Back to Journals » Clinical Ophthalmology » Volume 17
Visual Outcomes, Quality of Vision, Patient Satisfaction and Spectacle Independence After Bilateral Implantation of the Synergy™ Intraocular Lens
Authors De Rojas JO, Sandoval HP, Potvin R , Solomon KD
Received 13 May 2023
Accepted for publication 26 June 2023
Published 9 August 2023 Volume 2023:17 Pages 2277—2285
DOI https://doi.org/10.2147/OPTH.S421185
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Joaquin O De Rojas,1 Helga P Sandoval,2 Richard Potvin,3 Kerry D Solomon2
1Center for Sight/US Eye, Sarasota, FL, USA; 2Carolina Eyecare Physicians/US Eye, Mt. Pleasant, SC, USA; 3Science in Vision, Bend, OR, USA
Correspondence: Joaquin O De Rojas, Center for Sight, PL, 2601 S. Tamiami Trail, Sarasota, FL, 34239, USA, Email [email protected]
Purpose: To evaluate vision, visual quality, patient satisfaction and spectacle independence after bilateral implantation of the TECNIS Synergy™ intraocular lens.
Setting: Two clinical practices in the USA.
Design: Ambispective unmasked non-randomized clinical trial.
Methods: Patients with a history of uneventful bilateral femtosecond laser assisted cataract surgery with the study IOL implanted, targeted for emmetropia, at least 3 months prior to the study visit were enrolled. Monocular and binocular visual acuity (VA) were measured at distance, intermediate and near, along with binocular mesopic VA. Low contrast binocular VA and reading speed in mesopic and photopic conditions were also measured. Patient satisfaction, spectacle independence, visual symptoms, and functional vision questionnaires were completed.
Results: Results from 52 subjects were available for analysis. Mean binocular unaided visual acuity was ~0.1 logMAR (20/20) from distance to 33 cm, with 81% of subjects having 0.2 logMAR (20/25) vision or better at all test distances and 92% reporting never needing glasses at any distance. Average reading speed at 40 cm was only 10 words/minute slower in dim light (p = 0.03). Mesopic and low contrast acuity appeared good. Halos were the most frequent and bothersome visual disturbances, with the greatest effect on driving at night. Eighty-eight percent of subjects reported being “completely” or “mostly” satisfied with their overall unaided vision.
Conclusion: This hybrid technology IOL provided a range of binocular visual acuity from distance to 33 cm and good functional vision, even in dim light. Patients should be advised of the likelihood of visual disturbances, particularly halos.
Keywords: synergy, multifocal IOL, diffractive, hybrid technology
Introduction
There are a considerable number of intraocular lens (IOL) options for patients interested in reducing their dependence on spectacles after cataract surgery. Standard monofocal spherical or toric IOLs generally provide excellent distance vision, but no correction for intermediate (computer) or near (reading) vision. Intermediate and near vision is not as good as can be achieved with presbyopia-correcting IOLs, but visual disturbances are less frequently noted.1 Enhanced monofocal IOLs extend the distant focal point range using spherical aberration, providing improved intermediate vision with little to no increase in the frequency of visual disturbances relative to a standard monofocal IOL.2–4 Extended depth of focus (EDOF) IOLs further increase the distance focal point range using a variety of optical principles including wavefront shaping,5 spherical aberration6 and diffractive technologies.7 EDOF lenses improve intermediate and near vision, but results at near are not as good as can be achieved with diffractive multifocal IOLs, though the likelihood of visual disturbances may be lower.8 Previous studies have shown that diffractive trifocal IOLs provide the greatest range of vision to patients, from distance to near, though the potential for visual disturbances may be slightly higher than for other correction options.1,8,9
The TECNIS Synergy™ intraocular lens has a unique proprietary design that incorporates both diffractive EDOF and bifocal technology on the posterior optic, to provide a range of vision from distance to near.10 Rather than from a trifocal effect, intermediate focus is provided from the EDOF design element while the bifocal component provides near and distance focal points. The aspheric anterior surface neutralizes the average spherical aberration in the eye, the improved high resolution lathing process decreases light scatter, and a violet-filtering chromophore is included to improve contrast sensitivity in dim light.11 For the purposes of this manuscript the IOL is referred to as a hybrid technology IOL or HT IOL.
There have been several international studies of the performance of this HT IOL, evaluating both monocular optical performance and binocular clinical outcomes. Shin et al compared optical performance to a monofocal IOL of similar design and material.12 They found significantly better intermediate and near vision with the HT IOL, though with a higher likelihood of visual disturbances based on objective optical quality measures. The study analyzed monocular data and did not include subjective outcomes. Ribeiro et al13 and Ozturkmen et al14 evaluated the lens after binocular implantation, which allowed inclusion of subjective patient responses.
The current study was designed to provide the first normative data (clinical outcomes and subjective responses) in the USA related to bilateral implantation of this lens with a target of emmetropia in both eyes.
Methods
This was an ambispective (surgery was completed in the past, the study evaluation visit was prospective), unmasked, non-randomized bilateral eye study conducted at two sites. It was designed to evaluate the clinical outcomes and subjective patient responses associated with bilateral implantation of the study lens when both eyes were targeted for a plano refraction. The study was registered with clinicaltrials.gov (record NCT05418153) after review and approval by an institutional review board (Salus IRB, Austin, TX, USA). The study adhered to the tenets of the Declaration of Helsinki.
Patients 18 years or older who had uneventful bilateral femtosecond laser assisted cataract surgery and implantation of the study lens (with a target of emmetropia in both eyes) at least 3 months prior to their diagnostic visit were eligible for inclusion. Lenses could be toric or non-toric. For non-toric cases, low amounts of astigmatism (> 0.50 diopters but <1.25 diopters) were corrected with using the surgeon’s preferred methodology (limbal relaxing incisions or laser arcuate incisions). Patients with ocular pathology that was likely to affect the final visual outcome (eg, glaucoma, uveitis, severe dry eye, corneal dystrophy) were excluded, as were patients with a history of prior refractive or intraocular surgery. Corrected distance vision in both eyes at enrollment had to be 20/32 (0.2 logMAR) or better. This criterion was adopted to avoid any effects of compounding pathology; previous studies of the lens indicate that 99% or more of subjects would meet this criterion.12,13 Subjects read and signed an IRB-approved informed consent document on enrollment. No vulnerable subject populations were recruited.
Prior to the diagnostic study visit, the relevant preoperative and surgical data were extracted from the clinical records. At the diagnostic visit (or visits, if the patient preferred two visits to reduce fatigue) the manifest refraction was determined and the uncorrected and corrected distance visual acuity (UDVA and CDVA, respectively) were measured monocularly and binocularly. Binocular intermediate (66 cm) and near (40 cm and 33 cm) VA were also measured in the corrected and uncorrected state, in both photopic and mesopic conditions. Corrected binocular low contrast (10%) CDVA was also measured at distance (4 m) in both photopic and mesopic conditions. The subject’s reading speed with a target at 40 cm was measured under both photopic and mesopic conditions.
In addition to the objective testing above, several questionnaires were completed by subjects at the postoperative visit, including the Patient Reported Spectacle Independence Questionnaire (PRSIQ), the Patient Reported Visual Symptoms Questionnaire (PRVSQ), and the VFQ-25 visual function questionnaire. Subjects also had the opportunity to provide unsolicited comments on their vision at the study visit.
The diagnostic data was collected during the study visit and assembled into Excel spreadsheets, which were then imported into an Access database for data checking and preliminary analysis (both Microsoft Corp., Redmond, USA). The Statistica data analysis software system, version 12 (TIBCO Software Inc., Palo Alto, CA, USA) was used for more detailed analyses. A deidentified copy of the data set on which this study is based can be obtained by emailing a request to [email protected].
Results
A total of 52 subjects completed the study visit; no subject required a second visit to complete the testing. Toric IOLs were implanted in 22 of 104 eyes (21%). The demographics and postoperative refractive status of study subjects were typical of a US surgical practice (Table 1). Eighty of 104 eyes (77%) had a postoperative manifest refraction spherical equivalent (MRSE) within 0.50 D of plano with 0.50 D or less of cylinder. Fifty of 52 subjects (96%) had one or both eyes in that range. There was no statistically significant difference in the MRSE, refractive cylinder, UDVA or CDVA between the eyes implanted with toric or non-toric IOLs (p > 0.05 in all cases).
 |
Table 1 Demographic and Refractive Data (n = 52 Subjects, 104 Eyes) |
Figure 1 shows the recently recommended standard set of graphs for evaluating the performance of presbyopia correcting IOLs.15 Note that the cumulative VA data on the left are binocular, while the refractive and CDVA/UDVA data are monocular. Figure 2 shows the mean binocular uncorrected and distance corrected VA by test distance. In both uncorrected and distance corrected conditions at all distances the mean VA was logMAR 0.02 (20/20−1) or better. Distance correction significantly improved distance vision (p < 0.01), but there was no statistically significant difference between the mean uncorrected and distance corrected VA at any of the other distances (p > 0.05 in all cases). Forty-two of 52 subjects (81%) had an uncorrected VA of logMAR 0.1 (20/25) or better at all test distances.
 |
Figure 1 Composite standard graph for evaluating EDOF and multifocal IOL outcomes. |
 |
Figure 2 Mean binocular visual acuity at various test distances. Abbreviation: logMAR, the log of the minimum angle of resolution. |
Table 2 contains a summary of the mesopic and low contrast visual acuity testing. Note that mesopic data from 17 subjects was unavailable due to incorrect testing procedures (tests were conducted under scotopic conditions instead of mesopic). The mean binocular mesopic VA at intermediate and near, in both the uncorrected and distance corrected conditions ranged between 0.21 and 0.24 logMAR (between 20/32 and 20/32−2) in all cases, about a 1.5 letter difference. There were no statistically significant differences between the uncorrected and distance corrected VA at any distance, and no statistically significant difference in VA at the various test distances for the given test condition (p > 0.05 in all cases). Fifty-one percent of subjects (18/35) had a mesopic binocular DCNVA at 33 cm of 0.2 (20/32) or better. The mean low contrast acuity in photopic conditions was 0.13 logMAR (~20/25-1) and was about 3 lines worse in mesopic conditions. The photopic low contrast acuity was about 2 lines lower than the photopic high contrast acuity (Figure 1). Ninety-eight percent of subjects (51/52) had a photopic low contrast acuity of 0.3 logMAR (20/40) or better.
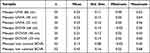 |
Table 2 Mesopic and Low Contrast Visual Acuity Results (logMAR) |
A plot of reading speed by reading acuity is shown in Figure 3, in both mesopic and photopic conditions. There were fewer results for the mesopic condition, again due to incorrect test procedures while evaluating some subjects. Mean reading speed was slightly slower in dim light vs bright light (172 ± 5 vs 182 ± 4, p = 0.03) in the letter size range from 1.1 to 0.6 logRAD (log of the reading acuity determination, equivalent to logMAR letter size). The critical print size for reading in photopic conditions was 0.2 logMAR, the size of small column newsprint. The critical print size in mesopic conditions was about 0.6 logMAR.
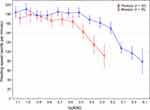 |
Figure 3 Reading speed and reading acuity in photopic and mesopic conditions. Abbreviation: logRAD, the log of the reading acuity determination. |
Table 3 contains a summary of the results for the PRSIQ questionnaire. Forty-eight of 52 subjects (92%) reported not needing glasses at any distance. The use of glasses was lower, with only two subjects reporting they wore glasses sometimes for near work while one wore them sometimes for various distances. The strain to see without glasses was highest for distance viewing, with 5 of 52 subjects (10%) reporting straining to see all or most of the time. There was no apparent correlation between this strain with distance viewing and the residual refractive error. Subjects tended to be most satisfied with their intermediate vision and least satisfied with distance vision, with 88% of subjects stating they were “completely” or “mostly” satisfied overall.
 |
Table 3 PRSIQ Summary Results (n = 52) |
Figure 4 shows the frequency and degree of bother for the visual disturbances identified in the PRVSQ questionnaire. Halos were the most reported disturbances and were the disturbance that was most often rated extreme. Starbursts and light sensitivity were the next most reported, though the degree of bother associated with them was lower. In the four subjects that always experienced glare, the degree of bother was rated extreme. As part of the questionnaire, subjects were allowed to comment on the effect of any visual disturbances on their daily life; twenty-two subjects provided comments regarding these visual disturbances. Difficulty driving was the single most identified item, with 15 of 22 subjects (68%) reporting this due to one or more of halos, light sensitivity, starbursts and glare. Outside of the questionnaires, subjects were asked if they had any general comments regarding their vision. The most common comment from subjects was the presence of halos (15/52, 29%), with most mentioning night/dim light conditions.
 |
Figure 4 Reported visual disturbances from the PRVSQ. (A) Frequency of occurrence and (B) Degree of associated bother. Abbreviation: PRVSQ, patient reported visual symptoms questionnaire. |
Selected responses to the VFQ-25 visual function questionnaire are shown in Table 4, ranked roughly by distance from near to far. Subjects reported little or no difficulty with a wide range of tasks at varying distances. The most difficulty was reported with driving at night. Nine of the 52 subjects (17%) reported severe difficulty (6) or that they had discontinued driving at night because of their vision (3).
 |
Table 4 VFQ-25 Questionnaire, Selected Responses |
Discussion
Ribeiro et al reported a functional range of vision of 3.0 D with this HT IOL, with a relatively flat binocular defocus curve in that range, between 0.0 logMAR and 0.1 logMAR.13 This appears consistent with our binocular visual acuity results at the 4 distances we tested. Dick et al reported similar results, with CDVA outcomes at various test distances that matched those in the current study.16 The findings of Dick et al regarding mesopic DCNVA at 33 cm and low contrast CDVA were also similar to those in the current study, and somewhat better than results reported for the Panoptix trifocal IOL (Alcon).16 VA results from Ozturkmen et al at various test distances were also very similar to the results in the current study.14
The average reading speed found here matched the speed determined by Benyoussef et al for the same lens, and was higher than that reported for the FineVision HP trifocal (PhysIOL).17 Reading distances were similar in all cases. We could find no comparative mesopic reading speed results in the literature. This would be an area of interest for future research, as functional reading may often take place in suboptimal illumination conditions (eg, reading on a bus or reading the menu in a restaurant).
Spectacle independence at all distances was very high, which corroborates the findings of Ribeiro et al13 and Ozturkmen et al,14 though the latter study found complete spectacle independence at near while several subjects in the current study reported needing/wearing spectacles for near vision. The former study found 3.7% of subjects required some use of spectacles for intermediate and/or near work, which is in line with the findings in the current study.
Ribeiro et al13 also reported on visual disturbances. As with the current study, halos were the most commonly reported and one of the most bothersome. Glare was reported less frequently, but tended to be more severe and more bothersome than halos. This appears consistent with the findings in the current study, though both of these studies reported frequency/bother of halos that were much higher than reported by Gabric et al for the same lens.18 Using a different questionnaire, Ferreira et al found results for visual disturbances that were very similar to those in the current study.19 They also reported that the frequency, severity and degree of bother of visual disturbances from this HT IOL were similar to those found with two diffractive trifocal IOLs: the Panoptix trifocal (Alcon) and the FineVision trifocal (Physiol). Dick et al15 also found halos were the most common visual disturbance with the HT IOL, with overall rates/severity of visual disturbances similar between the HT IOL and the Panoptix trifocal. Ozturkmen et al14 found in their study of the same HT IOL that driving at night was rated the most difficult task by study subjects, an observation that appears confirmed in the current study. These results suggest that a “mix-and-match” approach with the lens may be a preferred alternative in some patients, replacing the HT IOL in one eye, presumably in the dominant eye, with an EDOF IOL designed to provide superior distance vision (ongoing study).
The level of satisfaction reported in the current study is remarkably similar to the level found by Ribeiro et al,13 with 88% of subjects being “completely” or “mostly” satisfied with their overall vision.
There are limitations to the current study. The COVID pandemic significantly reduced the number of patients interested in participating in a post-operative diagnostic visit, so enrollment was lower than planned. Mesopic testing was conducted incorrectly in some patients, reducing the effective sample size for those tests.
In summary, visual outcomes with the HT IOL studied here showed a wide range of functional vision, with better very near to intermediate vision than has been reported for other presbyopia-correcting IOLs, and with a similar profile for the frequency/severity of visual disturbances.
Funding
The study was supported by an investigator-initiated study grant from J&J Vision, USA (IIT: JD-1262).
Disclosure
Joaquin O. De Rojas is a consultant for Advanced Euclidean Solutions, Johnson & Johnson Vision, Oculus Biologics, Carl Zeiss Meditec and Sun Pharmaceuticals. Helga Sandoval reports grants paid to institution from Johnson and Johnson Vision and royalties from TissueTech. Richard Potvin is a consultant to and reports personal fees from Alcon, Hoya, and Carl Zeiss Meditec. Kerry D. Solomon is a consultant for Alcon Laboratories, Allergan, Aquesys, Bausch and Lomb, Clarvista Medical, Glaukos, Icon Bioscience, Imprimis, Integrity Digital Solutions, Johnson & Johnson Vision, Kala Pharmaceuticals, Lenstec, Mati Therapeutics, Octane Visionary VC Fund, Ocuhub, Omeros Corporation, Pogotec, PRN, Tearlab, Versuant. The authors report no other conflicts of interest in this work.
References
1. de Silva SR, Evans JR, Kirthi V, Ziaei M, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2016;12(12):CD003169. doi:10.1002/14651858.CD003169.pub4
2. Steinmüller LN, Greve D, Rua Amaro D, Bertelmann E, von Sonnleithner C. Analysis of higher-order aberrations in relation to the clinical outcome of an enhanced monofocal IOL. Eur J Ophthalmol. 2022;11206721221134171. doi:10.1177/11206721221134171
3. Garzón N, Poyales F, Albarrán-Diego C, Rico-Del-Viejo L, Pérez-Sanz L, García-Montero M. Visual and optical quality of enhanced intermediate monofocal versus standard monofocal intraocular lens. Graefes Arch Clin Exp Ophthalmol. 2022;260:3617–3625. doi:10.1007/s00417-022-05700-y
4. Wan KH, Au ACK, Kua WN, et al. Enhanced monofocal versus conventional monofocal intraocular lens in cataract surgery: a meta-analysis. J Refract Surg. 2022;38:538–546. doi:10.3928/1081597X-20220707-01
5. Kohnen T, Petermann K, Böhm M, et al. Nondiffractive wavefront-shaping extended depth-of-focus intraocular lens: visual performance and patient-reported outcomes. J Cataract Refract Surg. 2022;48:144–150. doi:10.1097/j.jcrs.0000000000000826
6. Ruiz-Mesa R, Blanch-Ruiz J, Ruiz-Santos M, Montés-Micó R. Optical and visual quality assessment of an extended depth-of-focus intraocular lens based on spherical aberration of different sign. Int Ophthalmol. 2021;41:1019–1032. doi:10.1007/s10792-020-01659-z
7. Sakisaka T, Minami K, Takada K, Mori Y, Miyata K. Functional visual acuity after implantation of diffractive extended depth-of-focus intraocular lenses using an echelett optics. BMC Ophthalmol. 2021;21(1):418. doi:10.1186/s12886-021-02189-7
8. Rodov L, Reitblat O, Levy A, Assia EI, Kleinmann G. Visual outcomes and patient satisfaction for trifocal, extended depth of focus and monofocal intraocular lenses. J Refract Surg. 2019;35:434–440. doi:10.3928/1081597X-20190618-01
9. Cho JY, Won YK, Park J, et al. Visual outcomes and optical quality of accommodative, multifocal, extended depth-of-focus, and monofocal intraocular lenses in presbyopia-correcting cataract surgery: a systematic review and Bayesian network meta-analysis. JAMA Ophthalmol. 2022;140:1045–1053. doi:10.1001/jamaophthalmol.2022.3667
10. Johnson & Johnson Vision. TECNIS Synergy IOL with TECNIS Simplicity Delivery System. 05/2021. Santa Ana, CA: Johnson & Johnson Vision; 2021.
11. Nakano S, Miyata A, Kizawa J, Kurosaka D, Miyata K, Oshika T. Blue light-filtering and violet light-filtering hydrophobic acrylic foldable intraocular lenses: intraindividual comparison. J Cataract Refract Surg. 2019;45:1393–1397. doi:10.1016/j.jcrs.2019.05.027
12. Shin DE, Lee H, Koh K. Comparative analysis of a presbyopia-correcting intraocular lens that combines extended depth-of-focus and bifocal profiles with a standard monofocal intraocular lens. BMC Ophthalmol. 2022;22:302. doi:10.1186/s12886-022-02516-6
13. Ribeiro FJ, Ferreira TB, Silva D, Matos AC, Gaspar S. Visual outcomes and patient satisfaction after implantation of a presbyopia-correcting intraocular lens that combines extended depth-of-focus and multifocal profiles. J Cataract Refract Surg. 2021;47:1448–1453. doi:10.1097/j.jcrs.0000000000000659
14. Ozturkmen C, Kesim C, Karadeniz PG, Sahin A. Visual acuity, defocus curve and patient satisfaction of a new hybrid EDOF-multifocal diffractive intraocular lens. Eur J Ophthalmol. 2022;32:2988–2993. doi:10.1177/11206721211057338
15. Fernández J, Ribeiro FJ, Rodríguez-Vallejo M. Standard for collecting and reporting outcomes of IOL–based refractive surgery: update for enhanced monofocal, EDOF, and multifocal IOLs. J Cataract Refract Surg. 2022;48(11):1235–1241. doi:10.1097/j.jcrs.0000000000001013
16. Dick HB, Ang RE, Corbett D, et al. Comparison of 3-month visual outcomes of a new multifocal intraocular lens vs a trifocal intraocular lens. J Cataract Refract Surg. 2022;48(11):1270–1276. doi:10.1097/j.jcrs.0000000000000971
17. Benyoussef AA, Reboux N, Cochener B. Comparison of bilateral reading performance among two presbyopia-correcting intraocular lenses. J Refract Surg. 2022;38:428–434. doi:10.3928/1081597X-20220516-02
18. Gabrić N, Gabrić I, Gabrić K, Biščević A, Piñero DP, Bohač M. Clinical outcomes with a new continuous range of vision presbyopia-correcting intraocular lens. J Refract Surg. 2021;37:256–262. doi:10.3928/1081597X-20210209-01
19. Ferreira TB, Ribeiro FJ, Silva D, Matos AC, Gaspar S, Almeida S. Comparison of refractive and visual outcomes of 3 presbyopia-correcting intraocular lenses. J Cataract Refract Surg. 2022;48:280–287. doi:10.1097/j.jcrs.0000000000000743
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
