Back to Journals » Clinical Ophthalmology » Volume 17
Visual Outcomes, Spectacle Independence, and Patient-Reported Satisfaction of the Vivity Extended Range of Vision Intraocular Lens in Patients with Early Glaucoma: An Observational Comparative Study
Authors Kerr NM, Moshegov S , Lim S, Simos M
Received 31 March 2023
Accepted for publication 17 May 2023
Published 30 May 2023 Volume 2023:17 Pages 1515—1523
DOI https://doi.org/10.2147/OPTH.S411561
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Nathan Mitchell Kerr,1– 3 Sophia Moshegov,4 Samantha Lim,3 Maria Simos3
1Centre for Eye Research Australia, Melbourne, VIC, Australia; 2Glaucoma Investigation and Research Unit, Royal Victorian Eye and Ear Hospital, Melbourne, VIC, Australia; 3Eye Surgery Associates, Melbourne, VIC, Australia; 4Department of Ophthalmology, The Royal Melbourne Hospital, Melbourne, VIC, Australia
Correspondence: Nathan Mitchell Kerr, Centre for Eye Research Australia, Level 7, 32 Gisborne St, East Melbourne, VIC, 3002, Australia, Tel +61 3 9929 8360, Email [email protected]
Purpose: This study aimed to evaluate and compare visual outcomes, spectacle independence, and patient satisfaction on bilaterally implanted Vivity extended depth-of-focus (EDOF) or monofocal intraocular lenses (IOLs) after cataract surgery in patients with early glaucoma.
Patients and Methods: In this retrospective, non-randomized, interventional cohort study, patients with early glaucoma undergoing cataract surgery received bilateral implantation of either EDOF (AcrySof IQ Vivity; Alcon) or monofocal (Clareon/SN6ATx/SN60WF; Alcon) IOLs. The primary outcome was monocular uncorrected intermediate visual acuity (UIVA). The secondary outcomes were monocular uncorrected distance (UDVA) and near (UNVA) visual acuity, spectacle independence, patient satisfaction, and photic phenomena. Fifty-eight eyes from 29 patients, including 32 eyes in the EDOF group and 26 eyes in the monofocal group, were included in the study.
Results: UIVA (0.06 ± 0.16 versus 0.39 ± 0.10 LogMAR; P < 0.001) and UNVA outcomes (0.29 ± 0.10 versus 0.55 ± 0.18 LogMAR; P < 0.001) were significantly better in the EDOF group than in the monofocal group, respectively. There was no difference in UDVA and corrected distance visual acuity outcomes between the groups (P > 0.05), but both spectacle independence and patient satisfaction scores were significantly higher in the EDOF group (P < 0.001 and P < 0.05, respectively). There was no difference in self-reported photic phenomena.
Conclusion: Bilaterally implanted EDOF IOLs provided excellent distance vision and better intermediate and near vision than monofocal IOLs in patients with early glaucoma. Spectacle independence and patient satisfaction were significantly higher in patients who received EDOF IOLs. Photic phenomena were rare and seldom bothersome.
Keywords: cataract, intraocular lenses, glaucoma
Introduction
Cataract surgery is one of the most common and successful operations worldwide.1 Traditional monofocal IOLs for emmetropia provide excellent distance vision, but they require spectacle use for intermediate and near vision tasks. Due to increasing demands for spectacle independence from patients,2 monovision or multifocal IOLs may be utilized.
Monovision, while reducing but not eliminating spectacle dependence,3 may be associated with loss of depth perception and suboptimal vision at intermediate distances.4 In contrast, multifocal IOLs provide a high level of spectacle independence and patient satisfaction, but they may be associated with unwanted photic phenomena, such as glare and halos.5 In particular, trifocal IOLs utilizing diffractive or refractive technology provide excellent near, intermediate, and distance vision but may impair contrast sensitivity due to the need to distribute light to different foci.6 As such, multifocal IOLs are relatively contraindicated in glaucoma, which is a common optic neuropathy that causes a reduction in contrast sensitivity that correlates with the degree of visual field loss.7
Extended depth-of-focus (EDOF) IOLs are a new technology designed to improve the range of vision, especially intermediate vision, with few photic phenomena and less loss of contrast sensitivity compared to traditional multifocal IOLs. As such, EDOF IOLs may be an option for people with glaucoma who wish to reduce their dependence on glasses but otherwise may not be candidates for multifocal IOLs. AcrySof IQ Vivity (Alcon, USA) is the first non-diffractive EDOF IOL that can deliver an extended focal range with a monofocal-like visual disturbance profile. Unlike multifocal IOLs, light is not split or distributed to several focal points, allowing the entire light energy to be used. In a prospective, randomized, controlled trial of 220 subjects bilaterally implanted with either Acrysof IQ Vivity IOLs or monofocal IOLs, the AcrySof IQ Vivity group had superior intermediate and near vision without degradation of distance vision compared to the monofocal control group. The incidence of bothersome visual disturbances in the Vivity group was low or similar to the monofocal group, with only 1% of patients bothered very much by halos. To date, there are limited clinical data on the performance of Acrysof IQ Vivity IOLs in glaucomatous eyes. This study aimed to evaluate the visual outcomes, spectacle independence, photic phenomena, and patient satisfaction on bilateral Acrysof IQ Vivity IOL implantation compared to bilateral monofocal IOLs in patients with early glaucoma.
Patients and Methods
Study Design and Patients
This was an investigator-initiated, retrospective, comparative cohort study conducted at a single-center in Melbourne, Australia. The study included consecutive patients with glaucoma who underwent bilateral cataract surgery. Patients were divided into two groups based on whether an EDOF or monofocal IOL was implanted. The same type of IOLs was inserted into each eye, and the choice of IOLs was determined according to the patient’s desire for spectacle independence post-operatively.
Inclusion criteria were a diagnosis of early glaucoma and visually significant cataract requiring cataract surgery. Glaucoma was defined as an optic disc appearance of neuroretinal rim or retinal nerve fiber layer thinning under slit-lamp examination, as confirmed by optical coherence tomography imaging (Zeiss Cirrus; Carl Zeiss AG, Oberkochen, Germany) associated with repeatable visual field defects on automated perimetry (Humphrey visual field analyzer; Carl Zeiss AG, Oberkochen, Germany), matching the anatomic appearance of the optic disc. Only patients with early-stage glaucoma based on the Hodapp-Parish-Anderson classification of visual field loss8 were included. Exclusion criteria included amblyopia, ocular surface disease, keratoconus, corneal endothelial dystrophy, prior corneal or refractive surgery, uveitis, macular pathology, angle-closure glaucoma, neovascular glaucoma, uveitic glaucoma, and non-glaucomatous optic neuropathy. This study was approved by the human research ethics committee at St Vincent’s Hospital Melbourne, which is affiliated with the Royal Victorian Eye and Ear Hospital and provides ethics approvals for private practices which do not have their own ethics committee. Informed consent was obtained from each patient. This study adhered to the tenets of the Declaration of Helsinki.
Intraocular Lenses
The AcrySof IQ Vivity (Alcon, USA) IOL is a single-piece, non-diffractive, extended vision posterior chamber IOL manufactured from hydrophobic acrylic materials with blue light-filtering chromophores. It has a 6.0-mm diameter biconvex aspheric optic manufactured from soft acrylic materials with high refractive index capable of being folded prior to insertion. The depth of field extension and monofocal-like visual disturbance profile were achieved through a proprietary wavefront focusing technology located on the anterior surface of IOLs. Two smooth surface transition elements stretch and shift light without splitting, allowing all light energy to be transmitted across the range of vision. The lens was designed to treat the effects of presbyopia by providing a full range of vision from distance to functional reading vision. The IOL had a negative spherical aberration to compensate for the positive spherical aberration of the cornea. Lastly, a blue light-filtering chromophore was designed to filter light to approximate the human crystalline lens and reduce the transmittance of potentially harmful ultraviolet and blue light wavelengths.
The control group received either AcrySof IQ (Alcon, USA) or Clareon (Alcon, USA) IOLs. Both are single-piece, aspheric, monofocal hydrophobic acrylic posterior chamber IOLs with a 6-mm optic. Like Vivity IOLs, these IOLs are biconvex and have negative spherical aberration to compensate for the positive spherical aberration of the cornea and they contain covalently bonded blue light-filtering chromophores. However, unlike Vivity IOLs, these lenses provide a single focus and are not designed to provide an extended range of vision. For insured patients, there was no additional cost to the patient to receive a Vivity IOL compared to a monofocal. Uninsured patients were required to pay an additional amount to receive a premium intraocular lens.
Surgical Technique
All surgeries were performed by an experienced cataract surgeon (NK) using a standardized phacoemulsification or femtosecond-laser assisted technique. Femtosecond pretreatment consisted of capsulotomy and lens fragmentation using a LenSx laser platform (Alcon, USA). Limbal relaxing incisions were not performed in either group. All IOLs were inserted into a capsular bag through a 2.4-mm temporal clear corneal incision. In patients who were not adequately responsive or intolerant to anti-glaucoma medications, a trans trabecular micro-bypass stent (iStent; Glaukos, USA) or Schlemm canal microstent (Hydrus; Ivantis, USA) was inserted at the time of cataract surgery. Postoperative treatment consisted of topical nepafenac 0.3% daily for two weeks and 1% prednisolone acetate four times a day for one month. Biometry was performed using an IOL Master 700 (Carl Zeiss AG, Germany), and all cases were targeted for emmetropia using the Barrett toric calculator and the manufacturer’s recommended a-constant. For all patients where regular corneal astigmatism was present, a toric IOL was selected to achieve the lowest level of residual astigmatism.
Data Collection
Preoperative data were collected, including patient demographics like age and sex, past ophthalmic history, and medication usage. All patients underwent comprehensive preoperative examinations, including uncorrected (UDVA) and corrected (CDVA) distance visual acuity tests, manifest refraction expressed as mean refractive spherical equivalent, automated perimetry (Humphrey visual field analyzer; Carl Zeiss AG, Germany), tonometry, slit-lamp anterior segment examination, dilated fundus examination, computerized and/or manual keratometry, optical biometry, IOL power, and target spherical equivalent. Intraoperatively, intraoperative complications were recorded.
Postoperative examinations were performed at 3–4 weeks after surgery. At this visit, the following parameters were recorded: monocular UDVA and CDVA, uncorrected intermediate visual acuity (UIVA) at 66 cm, and uncorrected near visual acuity (UNVA) at 40 cm. Visual acuity was measured using standardized Early Treatment Diabetic Retinopathy Study charts in photopic conditions (85 candelas/m). To prevent letter set memorization, different charts were presented to the same patient at each visit. Manifest refraction was performed, and the mean absolute error was calculated to assess deviations from the target refraction. Unsolicited, subjective, self-reported photic phenomena, defined as glare, halos, and/or dysphotopsia, were recorded.
Patient-reported outcomes were assessed three months after cataract surgery in the second eye. A questionnaire was administered by a trained orthoptist, and care was taken to ensure the full understanding of questions and to avoid influencing their responses. Patients were asked about spectacle dependence following surgery, bothering photic phenomena, and overall satisfaction with spectacle-free vision at certain distances. Lastly, patients were asked if they would choose the same lens again and if they would recommend the lens to relatives or friends. The questionnaire included the following questions:
- How often do you need to wear spectacles for distance/intermediate/near distances? Grading scale: 0, never; 1, rarely; 2, sometimes; 3, often; 4, always.
- How bothered have you been in the past 7 days by glares/halos/starbursts? Grading scale: 0, not at all; 1, a little; 2, somewhat; 3, very.
- In general, how satisfied are you with your spectacle-free vision for distance/intermediate/near distances? Grading scale: 0, very dissatisfied; 1, somewhat dissatisfied; 2, somewhat satisfied; 3, very satisfied.
- Would you choose the same lens again? Yes/no.
- Would you recommend this lens to your relatives or friends? Yes/no.
Primary Outcomes and Statistical Analysis
The primary outcome was UIVA at 66 cm. Secondary outcomes included monocular UDVA and CDVA, UNVA at 40 cm, spectacle independence, patient-reported satisfaction, and incidence of self-reported photic phenomena.
For continuous outcomes, descriptive statistics were presented as means and standard deviation for normally distributed data and as medians and interquartile ranges for non-normally distributed variables. Proportions were used to describe categorical characteristics. Depending on the normality of data, continuous outcomes were compared with Student’s t-test or Wilcoxon test. Categorical variables were compared using chi-square test or Fisher’s exact test. A P-value of <0.05 was considered statistically significant. Statistical analysis was performed in a JASP software (version 0.14.1, JASP Team).
Results
A total of 58 eyes from 29 patients were included in this study. There were 32 eyes from 16 patients in the EDOF group and 26 eyes from 13 patients in the monofocal group. Table 1 shows the demographic information of the IOL group. All patients had early glaucoma, and there was no statistically significant difference in the type of glaucoma, IOP, or degree of visual field loss between the two groups. Patients in the monofocal group were older and had a greater cup-to-disc ratio than those in the EDOF group. Preoperative measurements and refractive data are shown in Table 2, and there were no statistically significant differences between the two groups at baseline. The most common method of cataract surgery was phacoemulsification, being performed in 26 eyes in the EDOF group and 22 eyes in the monofocal group (P = 0.718) with the remainder of eyes receiving laser assisted cataract surgery. During cataract surgery, a transtrabecular minimally invasive stent was placed in 14 eyes in the EDOF group and 10 eyes in the monofocal group (P = 0.297).
 |
Table 1 Patient Demographics and Clinical Characteristics |
 |
Table 2 Preoperative Visual Acuity, Refraction, and Biometric Data |
Visual Outcomes and Spectacle Independence
Table 3 shows the visual and refractive outcomes of the EDOF and monofocal groups after surgery. The EDOF group had significantly better UIVA and UNVA than the monofocal group. Unaided reading performance was significantly better in the EDOF group, with this group reading a mean print size of N6 compared to N15 in the monofocal group. There was no statistically significant difference in UDVA and CDVA, and they had similar mean spherical equivalents. In the EDOF group, the level of spectacle independence was high, with the majority of patients never or rarely requiring spectacles for distance, intermediate, or near activities (Table 4). Spectacle independence for intermediate and near activities was significantly better in the EDOF group compared to the monofocal group (Table 4). In the monofocal group, 3 patients reported always requiring glasses for distance activities. In these cases, spectacle dependence for distance may not necessarily reflect dissatisfaction with their visual function, but rather habitual use or use of multifocal glasses. All surgeries were uncomplicated, and there were no adverse events.
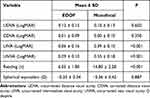 |
Table 3 Postoperative Visual Outcomes |
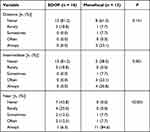 |
Table 4 Postoperative Spectacle Independence |
Photic Phenomena
Photic phenomena were infrequent and seldom bothersome for most patients. Most participants did not experience any glares, halos, or starbursts or reported that these were only a little bothersome. There was no significant difference in the incidence of any photic phenomena between the two groups (Table 5).
 |
Table 5 Incidence and Level of Photic Phenomena |
Patient Satisfaction
Patient satisfaction with spectacle-free vision was significantly higher in the EDOF group for distance, intermediate, and near vision than in the monofocal group (Table 6). All patients in the EDOF group were “very satisfied” with their distance and intermediate vision compared to 9/13 (69.2%) and 6/13 (46.2%) in the monofocal group, respectively. For near vision, 12/16 (75.0%) in the EDOF group were “very satisfied” with their unaided near vision compared to 5/17 (38.5%) in the monofocal group (P = 0.059). Patients who received an EDOF lens were more likely to report that they would choose the same lens again (16/16 [100%] in the EDOF group compared to 10/13 [76.9%] in the monofocal group; P = 0.085).
 |
Table 6 Satisfaction with Spectacle-Free Vision |
Discussion
This study compared the clinical performance of Acrysof IQ Vivity IOLs to that of monofocal IOLs for cataract surgery in people with glaucoma. In eyes with early glaucoma, Acrysof IQ Vivity IOLs provided an extended range of vision with significantly better intermediate and near vision while delivering similar distance vision and visual disturbance profile comparable to monofocal IOLs. Consistent with improvements in UIVA and UNVA, Acrysof IQ Vivity IOLs were associated with higher levels of spectacle independence and patient satisfaction than monofocal IOLs.
Other studies on eyes without glaucoma or concurrent diseases showed similar findings. Bala et al compared Acrysof IQ Vivity IOLs to aspheric SN60WF monofocal IOLs.9 In this prospective, randomized, double-masked clinical study, Acrysof IQ Vivity IOLs demonstrated superior mean distance-corrected intermediate vision, with >1-line difference in favor of Vivity IOLs compared with aspheric monofocal IOLs (0.075 ± 0.126 and 0.196 ± 0.160 logMAR, respectively).9 Similarly, Vivity IOLs showed superior distance-corrected near vision compared to monofocal IOLs, with approximately 1-line difference in favor of Vivity IOLs (0.306 ± 0.157 and 0.404 ± 0.175 logMAR, respectively).9 Intermediate vision is becoming increasingly relevant to quality of life due to the increasing use of computers, tablets, and smartphones. In this study, UIVA and UNVA were examined rather than CDVA to better reflect the vision-related quality of life.
The intermediate vision findings were consistent with the design features of the IOLs. Vivity IOLs creates an elongated focal point to enhance the range of vision and provide better UIVA and UNVA. This is achieved by two smooth surface transition elements that simultaneously stretch and shift light without splitting it into distinct focal points, which occurs in multifocal IOL technologies. By utilizing all available light energy, any reduction in contrast sensitivity can be minimized. This is important because contrast sensitivity is reduced in glaucoma, and this reduction correlates with the degree of visual field loss.7,10,11 Two Cochrane reviews showed that while multifocal IOLs provide greater near vision than monofocal IOLs, they reduce contrast sensitivity.12,13 Hence, multifocal IOL insertion is relatively contraindicated to patients with glaucoma.
EDOF lenses represent a new class of IOL that may have less contrast sensitivity loss compared to multifocal IOLs. This could provide an option for patients with glaucoma who wish to reduce their dependence on glasses.14 However, Bala et al found modest reductions in contrast sensitivity at higher spatial frequencies. At month 6, the difference in mean mesopic and photopic contrast sensitivity between Acrysof IQ Vivity IOLs and SN60WF monofocal IOLs were ≤0.23 and ≤0.16 log units, respectively.9 Additionally, aspheric IOLs used in Vivity IOLs provide higher mesopic contrast sensitivity than spherical and multifocal IOLs, which is a desirable feature for patients with glaucoma.15,16
In this study, the superior intermediate visual outcomes with Acrysof IQ Vivity IOLs were associated with high levels of glasses independence. In the Acrysof IQ Vivity IOL group, 81% of patients reported no need for glasses to perform intermediate visual activities compared to only 39% of patients who received monofocal IOLs. For near vision, only 6% of patients who received an extended range of vision IOLs always required glasses compared to 85% in the monofocal group. While EDOF IOLs did not improve near vision to the same extent as multifocal IOLs, the levels of spectacle independence were not greatly different to those reported for multifocal IOLs. Asena compared two models of trifocal IOLs and reported that 1% of patients always required glasses for near vision.17 In our study, the refractive target was emmetropia. Using monovision or mini-monovision may further improve near vision and spectacle independence.
The incidence of subjective photic disturbance in the Acrysof IQ Vivity IOL group was low, and the visual disturbance profile was similar to that of monofocal IOLs. There were no significant differences in the rates of glare, halos, or starbursts between the two IOL types. Halos were reported in 6.2% and 7.7% of patients who received EDOF and monofocal IOLs, respectively. The low incidence of halos may be related to their non-diffractive IOL design. By comparison, Law et al found that 80% of patients had difficulties with halo perception at 1 month following trifocal IOL insertion, and this decreased to 40% at 6 months after surgery.18 Patient satisfaction was high in 100% of patients who received Acrysof IQ Vivity IOLs, reporting that they would choose the same lens again compared to 76.9% in the monofocal group.
This study has several limitations. The two groups were not randomized or masked because patients selected their IOL prior to surgery. However, the objective visual acuity measurements are unlikely to be influenced by the patient’s knowledge of which IOL they had received, and the higher satisfaction scores correlated with better unaided intermediate vision suggesting that improved patient satisfaction was not solely based on pre-operative expectations. The participants had early glaucoma, so the results may not be generalizable to patients with moderate or advanced glaucoma. Visual outcomes were recorded at 3 weeks to 3 months after surgery, so the opportunity for neuroadaptation was limited. Contrast sensitivity and impact on automated perimetry were not assessed in this study. The impact of IOL choice on glaucoma monitoring with automated perimetry and retinal nerve fiber layer imaging was not assessed in this study. While we did not formally assess contrast sensitivity, the visual outcomes and high patient satisfaction scores would suggest that any degradation in contrast sensitivity is not clinically significant in this patient population. Based on the findings of this retrospective study, there is a need for future prospective studies to evaluate the performance of Acrysof IQ Vivity IOLs in moderate and advanced glaucoma, including defocus curves and modular transfer functions. Nonetheless, this is the first study to demonstrate the safety and efficacy of the Acrysof IQ Vivity IOL in patients with early glaucoma and it shows that the results are comparable to those achieved in non-glaucomatous eyes. For patients with early glaucoma, the Acrysof IQ Vivity may be an option for patients wishing to reduce their dependence on glasses. This can be combined with a minimally invasive procedure to reduce medication burden.
In conclusion, Acrysof IQ Vivity IOLs successfully restored the distance vision of people with early glaucoma after cataract surgery and provided superior UIVA and UNVA compared to monofocal IOLs. The aspheric, non-diffractive design was associated with a monofocal-like visual disturbance profile, even in patients with early glaucomatous visual field loss. Patient satisfaction and spectacle independence were high, with excellent, unaided intermediate vision. Acrysof IQ Vivity IOLs can be considered to correct presbyopia and reduce the dependence on glasses of patients with ocular hypertension and stable early glaucoma undergoing cataract surgery.
Disclosure
Dr Nathan Kerr has received consulting honoraria from Alcon (Fort Worth, Texas), Allergan (Irvine, California), Glaukos (San Clemente, California), Ivantis, NOVA Eye Medical, and Santen Pharmaceuticals (Osaka, Japan). Samantha Lim, Sophia Moshegov, and Maria Simos have no financial or proprietary interests to declare.
References
1. Gollogly HE, Hodge DO, St Sauver JL, Erie JC. Increasing incidence of cataract surgery: population-based study. J Cataract Refract Surg. 2013;39(9):1383–1389. doi:10.1016/j.jcrs.2013.03.027
2. Hawker MJ, Madge SN, Baddeley PA, Perry SR. Refractive expectations of patients having cataract surgery. J Cataract Refract Surg. 2005;31(10):1970–1975. doi:10.1016/j.jcrs.2005.03.065
3. Greenstein S. The quest for spectacle Independence: a comparison of multifocal intraocular lens implants and pseudophakic monovision for patients with presbyopia. Semin Ophthalmol. 2016;32:1–5. doi:10.1080/08820538.2016.1228408
4. Wilkins MR, Allan BD, Rubin GS, et al. Randomized trial of multifocal intraocular lenses versus monovision after bilateral cataract surgery. Ophthalmology. 2013;120(12):2449–2455.e1. doi:10.1016/j.ophtha.2013.07.048
5. Shah S, Peris-Martinez C, Reinhard T, Vinciguerra P. Visual outcomes after cataract surgery: multifocal versus monofocal intraocular lenses. J Refract Surg. 2015;31(10):658–666. doi:10.3928/1081597X-20150611-01
6. Gil MA, Varón C, Cardona G, Vega F, Buil JA. Comparison of far and near contrast sensitivity in patients symmetrically implanted with multifocal and monofocal IOLs. Eur J Ophthalmol. 2014;24(1):44–52. doi:10.5301/ejo.5000335
7. Hawkins AS, Szlyk JP, Ardickas Z, Alexander KR, Wilensky JT. Comparison of contrast sensitivity, visual acuity, and Humphrey visual field testing in patients with glaucoma. J Glaucoma. 2003;12(2):134–138. doi:10.1097/00061198-200304000-00008
8. Hodapp E, Parrish RK, Anderson DR. Clinical decisions in glaucoma. Mosby Incorporated. 1993;1:64.
9. Bala C, Poyales F, Guarro M, et al. Multicountry clinical outcomes of a new nondiffractive presbyopia-correcting IOL. J Cataract Refract Surg. 2022;48(2):136–143. doi:10.1097/j.jcrs.0000000000000712
10. Liska V, Eliásová M, Svĕrák J. Contrast sensitivity in glaucoma and ocular hypertension. Cesk Slov Oftalmol. 1998;54(6):373–382.
11. Wilensky JT, Hawkins A. Comparison of contrast sensitivity, visual acuity, and Humphrey visual field testing in patients with glaucoma. Trans Am Ophthalmol Soc. 2001;99:213–217.
12. Calladine D, Evans JR, Shah S, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2012;9(9):CD003169.
13. Silva de SR, Evans JR, Kirthi V, Ziaei M, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2016;12(12):CD003169. doi:10.1002/14651858.CD003169.pub4
14. Liu J, Dong Y, Wang Y. Efficacy and safety of extended depth of focus intraocular lenses in cataract surgery: a systematic review and meta-analysis. BMC Ophthalmol. 2019;19(1):198. doi:10.1186/s12886-019-1204-0
15. Caporossi A, Casprini F, Martone G, Balestrazzi A, Tosi GM, Ciompi L. Contrast sensitivity evaluation of aspheric and spherical intraocular lenses 2 years after implantation. J Refract Surg. 2009;25(7):578–590. doi:10.3928/1081597X-20090610-03
16. Zeng M, Liu Y, Liu X, et al. Aberration and contrast sensitivity comparison of aspherical and monofocal and multifocal intraocular lens eyes. Clin Exp Ophthalmol. 2007;35(4):355–360. doi:10.1111/j.1442-9071.2007.01452.x
17. Asena BS. Visual and refractive outcomes, spectacle Independence, and visual disturbances after cataract or refractive lens exchange surgery: comparison of 2 trifocal intraocular lenses. J Cataract Refract Surg. 2019;45(11):1539–1546. doi:10.1016/j.jcrs.2019.06.005
18. Law EM, Aggarwal RK, Kasaby H. Clinical outcomes with a new trifocal intraocular lens. Eur J Ophthalmol. 2014;24(4):501–508. doi:10.5301/ejo.5000407
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
