Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 10 » Issue 1
Wheezing, a significant clinical phenotype of COPD: experience from the Taiwan Obstructive Lung Disease Study
Authors Huang W , Tsai Y, Wei Y , Kuo P , Tao C, Cheng S, Lee C, Wu Y , Chen N , Hsu W, Hsu J , Wang, Lin M, Chang H
Received 10 July 2015
Accepted for publication 18 August 2015
Published 7 October 2015 Volume 2015:10(1) Pages 2121—2126
DOI https://doi.org/10.2147/COPD.S92062
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Wan-Chun Huang,1 Ying-Huang Tsai,2 Yu-Feng Wei,3 Ping-Hung Kuo,4 Chi-Wei Tao,5 Shih-Lung Cheng,6 Chao-Hsien Lee,7 Yao-Kuang Wu,8 Ning-Hung Chen,9 Wu-Huei Hsu,10 Jeng-Yuan Hsu,11 Chin-Chou Wang,12 Ming-Shian Lin1,13
1Division of Pulmonary Medicine, Department of Internal Medicine, Ditmanson Medical Foundation Chia-Yi Christian Hospital, Chiayi, 2Department of Internal Medicine, Chang Gung Memorial Hospital, Chiayi, 3Department of Internal Medicine, E-Da Hospital/I-Shou University, Kaohsiung, 4Department of Internal Medicine, National Taiwan University Hospital, 5Department of Internal Medicine, Cheng-Hsin General Hospital, 6Division of Thoracic Medicine, Department of Internal Medicine, Far Eastern Memorial Hospital, 7Division of Pulmonary and Critical Care Medicine, Mackay Memorial Hospital, 8Division of Pulmonary Medicine, Department of Internal Medicine, Taipei Tzu Chi Hospital, Taipei, 9Department of Pulmonary and Critical Care Medicine, Chang Gung Memorial Hospital, Linkou, 10Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, China Medical University Hospital, 11Division of Chest Medicine, Taichung Veterans Genera Hospital, Taichung, 12Division of Pulmonary and Critical Care Medicine, Kaohsiung Chang Gung Memorial Hospital and Chang Gung University College of Medicine, Kaohsiung, 13Department of Respiratory Care, Chang Gung University of Science and Technology, Chiayi, Taiwan, Republic of China
Background: COPD is an important public health challenge with significant heterogeneity of clinical presentation and disease progression. Clinicians have been trying to find phenotypes that may be linked to distinct prognoses and different therapeutic choices. Not all patients with COPD present with wheezing, a possible clinical phenotype that can help differentiate patient subgroups.
Methods: The Taiwan Obstructive Lung Disease study was a retrospective, multicenter research study to investigate the treatment patterns of COPD after the implementation of the Global Initiative for Chronic Obstructive Lung Disease 2011 guidelines. Between November 2012 and August 2013, medical records were retrieved from patients with COPD aged ≥40 years; patients diagnosed with asthma were excluded. Demographic data, lung function, symptom scores, and acute exacerbation were recorded and analyzed, and the differences between patients with and without wheezing were evaluated.
Results: Of the 1,096 patients with COPD, 424 (38.7%) had the wheezing phenotype. The wheezing group had significantly higher COPD Assessment Test scores (12.4±7.8 versus 10.5±6.7, P<0.001), higher modified Medical Research Council grade (2.0±1.0 versus 1.7±0.9, P<0.001), and more acute exacerbations within the past year (0.9±1.3 versus 0.4±0.9, P<0.001) than the nonwheezing group. The postbronchodilator forced expiratory volume in 1 second was lower in wheezing patients (1.2±0.5 L versus 1.5±0.6 L, P<0.001). Even in patients with maintenance treatment fitting the Global Initiative for Chronic Obstructive Lung Disease 2011 guidelines, the wheezing group still had worse symptom scores and more exacerbations.
Conclusion: Wheezing is an important phenotype in patients with COPD. Patients with COPD having the wheezing phenotype are associated with worse symptoms, more exacerbations, and worse lung function.
Keywords: chronic obstructive pulmonary disease, acute exacerbation, wheezing phenotype
Introduction
COPD is a leading cause of morbidity and mortality worldwide and its burden is both substantial and increasing.1 Previous studies have shown heterogeneity of clinical phenotypes in patients with COPD, which may correlate with treatment response and disease progression.2–5 Identification of these phenotypes can help determine treatment choices to achieve better disease control.6,7
Wheezing is a feature of small airway narrowing that frequently occurs in patients with asthma; some clinicians used wheezing as a diagnostic criterion for asthma and asthma-COPD overlap syndrome (ACOS) if the patients had fixed airway obstruction.8 Previous studies showed that patients with ACOS are more likely to have wheezing and a higher risk of exacerbations.9–12 Notably, acute exacerbation (AE) is positively correlated with increased respiratory failure, hospitalizations, emergency department visits, and deaths in patients with COPD.13,14
Patients with COPD alone may also have wheezing; however, not all of them present with wheezing. The significance of wheezing and its correlation with clinical parameters in patients with COPD have not yet been identified.
In this study, we conducted a retrospective analysis of the Taiwan Obstructive Lung Disease (TOLD) cohort. The primary end point of this study was to investigate the prevalence of patients with COPD having the wheezing phenotype in Taiwan. The secondary end point was to analyze the clinical symptoms and the risk factors in patients with COPD with and without the wheezing phenotype.
Materials and methods
Study design and study subjects
In this study, we examined the data of participants enrolled in the TOLD study. Twelve hospitals across Taiwan participated in this study to investigate the relevant comorbidities and evaluate the implementation of the Global Initiative for Chronic Obstructive Lung Disease (GOLD) management strategy in patients with COPD. Data were abstracted from medical charts, including demographic characteristics, presence of wheezing, COPD severity, smoking history, pulmonary function test, and pharmacological therapy for the previous year.
Between November 2012 and August 2013, the participating physicians screened patients for entry into the study. Eligible patients were ≥40 years old with diagnosis of COPD based on the GOLD 2011 guidelines. Patients with a history of asthma were excluded. Demographic characteristics, symptom scores, presence of wheezing, AE, and pharmacological therapy were recorded and analyzed.
Data collection
Interviews were conducted by trained staff in charge of COPD case management who used a well-established questionnaire to collect the demographic information of the study participants, including date of birth, sex, smoking status, height, weight, and personal medical history. Body weight, height, and blood pressure were measured for each participant. Presence of wheezing was identified if the physicians of the participants recorded a positive result for wheezing in the medical charts. The questionnaire tools, including the modified Medical Research Council (mMRC) grade and COPD assessment test (CAT) score, were obtained to evaluate each patient’s severity of symptoms. An AE was defined as a worsening of symptoms that required antibiotics or steroids, emergency room visits, or hospitalizations. Frequent exacerbators referred to patients with two or more exacerbations within past 1 year. Postbronchodilator forced expiratory volume in 1 second (FEV1) criteria were assessed using the patients’ latest postbronchodilator FEV1. FEV1 within 1 year prior to the enrollment or the latest prebronchodilator FEV1 was substituted for the latest postbronchodilator FEV1 if it was not retrievable. Patients were classified into four grades, A, B, C, or D, by their COPD symptoms and risk of exacerbation according to the GOLD 2011 report.
Prescriptions of pharmacological therapy for COPD up to 1 year prior to the enrollment were collected. Inhaled bronchodilators or inhaled corticosteroids (ICSs) prescribed ≥6 months were regarded as the use of maintenance inhalers. Inhaled medications were evaluated according to the GOLD 2011 recommended pharmacological model. Overmedication was defined as overprescribed medication, despite GOLD 2011 recommendations.
Differences in basic demographics, pharmacological therapy, and pulmonary function tests were compared between patients with and without wheezing. Clinical symptoms and exacerbations were also assessed.
The study protocol was reviewed and approved by institutional review boards of all the hospitals involved.
Statistical analysis
Data were analyzed using SAS statistical software for Windows, version 9.3 (SAS Institute Inc., Cary, NC, USA). Continuous data were expressed as mean ± standard deviation. Student’s t-test was used when the data were normally distributed; otherwise, the nonparametric Mann–Whitney U-test was used. Categorical data were compared using the chi-square test if the observed numbers in all categories were larger than 5; otherwise, Fisher’s exact test was used.
Results
Of the 1,096 participants, 424 patients (38.7%) had wheezing. There was no significant difference in age, sex, body mass index, and smoking history between patients with COPD with and without the wheezing phenotype. Table 1 shows that the wheezing group had significantly higher CAT (12.4±7.8 versus 10.5±6.7, P<0.001) and mMRC scores (2.0±1.0 versus 1.7±0.9, P<0.001) than the nonwheezing group. Notably, the wheezing group had significantly more episodes of AE within the past 1 year (0.9±1.3 versus 0.4±0.9, P<0.001) and a higher risk of developing the frequent exacerbator phenotype (23.3% versus 8.2%, P<0.001) than the nonwheezing group.
Table 2 shows the spirometry data of the study population. Postbronchodilator FEV1 and forced vital capacity were significantly lower in patients with the wheezing phenotype (1.2±0.5 L versus 1.5±0.6 L and 2.2±0.7 L versus 2.5±0.7 L, both P<0.001) compared with patients without the wheezing phenotype. However, in terms of reversibility of FEV1 after bronchodilator, no statistical difference was found.
Among patients who received long-term maintenance treatment fitting the GOLD 2011 guidelines (470/1,096; 42.9%), patients with the wheezing phenotype (183/470; 38.8%) also had significantly higher CAT (12.6±8.1 versus 9.9±6.5, P<0.001) and mMRC scores (2.1±1.1 versus 1.7±0.8, P<0.001) compared with patients without the wheezing phenotype. Additionally, a significantly higher percentage of AE was also found in the wheezing group than in the nonwheezing group (1.1±1.4 versus 0.5±1.1, P<0.001; Table 3).
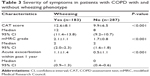  | Table 3 Severity of symptoms in patients with COPD with and without wheezing phenotype |
Table 4 shows that patients with wheezing history in GOLD groups A and B had significantly higher percentages of ICS usage than patients without wheezing history (43.2% versus 23.4% in GOLD group A, P=0.0088; 45.6% versus 29.8% in GOLD group B, P=0.0017). In addition, high rates of overmedication were also found in patients with wheezing history.
Discussion
This study shows the prevalence of wheezing in a nationwide COPD cohort. Patients with the wheezing phenotype had worse clinical symptoms and lower levels of spirometry results. Wheezing also correlated with a higher possibility of AE. Even among those who were treated according to the GOLD 2011 guidelines, patients with wheezing still had worse symptom scores and more exacerbations.
Wheezing can be detected in all mechanisms causing airway narrowing, especially COPD and asthma. In addition, patients with COPD do not always present with wheezes.15 Godfrey et al indicated that only 70% of severe airflow obstruction patients presented with wheezing.16 Notably, Kulich et al used electronic diaries to identify the relevant symptoms, including wheezing, and degree of bother due to symptoms in moderate-to-severe patients with COPD;17 their results indicated that only “shortness of breath” showed a significant association with “bother” and “difficulty with activities”.17 However, to date, little is known regarding whether or not wheezing present in patients with COPD is associated with other clinical conditions. In this study, we confirmed that wheezes in patients with COPD had a significantly higher frequency of AE and worse clinical symptoms than patients without wheezes. Similar results were observed in patients with COPD having adequate maintenance therapy according to GOLD 2011 guidelines. Therefore, wheezing should be identified as a phenotype of COPD, which we would suggest a definition as audible wheezing breathing sounds identified by clinicians in a patient with COPD.
ACOS has been discussed extensively as a phenotype of COPD. Patients with ACOS had a significantly higher risk of frequent exacerbations than patients with COPD.9,11,12,18 Additionally, Kauppi et al reported that patients with ACOS had significantly worse quality of life than patients with COPD alone.10 The Spanish guideline reported by Miravitlles et al was the first guideline that clearly described the multidimensional basis of recognition of clinical phenotypes, severity of rating scales, and specific therapeutic approach in patients with ACOS and/or COPD.19 However, accurate diagnosis of ACOS is still difficult for clinicians to obtain. Nevertheless, patients with a history of asthma were excluded from our cohort. Moreover, the airway responsiveness, the change in FEV1 after administration of an inhaled short-acting bronchodilator, was not different between patients with and without wheezing phenotypes. Therefore, the patients enrolled in our cohort should have COPD alone. This suggests that the presence of wheezing is a phenotype of COPD that is associated with poor patient-rated symptom scores and more frequent exacerbations, instead of a characteristic of ACOS.
According to the GOLD 2011 guidelines, ICSs are not a recommended therapy for patients with COPD in the GOLD A and GOLD B groups. Our results revealed that patients with the wheezing phenotype in both GOLD groups had a significantly higher frequency of ICS use and ratio of overmedication than patients without the wheezing phenotype. This observation was possible due to the concern of ACOS by clinicians, for which an ICS is suggested in the treatment regimen.20,21 Since the possibility of ACOS in our cohort was actually low, the observation warrants the necessity of better diagnosis to achieve better discrimination between COPD alone and ACOS.
In the study of Sanchez Morillo et al, computerized analysis of respiratory sounds identified two possible phenotypes of COPD exacerbation.22 The patients who belonged to the first phenotype were characterized by higher values of FEV1 and absence of abnormal sounds. The other phenotype included patients who presented with pronounced adventitious breathing sounds. The result, alone with our findings and previous reports, suggests that wheezes can be absent in patients with COPD and that COPD may actually include heterogeneous patient groups who have different clinical and prognostic characteristics.2,7 More studies about breathing sounds evolution in patients with COPD are warranted to validate this idea and to connect clinical features with underlying pathophysiology and etiology. The consistency in breathing sounds evaluation between clinicians and computerized analysis should also be researched.
Previous studies reported higher risk of wheezing in current smokers, and female smokers had even greater risk than male smokers.23,24 In this study, the percentage of current smoking did not show statistical significance between patients with wheezing and without wheezing. However, our cohort included only patients with COPD and consisted of mainly male patients, which may explain the inconsistent findings between our study and previous reports. Further studies are necessary to identify the influence of smoking habit on the risk of wheezing in patients with COPD.
Researches regarding phenotypes of childhood wheezing disorders have been available in the past few decades.25,26 Spycher et al recently reviewed the definitions of those phenotypes and their prospective validation.27 The authors also suggested multidimensional approaches to define phenotypes that can help with genetic research and our understanding about underlying pathophysiological pathways. Similarly, phenotypes of COPD, in addition to ACOS, need to be validated more carefully so that we can identify risk factors, prognostic, and distinct treatment plans.
The study was limited by its retrospective data collection. Although the presence of wheezing was associated with poor symptoms and more exacerbations, whether or not patients were treated according to widely accepted guidelines, the prediction of wheezing phenotype for quality of life, and risk of exacerbation in the future is not known. Further prospective study is necessary to confirm its clinical relevance as a phenotype of COPD.
Another limitation of this study was the possibility of ACOS in our cohort. There is currently no consensus regarding the diagnosis of ACOS, which brings difficulties for study design. We excluded patients with history of asthma so that the diagnosis of ACOS should be unlikely for our patients. Furthermore, there were only 31 patients (2.8%) who had a postbronchodilator increase in FEV1 >12% and 400 mL, a spirometric feature of ACOS proposed by Global Initiative for Asthma (GINA) and GOLD.20 Nevertheless, the accuracy would be even better if more parameters were used, for example, blood eosinophils, sputum samples, and more detailed past history and family history.
Conclusion
In conclusion, wheezing is a clinical significant phenotype of COPD. Patients with COPD having the wheezing phenotype are associated with worse quality of life, more exacerbations, and a lower level of pulmonary function test performance. Even among those patients who were treated according to the GOLD 2011 guidelines, patients with wheezing still had worse symptom scores and more exacerbations. More studies are needed to further validate its clinical relevance; adjustment in treatment suggestions for patients with wheezing may also be necessary.
Acknowledgments
The TOLD study received financial support from Novartis Pharmaceuticals Corporation. Data management and statistical analysis were supported by the CRO service division of Formosa Biomedical Technology Corp. The abstract of this paper was presented at the American Thoracic Society 2015 International Conference as a poster presentation with interim findings.28 The actual paper, however, has never been published.
Disclosure
The authors report no conflicts of interest in this work.
References
Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347–365. | ||
Agusti A, Sobradillo P, Celli B. Addressing the complexity of chronic obstructive pulmonary disease: from phenotypes and biomarkers to scale-free networks, systems biology, and P4 medicine. Am J Respir Crit Care Med. 2011;183(9):1129–1137. | ||
Han MK, Agusti A, Calverley PM, et al. Chronic obstructive pulmonary disease phenotypes: the future of COPD. Am J Respir Crit Care Med. 2010;182(5):598–604. | ||
Pistolesi M, Camiciottoli G, Paoletti M, et al. Identification of a predominant COPD phenotype in clinical practice. Respir Med. 2008;102(3):367–376. | ||
Jo KW, Ra SW, Chae EJ, et al. Three phenotypes of obstructive lung disease in the elderly. Int J Tuberc Lung Dis. 2010;14(11):1481–1488. | ||
Bahadori K, FitzGerald JM. Risk factors of hospitalization and readmission of patients with COPD exacerbation – systematic review. Int J Chron Obstruct Pulmon Dis. 2007;2(3):241–251. | ||
Allen-Ramey FC, Gupta S, DiBonaventura MD. Patient characteristics, treatment patterns, and health outcomes among COPD phenotypes. Int J Chron Obstruct Pulmon Dis. 2012;7:779–787. | ||
Chung JW, Kong KA, Lee JH, Lee SJ, Ryu YJ, Chang JH. Characteristics and self-rated health of overlap syndrome. Int J Chron Obstruct Pulmon Dis. 2014;9:795–804. | ||
Hardin M, Silverman EK, Barr RG, et al; COPDGene Investigators. The clinical features of the overlap between COPD and asthma. Respir Res. 2011;12:127. | ||
Kauppi P, Kupiainen H, Lindqvist A, et al. Overlap syndrome of asthma and COPD predicts low quality of life. J Asthma. 2011;48(3):279–285. | ||
Miravitlles M, Soriano JB, Ancochea J, et al. Characterisation of the overlap COPD-asthma phenotype. Focus on physical activity and health status. Respir Med. 2013;107(7):1053–1060. | ||
Menezes AM, Montes de Oca M, Pérez-Padilla R, et al; PLATINO Team. Increased risk of exacerbation and hospitalization in subjects with an overlap phenotype: COPD-asthma. Chest. 2014;145(2):297–304. | ||
Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet. 2007;370(9589):786–796. | ||
MacIntyre N, Huang YC. Acute exacerbations and respiratory failure in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2008;5(4):530–535. | ||
Meslier N, Charbonneau G, Racineux JL. Wheezes. Eur Respir J. 1995;8(11):1942–1948. | ||
Godfrey S, Edwards RH, Campbell EJ, Armitage P, Oppenheimer EA. Repeatability of physical signs in airways obstruction. Thorax. 1969;24(1):4–9. | ||
Kulich K, Keininger DL, Tiplady B, Banerji D. Symptoms and impact of COPD assessed by an electronic diary in patients with moderate-to-severe COPD: psychometric results from the SHINE study. Int J Chron Obstruct Pulmon Dis. 2015;10:79–94. | ||
Barrecheguren M, Esquinas C, Miravitlles M. The asthma-chronic obstructive pulmonary disease overlap syndrome (ACOS): opportunities and challenges. Curr Opin Pulm Med. 2015;21(1):74–79. | ||
Miravitlles M, Soler-Cataluna JJ, Calle M, et al. Spanish guideline for COPD (GesEPOC). Update 2014. Arch Bronconeumol. 2014;50(suppl 1):1–16. | ||
Global Initiative for Asthma, Global Initiative for chronic Obstructive Lung Disease (GOLD). Asthma, COPD, and asthma-COPD overlap syndrome. 2014. Available from: http://www.goldcopd.org/asthma-copd-overlap.html. | ||
Kitaguchi Y, Komatsu Y, Fujimoto K, Hanaoka M, Kubo K. Sputum eosinophilia can predict responsiveness to inhaled corticosteroid treatment in patients with overlap syndrome of COPD and asthma. Int J Chron Obstruct Pulmon Dis. 2012;7:283–289. | ||
Sanchez Morillo D, Astorga Moreno S, Fernandez Granero MA, Leon Jimenez A. Computerized analysis of respiratory sounds during COPD exacerbations. Comput Biol Med. 2013;43(7):914–921. | ||
Bjerg A, Ekerljung L, Middelveld R, et al. Increased prevalence of symptoms of rhinitis but not of asthma between 1990 and 2008 in Swedish adults: comparisons of the ECRHS and GA(2)LEN surveys. PLoS One. 2011;6(2):e16082. | ||
Bjerg A, Ekerljung L, Eriksson J, et al. Higher risk of wheeze in female than male smokers. Results from the Swedish GA 2 LEN study. PLoS One. 2013;8(1):e54137. | ||
Martinez FD, Wright AL, Taussig LM, Holberg CJ, Halonen M, Morgan WJ. Asthma and wheezing in the first six years of life. The Group Health Medical Associates. N Engl J Med. 1995;332(3):133–138. | ||
Brand PL, Baraldi E, Bisgaard H, et al. Definition, assessment and treatment of wheezing disorders in preschool children: an evidence-based approach. Eur Respir J. 2008;32(4):1096–1110. | ||
Spycher BD, Silverman M, Kuehni CE. Phenotypes of childhood asthma: are they real? Clin Exp Allergy. 2010;40(8):1130–1141. | ||
Huang WC, Chen W, Lin MS. Wheezing, A Significant Clinical Phenotype of Chronic Obstructive Pulmonary Disease. Experience From TOLD (Taiwan Obstructive Lung Disease) Study. In: American Thoracic Society 2015 International Conference; May 15–20, 2015; Denver; Meeting Abstract, Vol 191. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



