during and after urology residency. Statistical analysis was conducted using SPSS software. Responses were presented as frequencies and percentages, while associations were studied using the Chi-squared test/Fisher’s exact test. A p-value of ≤ 0.05 was considered significant.
Results: Out of 552 female physicians, 466 completed the survey. The survey items compared urologists and non-urologists among female physicians. Among both cohorts, the most influencing factors in choosing urology were the diversity of practice and urological procedures (p =0.002, p< 0.001). There were no social barriers or challenges when applying for urology residency (p< 0.001). Overall, the majority of female urologists reported a high level of agreement that they have more time to work at the clinic (55.2%), they are satisfied as they are currently being urologists (75.8%), satisfied with their current lifestyle (72.6%). They would choose urology again as a future career (58.6%). Non-urologist female physicians 326 (74.6%) think they are more likely to have experienced gender discrimination than urologists 15 (51.7%) (p< 0.001). Female urologists were less likely to face social barriers when applying for urology residency than non-urologists (p< 0.001).
Conclusion: As urologists, we must understand women’s struggles, such as gender discrimination, a lack of academic advancement, and a lack of mentorship. To foster women’s careers in urology, we must understand their unique needs, provide adequate mentorship, exterminate gender discrimination bias, and improve mentorship.
Keywords: women, female, urology, training, residency, challenges, Saudi Arabia
Introduction
Women represent a minority in urology. In 1985, there were less than 50 female urologists globally.1 However, there has been a considerable increase in women going into surgical specialties.2,3 There has been a constant rise in the ratio of female residents across all disciplines. Interestingly, the most remarkable change was seen in urology.2 From 1978 to 2013, the proportion of female residents increased; specifically in urology, it rose from 0.9% to 24%.4 In Canada, urology has seen an increase in female applicants.5 For the first time in history, women made up more than 10% of the urologists’ workforce in 2020.6 The highest reported rate to date, this percentage grew further to 10.9% in 2021.7 However, there are still significant gaps in role models for women in urology.8
There are many reasons why women choose to pursue a career in urology. In a study published by Jackson et al, they found that the most critical factors were lifestyle, practice diversity, and procedure diversity.2 Interest in surgery, prior clinical exposure to the field, mentorship in urology, and research opportunities also played a key role.2,5,9 Nonetheless, this decision does not come without challenges; today, women still face obstacles in this field. A survey among female urology residents in the USA revealed that 60% of residents had male patients who refused to be seen by a female urologist.5 In addition, some residents reported mistreatment and discrimination by male patients and colleagues. Moreover, the fact that urology has a male predominance dissuaded some women from this career path.1,5,9,10
In Saudi Arabia, no current study evaluates female urologists choosing urology as a future career and assesses the challenges faced by urology applicants and those currently in practice, whether during residency or after residency. Therefore, this study aims to evaluate and identify the different aspects of female urologists’ training and challenges in Saudi Arabia and their subspeciality choices after residency. Our study is the first to compare urologist vs non-urologist physicians regarding choosing a career in urology.
Materials and Methods
This comparative cross-sectional survey study was conducted after obtaining the institutional review board (IRB) approval from the Saudi Ministry of Health (MOH) - General Department of Research and Studies (GDRS) - Central IRB under Project Number (20 −165E). After questionnaire construction, our co-author senior academic members (M.A.A, M.A., and S.A.) reviewed and approved the survey content. The survey’s list of questions and items was created into five main sections, with 46 items constructed from previous publications.2,5,9 The survey (Google form-based) was conducted among female physicians attending private and public hospitals in Saudi Arabia from October 2022 to December 2022. We approached 552 female physicians, including 29 (5.2%) urologists and 523 (94.7%) non-urologists. The main aim was to target female physicians in the form of two groups: urologists and non-urologists. The main objectives were to identify the following questions:
- What are the main influencing factors in choosing urology?
- What are the main challenges during to urology residency application?
- What are the main challenges during residency and post-training periods?
- What are the current employment and academic status of a female urologist?
- What is the attitude of female urologists toward urology as a career?
A survey containing demographic data (Section-1) including age, marital status, raising children or not, the timing of having first child, current region of work, current professional level, current work setting (private/military/MOH/university hospital), and years of practice as a health care provider were collected from the participants. Furthermore, female physicians were asked about the factors that might influence them to consider or choose urology as a future specialty. Participants from both groups were asked about their point of view in (Materials and Methods–4) about specific significant questions in the field of career choices and practicing medicine, including: “What are the influencing factors if you think about/or choose urology as a future career specialty” (Section-2), “what specific challenges do you think female physician might face when they apply to urology residency (Section-3)”, what specific challenges do you think the female physician might face during urology residency or post-residency practice period (Section-4). Female physicians specializing in Urology were asked exclusively in (Section-5) to assess their employment and academic status, including current and future subspecialty in urology, current working hours, and reading habits. Finally, in (Section-6) the female urologists were asked about their attitude toward urology as a career. A complete version of the survey is presented in (Appendix A). The questions were designed mainly into the Likert scale (strongly agree, agree, neutral, disagree, strongly disagree), binary (yes/no), and multiple-choice questions. All participants were informed about the purpose of the study, and consent was taken from all targeted populations regarding their participation in the survey. Participants were requested to choose the most appropriate answer for each question. All survey data were recorded electronically and anonymously using the Microsoft Excel spreadsheet.
Statistical analysis was performed by using SPSS software version 20.0. Cronbach’s alpha to measure item reliability showed acceptable reliability (0.716). Descriptive statistics were presented as the median, interquartile range (IQR), and percent. For comparative statistics, Chi-squared and Fisher’s exact test were used as appropriate. A p-value of <0.05 was used to indicate statistical significance for a two-tailed comparison.
Results
Responders’ Demographics
The questionnaire was distributed to 552 physicians, and 466 returned the filled questionnaire with a response rate of 84.4%. Among the whole cohort, 437 (93.7%) were non-urologist physicians. There was more unmarried female urologist 17 (58.6%) than female non-urologist physicians 211 (48.3%). For female urologists, 11 were married (37.9%), while 9 (31%) had children, and 4 (13.8%) and 5 (17.2%) of them gave birth before and after residency training, respectively. Regarding the current professional level, 59 (13.5%) non-urologist and 6 (20.7%) urologists were working as a consultant, while 104 (23.8%) non-urologists were working as general practitioners and none from the urologist group. Most respondents worked in the Ministry of Health (MOH) hospitals (non-urologists 52.4%, urologists 44.8%). The majority of non-urologist, as well as urologists, had less than 5 years of practicing experience (66.1%, 65.5%), respectively (Table 1).
 |
Table 1 Respondent Demographics |
Influencing Factors in Choosing Urology
When it was asked from the respondent about the diversity of practice, 25 (86.2%) urologists while 220 (50.4%) non-urologists agreed, which is significantly different (p 0.002). Twenty-six (89.7%) urologists and 199 (45.5%) non-urologists agreed to the diversity of urological procedures with a p-value <0.001. For both interest in urology as a surgical specialty and urology having a better life-work balance compared to other specialties, female urologists agreed more than non-urologist physicians with a significant p-value (<0.001). Other factors were found to be not significant (Table 2).
 |
Table 2 Influencing Factors to Choose Urology as a Future Career Among Responders |
Challenges for Female Physicians When Applying for Urology Residency
More female urologists disagreed with 20 (69%) in part for 154 (35.3%) non-urologists when asked if it was difficult to get a recommendation letter from a urologist with a significant p-value (<0.001). More than two-thirds of non-urologist physicians, 288 (65.9%), agreed that there was an alternative specialty other than urology in contrast to urologist physicians 9(31%) p-value <0.001. Regarding the social barriers, 11 (37.9%) urologists disagreed as compared to their non-urologist counterparts, 50 (11.4%), which was significantly different with a p-value <0.001. About 3/4th of the non-urologist physician 326 (74.6%) confirmed that they are not comfortable performing male genitourinary exams as fewer urologists agreed 7(24.1%) as well as refused examination and treatment by male patients for non-urologists 290 (66.4%) versus 10 (34.4%) urologists with highly significant p-value<0.001 for both. Another finding can be found in (Table 3).
 |
Table 3 Challenges That Might Face Female Applicants to Saudi Urology Programs |
Challenges for Female Physicians During Urology Residency
When inquired about the challenges faced by the female during urology residency, in all the surveys (male patients refusing to be seen by a female urologist, inappropriate treatment by male patients, inappropriate treatment by male superiors, colleagues, or staff, and gender discrimination or harassment) non-urologist physicians agreed more as compared to urologist physicians which had significant difference with p-value<0.001. More gender discrimination or harassment might be perceived was found to be a significant difference for patients among non-urologists 326 (74.6%) while in urologists 15 (51.7%) p <0.001. The other challenges were not significant among the groups of respondents (Table 4).
 |
Table 4 Challenges That Might Face Female Physicians During and After the Urology Residency Period |
Female Urologist Employment and Academic Status
More than three-quarters of female urologists choose female urology and pelvic reconstructive (79.3%), followed by pediatric urology (65.5%) as the most common subspecialty choice and the least likely subspecialty was andrology and male infertility (24.1%) (Figure 1). The average time of working hours per week for the female urologist was 24.1% for 50–60 hours and 60–70 hours each (Figure 2). About two-thirds of the participants (62.1%) spend 2–5 hours studying urology every week (Figure 3).
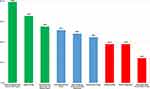 |
Figure 1 Urology subspecialty choices among female urologists (n=29). |
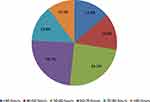 |
Figure 2 Working hours per week among female urologists (n=29). |
 |
Figure 3 Reading habits per week among female urologists (n=29). |
Female Urologist Perception and Attitude Toward Urology
Finally, the female urologist reported their attitude toward practicing urology. Overall, the majority reported a high level of agreement that they have more time to work at the clinic (55.2%), they are satisfied as they are currently being urologists (75.8%), satisfied with their current lifestyle (72.6%), satisfied with financial income (55.1%), satisfied with patient outcome (76%). Furthermore, they would choose urology again as a future career (58.6%) (Figure 4).
 |
Figure 4 Perception and attitude toward choosing urology among female urologists (n=29). |
Discussion
This nationwide survey explores influencing factors to choosing urology, challenges toward applying to urology, and challenges during and after urology residency between female urologist and non-urologist physicians.
Urology is a surgical specialty that treats female and male urinary tract diseases; female medical students face barriers such as lack of exposure, perceptions of the male-dominant patient and colleague demographics, and lack of mentorship.11 Furthermore, insufficient female participation in academic environments and scientific conferences.12 To bring about change, the urological community must collaborate to enhance women’s contribution to Urology.
We reported a low percentage of female urologists currently in urology practice in Saudi Arabia (Table 1). Ensuring that medical students receive adequate mentorship, have clinical experience in urology, and develop accurate perceptions of the specialty may significantly aid in attracting applicants.9 With the proportion of women enrolling in urology training programs increasing, more women are expected to enroll in urology training programs. In 2010, Saudi Arabia had 600 urologists (ratio 1:40,000 urologist/population), 66% of whom are specialists, and 49% of consultants are Saudi.13 The Saudi Commission for Health Specialties (SCFHS) has improved Saudi urology residency curriculum and training capacity, with 166 training centers in 2012 and 243 in 2016,14–18 with a 46.4% increase proportion in acceptance within five years interval. With an increasing proportion of urology matching systems, more women are anticipated to enroll in urology training programs and the urology community.
In the demographic section of this questionnaire (Table 1), married urologist residents are 11 (37.9%), which is lower in proportion compared to married non-urologist female residents 214 (49%), and while compared to other studies conducted in Canada3 among 60 female urologists, the married urologist is 38 (64.4%). The median age of female urologists in our study was 29. The average age of marriage for females is 20.4 years in Saudi Arabia, as reported in 2018.19 In Saudi Arabia, a study reported female doctors did not believe that being doctors made women more eligible for marriage.20 There is much evidence for women postponing or even giving up marriage and children for their medical careers worldwide, including the industrial countries.21 Women in urology also tend to have children 7–8 years later than the national average and have fewer children overall.22 Women in urology experienced more pregnancy difficulties than African-American women in rural Alabama, who share the highest prevalence of pregnancy complications in the USA.22 Such challenges were not only observed among women in urology but also were similar to female orthopedic surgeons when compared to the general population; there is an increased risk of pregnancy problems and preterm birth. Additionally, it has been reported that pregnant surgeons who work 60 hours per week have a higher risk of preterm labor.23
This sociocultural background may explain why most female urologists are not married.
In our data, female urologists disagreed with non-urologists when asked if it was difficult to get a recommendation letter from a urologist (p <0.001). Non-urologist physicians are likelier to have an alternative specialty than urologist physicians (<0.001). At the same time, when they asked about research opportunities in urology, they were insignificant between the two groups (Table 2 and Table 3). Insufficient female participation in academic environments and scientific conferences has been reported.12 The percentage of female academic urologists reaching full professor is 19% compared with 31% for all-female academic positions.24 Data from the USA among academic urologists showed proportionally fewer women attained senior academic ranking (professor/chair) (P < 0.05).25
A 2004 study of Saudi women in academic medicine found that promotion to higher ranks lagged behind males, and this may be attributed to family responsibilities, lack of institutional support, and bias.26 Binsaleh et al reported that urology residents in Saudi Arabia do not perceive their learning environment positively.27 In this study, compared between different training centers, The urology residents trained in the military hospital had higher satisfaction with their teachers, environment, education, and teamwork.27 Since the urology curriculum is used uniformly throughout Saudi Arabia, this primarily reflects local differences among various healthcare sectors. Greater efforts are required to achieve gender equality in academia. The participation of women on scientific program committees is a crucial step in the right direction to address the issue.
According to a Saudi study of medical undergraduates reported by Binsaleh et al, (13.3%) of participants were interested in pursuing a career in urology. The main reasons for not choosing urology as a career were social barriers (39.8%), an unappealing lifestyle (24.4%), and a limited specialty (13.1%).28 From our data, female urologists disagreed as compared to their non-urologist counterparts regarding social barriers, which were not challenging factors when applying for urology residency (p<0.001) (Table 3). A study from the United Kingdom; found that 28% of urologists said their undergraduate exposure to urology affected their specialty choice. Their top four reasons for choosing urology as a career were 1) inspiring role models, 2) exposure to urology as a house officer, 3) diversity of open and endoscopic urological procedures, and 4) the calm on-calls and sociable lifestyle.29 Similarly, a study reported that female applicants are more likely to match programs with more female residents and faculty.30 Data from one medical college in Saudi Arabia reported that most medical students could efficiently take a sexual history and perform genitourinary and digital rectal examination (DRE);28 the same author reported that knowledge of medical school graduates is insufficient in many urologic subjects and mainly due to lack of urology exposure, social reasons and lack of knowledge.28 Medical schools with mandatory urology rotations consistently produce more urology applicants,31 and clinical exposure is a critical factor in choosing a career in urology.9,30,32
Generally, the perception toward those challenges changed positively among female urologists as they reported less agreement than the non-urologist group (p <0.001) (Table 4). In previous literature, women experienced a variety of barriers in urology. According to a 2006 survey, the most common challenges faced by female urology residents were refusal to see male patients (60%), inappropriate treatment by male colleagues (36%) or male patients (29%), and sexual harassment (22%).2 A 2000 survey of 3000 full-time faculty members in the USA found that about half of the female faculty had experienced sexual harassment.33,34 More recently, in a 2016 study in the USA of 1066 physician-scientists, 30% of women reported sexual harassment and 66% gender bias in professional advancement.35
From our data, a minority of female urologists, 20%, think that gender discrimination or harassment would be a challenging issue compared to most non-urologist females; 58% think it would be a challenge (Table 4). Data from Saudi Arabia reported that more than three-quarters of Saudi residents experienced harassment and discrimination, significantly more among female than male residents (P=0.0061).36 Studies to determine whether females are socially integrated into the profession of medicine suggest that women typically receive more emotional support than men but less informational and instrumental support from their departments, supervisors, and co-workers.37
In addition to workplace discrimination and harassment, there is a lack of mentoring for females in urology. In 1985, none of the 22 women in urology practice said they knew a female surgeon, according to a survey.38 The numbers in a modern study on women in urology were similar, with 65% reporting male mentors and 29% reporting no mentor in urology.39 While female urologists in Canada, 40% found it challenging to find a mentor during their training. It is undeniable that mentorship in the medical field has great professional value for both mentor and mentee. The lack of mentorship for female urology is remarkable.11,24,39 Data from USA urology programs showed the most common reason for not having a formal mentorship program was because the program felt that informal mentorship sufficed.40 A study among women in Emergency Medicine reported that Mentoring programs had shown benefits for both the mentee and mentor, with improvements in career satisfaction, stress management, academic productivity, and work-family balance for mentees and, for mentors, increased research productivity, personal satisfaction, and opportunities for career advancement.41 From our study, the lack of mentorship among both groups was not statistically significant as a challenging factor in choosing urology as a specialty (Table 4). A study from Saudi Arabia showed a positive perspective and high principles of mentorship held by anesthesiology residents.42 The SCFHS reported the number of medical students under graduation with an MBBS degree in 2018 was 26,216, 11,600 (44.2%) were women in Saudi Arabia, distributed in 37 medical schools in Saudi Arabia (28 governmental and nine private sectors).43 That may reflect a generally growing women’s mentorship program in Saudi Arabia.
In our study, among both groups (female urologists vs non-urologist), work-related pregnancy complications and maternity leave were statistically insignificant challenges during urology residency (Table 4). However, women urologists have children later in life, a smaller number, a higher induction rate, and a higher incidence of pregnancy complications.22 This is similar to female orthopedic surgeons, who have an increased risk of pregnancy complications and preterm delivery than the general population.23 In addition, an increased risk of preterm labor has been reported in surgeons working > 60 hours/ week during pregnancy.23
Among female urologists, our data likewise data from the USA,2,25 the two most common fellowship choices were female urogynecology/reconstruction and pediatrics (Figure 1). Oberlin et al found that female urologists operated on more female patients than their male counterparts (54% vs 32%), even when performing gender-neutral surgeries or having gender-neutral fellowship training such as endourology.44 Some literature also shows that female patients have a gender preference for female physicians.45 Urology practice has expanded to address a variety of diseases classified as female-specific disorders. As a result, such an expanding array of patients allowing treating people of both sexes and all ages appears essential to female medical students and residents when choosing urology in general and fellowship opportunities in particular.2 On the other hand, when we asked the female physicians about research opportunities in urology, it was statistically insignificant among both groups (female urologists vs non-urologist) (Table 3). Mentoring programs have shown benefits in improving research productivity.41 Improving psychosocial barriers to advancement, such as lack of mentorship, discriminatory policies, increased engagement and representation in clinical research, academic conferences, and scientific meetings, may help pioneering female urologists as they progress in their careers.
The working hours among female physicians from previous data are variable. In our study, 24.1% of female urologists reported average working hours of 50–60 and 60–70 (Figure 2). For female urologists, data from the USA showed they work the same hours as male colleagues; 61% reported working 51 or more hours a week.24 A survey in the USA of 1049 academic physicians found that women spent 8.5 more hours per week on domestic activities and were more likely to take time off for childcare than men.46 Another study reported that marriage and raising children among women but not men resulted in fewer work hours.47 In Canada, physicians are paid according to a standard fee schedule and have substantial discretion in setting their work hours; male and female physicians have statistically indistinguishable hours of market work when never married and without children.48 Recent data from Saudi Arabia among 215 urology residents showed mean personal burnout was 57.92, while the mean work-related burnout was 55.26 using Copenhagen Burnout Inventory (CBI) questionnaire; females have higher work-related burnout with a mean of 57.5.49
In our study, the reading habits among female urologists are still low; about two-thirds of the female urologist, 18 (62.1%), spend 2–5 hours studying urology every week (Figure 3). Our result is similar to recent data from Saudi Arabia; among 142 urology residents, females represented few in this study 5 (3.5%), showed 37.3% read for 2–5 hours weekly, with the majority studying up to 10 hours, and the minority for 10–40 hours in aggregated percentages, and remarkably juniors read more than seniors (P = 0.034).50 Most Saudi urology residents (82.3%) reported studying up to 10 hours per week,50 which exceeds the 4 hours for surgical residents51 but is less than the 10 hours for Canadian urologists.52 Our data (Figure 4) were like the USA found 87% were happy with the choice of urology, 81% would repeat the decision, and 91% would again choose a surgical subspecialty.53 According to a previous study, most respondents (91.1%) had a urology rotation, 52.7% defined urology as a surgical specialty and 46.3% considered it a medico-surgical specialty.31
Limitation
Selection bias was one of the limitations of this study. The inability to show temporal relationships, one of our study design limitations, restricts the ability to infer causation. Since there are no statistics on female urologists in training, assessing the precise level of female representation is difficult. Due to a shortage of female urologists, Fisher’s exact tests had to be used, given the small number of female urologists nationwide. Nevertheless, this is the first study comparing different aspects of the urology specialty among female and non-urologist physicians. Our study strength showed a higher response rate of 84.4% to the study survey with a large sample size and the use of a control group of non-urology female physicians to assess different aspects of choosing urology as a future career.
Conclusions
We reported a low percentage of females practicing urology in Saudi Arabia. In our study, the most influencing factor in choosing urology was the diversity of practice, urological procedures, and a well-balanced work-to-life commitment. Female urologists, as opposed to non-urologists, reported having no obvious challenges that might affect their application to urology. Further research is needed to explore differences between men and women in urology throughout their careers. If we want to increase the number of women in urology, it seems important to increase the number of women applying to urology and improve women’s wellness, leadership, and mentorship programs.
Ethics
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Saudi Ministry of Health (MOH) - General Department of Research and Studies (GDRS) - Central Institutional Review Board under Project Number (20 −165E), approval date (19/8/2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Acknowledgments
The authors would like to thank the Deanship of Scientific Research at Majmaah University for supporting this work under Project Number R-2023-486.
Disclosure
The authors declare no conflicts of interest.
References
1. Grimsby GM, Wolter CE. The journey of women in urology: the perspective of a female urology resident. Urology. 2013;81(1):3–6. doi:10.1016/j.urology.2012.07.050
2. Jackson I, Bobbin M, Jordan M, Baker S. A survey of women urology residents regarding career choice and practice challenges. J Womens Health. 2009;18(11):1867–1872. doi:10.1089/jwh.2008.1236
3. Hird AE, St-Laurent MP, Nadeau G, Carr L, Farcas M. Exploring the patterns of practice and satisfaction among female urologists in Canada. Can Urol Assoc J. 2020;14(8):245–251. doi:10.5489/cuaj.6184
4. Aisen CM, Sui W, Pak JS, Pagano M, Cooper KL, Badalato GM. Gender differences in the urology residency match-does it make a difference? Urology. 2018;111:39–43. doi:10.1016/j.urology.2017.07.061
5. Anderson K, Tennankore K, Cox A. Trends in the training of female urology residents in Canada. Can Urol Assoc J. 2018;12(3):E105–E111. doi:10.5489/cuaj.4697
6. American Urological Association. Female urologists make history in urology; 2021. Available from: https://auanet.mediaroom.com/2021-05-27-Female-Urologists-Make-History-in-Urology#assets_all.
7. American Urological Association. The American urological association releases 2021 AUA census results. Available from: https://auanet.mediaroom.com/2022-04-12-The-American-Urological-Association-Releases-2021-AUA-Census-Results.
8. Hüsch T, Haferkamp A, Thomas C, Steffens J, Fornara P, Kranz J. Gender gap at a large European urological congress: still at the beginning. World J Urol. 2022;40(1):257–262. doi:10.1007/s00345-021-03777-4
9. Kerfoot BP, Nabha KS, Masser BA, McCullough DL. What makes a medical student avoid or enter a career in urology? Results of an international survey. J Urol. 2005;174(5):1953–1957. doi:10.1097/01.ju.0000177462.61257.4e
10. Hu YY, Ellis RJ, Hewitt DB, et al. Discrimination, Abuse, Harassment, and burnout in surgical residency training. N Engl J Med. 2019;381(18):1741–1752. doi:10.1056/NEJMsa1903759
11. Kim S, Farrokhyar F, Braga LH. Survey on the perception of urology as a specialty by medical students. Can Urol Assoc J. 2016;10(9–10):349–354. doi:10.5489/cuaj.3621
12. Hüsch T, Osman NI, Herve F, et al. Gender representation at scientific congresses: focus on functional and female urology-a study from the EAU young academic urologist functional urology group. World J Urol. 2023;41(5):1445–1450. doi:10.1007/s00345-023-04355-6
13. Al Otaibi KE. Urology Training. Urol Ann. 2016;8(Suppl 2):S184–S188.
14. SCFHS. Postgraduate training programs statistics; 2016. Available from: https://www.scfhs.org.sa/MESPS/Statistics/Pages/default.aspx.
15. Postgraduate training programs statistics 2018; 2019. Available from: https://www.scfhs.org.sa/MESPS/Pages/statistics.aspx.
16. Medical specialty selection guide for medical graduates. Available from: https://www.scfhs.org.sa/en/Media/OtherPublications/Documents/Medical%20Specialty%20Selection%20Guide.pdf.
17. SCFHS-MS 2018. Saudi commission for health specialties matching system; 2019. Available from: https://scfhs.org.sa/MESPS/AcceptanceRegister/Documents/score.pdf.
18. Saudi board urology curriculum; 2014. Available from: https://www.scfhs.org.sa/MESPS/TrainingProgs/TrainingProgsStatement/Documents/Urology%20new.pdf.
19. General Authority for statistics. Available from: https://www.stats.gov.sa/en/node.
20. Baqi S, Albalbeesi A, Iftikhar S, Baig-Ansari N, Alanazi M, Alanazi A. Perceptions of gender equality, work environment, support and social issues for women doctors at a university hospital in Riyadh, Kingdom of Saudi Arabia. PLoS One. 2017;12(10):e0186896. doi:10.1371/journal.pone.0186896
21. Simpson AN, Cusimano MC, Baxter NN. The inconvenience of motherhood during a medical career. CMAJ. 2021;193(37):E1465–E1466. doi:10.1503/cmaj.211255
22. Lerner LB, Stolzmann KL, Gulla VD. Birth trends and pregnancy complications among women urologists. J Am Coll Surg. 2009;208(2):293–297. doi:10.1016/j.jamcollsurg.2008.10.012
23. Hamilton AR, Tyson MD, Braga JA, Lerner LB. Childbearing and pregnancy characteristics of female orthopaedic surgeons. J Bone Joint Surg Am. 2012;94(11):e77. doi:10.2106/JBJS.K.00707
24. Lightner DJ, Terris MK, Tsao AK, Naughton CK, Lohse CM. Status of women in urology: based on a report to the Society of University Urologists. J Urol. 2005;173(2):560–563. doi:10.1097/01.ju.0000149739.51103.d3
25. Mayer EN, Lenherr SM, Hanson HA, Jessop TC, Lowrance WT. Gender differences in publication productivity among academic urologists in the United States. Urology. 2017;103:39–46. doi:10.1016/j.urology.2016.12.064
26. Al-Tamimi DM. Saudi women in academic medicine. Are they succeeding? Saudi Med J. 2004;25(11):1564–1567.
27. Binsaleh S, Babaeer A, Alkhayal A, Madbouly K. Evaluation of the learning environment of urology residency training using the postgraduate hospital educational environment measure inventory. Adv Med Educ Pract. 2015;6:271–277. doi:10.2147/AMEP.S81133
28. Binsaleh S, Al-Jasser A, Almannie R, Madbouly K. Attitude and perception of urology by medical students at the end of their medical school: an appraisal from Saudi Arabia. Urol Ann. 2015;7(2):211–220. doi:10.4103/0974-7796.150511
29. Shah J, Manson J, Boyd J. Recruitment in urology: a national survey in the UK. Ann R Coll Surg Engl. 2004;86(3):186–189. doi:10.1308/003588404323043328
30. Wong D, Ganesan V, Kuprasertkul I, Khouri RK Jr, Lemack GE. Reversing the decline in urology residency applications: an analysis of medical school factors critical to maintaining student interest. Urology. 2020;136:51–57. doi:10.1016/j.urology.2019.10.028
31. Kutikov A, Bonslaver J, Casey JT, et al. The gatekeeper disparity--why do some medical schools send more medical students into urology? J Urol. 2011;185(2):647–652. doi:10.1016/j.juro.2010.09.113
32. Lebastchi AH, Khouri RK Jr, McLaren ID, et al. The urology applicant: an analysis of contemporary urology residency candidates. Urology. 2018;115:51–58. doi:10.1016/j.urology.2017.10.065
33. Bradbury CL, King DK, Middleton RG. Female urologists: a growing population. J Urol. 1997;157(5):1854–1856. doi:10.1016/s0022-5347(01)64884-5
34. Carr PL, Ash AS, Friedman RH, et al. Faculty perceptions of gender discrimination and sexual harassment in academic medicine. Ann Intern Med. 2000;132(11):889–896. doi:10.7326/0003-4819-132-11-200006060-00007
35. Jagsi R, Griffith KA, Jones R, Perumalswami CR, Ubel P, Stewart A. Sexual harassment and discrimination experiences of academic medical faculty. JAMA. 2016;315(19):2120–2121. doi:10.1001/jama.2016.2188
36. Fnais N, al-Nasser M, Zamakhshary M, et al. Prevalence of harassment and discrimination among residents in three training hospitals in Saudi Arabia. Ann Saudi Med. 2013;33(2):134–139. doi:10.5144/0256-4947.2013.134
37. Wallace JE. Gender and supportive co‐worker relations in the medical profession. Gend Work Organ. 2014;21(1):1–17. doi:10.1111/gwao.12007
38. Yang JH, Donat SM. Elisabeth Pauline Pickett (1918-): opening the door for women in urological oncology. J Urol. 2007;178(5):1875–1877. doi:10.1016/j.juro.2007.07.004
39. Harnisch BA, Stolzmann KL, Lerner LB. Mentoring, fellowship training and academic careers of women urologists. BJU Int. 2010;105(12):1629–1631. doi:10.1111/j.1464-410X.2010.09391.x
40. Bortnick E, Stock J, Simma-Chiang V. Mentorship in urology residency programs in the United States. Urology. 2020;136:58–62. doi:10.1016/j.urology.2019.09.053
41. Welch JL, Jimenez HL, Walthall J, Allen SE. The women in emergency medicine mentoring program: an innovative approach to mentoring. J Grad Med Educ. 2012;4(3):362–366. doi:10.4300/JGME-D-11-00267.1
42. Bin Ghali KN, AlSubaie AT, Nawab AA. Mentorship in anesthesia: a perspective survey among anesthesia residents in Riyadh, Saudi Arabia. Saudi J Anaesth. 2021;15(2):144–148. doi:10.4103/sja.sja_1145_20
43. Conference on the reality of the Saudi health workforce during the next ten years. Available from: https://www.dropbox.com/s/35ksprb8jrauz6n/%D9%88%D8%A7%D9%82%D8%B9%20%D8%A7%D9%84%D9%82%D9%88%D9%89%20%D8%A7%D9%84%D8%B9%D8%A7%D9%85%D9%84%D8%A9%20%D8%A7%D9%84%D8%B5%D8%AD%D9%8A%D8%A9%20%D8%A7%D9%84%D8%B3%D8%B9%D9%88%D8%AF%D9%8A%D8%A9%20%D8%AE%D9%84%D8%A7%D9%84%20%D9%A1%D9%A0%D8%B3%D9%86%D9%88%D8%A7%D8%AA%20%D8%A7%D9%84%D9%82%D8%A7%D8%AF%D9%85%D8%A9.pdf?dl=0.
44. Oberlin DT, Vo AX, Bachrach L, Flury SC. The gender divide: the impact of surgeon gender on surgical practice patterns in urology. J Urol. 2016;196(5):1522–1526. doi:10.1016/j.juro.2016.05.030
45. Tempest HV, Vowler S, Simpson A. Patients’ preference for gender of urologist. Int J Clin Pract. 2005;59(5):526–528. doi:10.1111/j.1368-5031.2005.00465.x
46. Jolly S, Griffith KA, DeCastro R, Stewart A, Ubel P, Jagsi R. Gender differences in time spent on parenting and domestic responsibilities by high-achieving young physician-researchers. Ann Intern Med. 2014;160(5):344–353. doi:10.7326/M13-0974
47. Wang C, Sweetman A. Gender, family status and physician labour supply. Soc Sci Med. 2013;94:17–25. doi:10.1016/j.socscimed.2013.06.018
48. McMurray JE, Linzer M, Konrad TR, Douglas J, Shugerman R, Nelson K. The work lives of women physicians results from the physician work life study. The SGIM career satisfaction study group. J Gen Intern Med. 2000;15(6):372–380. doi:10.1111/j.1525-1497.2000.im9908009.x
49. Aljuhayman AM, Alkhamees MA, Alkanhal HF, Al-Zahrani MA, Almutair SA, Alkhamees AA. Assessment of burnout among urology residents in KSA: a cross-sectional study. J Taibah Univ Med Sci. 2020;16(1):29–33. doi:10.1016/j.jtumed.2020.10.014
50. Alkhamees M, Al-Zahrani MA, Almutairi S, Alkanhal H, Almuhaideb M, Abumelha SM. Study habits of urology residents in Saudi Arabia: identifying defects and areas for curricular development - a trainee-based survey. Adv Med Educ Pract. 2020;11:707–715. doi:10.2147/AMEP.S269059
51. Yeh DD, Hwabejire JO, Imam A, et al. A survey of study habits of general surgery residents. J Surg Educ. 2013;70(1):15–23. doi:10.1016/j.jsurg.2012.08.006
52. Skinner TAA, Ho L, Touma NJ. Study habits of Canadian urology residents: implications for development of a competence by design curriculum. Can Urol Assoc J. 2017;11(3–4):83–87. doi:10.5489/cuaj.4132
53. Marley CS, Lerner LB, Panagopoulos G, Kavaler E. Personal, professional and financial satisfaction among American women urologists. Int Braz J Urol. 2011;37(2):187–194. doi:10.1590/s1677-55382011000200005
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
