Back to Journals » Patient Preference and Adherence » Volume 16
Willingness to Receive COVID-19 Vaccination Among Adult Diabetes Patients in Woldia Comprehensive Specialized Hospital, North Ethiopia; A Cross-Sectional Study
Authors Mesele H , Shiferaw M , Tunta A , Seid A, Kassahun W
Received 24 June 2022
Accepted for publication 25 August 2022
Published 2 September 2022 Volume 2022:16 Pages 2451—2459
DOI https://doi.org/10.2147/PPA.S379531
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Johnny Chen
Habtamu Mesele,1 Mulu Shiferaw,2 Abayneh Tunta,2 Addisie Seid,1 Woldeteklehymanot Kassahun3
1Woldia Comprehensive Specialized Hospital, Woldia, Ethiopia; 2Biomedical Unit, School of Nursing, College of Health Sciences, Woldia University, Woldia, Ethiopia; 3Department of Medical Laboratory Sciences, College of Health Sciences, Woldia University, Woldia, Ethiopia
Correspondence: Mulu Shiferaw, Biomedical Unit, School of Nursing, College of Health Sciences, Woldia University, PO Box 400, Woldia, Ethiopia, Email [email protected]
Background: According to recently published data, individuals infected with COVID-19 having concomitant diabetes may experience disease worsening or even death. The purpose of this study was to determine diabetes patients’ willingness to get the COVID-19 vaccine as well as its magnitude and determinants.
Methods: Three hundred eighty six diabetes patients who visited Woldia Comprehensive Specialized Hospital during February and March 2022 participated in this institution-based cross-sectional study. Descriptive statistics were used to demonstrate frequencies and percentages, while logistic regression was used to identify the relevant determinants of vaccination readiness. Age, gender, income, place of residence, COVID-19 exposure, length of diabetes, awareness of and attitudes toward the COVID-19 immunization were all evaluated as associated factors.
Results: Out of 386 study participants, 268 (69.43%) were male and 146 (37.82) completed their secondary schooling. From 386 study participants 82.6% (95% CI; 78.5– 86.3%) were willing to get vaccinated. The uptake of the COVID-19 vaccination among diabetes patients was independently influenced by sex (Adjusted Odd Ratio [AOR] = 6.84 (2.98, 15.68)), exposure to the illness (AOR 8.98 (3.22, 25.04)), attitude (AOR = 2.63 (1.2, 5.77)), and length of the disease (AOR = 0.62 (0.51, 0.76)).
Conclusion: Most of the study participants were willing to get the COVID-19 immunization. The relevant agency should make the immunization available in order to enhance disease control and reduce infection-related complications with special consideration of diabetes patients.
Keywords: COVID-19, diabetes, willingness
Introduction
A huge global threat is posed by the continuing coronavirus disease 2019 (COVID-19) pandemic, which is caused by the SARS-CoV-2 coronavirus. COVID-19 can cause mild to severe symptoms, including asymptomatic infection, mild upper respiratory tract disease, and severe viral pneumonia, which can cause respiratory failure and even death.1
Although the majority of COVID-19 infected patients are expected to have a good prognosis, chronic disorders common in the elderly, such as hypertension, diabetes, and cerebral vascular disease, as well as their susceptibility conditions, can contribute to poor clinical results.2
The most prevalent comorbidities among COVID-19 patients were hypertension and diabetes, followed by cardiovascular diseases and respiratory system conditions.3 Symptomatic COVID-19 infection was connected to diabetes and hypertension, according to another cross-sectional study conducted in Ethiopia. Additionally, it is thought that having diabetes and COVID-19 infection at the same time will make the disease worse.4
Emerging information suggests that diabetes comorbidity in patients with COVID-19 is associated with disease deterioration and even death. According to the Centers for Disease Control and Prevention (CDC), diabetes patients had a fivefold increased risk of acquiring SARS-CoV-2 and a threefold increased risk of dying from COVID-19. This might be as a result of acute or chronic immune-compromising diabetes complications.5 According to Wang et al COVID-19 patients admitted to the intensive care unit (ICU) were more likely to have preexisting diabetes compared to who were not admitted.5 Similarly, Wu et al found that comorbid diabetes was more commonly seen in patients who developed acute respiratory distress syndrome (ARDS) than in those who did not develop.6 Guo et al also compared the clinical features of COVID-19 patients with and without diabetes and found that those with diabetes had a greater likelihood of becoming severely ill, as evidenced by a higher incidence of organ damage, hypercoagulability, and elevated levels of inflammatory markers.7 In keeping with the aforementioned findings, in Ethiopia, diabetes was linked to reduced probabilities of achieving clinical recovery compared to individuals without the condition.8 The prevalence of 1.3% diagnosed and 5% undiagnosed diabetes patients during this period of COVID-19 creates challenge for health-care systems of Ethiopia.9
One of the prevention methods, COVID-19 vaccination, produced the same strength of immune response and side effects in diabetes patients compared to the general population.10 COVID-19 immunization was introduced in Ethiopia on March 13, 2021, and numerous vaccines (eg, Johnson & Johnson, AstraZeneca, Pfizer, Sinopharm, Sinovac) were made accessible.11,12 Following the WHO’s prioritization road map, a nationwide deployment and vaccination strategy was designed, with priority immunization for frontline health professionals and support personnel, the elderly with underlying illnesses, and other high-risk categories.13
As Ethiopia marks one year of COVID-19 vaccination by the middle of March 2022, more than 21 million people—roughly 20% of the population—have gotten at least one dose of the vaccine.14 Global vaccine inequity combined with vaccine hesitancy has contributed to low COVID-19 vaccine coverage in Ethiopia. According to a study among the general population of Ethiopia, only 31.4% were willing to get COVID-19 vaccinated.15
We are aware of no published data on the factors influencing vaccine acceptance among people with diabetes in Ethiopia. In order to ensure optimal vaccine distribution and improve immunization rates, research is needed to determine the acceptability of vaccines among diabetes patients.
Method
Study Setting
This facility-based cross-sectional study was conducted from March 15 to April 20, 2022, in Woldia, a comprehensive specialized hospital located in North Ethiopia. The study was conducted at a diabetes clinic of WCSH, which is found in Woldia town. According to the 2014 national population project conducted by the central statistical agency of Ethiopia (CSA), there are about 180,000 inhabitants in the town. The hospital serves the residents of North Wollo district as well as nearby populations from the Tigray and Afar regions. WCSH has Emergency OPD service, Adult OPD, diabetes clinic, youth friend service, under five OPD, inpatient room, maternal and child health service, laboratory, card room and drug store. There are about 17 specialists, 45 general practitioners, 172 nurses, and 66 midwives. In the previous month of data collection, around 850 diabetes patients visited the diabetes clinic. Consecutive sampling techniques were used.
Sample Size Determination
Since there are no published data on the prevalence of willingness to receive the COVID-19 vaccine among diabetes patients in Ethiopia, the sample size was calculated using a single population proportion formula, taking a 50% proportion into account. The final sample size was 386, with a margin of error (d) of 0.05 and a 95% confidence interval.
Populations of the Study
The source population of the study was all diabetes patients who had follow-up at Woldia Comprehensive Specialized Hospital, whereas the study population was all diabetes patients who had visited Woldia Comprehensive Specialized Hospital during the data collection time.
Eligibility Criteria
Patients with diabetes who had already begun the immunization and registered on their medical record charts, and/or who were unable to respond due to a serious illness were not included in the study.
Study Variables
The outcome variable of the study was the willingness to receive the COVID-19 vaccine (yes/no options). The independent variables were respondents’ sociodemographic data (sex, marital status, age, religion, educational level, average monthly income, occupation, residence, presence of health insurance, duration of chronic illness, exposure to COVID-19 infected individuals), knowledge, and attitude towards COVID-19 vaccine.
Operational Definition
Willingness to receive COVID-19 vaccine: a “yes” response to the question “are you willing to take the COVID-19 vaccine?” Was considered willing to get vaccinated.16
Knowledge about COVID-19 vaccine; Respondents scored 70% and above on questions assessing knowledge about the COVID-19 vaccine were considered to have good knowledge while respondents who scored less than 70% were considered to have poor knowledge. There were seven questions which were targeted for the assessment of knowledge about COVID-19.
Attitude towards the COVID-19 vaccine: Respondents who scored greater than or equal to 70% scored attitude questions were considered to have a positive attitude while respondents who scored less than 70% were considered as having a negative attitude.16 Nine questions were used to assess the attitude towards COVID-19 vaccine.
Data Collection Procedures and Quality Control
The data were collected through a face-to-face interview using a pre-tested structured questionnaire adapted from various published literatures.16–18 The questionnaire was prepared in English and translated to the local language (Amharic) and re-translated back to the English version to ensure consistency. Training was given to the data collectors and supervisors on the aim of the study, clarity of the measuring tool, and ethical considerations. The data were collected by three BSc. nurses, and one supervisor supervised the data collection process. A daily meeting and supervision was also established to assess challenges that occur during data collection.
Data Processing and Analysis
The data were entered into Epi data and exported to SPSS version 25 software. A description summary (frequency distribution, proportion, mean and standard deviation) was used to summarize the variables. A binary logistic regression model was used to investigate factors associated with willingness to receive the vaccine. Variables that were significantly associated with the dependent variable in bivariate analysis and with P-value <0.25 were further analyzed in the multivariate analysis to identify their associated effects on taking the COVID-19 vaccine.
Result
Sociodemographic Characteristics
Out of a total of 386 study participants, 268 (69.43%) were male and 146 (37.82) completed their secondary schooling. The mean age of the study participants was 56.7±7.9 (the minimum age was 21 and the maximum age was 72 years) (Table 1).
 |
Table 1 Sociodemographic Related Characteristics of Study Participants in Woldia Comprehensive Specialized Hospital |
Health Related Characteristics of the Study Participants
Above half (55.44%) of the study participants had type 2 diabetes mellitus, out of them 169 (91.6%) were willing to receive the vaccine (Figure 1). Hypertension, cardiac diseases and Asthma were found among 141 (36.53%), 77 (19.95%) and 75 (19.43%) study participants, respectively. From study participants whose family member were infected with COVID-19 (223 (57.77%), 211 (96.4%)) were willing to receive COVID-19 vaccine (Table 2)
 |
Table 2 Health-Related Characteristics of the Study Participants in Woldia Comprehensive Specialized Hospital |
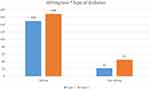 |
Figure 1 Willingness of study participant to receive COVID-19 vaccine stratified by type of diabetes in Woldia comprehensive specialized hospital. |
Proportion of Willingness to Receive COVID-19 Vaccine and Determining Factors
The proportion of willingness to receive COVID-19 was 82.6% with 95% CI (78.5, 86.3). The probability of diabetes patients to take COVID-19 vaccine was six times higher among male patients compared to female (Adjusted Odd Ratio [AOR]=6.84 (2.98, 15.68)). The study also indicated that the odds of intention to take the COVID-19 vaccine were 2.63 times (AOR = 2.63 (1.2, 5.77)) times higher among those participants who had positive attitude of COVID-19 vaccine compared counterparts. Diabetes patients who had history of exposure to COVID-19 had 8.9 times (AOR 8.98 (3.22, 25.04)) more willing to receive COVID-19 vaccine than their counterpart (Table 3).
 |
Table 3 Determinants of Willingness to Take COVID-19 Vaccine Among Diabetic Patients in Woldia Comprehensive Specialized Hospital |
Discussion
Vaccination is a crucial method for hampering the COVID-19 pandemic by achieving herd immunity in the population. The efficiency of this approach depends on vaccination uptake in the population. The up-to-date assessments on COVID-19 have shown 60–75% of the population needs to be vaccinated to attain herd immunity and stop the transmission of the disease.19
The magnitude of willingness to get COVID-19 vaccinated in our study was 82.6%. This was in-line with findings from Italy20 and Wolaita, Ethiopia.21 While it was higher than reports from Saudi Arabia,22 china,23,24 Sub-Saharan Africa25 and Uganda.26 On the other hand, the magnitude was lower than from findings among the general population in Ethiopia.27 The discrepancy in these data may be due to sociodemographic characteristics.
In this investigation, male diabetes patients were six times more likely than female diabetes patients to receive COVID-19 vaccine, which was consistent with studies conducted in Ghana and Italy20,28 but not in Saudi Arabia.22 This disparity could be explained by males’ better health-seeking behavior than females.29,30 The perceived concern that adult males with COVID-19 have a higher risk of death than their female counterparts across all age groups may increase health-seeking behavior for COVID-19 vaccination. This may result in a high demand for vaccination among males.31 As a result, increasing COVID-19 vaccination adoption requires focusing on raising vaccine awareness among female diabetes patients.
Similarly, city dwellers were 4.03 times more likely than rural dwellers to receive the COVID-19 vaccine. This could be due to improved availability to vaccine information, which leads to an increase in health-seeking behavior among the more vulnerable urban population. Respondents with high awareness of the COVID-19 vaccination were 2.92 times more willing to take the vaccine in this study than those with low knowledge. This was consistent with findings from reports on Ethiopia’s HIV/AIDS patients,32 Palestine,33 and the USA.34 This could be related to the fact that the majority of respondents in our current study were from metropolitan areas and were educated, allowing for easier access to vaccine information and, as a result, higher awareness of COVID-19. Because people who have information on the effectiveness of the COVID-19 vaccine are more likely to get vaccinated, having good knowledge about the vaccine enhances compliance towards getting vaccinated.35
Positive attitude was associated with willingness to receive COVID-19 vaccine with an AOR of 2.63, which was supported by findings from Ethiopia among people living with HIV/AIDS, chronic patients, health-care workers, and those at risk of infection36,37 and South Africa.38 People who have a positive attitude toward the COVID-19 vaccine have a strong belief in the perceived benefits, cues to action, and perceived severity, all of which are significant associated factors of intention to acquire COVID-19 immunization.39 As a result, public awareness campaigns should focus on providing more information about COVID-19 vaccine safety and reassuring the public in order to continue this favorable attitude toward vaccination intentions.
Furthermore, patients with a history of COVID-19 exposure were 9 times more likely (AOR= 8.98)3,22,25 to want to be vaccinated against COVID-19, despite the fact that research from Nigeria contradicted this.40 It is possible that persons with a history of exposure have a higher inclination to get vaccinated because of their sickness experience. Diabetes patients who were longer lived with the diseases were less willing to receive vaccine than their counter part. This could be explained as those patients with longer duration will adapt the diseases condition and perceive as they are competent enough to fight the infection.
However, we have strived to report the current evidences on the willingness of diabetes patients to take COVID-19 vaccination, this study may be limited to its single center study.
Conclusion
According to this study, the majority of diabetes patients were willing to get the COVID-19 vaccine. The responsible body should offer the vaccine for better disease control and to reduce infection complications, particularly in diabetes patients. On the other hand, poor knowledge and a negative attitude toward the vaccine were identified as determinates for patients who were unwilling to receive the vaccine, so health professionals, religious leaders, and other influential persons should counsel about the benefits of COVID-19 vaccination and increase their awareness of the vaccine is recommended.
Data Sharing Statement
The data set used and analyzed for the study is available from the corresponding author on reasonable request.
Ethical Approval and Consent to Participate
The research was carried out in accordance with the Declaration of Helsinki’s guidelines and regulations. Ethical approval was obtained from Woldia University ethical review board. Permission letter was obtained from medical director office of Woldia comprehensive specialized hospital with protocol number ERC001/2022. Informed consent was obtained from the study participants. Confidentiality of patients’ information was kept anonymous in any process of the study.
Acknowledgments
Our everlasting appreciation is to the participants and the health-care workers working in study area.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funds were obtained to conduct this study.
Disclosure
All authors declared that there are no financial or non-financial competing interests for this study.
References
1. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi:10.1001/jama.2020.2648
2. Li B, Yang J, Zhao F, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109(5):531–538. doi:10.1007/s00392-020-01626-9
3. Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–95. doi:10.1016/j.ijid.2020.03.017
4. Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020;8(4):e21–e. doi:10.1016/S2213-2600(20)30116-8
5. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi:10.1001/jama.2020.1585
6. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180(7):934–943. doi:10.1001/jamainternmed.2020.0994
7. Guo W, Li M, Dong Y, et al. Diabetes is a risk factor for the progression and prognosis of COVID‐19. Diabetes Metab Res Rev. 2020;36(7):e3319. doi:10.1002/dmrr.3319
8. Leulseged TW, Hassen IS, Maru EH, et al. Characteristics and outcome profile of hospitalized African patients with COVID-19: the Ethiopian context. PLoS One. 2021;16(11):e0259454–e. doi:10.1371/journal.pone.0259454
9. UNAIDS. HIV and AIDS estimates; 2020. Available from: https://www.unaids.org/en/regionscountries/countries/ethiopia.
10. Pal R, Bhadada SK, Misra A. COVID-19 vaccination in patients with diabetes mellitus: current concepts, uncertainties and challenges. Diabetes Metab Syndr. 2021;15(2):505–508. doi:10.1016/j.dsx.2021.02.026
11. Africa W. Ethiopia launches a COVID-19 vaccination campaign targeting the 12 years and above population; 2021. Available from: https://www.afro.who.int/news/ethiopia-launches-covid-19-vaccination-campaign-targeting-12-years-and-above-population.
12. Africa W. Ethiopia introduces COVID-19 vaccine in a national launching ceremony; 2021. Available from: https://www.afro.who.int/news/ethiopia-introduces-covid-19-vaccine-national-launching-ceremony.
13. World Health Organization. WHO SAGE Roadmap for prioritizing uses of COVID-19 vaccines; 2022. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-Vaccines-SAGE-Prioritization-2022.1.
14. Africa W. More than 21 million people have received at least one dose of vaccine as Ethiopia marks one year of COVID-19 vaccination; 2022. Available from: https://www.afro.who.int/countries/ethiopia/news/more-21-million-people-have-received-least-one-dose-vaccine-ethiopia-marks-one-year-covid-19.
15. Belsti YGY, Akalu Y, Dagnew B, et al. Willingness of Ethiopian population to receive COVID-19 vaccine.. J Multidiscip Healthc. 2021;14:1233–1243. doi:10.2147/JMDH.S312637
16. Abebe H, Shitu S, Mose A. Understanding of COVID-19 vaccine knowledge, attitude, acceptance, and determinates of COVID-19 vaccine acceptance among adult population in Ethiopia. Infect Drug Resist. 2021;14:2015–2025. doi:10.2147/IDR.S312116
17. Berihun G, Walle Z, Berhanu L, Teshome D. Acceptance of COVID-19 vaccine and determinant factors among patients with chronic disease visiting dessie comprehensive specialized hospital, Northeastern Ethiopia. Patient Prefer Adherence. 2021;15:1795–1805. doi:10.2147/PPA.S324564
18. Mesfin Y, Argaw M, Geze S, Zewdu BT. Factors associated with intention to receive COVID-19 vaccine among HIV positive patients attending ART clinic in Southwest Ethiopia. Patient Prefer Adherence. 2021;15:2731–2738. doi:10.2147/PPA.S342801
19. Alagoz O, Sethi AK, Patterson BW, et al. The impact of vaccination to control COVID-19 burden in the United States: a simulation modeling approach. PLoS One. 2021;16(7):e0254456. doi:10.1371/journal.pone.0254456
20. Guaraldi F, Montalti M, Di Valerio Z, et al. Rate and predictors of hesitancy toward SARS-CoV-2 vaccine among type 2 diabetic patients: results from an Italian Survey. Vaccines. 2021;9(5):460. doi:10.3390/vaccines9050460
21. Strupat C, Shigute Z, Bedi AS, Rieger M, Mugo PM. Willingness to take COVID-19 vaccination in low-income countries: evidence from Ethiopia. PLoS One. 2022;17(3):e0264633. doi:10.1371/journal.pone.0264633
22. Aldossari KK, Alharbi MB, Alkahtani SM, Alrowaily TZ, Alshaikhi AM, Twair AA. COVID-19 vaccine hesitancy among patients with diabetes in Saudi Arabia. Diabetes Metab Syndr. 2021;15(5):102271. doi:10.1016/j.dsx.2021.102271
23. Wang B, Li R, Lu Z, Huang Y. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging. 2020;12(7):6049–6057. doi:10.18632/aging.103000
24. Wang Y, Duan L, Li M, et al. COVID-19 vaccine hesitancy and associated factors among diabetes patients: a cross-sectional survey in Changzhi, Shanxi, China. Vaccines. 2022;10(1):129. doi:10.3390/vaccines10010129
25. Osuagwu UL, Langsi R, Ovenseri-Ogbomo G, et al. Analysis of perception, reasons, and motivations for COVID-19 vaccination in people with diabetes across Sub-Saharan Africa: a mixed-method approach. Int J Environ Res Public Health. 2022;19(13):7875. doi:10.3390/ijerph19137875
26. Bongomin F, Olum R, Andia-Biraro I, et al. COVID-19 vaccine acceptance among high-risk populations in Uganda. Ther Adv Infect Dis. 2021;8:20499361211024376. doi:10.1177/20499361211024376
27. Kanyanda S, Markhof Y, Wollburg P, Zezza A. Acceptance of COVID-19 vaccines in sub-Saharan Africa: evidence from six national phone surveys. BMJ Open. 2021;11(12):e055159. doi:10.1136/bmjopen-2021-055159
28. Agyekum MW, Afrifa-Anane GF, Kyei-Arthur F, Addo B, Karimi-Sari H. Acceptability of COVID-19 vaccination among health care workers in Ghana. Adv Public Health. 2021;2021:9998176. doi:10.1155/2021/9998176
29. Gabrani J, Schindler C, Wyss K. Health seeking behavior among adults and elderly with chronic health condition(s) in Albania. Front Public Health. 2021;9. doi:10.3389/fpubh.2021.616014
30. Mengiste AM, Bogale A, Yilma T, Yilma T. Information-seeking behavior and its associated factors among patients with diabetes in a resource-limited country: a cross-sectional study. Diabetes Metab Syndr Obes. 2021;14:2155–2166. doi:10.2147/DMSO.S289905
31. Sanyaolu A, Okorie C, Marinkovic A, et al. Comorbidity and its Impact on Patients with COVID-19. SN Compr Clin Med. 2020;2(8):1069–1076. doi:10.1007/s42399-020-00363-4
32. Vallée A, Fourn E, Majerholc C, Touche P, Zucman D. COVID-19 vaccine hesitancy among French people living with HIV. Vaccines. 2021;9(4):302. doi:10.3390/vaccines9040302
33. Maraqa B, Nazzal Z, Rabi R, Sarhan N, Al-Shakhra K, Al-Kaila M. COVID-19 vaccine hesitancy among health care workers in Palestine: a call for action. Prev Med. 2021;149:106618. doi:10.1016/j.ypmed.2021.106618
34. Guidry JPD, Laestadius LI, Vraga EK, et al. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infect Control. 2021;49(2):137–142. doi:10.1016/j.ajic.2020.11.018
35. Vassallo A, Shajahan S, Harris K, et al. Sex and gender in COVID-19 vaccine research: substantial evidence gaps remain. Front Global Women’s Health. 2021;2. doi:10.3389/fgwh.2021.761511
36. Adane M, Ademas A, Kloos H. Knowledge, attitudes, and perceptions of COVID-19 vaccine and refusal to receive COVID-19 vaccine among healthcare workers in northeastern Ethiopia. BMC Public Health. 2022;22(1):128. doi:10.1186/s12889-021-12362-8
37. Zewude B, Habtegiorgis T. Willingness to take COVID-19 vaccine among people most at risk of exposure in Southern Ethiopia. Pragmat Obs Res. 2021;12:37–47. doi:10.2147/POR.S313991
38. Hoque AM, Alam AM, Hoque M, Hoque ME, Van Hal G. Knowledge, attitudes, and practices towards COVID-19 of pregnant women at a primary health care facility. South Afr Eur J Med Health Sci. 2021;3(1):50–55.
39. Shmueli L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health. 2021;21(1):804. doi:10.1186/s12889-021-10816-7
40. Adedeji-Adenola H, Olugbake OA, Adeosun SA, Yunusa I. Factors influencing COVID-19 vaccine uptake among adults in Nigeria. PLoS One. 2022;17(2):e0264371. doi:10.1371/journal.pone.0264371
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
