Back to Journals » Clinical Ophthalmology » Volume 17
Vitrectomy Results for Stages 4 and 5 Retinopathy of Prematurity in Iraq
Authors Bahrani HM, Alhasseny KF
Received 11 November 2023
Accepted for publication 18 December 2023
Published 29 December 2023 Volume 2023:17 Pages 4033—4041
DOI https://doi.org/10.2147/OPTH.S443810
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Hasan M Bahrani,1 Khitam Fakhir Alhasseny2
1American Eye & Retina Center, Erbil, Iraq; 2Pediatric Ophthalmology Department, Ibn Al-Haytham Teaching Eye Hospital, Baghdad, Iraq
Correspondence: Khitam Fakhir Alhasseny, Email [email protected]
Background: Stage 4 and 5 retinopathy of prematurity (ROP) is a serious condition that may require surgical intervention at some point. Timely intervention is a key element and, with the peculiarity of eyes among this group that necessities a certain level of surgical standards, operations cannot be undertaken in any surgical eye center.
Aim of the Study: To recognize the outcomes of vitrectomy in Iraqi preterm babies with stage 4 and 5 ROP, and to study factors that might increase the risk of re-detachment in operated eyes.
Methods: A prospective cohort study undertaken from November 2020 to June 2023 for Iraqi preterm babies presenting with stage 4 and 5 ROP requiring surgical intervention. Each patient had a follow-up duration of 9 months. The primary follow-up outcome was anatomical success rate (flat versus detached), and the secondary outcome was to identify the postoperative complications.
Results: This study enrolled 19 children; 11 males and eight females (number of eyes operated on was was 31), with a mean gestational age of 29.4± 2.1 weeks. There were six (19.4%) eyes that did not develop any complications, five (16.1%) eyes developed postoperative vitreous hemorrhage, five (16.1%) eyes developed cataract, three (9.7%) eyes underwent a second vitrectomy, and seven (22.6%) eyes developed secondary glaucoma. The surgical success rates were 90.9% for stage 4a, 57.1% for stage 4b, and 33.3% for stage 5a.
Conclusion: This study presented the first surgical experience for vitrectomy in children with retinopathy of prematurity in our country, and the results were encouraging with an overall surgical success rate of 64.5%, and 19.4% of eyes did not develop any complication until the 1-year of follow-up.
Keywords: retinopathy of prematurity, vitrectomy, scleral buckle, premature infants, lens sparing vitrectomy
Introduction
Retinopathy of prematurity (ROP) is a condition where the blood vessels in the retina of premature babies grow abnormally because the retina is not fully developed.1 It is important to detect ROP early, as it can cause serious vision problems with devastating social and economic implications on both the children and their families in the worst cases, such as Stage 5 ROP.2 In developing countries, ROP is a significant reason for blindness in children and, as more premature babies survive, along with a lack of screening guidelines or an effective healthcare program to regulate oxygen, this causes a new “third epidemic” in Latin America and Asia.3
Vitrectomy is indicated for advanced ROP cases that develop complete TRD despite peripheral retinal photocoagulation. It is typically observed in Zone 1 or Zone 2 posterior ROP with an open anterior and posterior RD pattern.4 As the lens is clear, lens-sparing vitrectomy (LSV) through the pars plicata is performed through the clear lens, since the pars plana is not formed until 8–9 months postnatal.2 LSV requires creating three openings through the pars plicata no further than 1.5 mm from the limbal margin.5 Preterm infants have much smaller ocular dimensions; thus, caution is needed to orient the MVR blade toward the central vitreous space to prevent lens contact.2 Moreover, to prevent the highly elevated retina in these eyes, caution is required to avoid inserting the MVR fully and causing a retinal contact or tear.6 With the development of a micro-incision vitrectomy system (MIVS), more surgeons opt to perform ROP surgeries also with MIVS due to the benefits of less surgical damage, improved patient comfort, and faster postoperative recovery.7 Gonzales et al described success in using of 25G system in eyes with stage 4 and 5 and, with the introduction of 23 and 25-gauge systems, LSV is becoming more common, the small instruments enable surgeons to easily reach to anterior membranes in peripheral detachment in these smaller eyes.8
Aim of the Study
To recognize the outcomes of vitrectomy in Iraqi preterm babies with stage 4 and 5 ROP, and to study factors that might increase the risk of re-detachment in operated eyes.
Patients and Methods
Study Design and Setting
A prospective cohort study undertaken from November 2020 to June 2023 for Iraqi preterm babies presenting with stage 4 and 5 ROP requiring surgical intervention. The cases were examined at Ibn Al-Haitham Teaching Eye Hospital, Baghdad, Iraq and the surgery was done at The American Eye Center, Erbil, Iraq. The follow-up duration was 1-year.
Participants: Patients with stage 4 or 5 ROP and visual acuity better than no light perception.
Variables: The primary follow-up outcome was anatomical success rate (flat versus detached), and the secondary outcome was to identify the postoperative complications. The general variables included gestational age, sex, birth weight, and neonatal intensive care unit admission durations, and the ophthalmic variables included laterality, visual acuity, ROP stage, intravitreal anti-VEGF injection (timing and type), type of vitrectomy, and intravitreal tamponade type, and any postoperative complication was recorded during the follow-up duration.
Data Measurements
The visual acuity was examined by menace reflex, reaction to light, fix and follow hand motion, and Catford drum when applicable. Preoperative and postoperative examination under general anesthesia including intraocular pressure (IOP) was measured using Perkins tonometer, anterior segment examination was done under a surgical microscope, retinal examination via indirect ophthalmoscopy using a 28-diopter lens with indentation, and RetCam images were obtained for identifying ROP-stage.
Surgical Details
All patients were prepped and draped in sterile ophthalmic surgery fashion. The drape was cut down using an iris scissor. A sterile ROP baby speculum was used and at times double different ROP baby speculums were used to expose the conjunctiva and sclerotomies areas. The seating position of the surgeon was determined based on the area of traction. At times, a nasal seating position was chosen in order to avoid temporal peripheral TRD. For all cases, 25 gauge plus beveled (Constellation Alcon System, Fort Worth, Texas, USA) was used. In general, three port transconjunctival sclerotomies were marked at 1.5–2.0 mm from the limbus at 5 or 8, 10, and 2 o’clock depending on the eye laterality. The infusion cannula is inspected and inserted and clamped. After identifying the infusion cannula within the vitreous cavity using the light pipe or the microscope light, the infusion cannula was unclamped. The vitrector and light pipe were introduced through the cannulas and vitrectomy commenced. Triamcinolone (Kenacort Bristol-Myers Squip) was used to delineate the vitreous hyaloid. Attempts were made to elevate the hyaloid and induce posterior vitreous detachment, but they were aborted if severe adherence to the posterior pole was discovered. Careful attempts were made to sever all anterior–posterior traction and peripheral traction without causing any iatrogenic break or tear. The ridge of the tractional detachment membrane was shaved and dissected carefully. In cases of posterior TRDs, ILM forceps were used to peel the tight adherent fibrovascular membranes from the optic disc allowing the posterior funnel to open and visualization of the disc. Cautery was applied to bleeding neovascularization and sometimes a laser was used instead of cauter, a 360° endo-laser was used in all areas of ischemia with careful attention to avoid the crystalline lens. Most cases did not require any tamponade; however, in cases of suspicious break or tear or in cases of high-risk, gas or silicon oil was used. In cases where silicon oil was used, the silicon oil was removed within 3 months. The conjunctiva and sclerotomies were closed using 7–0 Vicryl suture in all cases to avoid leakage and hypotony causing post-op vitreous hemorrhage.
Statistical Analysis
Data input and manipulation was done using the statistical package for social sciences (SPSS) version 26. Descriptive statistics included frequency, percentage, mean, median, and standard deviation. Chi-square and Fisher’s exact test were utilized to study the association between re-detachment and study variables.
Results
This study enrolled 19 children; 11 males and eight females (number of eyes operated on was 31), with a mean gestational age of 29.4±2.1 weeks, and the median duration of NICU admission was 4 weeks. The mean birth weight was 1046.9±216.6 g. There were 11 (35.5%) eyes with ICROP stage 4a, 14 (45.2%) stage 4b, and six (19.4%) stage 5a, as shown in Table 1.
 |
Table 1 Characteristics of Study Sample (Number of Patients=19) |
The mean gestational age at the time of IVA injection was 38.0±2.2 weeks. Four eyes did not receive IVA, 11 (35.5%) received ranibizumab, and 17 (54.8%) received Aflibercept. The mean gestational age at time of surgery was 39.6±2.3 weeks (duration from birth until surgery was 10.2±2.0 weeks). Three (40.6%) eyes had lensectomy and vitrectomy (LV), 28 (90.3%) had lens sparing vitrectomy, and in one patient we added a scleral buckle after PPV (Figure 1). Silicon was needed in four (12.9%) eyes, while gas was used as an intraocular tamponade in five (16.1%) eyes (as shown in Table 2).
 |
Table 2 Treatment Details of the Study Sample (Number of Eyes=31) |
 |
Figure 1 (A) Fundus view of the right eye showing Stage 4A ROP with macular dragging. (B) Postoperative LSV fundus photo showing flat retina with scleral buckle and peripheral endo-laser. |
There were five (16.1%) eyes which developed postoperative vitreous hemorrhage, five (16.1%) eyes which developed cataracts, three (9.7%) eyes which needed to undergo a second PPV, seven (22.6%) eyes which developed secondary glaucoma, and two eyes that ended up with phthisis bulbi. There were six (19.4%) eyes that did not develop any complication until the end of follow-up, 21 (67.7%) eyes with one complication, three (9.7%) eyes with two complications, and only one (3.2%) eye with three complications (as shown in Table 3).
 |
Table 3 Postoperative Complications (Number of Eyes=31, Classes are Not Mutually Exclusive) |
Figure 2 shows an eye with stage 4A ROP that was enrolled in the current study pre- and post-operatively.
Table 4 shows that there were 21 (67.7%) eyes that did not require any additional surgical intervention, four (12.9%) eyes that underwent lensectomy after the PPV (posterior subcapsular cataract), three (9.7%) eyes which received additional IVA, one (3.2%) eye which underwent goniotomy, one (3.2%) eye which underwent trabeculotomy, and one (3.2%) eye which underwent glaucoma valve implantation. The surgical success rate was 90.9% for stage 4a, 57.1% for stage 4b, and 33.3% for stage 5a, as illustrated in Figure 3.
 |
Table 4 Additional Surgical Interventions Done Following the Vitrectomy (Number of Eyes=31) |
 |
Figure 3 Surgical success rate of the study group. |
Figure 4 shows a case with stage 4B ROP that was enrolled in the current study.
There was a statistically significant association between the stage of disease and risk of F/re-RD as, among eyes with Stage 4a ROP, there was only one eye (9.1%) with F/re-RD, among eyes with Stage 4b, there were six (42.9%) eyes with F/re-RD, while among eyes with Stage 5a, there were four eyes (66.7%%) eye with F/re-RD. Eyes that had LV were significantly at more risk for developing F/re-RD, as all three eyes which underwent LV had F/re-RD, while from eyes with LSV there were eight (28.6%) eyes with F/re-RD. There were no statistically significant associations between failure of surgery/re-detachment (F/re-RD) and other study variables, as among those with GA <30 weeks there were four (30.8%) eyes with F/re-RD, there were six (33.3%) eyes with F/re-RD among those with BW ≤1,000g, in comparison to five (38.5%) eyes among those with BW >1,000g, and, regarding intraocular tamponade, the highest F/re-RD was seen among eyes injected with silicon (75%) (as shown in Table 5).
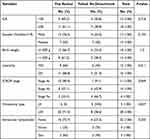 |
Table 5 Distribution of Eyes with Re-Detachment According to Study Variables (Number of Eyes=31) |
Discussion
The mean GA at time of surgery was 39.6±2.3 weeks (duration from birth until surgery was 10.2±2.0 weeks), and their mean BW was 1046.9±216.6 g. These results were comparable to results of Chandra et al in India, who studied 60 eyes of 30 babies who had stage 4 ROP, and reported that the mean GA at time of surgery was 40.8±2.2 weeks, and their birth weight was 1,214.5±329.7 g.9 In another study done by Iwahashi et al in Japan, LS-vitrectomy outcomes were studied in 61 eyes of 42 infants that had stage 4a ROP, and the reported GA at surgery was 41.4±5.9 years and their BW was 681.9±234.7 g.10 It is important to study the GA at surgery in order to know where we stand comparing to works done in other developing and developed countries, although the indications are almost the same in patients with stages 4 and 5, the rapid action and the decision to operate may differ, however, the GA at surgery was very close between our study and the aforementioned studies. It can be seen that the BW was close to the results of Chandra et al,9 while it was more than that reported by Iwahashi et al,10 this point was mentioned before by Vinekar et al, in India back in 2007, where they stated that the BW of children with ROP may be higher in developing countries.11 In addition, a recent study (2022) in Egypt, a developing Arab country, by Noor et al, reported that the mean BW of ROP infants was 1,900±562.2 g,12 and this could be attributed to the differences that cause an unstable clinical course in infants-of-developing countries, regardless having GA of more than 30 weeks or BW of more than 1,500 grams.13
In the current study, the overall surgical success rate was 64.5%, and it was 90.9% for stage 4a, 57.1% for stage 4b, and 33.3% for stage 5a. These rates are comparable to the results of Chandra et al, regarding stage 4a, (100% anatomic success rate), however better results were reported regarding stage 4b (89%).9 Another study done by Özdek et al, in Turkey, studied 70 eyes of babies with ROP whom underwent consecutive PPV, and reported success rates of 95.7% for stage 4a, 83.3% for stage 4b, and 50% for stage 5 (from a total of six eyes).14 Another Turkish study done by Karacorlu et al reported a success rate of 89% for stage 4a, 63% for stage 4b, and 42% for stage 5.15 Shah et al, in India, studied 20 eyes with ROP that underwent LSV, and reported a success rate of 100% for stage 4a and 89% for stage 4b.16 In another study that was carried out by Gadkari et al, also in India, for 20 eyes with stage 4b and 11 eyes with stage 5; the anatomic success rates were 90% and 45.45%, respectively.17 The families should have open discussions with their retinal surgeon to understand the potential risks, benefits, and expected outcomes of the procedure and it is important to understand that each case is unique and the success of PPV in eyes with ROP can depend on a combination of these factors including age and general health of the premature infant, presence of other ophthalmic comorbidities, such as cataracts or glaucoma, stage of ROP, extent of retinal detachment, aggressiveness of fibrovascular tissue on the retina, experience and skills of the surgeon, intraoperative complications and postoperative care, and more importantly technological advancements like equipment and visualization systems.
There were six (19.4%) eyes that did not develop any complication until the end of follow-up, five (16.1%) eyes developed postoperative vitreous hemorrhage, five (16.1%) eyes developed a cataract, three (9.7%) eyes underwent a second PPV, seven (22.6%) eyes developed secondary glaucoma, and two eyes ended up with phthisis bulbi. In 2010, Roohipoor et al, in Iran, reported higher rates of cataract (57%) but a similar rate of re-detachment (38%).18 Özdek et al reported postoperative complications in the form of cataract (2.8%), iatrogenic retinal break (1.4%), vitreous hemorrhage (11.4%), glaucoma (10%), esotropia (34%), nystagmus (20%), and phthisis bulbi (4.3%).14 One of the factors that might govern the postoperative complication rate is premedication with intravitreal anti VEGF, supporting that was a study done by Xu et al (2013) comparing between outcomes of PPV with and without intravitreal anti-VEGF premedication, and they reported that only the PPV group exhibited a significantly higher occurrence of preretinal hemorrhage (40%) when compared to the bevacizumab+PPV group, and some complication occurred only in the former group, including; Other complications in the control group included reproliferating of the fibrovascular tissues (two eyes), cataract (two eye), vitreous hemorrhage (two eyes), and glaucoma (one eye), and two eyes received lens surgery because of dense cataracts (13%).19 The causes of the re-detachment may be attributed to proliferative vitreoretinopathy, reopening of a previously treated break, or developing a new break (spontaneous or iatrogenic during vitrectomy),20 timing might help in identifying the cause, earlier re-detachments are more likely to be duo to new/re-opening of breaks, while late ones are attributed to peripheral vitreal traction.21
LSV has the advantage of better visual rehabilitation as it at least avoids aphakic amblyopia and aphakic glaucoma,16 however successful retinal reattachment following LSV for ROP does not prevent the occurrence of late complications, like recurrent RD, lens opacification, in addition to secondary glaucoma.22 The mechanism of secondary glaucoma might be explained by a number of factors, like is steroid response, which occur faster in comparison to other causes,23 trabecular angle dysgenesis,24 shallowing of the anterior chamber,2 and choroidal body swelling from retinal photocoagulation.25
It is important to evaluate the results of this study critically. Hence, the role of any prior to treatment such as injection or laser treatment can affect the surgical outcome profoundly. Most of the cases that were encountered had no prior treatment either by injection or laser. Most of the pre-op anti-VEGF injection was performed during Stage 4 within 48 hours prior to surgery not as an attempt to halt the progression of the disease at Stage 3. Therefore, most of the eyes that were operated on can be considered as “virgin” eyes with no prior treatment at Stage 3. This obviously can complicate intra-operative management especially due to the presence of active neovascularization at the edge of the ridges and epicenters. This also explains the finding of 16.1% post-operative vitreous hemorrhage. Dealing with an active disease intra-operatively is much more challenging than an eye which failed prior Stage 3 Anti-VEGF or laser retinopexy treatment. Additionally, this sheds light on the need for a more aggressive screening program to start earlier treatment and reduce having these cases need surgical intervention. As the Iraqi healthcare system improves and enables more of these premature babies to survive, the stricter the guidelines needed to address this increasing national healthcare problem.
Conclusions
This study presented the first surgical experience for vitrectomy in children with retinopathy of prematurity in our country, and the results were encouraging, with an overall surgical success rate of 64.5%, and 19.4% of eyes did not develop any complication until the 1-year follow-up.
Ethical Considerations
The caregiver(s) of each child were interviewed, and detailed information was provided regarding the disease, possible surgical interventions, expected outcomes and complications, along with written consent from each caregiver, and was in compliance with the Helsinki declaration and its subsequent update of ethical standards (Code: 2019/C081). This study was approved by the Ethical Committee at Ibn Al-Haitham Teaching Eye Hospital.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Coats DK. Retinopathy of prematurity: treatment and prognosis Online: upToDate, Inc.; 2023. Available from: https://www.uptodate.com/contents/retinopathy-of-prematurity-treatment-and-prognosis.
2. Sen P, Jain S, Bhende P. Stage 5 retinopathy of prematurity: an update. Taiwan J Ophthalmol. 2018;8(4):205–215. doi:10.4103/tjo.tjo_61_18
3. Courtright P, Hutchinson AK, Lewallen S. Visual impairment in children in middle-and lower‑income countries. Arch Dischildhood. 2011;96(12):1129–1134. doi:10.1136/archdischild-2011-300093
4. Kusaka S. Current concepts and techniques of vitrectomy for retinopathy of prematurity. Taiwan J Ophthalmol. 2018;8(4):216–221. doi:10.4103/tjo.tjo_102_18
5. Shah PK, Narendran V, Kalpana N, Tawansy KA. Anatomical and visual outcome of stages 4 and 5 retinopathy of prematurity. Eye. 2009;23(1):176–180. doi:10.1038/sj.eye.6702939
6. Hansen ED, Hartnett ME. A review of treatment for retinopathy of prematurity. Expert Rev Ophthalmol. 2019;14(2):73–87. doi:10.1080/17469899.2019.1596026
7. W-C W, Lai -C-C, Lin R-I, et al. Modified 23-gauge vitrectomy system for stage 4 retinopathy of prematurity. Archives of Ophthalmology. 2011;129(10):1326–1331. doi:10.1001/archophthalmol.2011.253
8. Gonzales CR, Boshra J, Schwartz SD. 25-Gauge pars plicata vitrectomy for stage 4 and 5 retinopathy of prematurity. Retina. 2006;26(7 Suppl):S42–6. doi:10.1097/01.iae.0000244288.63757.be
9. Chandra P, Kumawat D, Tewari R, Sinha R. Surgical outcomes of immediate sequential bilateral vitreoretinal surgery for advancing retinopathy of prematurity. Indian J Ophthalmol. 2019;67(6):903–907. doi:10.4103/ijo.IJO_741_18
10. Iwahashi C, Kurihara T, Kuniyoshi K, Kusaka S. Long-term visual prognosis of patients following lens-sparing vitrectomy for stage 4a retinopathy of prematurity. Int J Mol Sci. 2023;24(3):2416. doi:10.3390/ijms24032416
11. Vinekar A, Dogra MR, Sangtam T, Narang A, Gupta A. Retinopathy of prematurity in Asian Indian babies weighing greater than 1250 grams at birth: ten year data from a tertiary care center in a developing country. Indian J Ophthalmol. 2007;55(5):331–336. doi:10.4103/0301-4738.33817
12. Noor MS, Elbarbary M, Embabi SN, Zaki MA, Awad H, Al-Feky M. Screening and risk factors for retinopathy of prematurity in a tertiary care hospital in Cairo, Egypt. Clin Ophthalmol. 2022;16:3257–3267. doi:10.2147/OPTH.S383493
13. Fierson WM, Saunders RA, Good W; American Academy of Pediatrics Section on O, American Academy of O, American Association for Pediatric O, Strabismus, American Association of Certified O. Screening examination of premature infants for retinopathy of prematurity. Pediatrics. 2013;131(1):189–195. doi:10.1542/peds.2012-2996
14. Özdek Ş, Özmen MC, Yalınbaş D, Atalay HT, Coşkun D. Immediate sequential bilateral vitrectomy surgery for retinopathy of prematurity: a single surgeon experience. Turk J Ophthalmol. 2021;51(4):225–230. doi:10.4274/tjo.galenos.2020.07377
15. Karacorlu M, Hocaoglu M, Sayman Muslubas I, Arf S. Long-term functional results following vitrectomy for advanced retinopathy of prematurity. Br J Ophthalmol. 2017;101(6):730–734. doi:10.1136/bjophthalmol-2016-309198
16. Shah PK, Narendran V, Kalpana N. Safety and efficacy of simultaneous bilateral 25-gauge lens-sparing vitrectomy for vascularly active stage 4 retinopathy of prematurity. Eye. 2015;29(8):1046–1050. doi:10.1038/eye.2015.78
17. Gadkari S, Kamdar R, Kulkarni S, Kakade N, Taras S, Deshpande M. Vitreoretinal surgery for advanced retinopathy of prematurity: presentation and outcomes from a developing country. Can J Ophthalmol. 2015;50(1):54–60. doi:10.1016/j.jcjo.2014.08.017
18. Roohipoor R, Esfahani MR, Karkhaneh R, Ghassemi F, Ahmadabadi MN. Anatomical outcome of 25-gauge vitrectomy associated with scleral buckling in stage 5 retinopathy of prematurity: a case series study. Iran J Ophthalmol. 2010;22(2):25–31.
19. Xu Y, Zhang Q, Kang X, et al. Early vitreoretinal surgery on vascularly active stage 4 retinopathy of prematurity through the preoperative intravitreal bevacizumab injection. Acta Ophthalmologica. 2013;91(4):e304–e10. doi:10.1111/aos.12055
20. Kondo H, Arita N, Osato M, Hayashi H, Oshima K, Uchio E. Late recurrence of retinal detachment following successful vitreous surgery for stages 4B and 5 retinopathy of prematurity. Am J Ophthalmol. 2009;147(4):661–6.e1. doi:10.1016/j.ajo.2008.10.006
21. Nagpal M, Chaudhary P, Wachasundar S, Eltayib A, Raihan A. Management of recurrent rhegmatogenous retinal detachment. Indian J Ophthalmol. 2018;66(12):1763–1771. doi:10.4103/ijo.IJO_1212_18
22. Choi J, Kim JH, Kim S-J, Yu YS. Long-term results of lens-sparing vitrectomy for stages 4B and 5 retinopathy of prematurity. kjo. 2011;25(5):305–310. doi:10.3341/kjo.2011.25.5.305
23. Phulke S, Kaushik S, Kaur S, Pandav SS. Steroid-induced glaucoma: an avoidable irreversible blindness. J Curr Glaucoma Pract. 2017;11(2):67–72. doi:10.5005/jp-journals-10028-1226
24. Chandra P, Tewari R, Salunkhe N, Kumawat D, Chaurasia AK, Gupta V. Short-term incidence and management of glaucoma after successful surgery for stage 4 retinopathy of prematurity. Indian J Ophthalmol. 2019;67(6):917–921. doi:10.4103/ijo.IJO_33_18
25. Ajjarapu A, Dumitrescu A. Delayed anterior segment complications after the treatment of retinopathy of prematurity with laser photocoagulation. Frontiers in Ophthalmol. 2023;2:3.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


