Back to Journals » Clinical Ophthalmology » Volume 15
Visual and Refractive Outcomes and Patient Satisfaction Following Implantation of Monofocal IOL in One Eye and ERV IOL in the Contralateral Eye with Mini-Monovision
Authors Brar S , Ganesh S , Arra RR, Sute SS
Received 22 September 2020
Accepted for publication 4 December 2020
Published 4 May 2021 Volume 2021:15 Pages 1839—1849
DOI https://doi.org/10.2147/OPTH.S278648
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Sheetal Brar, Sri Ganesh, Raghavender Reddy Arra, Smith Snehal Sute
Department of Phaco-Refractive Surgery, Nethradhama Super Speciality Eye Hospital, Bangalore, Karnataka, India
Correspondence: Sheetal Brar
Nethradhama Super Speciality Eye Hospital, 256/14, Kanakapura Main Road, 7th Block, Jayanagar, Bengaluru, Karnataka, 560070, India
Tel +91 9591002092
Email [email protected]
Title: Visual and refractive outcomes and patient satisfaction following implantation of monofocal intraocular lens in one eye and ERV intraocular lens in the contralateral eye with mini-monovision.
Purpose: To evaluate the outcomes following implantation of monofocal intraocular lens in one eye and ERV intraocular lens in the contralateral eye with mini-monovision.
Methods: Twenty-five subjects underwent bilateral cataract surgery, wherein the dominant eye received monofocal Tecnis-1 IOL, while in the contralateral eye received the Tecnis Symphony ERV IOL. The dominant eye was targeted for emmetropia and the non-dominant eye for myopia of − 0.50 to − 0.75D. Binocular uncorrected and corrected distance (UDVA, CDVA), intermediate (UIVA, CIVA), and near (UNVA, DCNVA) visual acuity; reading speeds, defocus curve and contrast sensitivity were studied at 6 months post-operatively.
Results: At 6 months post-operatively the mean binocular UDVA, CDVA, UNVA and DCNVA were 0.007± 0.07, − 0.13± 0.06, 0.26± 0.09 and 0.44± 0.10 LogMAR, respectively. Binocular UIVA and DCIVA at 60 cm were 0.22± 0.10 and 0.18± 0.08 LogMAR and at 80 cm was 0.16± 0.11 and 0.15± 0.10 LogMAR, respectively. Mean uncorrected reading speeds evaluated with SRD at 40, 60 and 80 cm were 114.4± 6.9, 126.4± 7.9 and 123.16± 5.8 words per minute. Contrast sensitivity values did not show significant difference for any spatial frequency tested. At 6 months, only 12% (3 patients) reported mild halos. Spectacle independence satisfaction scores were 96%, 100% and 88% for distance, intermediate and near.
Conclusion: Implantation of monofocal intraocular lens in one eye and ERV intraocular lens in the contralateral with mini-monovision resulted in good outcomes for far and intermediate, and satisfactory outcomes for near vision, with good tolerance to mini-monovision at the end of 6 months.
Keywords: hybrid monovision, extended range of vision IOL, monofocal IOL
Introduction
Multifocal IOLs are known to provide better outcomes for near and intermediate vision, and a greater depth of focus; due to which they appear to deliver higher spectacle independence and patient satisfaction compared to monofocal IOLs.1,2 Due to these advantages, various varieties of MFIOLs have been paired with monofocal intraocular lenses to restore the loss of accommodation following cataract surgery, especially in patients who already have a monofocal implant in one eye. The concept of “Hybrid monovision” wherein a monofocal IOL was implanted in the dominant eye and a diffractive multifocal IOL in the non-dominant eye was shown to provide superior outcomes in terms of post-operative near vision and patient satisfaction following cataract surgery.3,4
The recently introduced Tecnis Symfony IOL (Johnson & Johnson, New Jersey, USA) is based on the concept of chromatic aberration correction through a proprietary achromatic technology. In addition, the IOL is claimed to extend the range of vision by virtue of its novel, diffractive step-like optical profile.5,6
The current study was conducted to evaluate the visual and refractive outcomes and patient satisfaction following planned “Hybrid monovision” with extended range of vision (ERV) IOLs, wherein a monofocal IOL was implanted in one eye and an ERV IOL in the contralateral eye, in a 6-month prospective clinical trial.
Methodology
This prospective, single-centre study was approved by the institutional review board of Nethradhama Super speciality Eye Hospital, Bangalore, and was conducted in accordance with the principles of the Declaration of Helsinki. Only those patients who provided written informed consent and whose follow-ups were assured were included.
Inclusion criteria were eyes with senile cataract without any ocular co-morbidity; corneal astigmatism within 0.5 dioptres (D); IOL powers within the range of +10.00 D and +32.00 D, uneventful surgery, and assured follow-ups.
Exclusion criteria were age outside the range of 40–80 years, eyes with irregular astigmatism due to keratoconus or corneal scars, previous history of refractive surgery, severe dry eye, corneal dystrophies, active conjunctivitis, glaucoma, uveitis, pupillary abnormalities, retinopathy or macular dystrophy, neuro-ophthalmic diseases, and inability to read English language fluently.
Pre-Operative Assessment and IOL Power Calculation
All patients underwent complete ophthalmic examination including subjective refraction, non-contact tonometry, and slit-lamp biomicroscopy and dilated fundus examination. Biometry was performed with the IOL Master 700 (Carl Zeiss Meditec, Jena, Germany) using the Barrett-II Universal formula. The dominance of the eyes was tested using the camera, shooting or hole in the card test. In all subjects, the dominant eye was targeted for emmetropia, whereas the non-dominant eye was targeted at myopia of −0.75 D. The dominant and the non-dominant eyes were planned for implantation of Tecnis-1 monofocal IOL and Tecnis Symfony IOL, respectively. In subjects, where clear dominance could not be identified, the eye with advanced cataract received Tecnis-1 monofocal IOL. For all cases, the Tecnis-1 monofocal eyes were planned first. Second eye surgery with Symfony ERV IOL was scheduled within 2 weeks from the first eye surgery. Patients were appropriately counselled about neuroadaptation due to dissimilar optical systems in both eyes.
Post-operative follow-ups were performed at 1 day, 1 week, 1 month, and 6 months post-surgery. The following tests were performed from the first week onwards: assessment of binocular uncorrected (UDVA) and corrected distance visual acuity (CDVA), binocular uncorrected (UNVA) and distance-corrected near visual acuity (DCNVA) at 40 cm, and binocular uncorrected (UIVA) and distance-corrected intermediate visual acuity (DCIVA) at 60 cm using ETDRS charts (Precision Vision, La Sella, IL, USA); binocular mesopic contrast sensitivity testing (F.A.C.T. Stereo Optical Co. Inc., Chicago) with distance correction; and defocus curve testing from +2.50 to −4.00 D.
Reading performance was evaluated using the Salzburg reading desk (SRD) (University Eye Clinic, Paracelsus Medical University of Salzburg, Austria) which provides for controlled reading distance and automated calculation of logarithmic reading acuity and the reading speeds. From one week onwards, and uncorrected (UCRS) and distance corrected reading speeds(DCRS) with a minimum reading speed of 80 words per minute (wpm), representing the lower limit for recreational sense-capturing reading, were evaluated.7 Also, a quality of vision (QOV) questionnaire was obtained at one and six months follow-ups regarding dysphotopsia symptoms and spectacle independence for various activities.8
Surgical Technique
All operations were performed by a single experienced cataract surgeon (S.G.), using a standard phacoemulsification technique (Phaco-chop) under topical anaesthesia. The UNFOLDER Platinum 1 Series Screw-Style Inserter (Johnson & Johnson, New Jersey, USA) was used to inject the IOL through a 2.8 mm temporal clear corneal incision for both the eyes. Post-operative medications included topical prednisolone (1%, Pred Forte, Allergan), moxifloxacin (0.5%, Vigamox, Alcon), and nepafenac (0.1%, Nevanac, Alcon) in tapering dosage for 6 weeks; along with lubricant eye drops on an SOS basis.
Statistical Analysis
Statistical analysis was performed using the SPSS software for Windows version 17.0.0 (IBM Corp., Armonk, NY). The normality of data samples was checked. Student’s t-test for paired data was used when parametric analysis was possible, whereas the Mann–Whitney test was applied to assess the significance of differences when parametric analysis was not possible. A p value of 0.05 or less was considered statistically significant. All values were expressed as mean ± standard deviation (SD).
Results
A total of 25 patients with a mean age of 64.76 ± 9.2 years, undergoing bilateral cataract surgery with Tecnis −1 monofocal IOL in one eye and Tecnis Symfony ERV IOL in the contralateral eye were recruited in the study. Table 1 provides the demographic and pre-operative data of all the study subjects. Since mini-monovision was performed, the post-operative visual outcomes and reading speeds were evaluated binocularly.
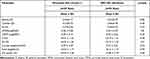 |
Table 1 Demographic and Pre-Operative Data of Patients Included in the Study |
Visual Outcomes
Table 2 shows the binocular visual outcomes for distance, near and intermediate visual acuity and reading speeds at 6 months post-operatively.
 |
Table 2 Binocular Visual Acuity Outcomes at 6 Months Post-Operatively |
At 6 months, 88% patients had binocular UDVA of 20/20 or better, whereas, all (100%) patients had a binocular UDVA of at least 20/32, (Figure 1). The binocular cumulative CDVA graph showed 92% of patients having 20/20 or better and 100% patients have CDVA of 20/32 or better (Figure 1). The mean UDVA in eyes with Tecnis-1 IOL was 0.04 ± 0.08 Log MAR, which was significantly better than eyes implanted with Symfony IOL (0.20 ±0.07 Log MAR), p= 0.00.
 |
Figure 1 Percentage binocular cumulative UDVA and CDVA for the monofocal and ERV groups, 6 months post-operatively. |
All patients had an uncorrected binocular near vision of 20/50; however, 8% of patients had a cumulative UNVA of 20/20 or better and 84% patients 20/32 or better (Figure 2). The UNVA in the ERV IOL eyes was significantly better compared to the monofocal eyes (LogMAR 0.21 ± 0.09 versus 0.47± 0.18), p=0.00.
 |
Figure 2 Percentage binocular uncorrected near visual acuity (UNVA), for the monofocal and ERV groups, 6 months post-operatively. |
The cumulative binocular UIVA of 20/40 or better was achieved in 100% and 96% patients at 60 and 80 cm, respectively. However, 43% of patients achieved UIVA of 20/25 or better at 60 cm, whereas this percentage was 65% at 80 cm (Figure 3). There was no statistically significant difference between the mean UIVA values at 60 and 80 cm (p =0.10) (Table 2).
 |
Figure 3 Percentage binocular uncorrected intermediate visual acuity (UIVA) @ 60 and 80 cm 6 months post-operatively. |
Refractive Outcome
The mean SE in the Tecnis −1 monofocal IOL group was −0.10 ±0.25 D, whereas in the Symfony ERV IOL group it was −0.79 ±0.31 D at six months post-operatively, the difference between the two being statistically significant (p= 0.00) (Table 3).
 |
Table 3 Uniocular Post-Operative Data |
Ninety-six percent of eyes in the monofocal group had post-op SE within ±0.50 D, and all eyes were within ± 1.00 D of SE predictability. On the other hand, in the ERV group, 16% eyes achieved post-op SE refraction within ±0.50 D, and all eyes were within ± 2.00 D of SE predictability (Figure 4).
 |
Figure 4 Post-operative spherical equivalent (SE) predictability for the Tecnis-1 monofocal and Symfony ERV groups, 6 months post-operatively. |
In the monofocal group, 88% percent eyes and in the ERV group 96% of eyes had post-operative refractive astigmatism within ±0.50 D. All eyes in both groups were within ± 1.00 D of cylindrical correction (Figure 5).
 |
Figure 5 Post-operative refractive astigmatism (dioptres) for the Tecnis-1 monofocal and Symfony ERV groups, 6 months post-operatively. |
Reading Speeds
Figure 6 shows the mean uncorrected and corrected reading speeds at 40, 60 and 80 cm, evaluated with the SRD. At 40 cm, the uncorrected reading speed was significantly better compared to corrected values (p-value=0.006), however, at 60 and 80 cm, no significant difference was observed between the uncorrected and corrected reading speeds (p-value =0.84 for 60 cm, 0.07 for 80 cm) (Table 2). The uncorrected reading speeds at 60cm and 80 cm were significantly better than at 40cm (p-value=0.00 for both comparisons), however, no significant difference was observed between the uncorrected reading speeds at 60 and 80cm (p-value=0.10) (Table 2)
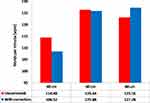 |
Figure 6 Reading speeds with Salzburg Reading Desk, for the Tecnis-1 monofocal and Symfony ERV groups, 6 months post-operatively. |
Contrast Sensitivity
Table 3 shows the mean contrast sensitivity values for Tecnis-1 monofocal and Symfony ERV IOL groups, measured after correction, using the F.A.C.T. chart in photopic conditions at 6 months post-operatively. The results did not show significant difference for any of the spatial frequencies evaluated (Table 3, Figure 7).
 |
Figure 7 Binocular photopic contrast sensitivity for Tecnis-1 monofocal and Symfony ERV groups at 6 months post-operatively. |
Defocus Curve
Binocular distance corrected defocus curves were charted from +1 to −4 D defocusing lenses, for all patients at 6 months. The curve showed a peak corresponding to best visual acuity at 0 D, followed by a gradual decline in best-corrected vision towards the myopic range. The curve was relatively smoother without any distinct multiple peaks thereafter (Figure 8). The range of functional vision, ie a visual acuity of 0.2 LogMAR (20/32) or better was seen to be spread over a defocus range of approximately 3.0 D.
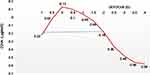 |
Figure 8 Defocus curves, y-axis= CDVA logMAR, x axes= level of defocus in dioptres for the Tecnis-1 monofocal and Symfony ERV groups. |
Patient Satisfaction Questionnaire
A QOV questionnaire which graded glare, haloes and starbursts on a score of 1–4 for each symptom (overall score 12, 1 being the highest and 4 being the lowest in severity) obtained at 1 and 6 months, showed 50% (12/25) patients complaining of mild to moderate haloes at 1 month, which reduced to 12% (3/25) of patients, reporting only mild haloes by the end of 6 months. No patient reported severe haloes post-operatively at any time point. Regarding spectacle independence; satisfaction scores were 96% (24/25), 100%, 80% (20/25) for distance, intermediate and near vision, respectively. Twelve percent (3/25) of patients reported the need for reading glasses for fine print at 6 months (Table 4).
 |
Table 4 QOV Questionnaire for Dysphotopsia Symptoms Grading and Spectacle Independence |
Adverse Effects and Complications
No intra-operative or post-operative complications such as cystoid macular oedema, post-op uveitis, secondary glaucoma or posterior capsule opacification requiring YAG- Capsulotomy were noted in any of the eyes of either group.
Discussion
The extended range of vision IOL evaluated in the current study has been shown to provide visual restoration which is better or comparable to that achievable with a multifocal IOL, but without the known level of visual degradation associated with this type of IOL. This can be possibly explained by the fact that the extended range of vision IOL does not induce aberrations or multiple foci to achieve depth of focus. Also, the correction of chromatic corneal aberration together with the specific diffractive pattern generates an extended range of clear vision.9,10 The objective of this study was to assess clinical outcomes, quality of vision and patient satisfaction with an intentional planning of a monofocal IOL in one eye and an ERV IOL in the contralateral eye. As a significant number of patients presenting for cataract surgery opinion already have one eye operated elsewhere with a monofocal implant, the acceptability of this combination was an interesting area to explore.
Studies comparing trifocal IOLs such as the Acrysof IQ PanOptix and Finevision trifocal IOLs, with the Symfony ERV IOL, clearly demonstrated significantly better near vision with trifocal IOLs.11,12 Hence, while planning hybrid monovision with ERV IOL, it becomes mandatory to target the non-dominant eye for slight myopia of −0.5 to −0.75 D, provided the monofocal eye is emmetropic; thus creating a mini-monovision. In a recent study by Cochener et al, where a sub-analysis of 411 patients from the multicenter CONCERTO study was performed aiming at evaluating the outcomes after bilateral implantation of the Tecnis Symfony IOL. In the study, visual acuity, spectacle independence, photic phenomena incidence, and patient satisfaction outcomes were evaluated in six groups defined according to the level of monovision: ranging from 0 to >1.0 D. The authors concluded that mini-monovision of around 0.75 D provided a complete visual rehabilitation with minimal photic phenomena and high levels of patient satisfaction after implantation of the Tecnis Symfony IOL.13 Besides good visual and spectacle independence outcomes, monovision levels of around 0.75 D were also found to provide low incidence of halos and glare, with 88.5% and 96.2%, respectively, not reporting them at all or reporting only occasionally. This incidence is minimal compared to the dissatisfaction rates and patient complaints due to these phenomena observed with multifocal IOLs.
It is a known fact that traditional MFIOL technologies can be associated with bothersome dysphotopsias, accounting up to 38.2% of the various causes of patient dissatisfaction following MFIOL implantation.14 Mini-monovision has been shown to be an effective approach for both reducing spectacle independence as well as dysphotopsia, which were found to be significantly less compared to multifocal intraocular lens implantation.15,16 Since Tecnis Symfony ERV IOL has been shown to result in fewer dysphotopsia symptoms compared to traditional MFIOLs,17 its combination with monofocal IOL in the contralateral eye, would theoretically result in further reducing the photic phenomena, potentially improving the tolerance and patient acceptability.
In contrast to our results with binocular implantation of Symfony ERV IOL,8 wherein 32% (8/25) of the patients had complaints of seeing moderate-to-severe halos at night; in the present study, only 12% (3/25) patients reported halos and glare of mild grade; while in the rest of the 22 patients, these symptoms had completely resolved by the end of six months. Surprisingly, the dysphotopsia symptoms were low despite the monovision, suggesting that patients may adapt to hybrid monovision better compared to traditional monovision practiced with bilateral ERV IOLs, since the dominant eye; which is aimed for distance, does not additionally contribute to dysphotopsia, resulting in better acceptability.
Pseudophakia monovision with monofocal IOLs is a tried and tested strategy to restore the loss of accommodation post-cataract surgery. However, to achieve satisfactory near vision, one needs to perform traditional monovision, ie anisometropia of −1.50 D or above, which may be associated with various side effects and reduced patient satisfaction.18,19 The advantage of hybrid monovision with ERV IOLs is that good near vision outcomes may be achieved by performing mini-monovision, thus avoiding most of the bothersome disadvantages of the traditional monovision.
A study by Cochener et al compared defocus curves of trifocal IOLs versus EDOF IOL, wherein with trifocal lenses, slight humps at the principal foci could be identified, however, the curve achieved with the EDOF Tecnis Symfony IOL was smoother in the shape of a dome.20 In the present study also, we found the binocular distance corrected defocus curves showing a relatively smoother and dome shaped (Figure 8). The range of functional vision, ie visual acuity of 20/32 or better, was seen to be spread over a defocus range of approximately 3.5 D; which was similar to those seen in both the above studies.
Regarding contrast sensitivity, we found no significant differences for any spatial frequency between monofocal and ERV IOL at 6 months post-op. This is in agreement with previously conducted studies wherein the contrast for both monofocal and Symfony ERV IOL was comparable.9 Especially in context to the present study, where the monofocal IOL implanted was the aspheric and chromatic aberration correcting Tecnis-1 IOL; which is already shown to deliver excellent contrast after cataract surgery.21 Both the IOLs, being manufactured on the same platform, when implanted together in contralateral eyes result in excellent quality of vision post-op.
Various studies have evaluated reading performance after MFIOLs following cataract surgery using Salzburg Reading Desk (SRD), which is a tool for systematic evaluation of everyday reading ability simulating natural conditions.22,23 Alio et al, in their study evaluating the reading performance following Acri.LISA 366D diffractive multifocal IOL,24 found that the average uncorrected reading speed at near (32.51 cm) was 117.7 words per minute(wpm). In our study, the average reading speeds at 40 cm was 114.48 wpm, which is almost similar to their study. Furthermore, we tested the reading speeds at distances of 60 cm and 80 cm, to see the performance of hybrid monovision for the complete range of near and intermediate vision. Compared to our previous study evaluating reading performance following bilateral Tecnis Symfony with mini-monovision,8 the reading speeds at 60 and 80 cm in the present study were found to be better, the mean reading speed at 60 cm being 126 versus 119 wpm and at 80 cm being 123 versus 115 wpm. A similar observation was noticed for reading speeds at 80 cm in a study by Attia et al.25 This could be possibly explained by the fact that bilateral implantation of Tecnis Symfony IOL in both these studies could have resulted in higher amount of glare and dysphotopsia arising from the screen while performing the test, thus potentially affecting the reading speed.
In the present study, we did not strictly follow the criteria for hybrid monovision, with respect to the dominance of the eye. In some patients, where the dominance of the eye could not be confirmed due to poor vision in one of the eyes, we decided to implant Tecnis-1 monofocal IOL in the eye with an advanced grade of cataract and Symfony ERV IOL in the contralateral eye. This does not have seem to make any difference in the outcomes, as it was shown in the earlier published studies that patient satisfaction as well as the visual results of crossed monovision were no different from conventional monovision.26–28
Conclusion
To our knowledge, this is the first study reporting clinical outcomes following hybrid monovision using ERV IOLs along with monofocal IOL in the contralateral eyes of the same patient. Although our sample size is small and follow-up relatively shorter, our results showed satisfactory visual outcomes for far, intermediate and near distances, with good patient satisfaction for the quality of vision and spectacle independence. This combination may be offered to patients who already have a monofocal implant in one eye (with minimum residual refraction) or may also be planned intentionally; as done in the present study.
Although we did not perform a direct comparison with a group where hybrid monovision was performed using a diffractive MFIOL, however, understanding the advantages of ERV IOL technology (better contrast, less photic phenomena, tolerance to residual refractive error) it may be suggested that these IOLs may be preferred over traditional MFIOLs for mix and match with monofocal IOLs. Further studies evaluating the results of hybrid monovision using ERV IOLs and their comparison with MFIOLs in a similar scenario are suggested to verify the results and inferences drawn from our paper.
Disclosure
The study was supported by an unrestricted grant from Johnson & Johnson Vision. However, none of the authors have any financial or proprietary interest in a product, method, or material described herein. Dr Sri Ganesh reports grants from Johnson & Johnson Vision, during the conduct of the study. The authors report no other potential conflicts of interest for this work.
This paper was presented at the ASCRS Conference at Washington DC, in 2018, as a free paper presentation with interim findings. The presentation link can be found here:
https://ascrs.confex.com/ascrs/18am/meetingapp.cgi/Paper/41301.
References
1. Salerno LC, Tiveron MC, Alió JL. Multifocal intraocular lenses: types, outcomes, complications and how to solve them. Taiwan J Ophthalmol. 2017;7(4):179–184. doi:10.4103/tjo.tjo_19_17
2. Rosen E, Alió JL, Dick HB, Dell S, Slade S. Efficacy and safety of multifocal intraocular lenses following cataract and refractive lens exchange: metaanalysis of peer-reviewed publications. J Cataract Refract Surg. 2016;42:310–328. doi:10.1016/j.jcrs.2016.01.014
3. Studený P, Kacerovský M, Kacerovská J, Gajarová N, Straňák Z. Hybridní monovision [Hybrid monovision]. Cesk Slov Oftalmol. 2017;73(1):13–16.
4. Iida Y, Shimizu K, Ito M. Pseudophakic monovision using monofocal and multifocal intraocular lenses: hybrid monovision. J Cataract Refract Surg. 2011;37(11):2001–2005. doi:10.1016/j.jcrs.2011.05.032
5. Akella SS, Juthani VV. Extended depth of focus intraocular lenses for presbyopia. Curr Opin Ophthalmol. 2018;29(4):318–322. doi:10.1097/ICU.0000000000000490
6. Breyer DRH, Kaymak H, Ax T, Kretz FTA, Auffarth GU, Hagen PR. Multifocal intraocular lenses and extended depth of focus intraocular lenses. Asia Pac J Ophthalmol (Phila). 2017;6(4):339–349. doi:10.22608/APO.2017186
7. Dexl AK. Einsatz des Salzburg Reading Desk für die Presbyopie- und Akkommodationsforschung [Application of the Salzburg reading desk in accommodation and presbyopic research]. Klin Monbl Augenheilkd. 2011;228(8):676–680. [Article in German]. doi:10.1055/s-0031-1281619
8. Ganesh S, Brar S, Pawar A, Relekar KJ. Visual and refractive outcomes following bilateral implantation of extended range of vision intraocular lens with micromonovision. J Ophthalmol. 2018;2018:7321794. doi:10.1155/2018/7321794
9. Pedrotti E, Bruni E, Bonacci E, Badalamenti R, Mastropasqua R, Marchini G. Comparative analysis of the clinical outcomes with a monofocal and an extended range of vision intraocular lens. J Refract Surg. 2016;32:436–442. doi:10.3928/1081597X-20160428-06
10. Millán MS, Vega F. Extended depth of focus intraocular lens: chromatic performance. Biomed Opt Express. 2017;8(9):4294–4309. doi:10.1364/BOE.8.004294
11. Monaco G, Gari M, DiCenso F, Poscia A, Ruggi G, Scialdone A. Visual performance after bilateral implantation of 2 new presbyopia-correcting intraocular lenses: trifocal versus extended range of vision. J Cataract Refract Surg. 2017;43:737–747. doi:10.1016/j.jcrs.2017.03.037
12. Sheppard AL, Shah S, Bhatt U, Bhogal G, Wolffsohn JS. Visual outcomes and subjective experience after bilateral implantation of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2013;39:343–349. doi:10.1016/j.jcrs.2012.09.017
13. Cochener B. Influence of the level of monovision on visual outcome with an extended range of vision intraocular lens. Clin Ophthalmol. 2018;12:2305–2312. doi:10.2147/OPTH.S184712
14. de Vries NE, Webers CA, Touwslager WR, et al. Dissatisfaction after implantation of multifocal intraocular lenses. J Cataract Refract Surg. 2011;37(5):859–865. doi:10.1016/j.jcrs.2010.11.032
15. Labiris G, Giarmoukakis A, Patsiamanidi M, Papadopoulos Z, Kozobolis VP. Mini-monovision versus multifocal intraocular lens implantation. J Cataract Refract Surg. 2015;41(1):53–57. doi:10.1016/j.jcrs.2014.06.015
16. Goldberg DG, Goldberg MH, Shah R, Meagher JN, Ailani H. Pseudophakic mini-monovision: high patient satisfaction, reduced spectacle dependence, and low cost. BMC Ophthalmol. 2018;18(1):293. doi:10.1186/s12886-018-0963-3
17. Giers BC, Khoramnia R, Varadi D, et al. Functional results and photic phenomena with new extended-depth-of-focus intraocular lens. BMC Ophthalmol. 2019;19(1):197. doi:10.1186/s12886-019-1201-3
18. Xiao J, Jiang C, Zhang M. Pseudophakic monovision is an important surgical approach to being spectacle-free. Indian J Ophthalmol. 2011;59(6):481–485. doi:10.4103/0301-4738.86318
19. Kelava L, Barić H, Bušić M, Čima I, Trkulja V. Monovision versus multifocality for presbyopia: systematic review and meta-analysis of randomized controlled trials. Adv Ther. 2017;34(8):1815–1839. doi:10.1007/s12325-017-0579-7
20. Cochener B, Boutillier G, Lamard M, et al. A comparative evaluation of a new generation of diffractive trifocal and extended depth of focus intraocular lenses. J Refract Surg. 2018;34(8):507–514. doi:10.3928/1081597X-20180530-02
21. Wahba SS, Riad RF, Morkos FF, Hassouna AK, Roshdy MM. Visual performance of the Tecnis one-piece lens ZCB00. Clin Ophthalmol. 2011;5:1803–1808. doi:10.2147/OPTH.S27324
22. Linz K, Attia MS, Khoramnia R, Tandogan T, Kretz FT, Auffarth GU. Clinical evaluation of reading performance using the Salzburg reading desk with a refractive rotational asymmetric multifocal intraocular lens. J Refract Surg. 2016;32(8):526–532. doi:10.3928/1081597X-20160603-02
23. Hirnschall N, Motaabbed JK, Dexl A, Grabner G, Findl O. Evaluation of an electronic reading desk to measure reading acuity in pseudophakic patients. J Cataract Refract Surg. 2014;40(9):1462–1468. doi:10.1016/j.jcrs.2013.12.021
24. Alió JL, Plaza-Puche AB, Piñero DP, et al. Optical analysis, reading performance, and quality-of-life evaluation after implantation of a diffractive multifocal intraocular lens. J Cataract Refract Surg. 2011;37(1):27–37. doi:10.1016/j.jcrs.2010.07.035
25. Attia MSA, Auffarth GU, Kretz FTA, et al. Clinical evaluation of an extended depth of focus intraocular lens with the Salzburg reading desk. J Refract Surg. 2017;33(10):664–669. doi:10.3928/1081597X-20170621-08
26. Kim J, Shin HJ, Kim HC, Shin KC. Comparison of conventional versus crossed monovision in pseudophakia. Br J Ophthalmol. 2015;99(3):391–395. doi:10.1136/bjophthalmol-2014-305449
27. Kim JY, Lee Y, Won HJ, et al. Diffractive multifocal intraocular lens implantation in patients with monofocal intraocular lens in the contralateral eye. Int J Ophthalmol. 2020;13(5):737–743. doi:10.18240/ijo.2020.05.07
28. Dell SJ. Evaluation of visual and subjective outcomes with mix-and-match of three one-piece Tecnis multifocal IOLs of varying add powers. Clin Ophthalmol. 2020;14:2903–2911. doi:10.2147/OPTH.S266120
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
