Back to Journals » Patient Preference and Adherence » Volume 17
What Do We Know about Medication Adherence Interventions in Inflammatory Bowel Disease, Multiple Sclerosis and Rheumatoid Arthritis? A Scoping Review of Randomised Controlled Trials
Authors King K , McGuinness S , Watson N, Norton C, Chalder T , Czuber-Dochan W
Received 2 June 2023
Accepted for publication 13 September 2023
Published 13 December 2023 Volume 2023:17 Pages 3265—3303
DOI https://doi.org/10.2147/PPA.S424024
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Video abstract presented by Kathryn King.
Views: 81
Kathryn King,1 Serena McGuinness,1 Natalie Watson,1 Christine Norton,1 Trudie Chalder,2 Wladyslawa Czuber-Dochan1
1Florence Nightingale Faculty Nursing, Midwifery and Palliative Care, King’s College London, London, UK; 2Department of Psychological Medicine, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, UK
Correspondence: Kathryn King, Email [email protected]
Purpose: Between 53% and 75% of people with inflammatory bowel disease, 30%– 80% with rheumatoid arthritis, and up to 50% with multiple sclerosis do not take medications as prescribed to maintain remission. This scoping review aimed to identify effective adherence interventions for inflammatory bowel disease, but with few studies found, multiple sclerosis and rheumatoid arthritis were included to learn lessons from other conditions.
Methods: Full and pilot randomised controlled trials testing medication adherence interventions for inflammatory bowel disease, multiple sclerosis, and rheumatoid arthritis conducted between 2012 and 2021 were identified in six electronic databases.
Results: A total of 3024 participants were included from 24 randomised controlled trials: 10 pilot and 14 full studies. Eight investigated inflammatory bowel disease, 12 rheumatoid arthritis, and four multiple sclerosis. Nine studies (37.5%) reported significantly improved medication adherence, all involving tailored, personalised education, advice or counselling by trained health professionals, with five delivered face-to-face and 1:1. Quality of effective interventions was mixed: five rated high quality, two medium and two low quality. Interventions predominantly using technology were likely to be most effective. Secondary tools, such as diaries, calendars and advice sheets, were also efficient in increasing adherence. Only 10 interventions were based on an adherence theory, of which four significantly improved adherence.
Conclusion: Tailored, face-to-face, 1:1 interactions with healthcare professionals were successful at providing personalised adherence support. Accessible, user-friendly technology-based tools supported by calendars and reminders effectively enhanced adherence. Key components of effective interventions should be evaluated and integrated further into clinical practice if viable, whilst being tailored to inflammatory conditions.
Plain Language Summary: Introduction: Inflammatory bowel disease (IBD), multiple sclerosis (MS), and rheumatoid arthritis (RA) are inflammatory diseases where the immune system causes inflammation by mistakenly attacking itself. These lifelong conditions cannot be cured, but can usually be controlled by medication. Medication is most effective when taken as prescribed, called “adherence”. For multiple reasons, between five and eight in 10 people with IBD, RA, and MS do not take medications as advised. This review aimed to identify research that tested ways to help people living with IBD, MS, and RA take medications as prescribed. Identifying and understanding what helps can increase patient well-being and improve quality of life through better controlled inflammatory conditions.
Methods: Studies testing medication adherence interventions for IBD, MS, and RA conducted between 2012 and 2021 were identified from six electronic databases.
Results: A total of 3024 people with inflammatory conditions took part in 24 studies (eight on IBD, four on MS, and 12 on RA). Nine studies reported significantly improved medication adherence, all involving personalised education, advice or counselling by trained health professionals, with five delivered face-to-face and individually. Interventions predominantly using technology were the most effective. Diaries, calendars, and advice sheets also increased adherence. Ten of the interventions were based on an adherence theory, of which four improved adherence.
Conclusions: Personalised adherence support was successful when:tailored to patient,one-to-one and face-to-face,with healthcare professionals,involving technology-based tools, andsupported by calendars/reminders.
Components of effective interventions should be used in clinical practice where possible, made specific to each inflammatory condition.
Keywords: IBD, MS, RA, treatment, medicine, drug, concordance
Introduction
Inflammatory diseases comprise a group of chronic conditions where the immune system mistakenly attacks the body’s tissue, causing inflammation.1 This can lead to chronic pain, redness, swelling, stiffness, and tissue damage. For the purposes of this review, the inflammatory diseases selected were inflammatory bowel disease (IBD), multiple sclerosis (MS), and rheumatoid arthritis (RA).2 All three conditions are incurable, yet have recognised medications to treat, induce, or maintain remission or treat a flare-up, altering the overall disease course for many people.
If treatment is taken as prescribed, for most individuals, outcomes are good, but typically this relies on a high adherence rate. However, like many chronic conditions, non-adherence is problematic in inflammatory diseases, potentially contributing to disease progression and the development of short- and long-term complications. Between 53% and 75% of people with IBD,3,4 30%–80% with RA,5 and up to 50% with MS6,7 do not take prescribed medications as advised. Some 15% of individuals with chronic conditions never even redeem their prescriptions.8 Therapeutic adherence has also been drastically impacted by the COVID-19 pandemic.9 Consequences of non-adherence include increased disease activity and rate of relapse, loss of response to treatment, poor quality of life (QoL), higher disability, morbidity and mortality and additional health expenditure.3 Non-adherence is not unique to a specific condition, yet recognising and improving adherence is a primary goal for treatment to keep symptoms quiescent.10
In many long-term conditions, when feeling well, an ability to cope “without medication” is often reported.11,12 This can lead to the adverse effect of poor disease control.13 More specifically, due to the fluctuating nature of IBD, for example, being “ill”, has been reported by some people living with IBD as not necessarily a continual state. Certain patients have taken this to mean that medication should only be taken during “illness” or flare-ups.14 Being told to take medications regardless of whether an individual feels well or not makes no sense to some, leading to non-adherence. In addition, people living with inflammatory conditions often query the need for pharmacological treatments, voicing concerns about dependence and harmful drug effects.12,14,15
Adherence is influenced by a multitude of interlinked patient-related and healthcare-related factors (eg, symptoms, treatment type, administration route, side effects, medication costs, healthcare beliefs, social circumstances, and culture).11–13 These result in multiple barriers to adherence behaviour.16 Barriers include perceptual and motivational issues (eg, intentionally missing doses through treatment concerns or wanting to be normal) or practical capabilities (eg, unintentionally forgetting doses). All of these are recognised in the perceptions and practicalities approach (PAPA) for supporting adherence.17 The PAPA suggests ways of facilitating adherence. The primary purpose of an adherence intervention is to identify barriers to adherence and target them for individual behaviour change. However, lifestyle change after an inflammatory condition diagnosis can be difficult,18 and few adherence interventions acknowledge these barriers.19 More specifically for IBD, MS, and RA, despite evidence showing non-adherence is largely associated with psychological factors, including anxiety or depression,2,16,20,21 these are often overlooked.11 Conversely, interventions designed to reduce anxiety or depression may not target or measure adherence,10,22 leading to short-term or minimal impact on adherence.20,23–27 Of those studies that have acknowledged the psychological background to non-adherence, few have explored the role of psychotherapy in improving medication adherence,28 yet those that did, found no impact on adherence.29
There has been a notable lack of theoretical frameworks addressing behaviour change in adherence research.3 Adherence changes have often been transient, minimally impacting longer-term clinical outcomes.30,31 Most positive results come from complex behaviour change interventions.30,31 Patient education is also lacking: it is rarely used in adherence promotion3 and seldom offered at clinical appointments.32 General Practitioners tend not to provide specialist inflammatory condition information and management, which can cause patient–clinician discordance.3,33 Poor patient understanding of treatment leads to patient frustration, low adherence, and dissatisfaction with care.34,35
Web-based interventions and telemedicine are favoured by many patients, due to ease of access and reduction in travel.36 However, these contemporary interventions have been criticised for lacking tailored, individualised support, resulting in limited information exchange and improvement in adherence.4,18,31,37 Interactive interventions with multifaceted education and psychological support have been found to be most efficacious in improving medication adherence.3,38,39 However, effective adherence interventions are rarely used in routine clinical practice.3,4,40
Overall, although there are many interventions designed to increase medication adherence, few have shown long-term effectiveness.41 Better management strategies are critical to improve adherence and thereby prevent adverse outcomes, including acute flare-ups and increased disability.4,42 To achieve this, identifying the most reliable evidence on the effectiveness of adherence intervention components is key. It was anticipated by the authors that there would be a greater number of IBD adherence interventions. However initial searching suggested this was very limited. The search was thus expanded to include the inflammatory conditions of MS and RA.
No previous review has drawn together evidence on the effect of adherence interventions in several conditions. We thus conducted a scoping review in which adherence interventions were evaluated for effectiveness by pilot and efficacy randomised controlled trials (RCTs) in the inflammatory conditions of IBD, MS, and RA. Finally, we identified the intervention techniques used by adherence interventions to feed into the development and evaluation of a new intervention to promote adherence.
Methods
The aim of this scoping review was to identify and review pilot and efficacy RCTs testing medication adherence interventions initially for IBD, with this subsequently being expanded to MS and RA. All papers written in English published from 2012 with participants ≥18 years of age with a diagnosis of IBD, MS or RA, who were prescribed one or more medications for their condition were included.
Search Strategy
Six electronic databases (Medline, PubMed, Embase, CINAHL, British Nursing Index, and PsycInfo) were searched systematically in December 2021 to identify published articles from peer-reviewed journals relevant to the review’s aims. Reference lists of included studies were also searched for appropriate papers and duplicates were removed. A combination of terms relating to adherence, the inflammatory conditions (IBD, MS, or RA), and interventions were used to search the databases. (A full list of formatted search terms adapted for each database can be found in Supplementary Table 1).
Retrieved studies were exported into EndNote 20 and transferred to Covidence (version 2) reference management software. Three reviewers (KK, SM, NW) screened the titles and abstracts of retrieved papers according to pre-determined inclusion criteria. Two reviewers (SM, NW) were assigned 50% each of the full text papers for data extraction. A third reviewer (KK) performed double data extraction on all included studies, and any disagreements were resolved through discussion with all three reviewers. A flow diagram (Figure 1) reports the selection process and provides reasons for exclusion, as suggested by PRISMA-P guidelines.43
 |
Figure 1 PRISMA flow diagram: selection of studies for scoping review. Notes: PRISMA figure adapted from Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. Creative Commons.43 |
Quality Appraisal
The Critical Appraisal Skills Programme (CASP) tool for RCTs was used to assess the quality of included papers. In line with recommendations,44 a CASP scoring system was not used. Instead, a systematic rating system was devised for scoring by the research team. Each study was given a base score of three. One point was subtracted if the study did not use a validated adherence measure and one point was subtracted if the authors did not use intention-to-treat analysis. This resulted in scores of three (high), two (medium), or one (low) quality. No study was excluded based on quality assessment.
Data Synthesis
Due to the heterogeneity of interventions, it was inappropriate to conduct a meta-analysis of the data. Therefore, studies were synthesised narratively along with descriptive tabulation (Results, Table 1).
 |
Table 1 Overview of included studies |
Results
A total of 14,466 papers were identified from six databases and from searching reference lists of included studies. After screening titles and abstracts, 369 papers remained for full text eligibility screening. A total of 24 papers were included in the scoping review and underwent data extraction (Table 1).
Demographics
Across the 24 studies, eight (33.3%) investigated IBD, four (16.7%) MS and 12 (50%) RA. Eleven studies were conducted in Europe (45.8%), including two in the UK (8%), with seven in the US (29%), four (16.6%) in Asia (Iran, China, Thailand and Singapore), and two studies did not report study country/continent. In total, 3024 participants were randomised, ranging from 18 to 909 per study. Participant ages ranged from 18 to 81 years, and all studies included both male and female participants, except one, which had 100% female participants.51
In terms of design, 10 (41.7%) studies were pilot RCTs (and thus may not be reasonably expected to reach statistical significance), with the remainder being efficacy RCTs. Studies largely had two arms and were delivered at a single centre. Two studies reported double-blinding, four did not report blinding, nine studies were unblinded, and the remaining nine used variants of single-blinding. Intervention length spanned from 15 minutes to 12 weeks, with follow-up duration ranging from six weeks to 18 months from randomisation. Table 1 gives further details of the included studies and Table 2 shows specific information regarding the interventions.
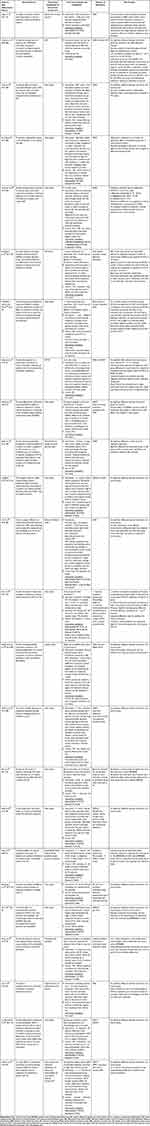 |
Table 2 Description of interventions |
Adherence Improvements
Four full RCTs showed a significant improvement in medication adherence,45,47,49,59 as did five pilot RCTs48,50,54,57,62 (Table 2). These full RCT interventions ranged from three 40 minute sessions over 3 weeks to a 12 month period, with 6−18-month follow-up. For the five pilot studies, interventions lasted from 90 days to 12 months, with follow-up of 3–12 months. One additional pilot study found significant outcomes measured by one adherence measure but not another.4 Intervention access and follow-up lasted 3 months.
There were also two (16.7%) pilot RCTs51,58 and two full RCTs60,61 with statistically significant adherence improvements shown during the course of follow-up, but not at the final post-intervention time point. Interventions for these full RCTs ran from an average of 9.2 minutes to 30 minutes, with follow-up from 12 weeks to 6 months. These pilot interventions ranged from 6 weeks to 6 months, with follow-up periods of 12 weeks to 6 months.51,58 However, one pilot study did not specify their primary outcome time point.58
All nine significantly effective interventions involved face-to-face or remote interaction with a healthcare professional throughout the intervention (separately from data collection staff). Either nurses,47,48,59 gastroenterologists,47 a therapist,62 pharmacist,54 researchers45,57 and rheumatologists49,52 were trained in an approach for intervention delivery. In one study, beneficial effects of involving nurses with knowledge of RA combined with delivery of patient-centred education was demonstrated.59 In another study using a web-based platform, continuous communication between patients and health providers was facilitated via electronic messaging, resulting in significant improvement in medication adherence.48 Adherence reached 100% in participants completing the web-based platform. This was attributed by the authors to continual adaptation of care in relation to the participant’s disease activity and optimal communication.
Effective interventions mostly incorporated a form of tailoring with educational support for participants, where they had opportunities to ask questions about their needs. Interactive education, counselling, goal setting and a joint fitness programme centred around RA resulted in significantly improved medication adherence.49 Monitoring with tailored support for participants with IBD led to positive, significant adherence effects, reduced social impairment and daily activity interference.45,51 Patient satisfaction was high and health-related QoL improved. Similarly, success of a tailored health behaviour change intervention to fit the needs of participants living with RA, including health literacy was also reported.45 Personalised tailoring was applied by another study,59 enabling intervention participants to have their individual needs as the central focus. Primary outcome measures indicated a significant increase in adherence rates for intervention participants, both at 12 and 24 weeks.
Over half (five of nine) of successful interventions were delivered face-to-face and 1:1.45,49,50,59,62 A range of approaches were used, including principles of cognitive behavioural therapy (CBT),49 motivational interviewing (MI)59 and visual feedback49,52 (see Table 2 and Figures 2 and 3; outlining intervention approaches used). Of the studies with statistically significant changes in adherence, all those involving a face-to-face intervention were graded highly in terms of quality,45,47,48,57 with one exception graded as medium.54 Interventions without a face-to-face approach were rated medium59,62 or low quality.49,52
 |
Figure 2 Categories of interventions. |
 |
Figure 3 Categories of significantly effective interventions. |
Adherence Measurement
The most common method of adherence measurement was via a self-report questionnaire. The Morisky Medication Adherence Scale (MMAS)68 was used in 10 studies, followed by the Medication Adherence Report Scale (MARS)69 in five studies. One intervention collated data via study-specific medication taking behaviours (for example, whether medication was stopped due to intolerance) to measure adherence.49 Four studies included pill and/or syringe counts to assess adherence,58,60,61,64 whereas only three used electronic medication monitoring,54,57,65 despite the latter approach being considered the “gold standard” of adherence monitoring.71–76 Objective physiological measures (blood and urine tests), calendars and diaries were less commonly used, and almost half the studies used a combination of methods to measure adherence.4,51,54–61,64,68
Ineffective Interventions
Eight studies showed no significant effect on medication adherence,36,46,52,53,55,56,63,65 but two of these were pilot studies only.52,55 These varied across length of intervention from 15 minutes63 to 12 months36,46,64–66 and follow-up from 1 month63 to 14 months.56 Sample size and attrition rate, use of theory and approach were also variable amongst these interventions. Within these eight, the two pilot studies52,53 and two of the full RCTs utilised behaviour change and psychological methods,46,65 and four applied education36,46,56,63 as intervention components.
An additional two full RCT interventions showed no significant difference compared to controls but also had detrimental effects on adherence at completion or on adherence-related beliefs.64,66 However both studies were graded high quality, interventions were not theoretically-based and involved pharmacists delivering motivational interviewing. Each study was 12 months duration, utilising the Compliance Questionnaire Rheumatology measure of adherence.76
Inflammatory Condition Type
The eight IBD interventions showed a variable success rate. The two effective IBD interventions utilised web-based interventions, one full RCT offering education modules and “red flag” monitoring of disease activity, with a web-based platform compared with telephone education.47 The effective pilot study used text message reminders with direct tailored feedback.48
For the four MS interventions, home-based coaching support with nurses, including a web-based journal to track participants’ progress with the Rebismart device led to adherence improvements in the intervention group.36 However, these were non-significant between groups. Similarly, an internet-based pilot programme delivering personalised text or email adherence reminders showed a moderate effect on adherence for only participants living alone and not in the main analysis.58 Pilot studies involving both an electronic pill bottle cap with audio-visual medication reminders57 and motivational interviewing–based telephone counselling62 led to significant adherence improvements for participants with MS compared with controls.
For the 12 RA interventions, five (41.6%) studies were effective,45,49,50,54,59 including two pilot interventions.50,54 Of the five studies that showed significant differences between groups, three used psychological behaviour change approaches.45,49,59 A mixture of educational and technological techniques were also successful through telephone-education sessions with trained nurses,59 participants viewing their disease progression on the clinical computer system50 or receiving weekly text message reminders to take RA medication.54
Multicomponent Interventions
All nine significantly effective interventions45,47–50,54,57,59,62 utilised two or more components within their intervention, often with a predominant component and then a secondary one (Figures 2 and 3. See Supplementary Table 2 for more detail). Two interventions incorporated a combination of technology, education, monitoring and web-based platforms that registered disease activity and adherence.47,48 Progression of IBD activity, medication use, body weight, vital signs and testing schedules were logged,48 all of which were fed back to the participant, researchers and the healthcare provider. Conversely, a mixture of 10 studies (both pilot and full RCTs) that were not significantly effective at improving adherence utilised at least two or more intervention components.4,36,46,53,55,58,60,64–66 Seven of these 10 were not theory-based,36,46,58,60,64–66 and those that were either had low intervention completion4,53 or were a pilot study with low sample size.55
In seven of the nine significantly effective studies, the application of technology was predominant. Two studies offered telephone-based education sessions.48,50 Reminder systems through text messages54 and a “Pillsy bottle” with audio-visual reminders (where the bottle blinked and beeped if unopened at the scheduled dosing time, every 10 minutes for up to an hour)57 were also utilised. Both disease activity monitoring48 and adherence monitoring57 only significantly impacted adherence in two studies when as the primary intervention, monitoring was combined with a technology-assisted approach. In two other studies, monitoring of disease activity47 and medication taking behaviour,62 was helpful as an additional secondary intervention. Another study using technology and counselling was tailored to participants’ needs with a view to empowering patients, yet did not significantly affect adherence.53 As secondary interventions, tools (such as diaries, calendars, and advice sheets) were most commonly used, with 80% of studies in this category being significantly effective. Frequent recording and checking of intended medication adherence via a calendar were successful in significantly improving medication taking.45 Only 37.5% of interventions with educational components resulted in significant adherence improvements. Of those which were effective, education was offered on a 1:1 basis with three to four sessions lasting between 20–40 minutes45,48,59 or educational information was accessible for at least 12 weeks or more.47,48
Theoretical Basis
There were inconsistent results with a wide range of theoretically-based interventions. Only 10 interventions offered a theory to explain adherence behaviours; of which four reported significant adherence improvements post intervention. The four theories were: a) the health belief model, where perception of threats, barriers and cues predict health behaviours,59 b) the health action process approach, applying coping planning techniques to overcome barriers to adherence,45 c) CBT; emphasising learning new skills helpful in disease management49 and d) transtheoretical model with motivational interviewing (MI) and multiple stages facilitating behaviour change, supported by different strategies minimising resistance and maximising engagement.62 Each of these approaches theoretically underpinned one intervention with statistically significant effects on adherence. Two studies64,66 utilised MI as the theoretical basis of the intervention, yet neither explained the evidence-basis for its use. Both reported non-significant results.
Intervention development was explored in most depth with the PAPA theoretical framework,4 outlining the application of a range of recommendations, guidelines and research. Advisory panels of experts and patients were consulted, and further usability testing was carried out. Behaviour change techniques were used to develop content, context, and delivery vehicle; however, no significant effects on adherence were reported. Similarly, CBT and MI,51 health behaviour and social learning theory,52 elaboration likelihood model (ELM),53 systems theory55 and cognitive theory of multimedia learning process63 were all incorporated within interventions, yet led to non-significant effects on adherence. The remaining 12 (58.3%) studies did not utilise a theory to develop their intervention.36,46–48,50,54,56–58,60,61,65 Despite this, almost half (five) of these significantly improved adherence.47,48,50,54,57
Completion Rates
Completion rates of both intervention and primary outcome were variable across studies, ranging from 38.9%51 to 100% for primary outcome completion62 and from 42.5%64 to 100%45,60,62 in intervention completion. Within those interventions significantly improving adherence, intervention completion rates were above 93.5% and primary outcome completion rates were above 73% for full RCTs,45,47,59 with unreported completion for one study.49 For pilot RCTs, intervention completion rates were above 81% and above 78% for primary outcome completion rates,48,54,57,62 again with one not reporting rates.50
For non-significant interventions, completion was 86% and above for intervention, primary outcome or both, for only five studies.58,60,61,63,66 Poorest completion was seen in a pilot RCT with 38.90% primary outcome completion,51 closely followed by 39.90%,56 42.50%,64 and 42.60%.4 These studies used a variety of subjective and objective measures of adherence, although the commonality was the subjective measure, this being the Morisky Medication Adherence Scale,68 the Medication Adherence Report Scale69 or both.
Discussion
Overall, just over a third (37.5%) of studies reviewed reported statistically significant difference in adherence and four of these were full RCTs, meaning there is an extremely limited evidence base. Of the three inflammatory conditions considered, IBD fared worst, with two of eight (25%) IBD interventions being effective in significantly improving adherence compared with controls. Two of the four (50%) MS studies (both pilot) and five of 12 (41.7%) RA studies reported statistically significant effects on adherence improvement.
This review has highlighted that a range of approaches have been applied to improve adherence. Results were contradictory in that both effective and ineffective interventions each used multiple approaches. However, the only consistent factor across all nine significantly effective studies was utilising at least one predominant intervention approach supported by at least one additional approach.45,47–50,54,57,59,62
Tailoring
Tailored approaches were primarily used in the successful interventions. Tailoring involved adapting information to a patient’s information-processing style and learning (such as need for cognition, affect or for autonomy). Mode of delivery was tailored or the patient was encouraged to adapt the intervention to their needs.78 Personalised tailoring, as opposed to group support,59 enabled individual needs to be the central focus, increasing likelihood of helping change behaviour.79 These adaptive encouragement strategies applied in adherence research exert more persuasive effects,80,81 facilitating self-efficacy to address barriers.53 The tailored RCTs largely had good power; sample sizes of 85 and above (with the exception of two pilots), intervention completion over 73%, significance level of 0.05 and below and overall good effect size, thus being more likely to lead to positive results.
Clinician Interaction and Training
Tailoring was found to be most effective when delivered by a trained healthcare professional, mainly nurses, applying consistent communication strategies.53,65 A high percentage of non-adherence was found to be associated with the physician–patient interaction.48 This is in line with previous findings that infrequent, poor communication between patient and clinician can potentially lead to 19% lower medication adherence.14,82,83 Patient interactions with pharmacists, for example, can be restricted and unfamiliar, impacting upon relations and subsequent adherence. All four studies/arms where pharmacists facilitated adherence support resulted in a non-significant difference,54,64–66 and in one arm was found to have a lower proportion of adherent patients compared to the control arm.54 To facilitate a skills-driven, disease-focused intervention, healthcare professionals require depth of knowledge of both psychological and physical demands of the disease and treatment.52 This is vital in assisting individuals to improve disease self-management and adherence84 and may in turn be a useful strategy for improving the patient–physician relationship.85,86 A high priority for research is training accessible healthcare practitioners in health decision–counselling methods and patient education skills.49
Patient Education
Patient education was incorporated within several successful interventions, but was most effective when integrated with technology, monitoring and psychological behaviour change via multiple sessions or long-term accessible information. Self-management and treatment decision-making in RA resulted from an educational and counselling intervention merged with a fitness programme.49 Similarly, a wide range of web-based learning methods proved to be beneficial in the 12 month IBD coach intervention.47
The challenge of an integrated approach incorporating multiple elements is difficulty in determining cause, impact, and extent. Overcoming this, one study provided their control group with intervention features of action plans and an educational curriculum, ensuring the impact of monitoring, prompting and interaction of a home telemedicine could be assessed.46 Action and coping planning have also been used successfully within previous interventions to significantly impact adherence.87
Adherence promotion through patient education as a single approach has limited effect.88 Former findings89,90 and this review45,55,56,61,63 have shown education alone has inconsistent short-term benefits in facilitating adherence, even if patients’ knowledge about disease and treatment is improved.54 If a non-adherent patient already has good knowledge of their disease and treatment, specific educational interventions may be inappropriate or may skew results on adherence impact.47 When two methods of patient education were used over 12 weeks to target medication taking in RA participants,60 this led to no significant difference. Health literacy was not tested, which could indirectly impact comprehension and utilisation of study educational materials and clinical resources. If providing participants with educational resources, their understanding of and ability to use them must be ensured to promote effectiveness.48,59,63,91 Studies thus far have found that to achieve sustainable impact, educational sessions and materials should be conveniently accessible for a substantial period, either a minimum of three one-on-one sessions, each lasting at least 20 minutes,45,48,59 or information being available for 12 weeks or more.47,48 Even if a patient chooses not to take medication for valid reasons, such as side effects or long-term effects of medications, these reasons still must be understood to allow treatment options to be explored.
Technology-Based Interventions
Technological and web-based interventions have become increasingly popular, with benefits demonstrated by five of the nine successful studies.47,48,50,55,60 This included a reduction in flare-ups, emergency visits and surgeries through systematic implementation of educational, supportive and monitoring strategies of patients and disease activity.47 Digital systems were accessible, feasible and modifiable,4 with ease of implementation.47,48 Continuity of care was established with fewer geographical restrictions, particularly in remote areas,92 reducing time travel to in-person clinics and related costs such as hospital parking.
Electronic diaries used as an adherence tool have been found to motivate patients in medication taking, maintaining a patient-centred focus.50 This may improve interactions between healthcare providers and patients.37,47,90 It also provides opportunities for personalised approaches to current models of care.4 Artificial intelligence adherence programmes can support strained health systems, minimising demands on outpatient and inpatient settings due to reduced relapses,4 whilst being safe and moderately cost-effective.93,94
This growing trend in online chronic disease programme management has demonstrated effectiveness through improved healthcare outcomes in a range of chronic conditions,95 including congestive heart failure,96 diabetes,97 chronic obstructive pulmonary disease98 and IBD.47,48,99–102Technological interventions are not always successful, however, with this being a main approach in five ineffective interventions in this review.4,37,46,54,59 Of course, patients who do not have internet access or are unable to use an appropriate electronic device may be excluded.37,46,47,102 One home telemanagement system46 required home installation, potentially impacting recruitment and attrition due to technical difficulties, questioning whether such a system would be favoured long-term. High attrition rates have also been found in intervention arms of more recent ineffective web-telemedicine studies,4 with the exception of one RCT,48 possibly due to the reminder system within the intervention and short 12 week follow-up period. Telemedicine systems may also be prone to functional errors, being based on incorrect design assumptions developed with minimal input from patients and clinicians.103 This can lead to inconsistent results for disease outcomes whilst being dependent on study type, design, patient population and healthcare system in which they are applied.98,100,101,104
A web-based system can also have a low impact on an individual’s behaviour as opposed to face-to-face sessions with a clinical professional or researcher,4 with few telemedicine systems being implemented in everyday clinical practice47 pre-COVID. However, restricted person-to-person contact during the pandemic led to substantial acceleration in development and implementation of digital healthcare.105 Systems have become more user-friendly, typically, with rising numbers of people accessing the internet.106 Intervention usability and acceptability is increasingly critical, with an intervention needing to be accessible and easy to use for all, including clinical staff and researchers.48 If participants recognise the importance of an intervention and the impact this has on their understanding and condition, it is more likely to have a positive effect on their adherence, and attrition rates. One significantly effective technology-based intervention was rated as highly successful by more than 90% of intervention participants, with no attrition for the intervention or primary outcome completion.63 The World Health Organization (WHO) acknowledges the necessity of digital healthcare, providing recommendations for its use,107 yet a framework for the development, evaluation and implementation of eHealth adherence interventions is still lacking. This would be beneficial for future technological research in adherence promotion.14
Theory
Use of appropriate theory for evidence-based adherence interventions has been suggested by the UK Medical Research Council framework for developing complex interventions108 and the UK National Institute of Health and Care Excellence.109 In support of this, one significantly effective intervention45 was theoretically underpinned by the health action process approach and mapped to behaviour change techniques.110 The PAPA theoretical framework was used to design an online intervention to change IBD adherence-related medication beliefs and concerns.4 However, adherence results were inconsistent.111
The argument that theory-based programmes demonstrate more effectiveness at promoting behaviour change compared with atheoretical approaches53 is thus questionable, with almost half of the significantly effective interventions reviewed not being theory-based.47,48,50,55,58 As only 10 (41.7%) of the RCTs reviewed reported a theoretically-based intervention (five being pilot studies and five full RCTs), this scoping review reinforces how theory has typically been overlooked in intervention development and evaluation.112 Studies rarely examine theory-related mechanisms to explain medication adherence.46 Theory-based interventions require further investigation.45,113
Limitations
There are several limitations of this review. The multiplicity of RCTs with varying designs and data across diverse clinical services, countries and continents has led to difficulties in identifying which intervention components and modes of delivery were most effective. Firstly, only three studies had inclusion criteria for low adherence at baseline,61,62,65 identified through pill counts and questionnaire completion. Screening for significantly poor adherers prior to recruitment is recommended practice to ensure sufficient capacity to benefit from the intervention. Monitoring any phenomenon such as “regression to the mean”114 and “Hawthorne effects”115 is equally important.
Identifying and subsequently monitoring adherence using self-report methods is typical, used by 75% of the studies, with measures such as the MARS being significantly associated with objectively assessed medication adherence.54 However, it is also commonly acknowledged they are more prone to memory or social desirability bias and lack objectivity.45 Such subjective measures may have led to participants under-reporting non-adherence,57 creating a ceiling effect on adherence improvements.4 Conversely, in another study, over-estimated adherence levels were reported,4 higher than previous in IBD research,116–118 which in part may be attributed to a lack of or non-specific operational definitions of medication adherence at intake. The inconsistency of studies measuring adherence based upon a single medication or across all medications, in all formats, adds further complexities. A more objective measure of adherence could therefore be beneficial; for example, urine levels of 5-ASA medication possession ratio,57 serum concentration of medication or electronic drug monitoring,45 also particularly useful for investigating disease activity in IBD and RA.
Cautious interpretation of results is required for several reasons. More than 50% of studies showing a significant effect on adherence were pilot studies, meaning typically low sample sizes. Some studies had low completion rates or unclear intervention completion and only five applied the intention-to-treat principle meaning their data may overestimate the true magnitude of effect. Per protocol analysis results in greater strength of association and increased biases. It is therefore recommended by the CONSORT guidelines for reporting of RCTs119 that both intention-to-treat and per protocol analyses should be reported, to enable readers to make their own interpretation.
Although significant adherence improvements were seen in some intervention arms, these were also evident in some control arms,48 suggesting change may not be due to the intervention. In addition, when no significant difference between groups was found, it is uncertain whether this is caused by attrition or ineffective treatment. This reinforces the criticality of the design, power and inclusion criteria of the study, monitoring adherence and fidelity to the intervention and adequate follow-up rates. Finally, comparison of variable intervention durations, intensities and many lacking a theory basis may also somewhat limit applicability and relevance of results.
Conclusion
Improved medication adherence has been found to enhance long-term inflammatory disease outcomes, promoting health, including quality of life. There have been a range of interventions aiming to boost adherence in the inflammatory conditions of IBD, MS and RA, yet the vast majority have been ineffective. Adherence support interventions in inflammatory conditions therefore need improving.
Intervention development would benefit considerably from healthcare professionals trained in adherence support. Their role in helping to promote in-depth understanding of inflammatory conditions and associated medications, whilst offering consistent and/or long-term patient-based, interactive approaches targeting a patient’s personalised needs, is essential. This has potential to simultaneously enhance the patient–clinician relationship, facilitating open, honest discussion and improved medication adherence.
The application of theory in medication intervention development has been extremely limited, and when used, demonstrates mixed evidence. Theoretically-based interventions therefore require further exploration so the impact can be more accurately assessed. Increasingly popular technology-based routes of intervention delivery must be accessible, user-friendly, practical and functional, which can be synchronised with useful self-management supportive tools offering patient feedback. Potential interventions ideally will be efficient yet cost-effective and evaluated in adequately powered RCTs, with the optimal goal to truly benefit patients, professionals, and services alike.
This article was a poster presentation at the 18th Congress of European Crohn’s and Colitis Organisation, Copenhagen, Denmark, 2023.
Abbreviations
bDMARD, biological disease modifying antirheumatic drugs; CD, Crohn’s disease; CQR-19, Compliance Questionnaire Rheumatology; DMT, disease modifying therapy; ELM, elaboration likelihood model; EMF, electronic monitoring feedback; HAT, home automated telemanagement; IBD, inflammatory bowel disease; ITT, intention-to-treat; MAQ, Medication Adherence Questionnaire; MARS, Medication Adherence Report Scale; MEMS, medication electronic monitoring system; MI, motivational interviewing; MMAS, Morisky Medication Adherence Scale; MPR, medication possession ratio; MS, multiple sclerosis; MSP, (tele) Medicine Patient Support Programme; MTX, methotrexate; MUSP, Musculoskeletal Ultrasound Programme; PAPA, perceptions and practicalities approach; PROMs, patient-reported outcome measures; PC, pharmacist counselling; RA, rheumatoid arthritis; TAU, treatment as usual; TM, text message; TMI, tailored multimedia intervention; UK, United Kingdom; USA, United States of America; VAS, visual analogue scale.
Data Sharing and Availability
The authors confirm that this manuscript, in addition to the findings, tables, and figures, have not been published previously elsewhere or are under consideration for publication. The data underlying this article are available in the article and in its online Supplementary Material.
Acknowledgments
We would like to express sincere gratitude specifically to the author Serena McGuinness for her contribution in the early stages of this scoping review, which included, amongst other tasks, the searching, screening, and data extraction of relevant articles. Thank you very much, Serena. Profound gratitude also goes out to the National Institute for Health and Care Research (NIHR) who are currently funding lead author Kathryn King’s NIHR Doctoral Fellowship programme and have made this scoping review possible.
Author Contributions
To confirm, all authors have made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; drafted, written, substantially revised, or critically reviewed the article; agreed on the journal to which the article will be submitted; reviewed and agreed on all versions of the article before submission, during revision, the final version accepted for publication, and any significant changes introduced at the proofing stage; agreed to take responsibility and be accountable for the contents of the article.
Funding
Any research work completed by the lead author (Kathryn King) was funded in part by the National Institute for Health and Care Research (NIHR), through the NIHR Doctoral Fellowship programme (NIHR302646 to KEK). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Disclosure
Professor Christine Norton reports grants from King’s College London during the conduct of the study and personal fees from Pfizer, Merck, Janssen, and WebMD outside the submitted work. The study authors report no other conflicts of personal interest.
References
1. Kuek A, Hazleman BL, Östör AJ. Immune-mediated inflammatory diseases (IMIDs) and biologic therapy: a medical revolution. Postgrad Med J. 2007;83(978):251–260. doi:10.1136/pgmj.2006.052688
2. Vangeli E, Bakhshi S, Baker A, et al. A systematic review of factors associated with non-adherence to treatment for immune-mediated inflammatory diseases. Adv Ther. 2015;32:983–1028. doi:10.1007/s12325-015-0256-7
3. Chan W, Chen A, Tiao D, Selinger C, Leong R. Medication adherence in inflammatory bowel disease. Intest Res. 2017;4:434–445. doi:10.5217/ir.2017.15.4.434
4. Chapman S, Sibelli A, St-Clair Jones A, Forbes A, Chater A, Horne R. Personalised adherence support for maintenance treatment of inflammatory bowel disease: a tailored digital intervention to change adherence-related beliefs and barriers. J Crohns Colitis. 2020;14:1–11. doi:10.1093/ecco-jcc/jjz034
5. van den Bemt BJ, Zwikker HE, van den Ende CH. Medication adherence in patients with rheumatoid arthritis: a critical appraisal of the existing literature. Expert Rev Clin Immunol. 2012;8(4):337–351. doi:10.1586/eci.12.23
6. Giedraitiene N, Taluntiene V, Kaubrys G. Relationship between cognition and treatment adherence to disease-modifying therapy in multiple sclerosis: a prospective, cross-sectional study. Sci Rep. 2022;12:12447. doi:10.1038/s41598-022-16790-3
7. Washington F, Langdon D. Factors affecting adherence to disease-modifying therapies in multiple sclerosis: systematic review. J Neurol. 2022;269:1861–1872. doi:10.1007/s00415-021-10850-w
8. Beardon PH, McGilchrist MM, McKendrick AD, McDevitt DG, MacDonald TM. Primary non‐compliance with prescribed medication in primary care. BMJ. 1993;307:846–848. doi:10.1136/bmj.307.6908.846
9. Pellegrino R, Pellino G, Selvaggi F, Federico A, Romano M, Gravina AG. Therapeutic adherence recorded in the outpatient follow-up of inflammatory bowel diseases in a referral center: damages of COVID-19. Dig Liver Dis. 2022;54(10):1449–1451. PMID: 35973931; PMCID: PMC9375145. doi:10.1016/j.dld.2022.07.016
10. Lenti ML, Selinger CP. Medication non-adherence in adult patients affected by inflammatory bowel disease: a critical review and update of the determining factors, consequences and possible interventions. Expert Rev Gastroenterol Hepatol. 2017;11(3):215–226. doi:10.1080/17474124.1284587
11. Gracie DJ, Irvine AJ, Sood R, Mikocka-Walus A, Hamlin PJ, Ford AC. Effect of psychological therapy on disease activity, psychological comorbidity, and quality of life in inflammatory bowel disease: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2017;2(3):189–199. doi:10.1016/S2468-1253(16)30206-0
12. Horne R, Parham R, Driscoll R, Robinson A. Patients’ attitudes to medicines and adherence to maintenance treatment in inflammatory bowel disease. Inflamm Bowel Dis. 2009;15(6):837–844. doi:10.1002/ibd.20846
13. Chang S, Stebbins M, Witt EA, Kirkham H, Santos T, Cocohoba J. Medication-related problems in chronic inflammatory conditions: a pharmacy claims and electronic health record analysis. J Am Coll ClinPharm. 2021;4:570–579. doi:10.1002/jac5.1417
14. Jackson CA, Clatworthy J, Robinson A, Horne R. Factors associated with non-adherence to oral medication for inflammatory bowel disease: a systematic review. Am J Gastroenterol. 2010;105:525–539. doi:10.1038/ajg.2009.685
15. Selinger CP, Robinson A, Leong RW. Clinical impact and drivers of nonadherence to maintenance medication for inflammatory bowel disease. Expert Opin Drug Saf. 2011;10:863–870. doi:10.1517/14740338.2011.583915
16. Cárdenas-Cloud E, Brambila-Tapia AJL, Meda-Lara RM, et al. Evaluation of a psychoeducational intervention including emotional intelligence to increase treatment adherence in rheumatoid arthritis (A pilot study). Reumatismo. 2021;73(3). PMID: 34814658. doi:10.4081/reumatismo.2021.1400
17. Horne R. Compliance, adherence and concordance. In: Taylor K, Harding G, editors. Pharmacy Practice. London: Taylor and Francis; 2001.
18. Webb TL, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res. 2010;12(1):e4. doi:10.2196/jmir.1376
19. Weinman J, Graham S, Canfield M, et al. The Intentional Non-Adherence Scale (INAS): initial development and validation. J Psychosom Res. 2018;115:110–116. doi:10.1016/j.jpsychores.2018.10.010
20. Gast A, Mathes T. Medication adherence influencing factors—an (updated) overview of systematic reviews. Syst Rev. 2019;8(112). doi:10.1186/s13643-019-1014
21. Moulton CD, Norton C, Powell N, Mohamedali Z, Hopkins CWP. Depression in inflammatory bowel disease: risk factor, prodrome or extraintestinal manifestation? Gut. 2020;69(3):609–610. PMID: 30808645. doi:10.1136/gutjnl-2019-318444
22. Drescher H, Lissoos T, Hajisafari S, Evans ER. Treat to target approach in inflammatory bowel disease: the role of advanced practice providers. J Nurse Pract. 2019;15(9):676–681. doi:10.1016/j.nurpra.2019.07.015
23. Timmer A, Preiss JC, Motschall E, Rücker G, Jantschek G, Moser G. Psychological interventions for treatment of inflammatory bowel disease. Cochrane Database Syst Rev. 2011;16(2):CD006913. PMID: 21328288. doi:10.1002/14651858.CD006913.pub2
24. Norton C, Czuber-Dochan W, Artom M, Sweeney L, Hart A. Systematic review: interventions for abdominal pain management in inflammatory bowel disease. Aliment Pharmacol Ther. 2017;46(2):115–125. doi:10.1111/apt
25. McCombie AM, Mulder RT, Gearry RB. Psychotherapy for inflammatory bowel disease: a review and update. J Crohns Colitis. 2013;7(12):935–949. doi:10.1016/j.crohns.2013.02.004
26. Ballou S, Keefer L. Psychological Interventions for Irritable Bowel Syndrome and Inflammatory Bowel Diseases. Clin Transl Gastroenterol. 2017;8(1):e214–e214. doi:10.1038/ctg.2016.69
27. Safren SA, O’Cleirigh C, Andersen LS, et al. Treating depression and improving adherence in HIV care with task-shared cognitive behavioural therapy in Khayelitsha, South Africa: a randomized controlled trial. J Int AIDS Soc. 2021;24(10):e25823. PMID: 34708929; PMCID: PMC8552453. doi:10.1002/jia2.25823
28. Gravina AG, Pellegrino R, Palladino G, et al. Targeting the gut-brain axis for therapeutic adherence in patients with inflammatory bowel disease: a review on the role of psychotherapy, Brain-Apparatus Communication. J Bacomics. 2023;2(1):2181101. doi:10.1080/27706710.2023.2181101
29. Keefer L, Kiebles JL, Kwiatek MA, et al. The potential role of a self-management intervention for ulcerative colitis: a brief report from the ulcerative colitis hypnotherapy trial. Biol Res Nurs. 2012;14(1):71–77. PMID: 21362636; PMCID: PMC3574577. doi:10.1177/1099800410397629
30. Chaiyachati KH, Ogbuoji O, Price M, Suthar AB, Negussie EK, Bärnighausen T. Interventions to improve adherence to antiretroviral therapy: a rapid systematic review. Aids. 2014;28 Suppl 2:S187–S204. doi:10.1097/QAD.0000000000000252
31. Michie S, West R, Sheals K, Godinho CA. Evaluating the effectiveness of behavior change techniques in health-related behavior: a scoping review of methods used. Transl Behav Med. 2018;8(2):212–224. doi:10.1093/tbm/ibx019
32. Hobden A. Strategies to promote concordance within consultations. Br J Community Nurs. 2006;11(7):286–289. PMID: 16926708. doi:10.12968/bjcn.2006.11.7.21443
33. Wilburn J, McKenna SP, Twiss J, Kemp K, Campbell S. Assessing quality of life in Crohn’s disease: development and validation of the Crohn’s Life Impact Questionnaire (CLIQ). Qual Life Res. 2015;24:2279–2288. doi:10.1007/s11136-015-0947-1
34. IBD Strategy Partnership & Quality Improvement. Working together for everyone affected by inflammatory bowel disease. Available from: https://www.ibduk.org/ibd-standards/ongoing-caremonitoring/shared-care.
35. IBD Strategy Partnership & Quality Improvement. IBD standards core statements. Available from: https://s3.eu-west-2.amazonaws.com/files.ibduk.org/documents/IBD-Standards-Core-Statements.pdf?mtime=20190708142622&fo.
36. Landtblom AM, Guala D, Martin C, et al. RebiQoL: a randomized trial of telemedicine patient support program for health-related quality of life and adherence in people with MS treated with Rebif. PLoS One. 2019;14(7):e0218453. PMID: 31276502; PMCID: PMC6611587. doi:10.1371/journal.pone.0218453
37. Elkjaer M, Shuhaibar M, Burisch J, et al. E-health empowers patients with ulcerative colitis: a randomised controlled trial of the web-guided ‘Constant-care’ approach. Gut. 2010;59:1652–1661. doi:10.1136/gut.2010.220160
38. Horne R, Glendinning E, King K, et al. Protocol of a 2-arm randomised, multi-centre, 12month controlled trial: evaluating Cognitive Behavioural Therapy (CBT)-based intervention Supporting Uptake and Adherence to antiretrovirals (SUPA) in adults with HIV. BMC Public Health. 2019;19(905):1–15. doi:10.1186/s12889-019-6893-z
39. King K, Horne R, Cooper V, Glendinning E, Michie S, Chalder T. The development of an intervention to support uptake and adherence to antiretroviral therapy in people living with HIV: the SUPA intervention. A brief report. Transl Behav Med. 2022;12(1):ibab104. PMID: 34379122. doi:10.1093/tbm/ibab104
40. Hawthorne AB, Rubin G, Ghosh S. Review article: medication non‐adherence in ulcerative colitis – strategies to improve adherence with mesalazine and other maintenance therapies. Aliment Pharmacol Ther. 2008;27:1157–1166. doi:10.1111/j.1365-2036.2008.03698.x
41. Moore GF, Audrey S, Barker M, et al. Process evaluation of complex interventions: medical research council guidance. BMJ. 2015;350:h1258. doi:10.1136/bmj.h1258
42. Benson-Pope SJ, Gearry RB. Editorial: increasing IBD prevalence and its complications in the context of the COVID-19 pandemic. Aliment Pharmacol Ther. 2020;51(12):1441–1442. doi:10.1111/apt.15759
43. Moher D, Shamseer L, Clarke M, et al.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. PMID: 25554246; PMCID: PMC4320440. doi:10.1186/2046-4053-4-1
44. Critical Appraisal Skills Programme. CASP (systematic review) checklist; 2022.Available from: https://casp-uk.net/images/checklist/documents/CASP-Systematic-Review-Checklist/CASP-Systematic-Review-Checklist-2018_fillable-form.pdf.
45. Asgari S, Abbasi M, Hamilton K, et al. A theory-based intervention to promote medication adherence in patients with rheumatoid arthritis: a randomized controlled trial. Clin Rheumatol. 2021;40(1):101–111. PMID: 32588274; PMCID: PMC7782392. doi:10.1007/s10067-020-05224-y
46. Cross RK, Cheevers N, Rustgi A, Langenberg P, Finkelstein J. Randomized, controlled trial of home telemanagement in patients with ulcerative colitis (UC HAT). Inflamm Bowel Dis. 2012;18(6):1018–1025. doi:10.1002/ibd.21795
47. de Jong MJ, van der Meulen-de Jong AE, Romberg-Camps MJ, et al. Telemedicine for management of inflammatory bowel disease (myIBDcoach): a pragmatic, multicentre, randomised controlled trial. Lancet. 2017;390(10098):959–968. PMID: 28716313. doi:10.1016/S0140-6736(17)31327-2
48. Del Hoyo J, Nos P, Faubel R, et al. A web-based telemanagement system for improving disease activity and quality of life in patients with complex inflammatory bowel disease: pilot randomized controlled trial. J Med Internet Res. 2018;20(11):e11602. PMID: 30482739; PMCID: PMC6301812. doi:10.2196/11602
49. El Miedany Y, El Gaafary M, El Arousy N, Ahmed I, Youssef S, Palmer D. Arthritis education: the integration of patient-reported outcome measures and patient self-management. Clin Exp Rheumatol. 2012;30(6):899–904.
50. El Miedany Y, El Gaafary M, Palmer D. Assessment of the utility of visual feedback in the treatment of early rheumatoid arthritis patients: a pilot study. Rheumatol Int. 2012;32(10):3061–3068. doi:10.1007/s00296-011-2098-1
51. Ferguson A, Ibrahim FA, Thomas V, et al. Improving medication adherence in rheumatoid arthritis (RA): a pilot study. Psychol Health Med. 2015;20:781–789. doi:10.1080/13548506.2015.1009917
52. Hebing RC, Aksu I, Twisk JW, Bos W, Van den Bemt B, Nurmohamed MT. Effectiveness of electronic drug monitoring feedback to increase adherence in patients with RA initiating a biological DMARD: a randomised clinical trial. RMD Open. 2022;8(1):e001712. PMID: 35121638; PMCID: PMC8819786. doi:10.1136/rmdopen-2021-001712
53. Keefer L, Doerfler B, Artz C. Optimizing management of Crohn’s disease within a project management framework: results of a pilot study. Inflamm Bowel Dis. 2012;18(2):254–260. PMID: 21351218; PMCID: PMC3111841. doi:10.1002/ibd.21679
54. Linn AJ, van Dijk L, van Weert JCM, Gebeyehu BG, van Bodegraven AA, Smit EG. Creating a synergy effect: a cluster randomized controlled trial testing the effect of a tailored multimedia intervention on patient outcomes. Patient Educ Couns. 2018;101(8):1419–1426. PMID: 29609899. doi:10.1016/j.pec.2018.03.017
55. Mary A, Boursier A, Desailly Henry I, et al. Mobile phone text messages and effect on treatment adherence in patients taking methotrexate for rheumatoid arthritis: a randomized pilot study. Arthritis Care Res. 2019;71(10):1344–1352. PMID: 30192070. doi:10.1002/acr.23750
56. Matteson-Kome ML, Winn J, Bechtold ML, Bragg JD, Russell CL. Improving maintenance medication adherence in adult inflammatory bowel disease patients: a pilot study. Health Psychol Res. 2014;2(1):1389. PMID: 26973930; PMCID: PMC4768558. doi:10.4081/hpr.2014.1389
57. Nikolaus S, Schreiber S, Siegmund B, et al. Patient education in a 14-month randomised trial fails to improve adherence in ulcerative colitis: influence of demographic and clinical parameters on non-adherence. J Crohns Colitis. 2017;11(9):1052–1062. PMID: 28486634. doi:10.1093/ecco-jcc/jjx062
58. Rice DR, Kaplan TB, Hotan GC, et al. Electronic pill bottles to monitor and promote medication adherence for people with multiple sclerosis: a randomized, virtual clinical trial. J Neurol Sci. 2021;428:117612. PMID: 34392138. doi:10.1016/j.jns.2021.117612
59. Settle JR, Maloni HW, Bedra M, Finkelstein J, Zhan M, Wallin MT. Monitoring medication adherence in multiple sclerosis using a novel web-based tool: a pilot study. J Telemed Telecare. 2016;22(4):225–233. PMID: 26253748. doi:10.1177/1357633X15597115
60. Song Y, Reifsnider E, Zhao S, Xie X, Chen HA. A randomized controlled trial of the Effects of a telehealth educational intervention on medication adherence and disease activity in rheumatoid arthritis patients. J Adv Nurs. 2020;76:1172–1181. doi:10.1111/jan.14319
61. Taibanguay N, Chaiamnuay S, Asavatanabodee P, Narongroeknawin P. Effect of patient education on medication adherence of patients with rheumatoid arthritis: a randomized controlled trial. Patient Prefer Adherence. 2019;13:119–129. PMID: 30666095; PMCID: PMC6333161. doi:10.2147/PPA.S192008
62. Tan YK, Teo P, Saffari SE, et al. A musculoskeletal ultrasound program as an intervention to improve disease modifying anti-rheumatic drugs adherence in rheumatoid arthritis: a randomized controlled trial. Scand J Rheumatol. 2022;51(1):1–9. PMID: 34107851. doi:10.1080/03009742.2021.1901416
63. Turner AP, Sloan AP, Kivlahan DR, Haselkorn JK. Telephone counseling and home telehealth monitoring to improve medication adherence: results of a pilot trial among individuals with multiple sclerosis. Rehabil Psychol. 2014;59(2):136–146. PMID: 24708232. doi:10.1037/a0036322
64. Unk JA, Brasington R. Efficacy study of multimedia rheumatoid arthritis patient education program. J Am Assoc Nurse Pract. 2014;26(7):370–377. PMID: 24170559. doi:10.1002/2327-6924.12064
65. van Heuckelum M, van den Ende CHM, van Dulmen S, van den Bemt BJF. Electronic monitoring feedback for improving medication adherence and clinical outcomes in early rheumatoid arthritis: a randomized clinical trial. Patient Prefer Adherence. 2021;15:1107–1119. PMID: 34079231; PMCID: PMC8164714. doi:10.2147/PPA.S297170
66. Zwikker HE, van den Ende CH, van Lankveld WG, et al. Effectiveness of a group-based intervention to change medication beliefs and improve medication adherence in patients with rheumatoid arthritis: a randomized controlled trial. Patient Educ Couns. 2014;94:356–361. doi:10.1016/j.pec.2013.12.002
67 Bartholomew LK, Parcel GS, Kok G. Intervention Mapping: A Process for Developing Theory and Evidence-Based Health Education Programs. Health Educ Behav. 1998;25(5):545–563. doi:10.1177/109019819802500502
68. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi:10.1097/00005650-198601000-00007
69. Horne R, Hankins M. The Medication Adherence Report Scale (Mars). Quality and Safety in Health Care; 2008. Available from: http://www.pharmacy.ac.uk/1076.html.
70. Profit D, Rohatagi S, Zhao C, Hatch A, Docherty JP, Peters-Strickland TS. Developing a digital medicine system in psychiatry: ingestion detection rate and latency period. J Clin Psychiatry. 2016;77(9):1095–1100. doi:10.4088/JCP.16m10643
71. De Bleser L, De Geest S, Vandenbroeck S, Vanhaecke J, Dobbels F. How accurate are electronic monitoring devices? A laboratory study testing two devices to measure medication adherence. Sensors. 2010;10(3):1652–1660. doi:10.3390/s100301652
72. Nerini E, Bruno F, Citterio F, Schena FP. Nonadherence to immunosuppressive therapy in kidney transplant recipients: can technology help? J Nephrol. 2016;29(5):627–636. doi:10.1007/s40620-016-0273-x.10.1007/s40620-016-0273-x
73. Arnet I, Walter PN, Hersberger KE. Polymedication Electronic Monitoring System (POEMS) - a new technology for measuring adherence. Front Pharmacol. 2013;4:26. doi:10.3389/fphar.2013.00026
74. Miguel-Cruz A, Bohórquez AF, Parra PA. What does the literature say about using electronic pillboxes for older adults? A systematic literature review. Disabil Rehabil Assist Technol. 2019;14(8):776–787. doi:10.1080/17483107.2018.1508514
75. Williams A, Low JK, Manias E, Dooley M, Crawford K. Trials and tribulations with electronic medication adherence monitoring in kidney transplantation. Res Social Adm Pharm. 2016;12(5):794–800. doi:10.1016/j.sapharm.2015.10.010.S1551-7411(15)00239-9
76. Levin JB, Sams J, Tatsuoka C, Cassidy KA, Sajatovic M. Use of automated medication adherence monitoring in bipolar disorder research: pitfalls, pragmatics, and possibilities. Ther Adv Psychopharmacol. 2015;5(2):76–87. doi:10.1177/2045125314566807
77. de Klerk E, van der Heijde D, van der Tempel H, van der Linden S. Development of a questionnaire to investigate patient compliance with antirheumatic drug therapy. J Rheumatol. 1999;26(12):2635–2641.
78. Smit ES, Linn AJ, van Weer JCM. Taking online computer-tailoring forward. The potential of tailoring the communication style and delivery mode of online health communication. Eur Health Psychol. 2015;17(1):1.
79. Connelly K, Segan J, Lu A, et al. Patients’ perceived health information needs in inflammatory arthritis: a systematic review. Semin Arthritis Rheum. 2019;48(5):900–910. doi:10.1016/j.semarthrit.2018.07.014
80. Petty RE, Wheeler SC, Bizer GY. Attitude functions and persuasion: an elaboration likelihood approach to matched versus mismatched messages. In: Maio GR, Olson JM, editors. Why We Evaluate: Functions of Attitudes. Lawrence Erlbaum Associates Publishers; 2000:133–162.
81. Greuter T, Manser C, Pittet V, et al. Gender differences in inflammatory bowel disease. Digestion. 2020;1(Suppl 1):98–104. doi:10.1159/000504701
82. Zolnierek KBH, DiMatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47:826–834. doi:10.1097/MLR.0b013e31819a5acc
83. Tahri N. [Treatment adherence and chronic inflammatory bowel diseases]. Presse Med. 2007;36(9 Pt 2):1236–1243. French. doi:10.1016/j.lpm.2007.01.010
84. Dures E, Almeida C, Caesley J, et al. Patient preferences for psychological support in inflammatory arthritis: a multicentre survey. Ann Rheum Dis. 2016;75(1):142–147. doi:10.1136/annrheumdis-2014-205636
85. Robinson A. Review article: improving adherence to medication in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2008;27(Suppl 1):9–14. doi:10.1111/j.1365-2036.2008.03604.x
86. Lai C, Sceats LA, Qiu W, et al. Patient decision-making in severe inflammatory bowel disease: the need for improved communication of treatment options and preferences. Colorectal Dis. 2019;21(12):1406–1414. doi:10.1111/codi.14759
87. Schwarzer R, Hamilton K. Changing behaviour using the health action process approach. In: Hagger MS, Cameron L, Hamilton K, Hankonen N, Lintunen T, editors. Handbook of Behavior Change. New York: Cambridge University Press; 2020:89–103.
88. Zhang CQ, Zhang R, Schwarzer R, Hagger MS. A meta-analysis of the health action process approach. Health Psychol. 2019;38(7):623–637. doi:10.1037/hea0000728
89. Schwarzer R. Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors? Appl Psychol;. 2008;57:1–29.
90. Joplin S, van der Zwan R, Joshua F, Wong PK. Medication adherence in patients with rheumatoid arthritis: the effect of patient education, health literacy, and musculoskeletal ultrasound. Biomed Res Int. 2015;2015:150658. doi:10.1155/2015/150658
91. Miles S, Davis T. Patients who can’t read. Implications for the health care system. JAMA. 1995;274(21):1719–1720. doi:10.1001/jama.1995.03530210073035
92. Casellas-Jorda F, Borruel-Sainz N, Torrejon-Herrera A, Castells I. Effect upon hospital activity of the application of a continued care model centered on patients with inflammatory bowel disease. Rev Esp Enferm Dig. 2012;104(1):16–20. doi:10.4321/S1130-01082012000100004
93. Berwick DM, Nolan TW, Whittington J. The triple AIM: care, health, and cost. Health Aff. 2008;27:759–769. doi:10.1377/hlthaff.27.3.759
94. Siegel CA, Allen JI, Melmed GY. Translating improved quality of care into an improved quality of life for patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2013;11:908–912. doi:10.1016/j.cgh.2013.05.027
95. Lorig K, Chastain RL, Ung E, Shoor S, Holman HR. Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis Rheum. 1989;32:37–44. doi:10.1002/anr.1780320107
96. Clarke M, Shah A, Sharma U. Systematic review of studies on telemonitoring of patients with congestive heart failure: a meta-analysis. J Telemed Telecare. 2011;17(1):7–14. doi:10.1258/jtt.2010.100113
97. Weinstock RS, Teresi JA, Goland R, et al. IDEATel Consortium. Glycemic control and health disparities in older ethnically diverse underserved adults with diabetes: five-year results from the Informatics for Diabetes Education and Telemedicine (IDEATel) study. Diabetes Care. 2011;34(2):274–279. doi:10.2337/dc10-1346
98. Bartoli L, Zanaboni P, Masella C, Ursini N. Systematic review of telemedicine services for patients affected by chronic obstructive pulmonary disease (COPD). Telemed J E Health. 2009;15(9):877–883. doi:10.1089/tmj.2009.0044
99. Krier M, Kaltenbach T, McQuaid K, Soetikno R. Potential use of telemedicine to provide outpatient care for inflammatory bowel disease. Am J Gastroenterol. 2011;106(12):2063–2067. doi:10.1038/ajg.2011.329
100. Carlsen K, Jakobsen C, Houen G, et al. Self-managed eHealth disease monitoring in children and adolescents with inflammatory bowel disease: a randomized controlled trial. Inflamm Bowel Dis. 2017;23(3):357–365. doi:10.1097/MIB.0000000000001026
101. Carlsen K, Houen G, Jakobsen C, et al. Individualized infliximab treatment guided by patient-managed eHealth in children and adolescents with inflammatory bowel disease. Inflamm Bowel Dis. 2017;23(9):1473–1482. doi:10.1097/MIB.0000000000001170
102. Heida A, Dijkstra A, Muller KA, et al. Efficacy of home telemonitoring versus conventional follow-up: a randomized controlled trial among teenagers with inflammatory bowel disease. J Crohns Colitis. 2018;12(4):432–441. doi:10.1093/ecco-jcc/jjx169
103. Rudin RS, Bates DW, MacRae C. Accelerating innovation in health IT. N Engl J Med. 2016;375:815–817. doi:10.1056/NEJMp1606884
104. Pedersen N, Thielsen P, Martinsen L, et al. eHealth: individualization of mesalazine treatment through a self-managed web-based solution in mild-to-moderate ulcerative colitis. Inflamm Bowel Dis. 2014;20(12):2276–2285. doi:10.1097/MIB.0000000000000199
105. Ronquillo Y, Meyers A, Korvek S. Digital health. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022.
106. Lee K, Kim S, Kim S, et al. Digital health interventions for adult patients with cancer evaluated in randomized controlled trials: scoping review. J Med Internet Res. 2023;25:e38333. doi:10.2196/38333
107. World Health Organization. WHO Guideline: Recommendations on Digital Interventions for Health System Strengthening. Geneva: World Health Organization; 2019.
108. Skivington K, Matthews L, A S, et al. A new framework for developing and evaluating complex interventions: update of medical research council guidance. BMJ. 2021;374:n2061. doi:10.1136/bmj.n2061
109. National Institute for Health and Clinical Excellence. Medicines adherence: involving patients in decisions about prescribed medicines and supporting adherence. NICE Guidance; 2009. https://www.nice.org.uk/guidance/cg76.
110. Kok G, Gottlieb NH, Peters G-JY, et al. A taxonomy of behavior change methods: an intervention mapping approach. Health Psychol Rev. 2016;10:297–312. doi:10.1080/17437199.2015.1077155
111. Nieuwlaat R, Wilczynski N, Navarro T, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2014;2014(11):1.
112. Randolph W, Viswanath K. Lessons learned from public health mass media campaigns: marketing health in a crowded media world. Annu Rev Public Health. 2004;25:419–437. doi:10.1146/annurev.publhealth.25.101802.123046
113. Patton DE, Hughes CM, Cadogan CA, Ryan CA. Theory based interventions to improve medication adherence in older adults prescribed polypharmacy: a systematic review. Drugs Aging. 2017;34(2):97–113. doi:10.1007/s40266-016-0426-6
114. Twisk JWR, De Vente W. The analysis of randomised controlled trial data with more than one follow-up measurement. A comparison between different approaches. Eur J Epidemiol. 2008;23:655–660. doi:10.1007/s10654-008-9279-6
115. McNicholas N, Patel A, Chataway J. It is better to be in a clinical trial than not: lessons learnt from clinical neurology – the management of acute multiple sclerosis relapses. QJM. 2012;105:775–780. doi:10.1093/qjmed/hcs070
116. Khan N, Abbas AM, Koleva YN, Bazzano LA. Long-term mesalamine maintenance in ulcerative colitis: which is more important? Adherence or daily dose. Inflamm Bowel Dis. 2013;19:1123–1129. doi:10.1097/MIB.0b013e318280b1b8
117. Robinson A, Thompson DG, Wilkin D, Roberts C, Northwest GRG. Guided self-management and patient-directed follow-up of ulcerative colitis: a randomised trial. Lancet. 2001;358(9286):976–981. doi:10.1016/S0140-6736(01)06105-0
118. Robinson A, Hankins M, Wiseman G, Jones M. Maintaining stable symptom control in inflammatory bowel disease: a retrospective analysis of adherence, medication switches and the risk of relapse. Aliment Pharmacol Ther. 2013;38:531–538. doi:10.1111/apt.12396
119. Schulz KF, Altman DG, Moher D; CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. PLoS Med. 2010;7:e1000251. doi:10.1371/journal.pmed.1000251
 © 2023 The Author(s). This work is published by Dove Medical Press Limited, and licensed under a Creative Commons Attribution License.
The full terms of the License are available at http://creativecommons.org/licenses/by/4.0/.
The license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
© 2023 The Author(s). This work is published by Dove Medical Press Limited, and licensed under a Creative Commons Attribution License.
The full terms of the License are available at http://creativecommons.org/licenses/by/4.0/.
The license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
