Back to Journals » Clinical Ophthalmology » Volume 18
Visual Improvement and Lowered Intraocular Pressure After Surgical Management of In-The-Bag Intraocular Lens Dislocation and Aphakia Correction; Retrospective Analysis of Scleral Suturing versus Retropupillary Fixated Iris-Claw Intraocular Lens During a 5-Year Period
Authors Johansson Iranipour B, Rosander JH, Zetterberg M
Received 17 October 2023
Accepted for publication 24 January 2024
Published 2 February 2024 Volume 2024:18 Pages 315—324
DOI https://doi.org/10.2147/OPTH.S445244
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Bella Johansson Iranipour,1 Jonas H Rosander,1 Madeleine Zetterberg2,3
1Department of Ophthalmology, The NU Hospital Group, Region Västra Götaland, Uddevalla, Sweden; 2Department of Clinical Neuroscience/Ophthalmology, Sahlgrenska University Hospital, Mölndal, Sweden; 3Institute of Neuroscience and Physiology, The Sahlgrenska Academy at University of Gothenburg, Gothenburg, Sweden
Correspondence: Madeleine Zetterberg, Department of Clinical Neuroscience/Ophthalmology, The Sahlgrenska Academy at University of Gothenburg, Sahlgrenska University Hospital, Mölndal, SE-431 80, Sweden, Tel +46-31-3433255 ; +46-709-12 61 42, Fax +46-31-412904, Email [email protected]
Purpose: We compare and evaluate the visual outcome and complication rate of two different techniques of surgical management of in-the-bag intraocular lens (IOL) dislocation or aphakia correction. In addition, we evaluate possible risk factors for IOL dislocation or aphakia.
Patients and Methods: This retrospective case series reviewed medical records for all patients who had undergone surgery for IOL dislocation or aphakia during a 5-year period at a single ophthalmic center in Sweden. The two most common procedures, scleral suturing of dislocated in-the-bag IOL and retropupillary fixation of iris-claw IOL, were further analyzed. Main outcome measures were best-corrected visual acuity (BCVA), reoperations, and complications.
Results: The study comprised 110 eyes, including scleral suturing procedures (n=35) and retropupillary iris-claw IOL (n=75). There was a significantly higher rate of dense cataract (p=0.030) and posterior capsular rupture (PCR), (p=0.016) among iris-claw cases at the primary cataract extraction with pseudoexfoliations in about two-thirds of patients in both groups. All eyes in the scleral suturing group had an IOL dislocation. In the iris-claw group, 23 eyes (30.7%) were aphakic following complicated cataract surgery with PCR. No intraoperative complications occurred in any eyes during the secondary IOL procedure. Both groups showed significant improvement in BCVA, yet there was no significant difference between groups in postoperative BCVA (p=0.263). However, the scleral suturing group experienced a significantly larger improvement in BCVA due to worse BCVA preoperatively (p=0.005). Intraocular pressure decreased significantly after both repositioning and exchange surgery (p=0.002 and 0.010 respectively), but improvement between groups was not significantly different (p=0.264).
Conclusion: Both surgical methods resulted in significantly improved BCVA and lowering of IOP and can be considered safe with limited complications. The outcome was similar between groups. Pseudoexfoliation prevalence was high in both groups indicating that it may be a risk factor for either aphakia or late IOL dislocation.
Keywords: cataract, iris-claw IOL, late-in-the-bag IOL dislocation, scleral sutured, surgery
Introduction
Cataract surgery with intraocular lens (IOL) implantation is one of the most successful procedures in ophthalmology and remains the ideal procedure following cataract extraction. However, in some patients where IOL implantation is not possible during primary cataract extraction or due to a late dislocation of the IOL a second procedure is necessary to obtain a well-positioned IOL. Management decisions are based on each individual case’s clinical features and the performing surgeon’s preference.1,2 Management options for a dislocated posterior chamber IOL (PC IOL) include IOL repositioning with or without scleral fixation sutures (depending on residual capsular support), and IOL exchange. If capsular support is adequate, IOL repositioning without scleral fixation suture is generally the preferred technique. When adequate capsular support is absent in cases with an IOL dislocation or an aphakic eye, surgical correction remains challenging. In these cases, an angle supported anterior chamber intraocular lens (AC IOL), an iris fixated posterior chamber IOL, a transscleral sutured posterior chamber lens (PC IOL), or an iris-claw intraocular lens can be implanted.1,3,4 Further experimentation has led to the development of the Canabrava and Yamane technique in recent years.5
The purpose of this study was to evaluate and compare visual outcomes, and the complication rate between the two most common techniques of surgical management of IOL dislocation or aphakia correction at our clinic.
Patients and Methods
This retrospective study was conducted in accordance with the tenets of the Declaration of Helsinki and was approved by the Regional Ethics Committee in Gothenburg, Västra Götaland County, Sweden (Dnr 040–14, 20140224). As this was a retrospective study that contained little demographic information and deidentified data were presented at group level, the Ethics Committee deemed it unnecessary with informed consent from patients.
Cases were identified by searching electronic medical records from January 2010 to December 2014 for patients who had surgical management of early/late IOL dislocation or aphakia at the Eye Clinic in Uddevalla, Sweden, with the Current Procedural Terminology Code CJF 00–99 for IOL repositioning, or IOL exchange procedures/aphakia correction. No patients were excluded to ensure that the data set was a true representation of the real-world setting.
IOL dislocation was defined as any case requiring IOL repositioning surgery that occurred after primary cataract surgery in which the initial IOL position had been noted as good during cataract surgery. Aphakia was defined as the absence of both an endogenous lens and an IOL.
A total of 165 patients who had received a secondary IOL were identified. Of these, 110 were managed by either scleral suturing or an iris-claw IOL. The preoperative data collection included basic demographics, status before primary surgery, such as pseudoexfoliation (PEX), dense cataract, ocular comorbidity, any medication that may affect the outcome of surgery (such as, alpha 1-antagonist), the date and characteristics of the cataract surgery, and intraoperative difficulties (mechanical pupil dilation, floppy iris syndrome, iris prolapse, and the intraoperative complications posterior capsule rupture or zonular dehiscence). Secondary procedures, that is, Neodymium: YAG (Nd: YAG) laser treatment for posterior capsule opacification after cataract surgery, were also noted.
In addition, data was collected from the examination performed just prior to secondary procedures, including best-corrected visual acuity (BCVA), intraocular pressure (IOP), axial length, ocular comorbidity (corneal dystrophy/edema, diabetes, age-related macular degeneration [AMD], glaucoma), and the grade of dislocation: grade 1=within optical axis; grade 2=haptic visible; grade 3=in to the vitreous.
These cases were individually reviewed to determine the indication for surgery (IOL dislocation, aphakia), surgical technique (repositioning, exchange, aphakia correction), time interval between primary cataract surgery and secondary procedure, surgical complications (intraoperative and postoperative), additional surgical procedures performed intraoperatively (vitrectomy, iridectomy), BCVA, and refractive prediction error.
Surgical Techniques
Surgical procedures were performed by the same two surgeons in subtenonal anesthesia or under general anesthesia according to patients’ needs. Anterior vitrectomy was performed if vitreous was present in the anterior chamber. Cefuroxime 1 mg was injected intracamerally at surgery end. When patients could not manage eye drops postoperatively, 0.5 mL Methylprednisolone 40 mg/mL was injected subconjunctivally. In remaining cases, dexamethasone 1 mg/mL or nepafenac 1mg/mL was prescribed topically for three to four weeks. The SRK/T formula with an estimated A-constant of 117.5 (range 117.0–118.0) was used together with conventional biometry (IOL Master; Carl Zeiss Meditec AG, Germany) to calculate the power of the iris-claw IOL positioned retropupillary.
Retropupillary Positioned Iris-Claw IOL
A 6.0 mm sclerocorneal tunnel incision was made at 12 o´clock or temporally, and two paracenteses were created at two clock-steps left and right of the main incision. An ophthalmic viscosurgical device (OVD) was placed in the anterior chamber through the paracentesis. In IOL dislocation cases, the IOL was removed with the aid of McPherson lens forceps under the protection of OVD. Anterior vitrectomy was then performed. Acetylcholine chloride 1% was injected if necessary. The inverted iris fixated IOL (Artisan aphakic IOL; Ophtec BV, Groningen, The Netherlands) was inserted anteriorly of the iris through the scleral tunnel and allowed to rest on the iris. The IOL was then rotated with hook 90 degrees from the main incision. The lens was grasped with a specifically designed lens-holding forceps and the haptics of the lens were sequentially pushed behind the iris through the pupil and centered behind. The mid-peripheral iris tissue was pushed to the claw haptics with a Simsky hook via a paracentesis. The incision was closed with interrupted 10–0 nylon sutures. The OVD was removed via irrigation and aspiration.
Scleral Suturing of Dislocated IOL
After conjunctival peritomy, a partial-thickness scleral flap was created, 1.0 mm posterior to the limbus. A limbal paracentesis site was prepared along the same axis, 180 degrees from the scleral suture site. OVD was placed in the anterior chamber through the paracentesis. One needle of a double-arm 10–0 Prolene needle was passed through the paracentesis site and then underneath the intraocular lens haptic. The free hand of the surgeon then passed a bent 27-gauge needle, attached to a 2.5 mL syringe, through a bed of partial thickness, limbus-based scleral flap. A needle attached to a 2.5 mL syringe, functioning as a guiding tube, was used to catch the 10–0 Prolene needle, and both were then removed together. The other needle of the Prolene suture was also passed through the same paracentesis site, above the same haptic, and guided out in a similar fashion. With the haptic being thus well supported, the knot was tied and buried under a scleral flap. A similar procedure was performed for the second haptic if necessary. The OVD was removed via irrigation and aspiration.
Statistical Analysis
Visual acuity was converted to LogMAR for arithmetic procedures. Statistical analysis was performed using SPSS for Mac software (version 25, SPSS, Inc.). For comparison between the two groups, the Pearson’s chi-square (χ2) test was used for categorical data and independent samples t-test for continuous parameters. If the number of cases was less than five in each group, the Fisher’s exact test was used. For within-group data comparison before and after surgery, a paired samples t-test was used. A p-value of less than 0.05 was considered statistically significant. Results are presented as mean with standard deviation and range or number (percentage) as appropriate.
Results
In total, 165 eyes were identified that had been subjected to any surgical procedure for IOL repositioning, IOL exchange, or aphakia correction. The study compared the two most common procedures, that is, scleral suturing (35 eyes, 11 men and 24 women) and a retropupillary iris-claw IOL (75 eyes, 27 men and 48 women).
Table 1 shows the procedures for surgical management of late IOL dislocation, IOL exchange procedures, or aphakia. The most frequent indications were exchange procedures or aphakia correction with retropupillary iris-claw IOL (45.5%) and repositioning procedures with scleral suturing (21.2%).
 |
Table 1 Surgical Management of Late IOL Dislocation, IOL Exchange Procedures, or Aphakia |
The mean age for the scleral suturing group was 81.8 years ±7.0 (SD); range 61–93 years and in the iris-claw group 77.7 years ±9.3 (SD); range 46–94 years. The scleral suturing group was significantly older than the iris-claw group (p=0.021) with no significant difference in gender (p=0.639). Women were overrepresented in both groups (Table 2).
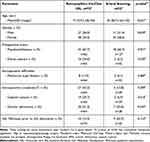 |
Table 2 Demographic Characteristics, Preoperative Findings, Intraoperative Difficulties, and Intra-/Postoperative Complications at the Primary Cataract Extraction |
In Table 2, significant differences in preoperative status and intraoperative difficulties in primary cataract extraction are demonstrated between the iris-claw group and the scleral suturing group. There was a higher rate of dense cataract (16 eyes [24.6%]) (p=0.030) and a higher rate of posterior capsular rupture (19 eyes [29.7%]) (p=0.016) in iris-claw patients. There were only two eyes (6.3%) with dense cataract and two eyes (6.9%) with posterior capsular rupture in the scleral suturing group.
There were no statistically significant differences in PEX, intraoperative mechanical pupil dilation, or Nd: YAG-laser before IOL dislocation between groups (Table 2).
All eyes in the scleral suturing group had an IOL dislocation (100%). In the iris-claw group, 23 eyes (30.7%) were aphakic after complicated cataract surgery with capsular rupture and vitrectomy and 52 eyes (69.3%) had IOL dislocation (p<0.001) (Table 3).
 |
Table 3 Preoperative Status Prior to IOL Correction Surgery and Additional Surgical Procedures Performed During the IOL-Repositioning/Exchange Procedure |
No intraoperative complications occurred in any eyes during the repositioning/exchange procedure, but a significantly higher rate of vitrectomy was performed in the iris-claw group (65.3%) than in the scleral suturing group (5.7%), (p<0.001) (Table 3).
Table 4 shows the postoperative outcomes after repositioning/IOL exchange surgery. There were significant differences between the two groups preoperatively, where the scleral suturing group had worse BCVA than the iris-claw group (p=0.002). However, there were no significant differences in postoperative BCVA (p=0.263) and both groups showed significant improvement, p<0.001. However, the improvement was significantly larger in the scleral suturing group (p=0.005).
 |
Table 4 Outcome After Repositioning/IOL Exchange Surgery |
Postoperative intraocular pressure decreased significantly in both groups, in the iris-claw group −2.1±6.9 mmHg (p=0.010) and in the scleral suturing group −3.7±6.5 (p=0.002), but this decrease did not differ significantly between groups (p=0.264).
Postoperative complications were few, including two cases of retinal detachment (2.7%) and one case of choroidal detachment (1.4%) in the iris-claw group, but none in the scleral suturing group (p=0.574). In addition, one patient in the iris-claw group experienced deterioration of a preexisting glaucoma. No cases of cystoid macular edema (CME) were observed in either of the groups.
Discussion
In the absence of adequate capsular support, the surgical management of dislocated IOL or aphakia can be a challenge. Several surgical procedures have been described.4,6–8 Each technique has advantages and disadvantages. Management decisions depend on the clinical features of each individual case and the surgeon’s preferences.1,2,4,9,10 If the IOL capsule complex is behind the pupillary area, the IOL can be repositioned or exchanged depending on clinic tradition. In our clinic, these patients are managed by cataract surgeons, whereas posterior segment surgeons may manage such patients in other clinical settings. Implantation of iris-claw and scleral-fixated IOL are the two most common surgical methods for correction of IOL dislocations or aphakia without adequate capsular support of the posterior capsule.1–3,11
This study compared 110 eyes managed by either scleral suturing (21.1%) or by obtaining a retropupillary iris-claw IOL (45.2%). The present retrospective study was non-randomized and as such, patients in this study were significantly older in the scleral suturing group; 81.8± 7.0 years (61–93) compared to the iris-claw group; 77.7±9.3 years (46–94) (p=0.021). In the study by Hazar et al,4 the mean age for patients at the time of repositioning/exchange was equivalent in both groups with no significant difference (p=0.89). Kristianslund et al1 also had the same mean age in both groups but with an older population in general.
A dense cataract is a risk indicator for PCR, vitrectomy, and aphakia.12,13 In cases with a large PCR and no capsular support, iris-claw IOL implantation was chosen. Patients with late IOL dislocation, who had a capsular tension ring or a three-piece IOL, were chosen for correction with scleral suturing of the preexisting IOL. This may explain why this study showed a significantly higher rate of PCR, dense cataract, vitrectomy, and aphakia in the primary cataract surgery data of iris-claw cases. However, there were no statistical differences between the two groups regarding intraoperative difficulties or complications during the secondary IOL-repositioning/exchange procedure.
Cataract is more common in women than men14 which reflects in postoperative cataract surgery status, such as dislocated IOL or aphakia. Women were overrepresented in both groups in our study, but no statistically significant difference in gender proportions was seen between the two groups.
Previous studies have reported that pseudoexfoliation (PEX) syndrome is an important risk factor for late in-the-bag dislocation or perioperative difficulties, such as poor pupil dilation, capsular tear, zonular dialysis, or vitreous loss.9,15–20 Medical records from primary cataract extraction in our study show that more than 66% of patients who needed repositioning or exchange of IOL had PEX without any statistically significant differences between the two groups.
Previous studies have shown shorter mean surgical time, shorter learning course, and easier technique for iris-claw compared to scleral fixation of PC-IOL in the absence of capsular support.1,11,21 Correction of aphakia with iris-claw was chosen in our study as it is an easier technique with a shorter learning curve compared to scleral fixation.
Several studies have confirmed that late in-the-bag dislocated IOL is the most frequent indication for IOL exchange or repositioning.22,23 Our study supports these earlier studies, 70% dislocated IOL in the iris-claw and 100% in the scleral suturing group. If the patient had received a three-piece IOL during primary cataract surgery, then the first choice of correction was scleral suturing of PC-IOL. If the patient had a one-piece IOL, exchange to iris-claw was chosen.
The overall mean interval between initial cataract surgery and second management was 7.8 years with a broad range from 2 weeks up to 54 years in our study. This broad range can result from retrospective, non-randomized study design that includes all cases with the need for secondary management of aphakia or dislocated IOL. No statistically significant difference was shown between the two groups, as is similar to previous studies.16,17,24
There were no intraoperative complications during repositioning/exchange surgery in any eyes in both groups. A significantly higher rate of vitrectomy was performed in cases with IOL exchange or secondary IOL implantation of iris-claw. This can be explained by different surgical methods between the two groups. The whole IOL-capsule complex was explanted through the anterior chamber in IOL exchange cases. This may break the anterior hyaloid membrane and cause vitreous prolapse with the need for vitrectomy. In cases with aphakia after complicated cataract surgery, there is a higher risk of vitreous prolapse. The risk is less in the scleral suturing group as the removal of the IOL-capsule complex is not needed and only cases with spontaneous vitreous prolapse require vitrectomy.
The rate of postoperative retinal detachment in previous studies varies from 3% to 8.2%.11,18,25,26 In our study, we had only one case of choroidal detachment (1.4%) 4 days after surgery and two cases of retinal detachment (2.7%) 2 weeks after IOL exchange in the iris-claw group, but none in the scleral suturing group with no statistically significant differences between the two groups. Despite having 110 patients in this study, the numbers were relatively small, which is a limitation. Within this group of patients, each complication is relatively rare and may not be easily estimated in a small group. Nonetheless, this retrospective two-group comparison can provide useful information and show a rate comparable to previous studies.11,18,25,26
Postoperative intraocular pressure decreased significantly in both groups, which is in line with other studies,7,18,25,27 and although the decrease was more pronounced in the scleral suturing group, this difference was non-significant. The majority of the aphakia cases resulted after complications during cataract surgery and in most cases, surgery was combined with an anterior vitrectomy procedure resulting in decreased IOP preoperatively before secondary IOL implantation. In contrast, IOL dislocation may cause increased IOP because of anatomical alterations18 preoperatively before scleral suturing. An IOL repositioning may lead to anatomical correction and cause decreased IOP. This may have resulted in significant differences between pre- and postoperative data in the scleral suturing group compared with the iris-claw group.
There were a few cases of persistent postoperative inflammation and persistent corneal edema and no statistically significant differences between the two groups. It is, however, important to decipher if the postoperative inflammation is a true inflammatory reaction or due to the mechanical trauma inflicted by the iris-claw. Furthermore, there were no statistically significant differences in postoperative BCVA between the two groups, with both groups experiencing a significant improvement in BCVA.
Although both surgeons had experience of scleral suturing and started with iris-claw implantation in 2010, no statistically significant difference in complications was shown between these two methods during the study period. Despite no data for comparison of the surgical procedure time required for iris-claw implantation and scleral suturing, there was an evident trend that surgeons implanted more iris-claw and performed less scleral suturing during the study period 2010–2014. Indeed, it is possible that the surgeons preferred the shorter surgical procedure time, which may have compounded the popularity of this technique. In 2014, the iris-claw implantation was the only type for correction in both aphakia and IOL dislocation. None of the IOL dislocations were sclerally sutured. This trend has continued after 2014 with most patients being subjected to iris-claw implantation in both aphakia and IOL dislocation. One explanation may be that a cataract surgeon who has learned and mastered iris-claw implantation may prefer shorter surgery time and reduced complexity that this technique offers, particularly in a local hospital setting without access to retinal surgeons. Another reason for preferring iris-claw implantation over scleral suturing is the limited lifespan of sutures in scleral suturing, which degrade over time, hence resulting in IOL redislocation and the need for reoperation. From an economic perspective, scleral suturing is less costly when only taking account of the material, that is, suture material compared to the iris-claw IOLs. However, given the shorter surgical time for the iris-claw technique and the high cost of surgical theatre time, the latter technique may be beneficial also from an economical perspective.
In this retrospective study, further study limitations include the inability to randomize patients and the small number of patients in each group, which has resulted in some unavoidable statistical differences between the two study groups. The scleral suturing group was significantly older than the iris-claw group and had significantly lower preoperative BCVA. Furthermore, the surgeon may be biased due to patients’ clinical status and history. However, only two surgeons performed all surgeries, hence thoroughly standardizing the procedure. Surgical complications were relatively rare in this group of patients and are thus not easily evaluated in such a small subpopulation. Follow-up duration varied with 57% of the cases having more than 1 month of follow-up, 32% more than 3 months of follow-up, and in some cases even longer follow-up. This limits the ability to monitor long-term postoperative complications warranting further research.
Conclusion
This study shows that both dislocated IOL and aphakia correction surgical procedures are safe and effective with limited complications. Significant improvement in visual acuity was shown in both groups. Most patients had pseudoexfoliations and IOP decreased in both groups.
As the rate of cataract surgery and the age of pseudophakic population around the world continues to increase, the rate of surgical management for IOL dislocation and aphakia correction will also continue to increase. A simple procedure with a shorter learning curve and shorter surgery time is desirable, which is possible to perform even by a cataract surgeon. However, the decision ultimately depends on surgeons’ comfort and experience with the procedure.
Acknowledgments
This work was supported by grants from the Swedish state under the agreement between the Swedish government and the county councils, the ALF agreement (ALF-GBG-725041 and 966230). The Göteborg Medical Society, Hjalmar Svensson Foundation, Greta Andersson Foundation, Herman Svensson Foundation, De Blindas vänner, Agneta Prytz-Folkes och Gösta Folkes stiftelse, and Kronprinsessans Margaretas Arbetsnämnd för Synskadade.
This work was presented as a poster at the ESCRS Annual meeting, Vienna, September 2018.
Disclosure
None of the authors has a financial or proprietary interest in any material or method mentioned. The authors report no conflicts of interest in this work.
References
1. Kristianslund O, Råen M, Østern AE, Drolsum L. Late in-the-bag intraocular lens dislocation: a randomized clinical trial comparing lens repositioning and lens exchange. Ophthalmology. 2017;124(2):151–159. doi:10.1016/j.ophtha.2016.10.024
2. Kim SS, Smiddy W, Feuer W, Shi W. Management of dislocated intraocular lenses. Ophthalmology. 2008;115(10):1699–1704. doi:10.1016/j.ophtha.2008.04.016
3. Acar N, Kapran Z, Altan T, Kucuksumer Y, Unver YB, Polat E. Secondary iris claw intraocular lens implantation for the correction of aphakia after pars plana vitrectomy. Retina. 2010;30(1):131–139. doi:10.1097/IAE.0b013e3181b32eef
4. Hazar L, Kara N, Bozkurt E, Ozgurhan EB, Demirok A. Intraocular lens implantation procedures in aphakic eyes with insufficient capsular support associated with previous cataract surgery. J Refract Surg. 2013;29(10):685–691. doi:10.3928/1081597x-20130723-02
5. Canabrava S, Canêdo domingos lima AC, Ribeiro G. Four-flanged intrascleral intraocular lens fixation technique: no flaps, no knots, no glue. Cornea. 2020;39(4):527–528. doi:10.1097/ico.0000000000002185
6. Touriño Peralba R, Lamas-Francis D, Sarandeses-Diez T, Martínez-Pérez L, Rodríguez-Ares T. Iris-claw intraocular lens for aphakia: can location influence the final outcomes? J Cataract Refract Surg. 2018;44(7):818–826. doi:10.1016/j.jcrs.2018.05.010
7. Gonnermann J, Klamann MKJ, Maier A-K, et al. Visual outcome and complications after posterior iris-claw aphakic intraocular lens implantation. J Cataract Refract Surg. 2012;38(12):2139–2143. doi:10.1016/j.jcrs.2012.07.035
8. Wagoner MD, Cox TA, Ariyasu RG, Jacobs DS, Karp CL. Intraocular lens implantation in the absence of capsular support: a report by the American Academy of ophthalmology. Ophthalmology. 2003;110(4):840–859. doi:10.1016/s0161-6420(02)02000-6
9. Dabrowska-Kloda K, Kloda T, Boudiaf S, Jakobsson G, Stenevi U. Incidence and risk factors of late in-The-bag intraocular lens dislocation: evaluation of 140 eyes between 1992 and 2012. J Cataract Refract Surg. 2015;41(7):1376–1382. doi:10.1016/j.jcrs.2014.10.040
10. Fernández-Buenaga R, Alio JL, Pérez-Ardoy AL, et al. Late in-The-bag intraocular lens dislocation requiring explantation: risk factors and outcomes. Eye. 2013;27(7):795–801; quiz 802. doi:10.1038/eye.2013.95
11. Jing W, Guanlu L, Qianyin Z, et al. Iris-claw intraocular lens and scleral-fixated posterior chamber intraocular lens implantations in correcting aphakia: a meta-analysis. Invest Ophthalmol Vis Sci. 2017;58(9):3530–3536. doi:10.1167/iovs.16-21226
12. Artzén D, Lundström M, Behndig A, Stenevi U, Lydahl E, Montan P. Capsule complication during cataract surgery: case-control study of preoperative and intraoperative risk factors: Swedish capsule rupture study group report 2. J Cataract Refract Surg. 2009;35(10):1688–1693. doi:10.1016/j.jcrs.2009.05.026
13. Johansson B, Lundström M, Montan P, Stenevi U, Behndig A. Capsule complication during cataract surgery: long-term outcomes: Swedish capsule rupture study group report 3. J Cataract Refract Surg. 2009;35(10):1694–1698. doi:10.1016/j.jcrs.2009.05.027
14. Zetterberg M, Celojevic D. Gender and cataract--The role of estrogen. Curr Eye Res. 2015;40(2):176–190. doi:10.3109/02713683.2014.898774
15. Fujikawa A, Mohamed YH, Kinoshita H, Tsuiki E, Kitaoka T. Spontaneous dislocation of the posterior chamber intraocular lens. Int Ophthalmol. 2018;38(3):1111–1117. doi:10.1007/s10792-017-0567-6
16. Davis D, Brubaker J, Espandar L, et al. Late in-The-bag spontaneous intraocular lens dislocation: evaluation of 86 consecutive cases. Ophthalmology. 2009;116(4):664–670. doi:10.1016/j.ophtha.2008.11.018
17. Jakobsson G, Zetterberg M, Lundström M, Stenevi U, Grenmark R, Sundelin K. Late dislocation of in-The-bag and out-of-The bag intraocular lenses: ocular and surgical characteristics and time to lens repositioning. J Cataract Refract Surg. 2010;36(10):1637–1644. doi:10.1016/j.jcrs.2010.04.042
18. Jakobsson G, Zetterberg M, Sundelin K, Stenevi U. Surgical repositioning of intraocular lenses after late dislocation: complications, effect on intraocular pressure, and visual outcomes. J Cataract Refract Surg. 2013;39(12):1879–1885. doi:10.1016/j.jcrs.2013.06.023
19. Gross JG, Kokame GT, Weinberg DV. In-The-bag intraocular lens dislocation. Am J Ophthalmol. 2004;137(4):630–635. doi:10.1016/j.ajo.2003.10.037
20. Jehan FS, Mamalis N, Crandall AS. Spontaneous late dislocation of intraocular lens within the capsular bag in pseudoexfoliation patients. Ophthalmology. 2001;108(10):1727–1731. doi:10.1016/s0161-6420(01)00710-2
21. Farrahi F, Feghhi M, Haghi F, Kasiri A, Afkari A, Latifi M. Iris claw versus scleral fixation intraocular lens implantation during pars plana vitrectomy. J Ophthalmic Vis Res. 2012;7(2):118–124.
22. Davies EC, Pineda R. Intraocular lens exchange surgery at a tertiary referral center: indications, complications, and visual outcomes. J Cataract Refract Surg. 2016;42(9):1262–1267. doi:10.1016/j.jcrs.2016.06.031
23. Gimbel HV, Condon GP, Kohnen T, Olson RJ, Halkiadakis I. Late in-The-bag intraocular lens dislocation: incidence, prevention, and management. J Cataract Refract Surg. 2005;31(11):2193–2204. doi:10.1016/j.jcrs.2005.06.053
24. Mönestam EI. Incidence of dislocation of intraocular lenses and pseudophakodonesis 10 years after cataract surgery. Ophthalmology. 2009;116(12):2315–2320. doi:10.1016/j.ophtha.2009.05.015
25. Bading G, Hillenkamp J, Sachs HG, Gabel VP, Framme C. Long-term safety and functional outcome of combined pars plana vitrectomy and scleral-fixated sutured posterior chamber lens implantation. Am J Ophthalmol. 2007;144(3):371–377. doi:10.1016/j.ajo.2007.05.014
26. Vote BJ, Tranos P, Bunce C, Charteris DG, Da Cruz L. Long-term outcome of combined pars plana vitrectomy and scleral fixated sutured posterior chamber intraocular lens implantation. Am J Ophthalmol. 2006;141(2):308–312. doi:10.1016/j.ajo.2005.09.012
27. Kristianslund O, Råen M, Østern AE, Drolsum L. Glaucoma and intraocular pressure in patients operated for late in-the-bag intraocular lens dislocation: a randomized clinical trial. Am J Ophthalmol. 2017;176:219–227. doi:10.1016/j.ajo.2017.01.026
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
