Back to Journals » Vascular Health and Risk Management » Volume 18
Vascular Responses Among Adults Four Years Post Exposure to 6 Weeks of Smoke from the Hazelwood Coal Mine Fire
Authors Mundisugih J, Gao CX, Ikin JF , Abramson MJ , Brown D, Biswas S, Dewar EM, Liew D, Stub D
Received 11 October 2021
Accepted for publication 8 March 2022
Published 13 April 2022 Volume 2022:18 Pages 253—265
DOI https://doi.org/10.2147/VHRM.S339439
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Pietro Scicchitano
Juan Mundisugih,1,2 Caroline X Gao,1,3 Jillian F Ikin,1 Michael J Abramson,1 David Brown,1 Sinjini Biswas,1,2 Elizabeth M Dewar,2,4 Danny Liew,1 Dion Stub1,2,4
1School of Public Health and Preventive Medicine, Monash University, Melbourne, VIC, Australia; 2Department of Cardiology, Alfred Health, Melbourne, VIC, Australia; 3Centre for Youth Mental Health (Orygen), University of Melbourne, Melbourne, VIC, Australia; 4Baker Heart and Diabetes Institute, Melbourne, VIC, Australia
Correspondence: Jillian F Ikin, Tel +61 3 9903 0308, Email [email protected]
Background and Aims: Mega-wild fires are exposing large communities to weeks or months of high concentration smoke-related fine particulate air pollution (PM). However, little research has examined the long-term vascular responses from exposure to PM of this concentration and duration. We investigated whether level of exposure to 6 weeks of PM from the 2014 Hazelwood coal mine fire was associated with abnormal vascular responses approximately four years later.
Methods: A cross-sectional analysis was undertaken of 387 participants (225 exposed, 162 unexposed) aged 55– 89 years, 3.5– 4 years after the mine fire. The primary outcome was flow-mediated dilatation (FMD), with time to reach peak diameter as the secondary outcome. Other secondary markers included high-sensitivity C-reactive protein (hsCRP) and ischaemic Electrocardiogram (ECG) changes.
Results: There was no evidence of a difference in FMD between participants with high, medium, low or no mine-fire related PM2.5 exposure (4.09% vs 4.06% vs 4.02% vs 3.98%, respectively, p=0.99). Likewise, there was no difference in hsCRP or ischaemic ECG changes. In contrast, there was evidence of a difference in time to peak diameter (p=0.002) with more unexposed participants reaching peak diameter within 30 seconds (36%) compared to those who had high, medium, or low exposure (23%, 22%, 13%, respectively). Multivariate ordinal logistic regression analysis suggested that township, Morwell (exposed) vs Sale (unexposed), but not level of PM2.5 exposure, was associated with delayed time to peak diameter (OR 2.71; 95% CI 1.56, 4.69). Smokers also had delayed time to peak diameter.
Conclusion: There was no association between level of exposure to PM2.5 from the 6-week Hazelwood coal mine fire smoke event and reduced FMD, elevated hsCRP or ischaemic ECG four years later. Evidence of delayed time to peak diameter observed in adults from the exposed town, compared to an unexposed town, requires further investigation.
Keywords: vascular responses, flow mediated dilatation, time to peak diameter, particulate matter, epidemiology, air pollution
Introduction
Both short (hours to days), and long-duration (months to years) exposures to fine particulate matter with an aerodynamic diameter <2.5µm (PM2.5) from ambient air pollution have been associated with decreased vascular responses1,2 and subsequent adverse cardiovascular outcomes.3,4 Decreased vascular response through endothelial dysfunction plays an essential role in the process of atherosclerosis5 and is also linked to systemic inflammation.6 Flow-mediated dilation (FMD) has been widely used as a non-invasive tool for examining peripheral artery endothelial function.7 Impaired FMD has been shown to represent an early step in developing subclinical target organ damage and later cardiovascular disease (CVD).8
However, particulate matter has a heterogeneous and dynamic chemical composition.9 The sources or chemical and physical properties, concentrations and duration of PM exposures are important. To date, limited clinical studies have explored any association between high-concentration, medium-duration (weeks to months) PM exposure from landscape fires such as wildfires or coal mine fire smoke and vascular responses. With climate change contributing to mega-wildfires which are exposing large populations to smoke for weeks to months,10,11 evidence about the long-term cardiovascular effects of high concentration, medium-duration PM exposure is increasingly important.
In February 2014, embers from a wildfire took hold in the Hazelwood power station open-cut brown coal mine, Latrobe Valley, Victoria, Australia. It was estimated that 140 kT of coal burned over a six week period, worsening local air quality, particularly in the adjacent town of Morwell (population 14,000).12 The Commonwealth Scientific and Industrial Research Organisation’s (CSIRO) Oceans and Atmosphere estimated hourly PM2.5 concentrations as high as 3730 μg m−3 compared to usual background levels of 6 μg m−3.12
A Victorian State Government appointed Board of Inquiry into the fire led to the establishment of the Hazelwood Health Study (HHS; www.hazelwoodhealthstudy.org.au), a collaborative program of research funded by the Victorian Department of Health (DH). The ongoing HHS aims to determine the potential long-term health consequences of the mine fire for the local population. Using daily counts of dispensed prescription medication from the Pharmaceutical Benefit Scheme (PBS) database, the Hazelinks Stream of the HHS observed an association between 10 mg/m3 unit increases in hourly PM2.5 concentrations and a 10% increase in dispensed cardiovascular medications over a lag range of 3–7 days exposure.13 Medical service utilisation data showed increases in general practitioner (GP) consultations, but there was no observed increase in cardiovascular-specific services.14 Hazelinks also utilised mortality data from the Australian Institute of Health and Welfare and estimated a 62% increase in risk of death from cardiovascular conditions in Morwell (95% CI 25%-110%) during the six months after the mine fire, including an 88% increase in deaths from ischaemic heart disease (IHD).15 In total there were 26 cardiovascular-related deaths in Morwell attributed to this six month, post mine fire period, including 17 with IHD. These 26 cardiovascular deaths represented 38% of all cardiovascular deaths in Morwell during this period.15
Three years after the mine fire, the HHS Early Life Follow up Stream demonstrated increased vascular stiffness, measured using pulse wave velocity, in locally residing infants who were aged up to two years at the time of the mine fire.16 During the 3.5 years after the fire, Hazelinks found that a 10 µg/m3 increase in individual-level mean PM2.5 exposure was associated with increased risk of cardiovascular related ambulance attendances (Adj HR:1.13; 95% CI 1.01, 1.28).17 However, approximately four years after the mine fire, the HHS adult Cardiovascular Stream observed no differences between 330 residents of Morwell, and 165 residents of an unexposed comparison town, Sale, aged 55 years and older, on clinical or subclinical cardiovascular markers including serum high sensitivity (hs) C-reactive protein (CRP), blood pressure, electrocardiogram (ECG) and serum levels of hs-troponin, N-terminal pro B-type natriuretic peptide and lipids.18
A subgroup of the adult Cardiovascular Stream participants underwent detailed assessment of endothelial function as measured by FMD. The aim of the present analysis was to categorise participants into no, low, medium or high levels of Hazelwood coal mine fire smoke-related PM2.5 exposure and undertake an in-depth investigation of any association between endothelial function and category of PM2.5 exposure. A secondary aim was to compare hsCRP and ischaemic ECG changes across the four exposure categories.
Materials and Methods
Study Design
The adult Cardiovascular Stream data collection was undertaken during October 2017 to May 2018, approximately 3.5–4 years after the mine fire. As shown in Figure S1, a weighted random sample of 1133 potential participants was drawn from 2198 people who had previously completed the HHS Adult Survey,19 lived in Morwell (exposed) or the comparison town of Sale (unexposed) at the time of the mine fire and were males aged 55–89 years or females 60–89 years. Participants with existing cardiovascular conditions were oversampled, such that they represented 50% of those invited.
The Cardiovascular Stream had a target sample size of 330 Morwell participants and 165 Sale participants. After preliminary data collection from 145 participants in Sale, FMD (%) was found to have a mean of 4.4 and an SD of 2.54. Hence, we assumed that the SD of FMD (%) was 0.6 times mean of FMD %. A meta-analysis20 reported that for a 1% increase in FMD (%), we would expect an 8% decrease in the future CV event risk. So, a 1% difference in mean FMD (%) between groups constituted a clinically important difference. In order to achieve 90% power to detect a 1% difference in mean FMD (%) between groups (4.4 in Sale and 5.4 in Morwell) using a two-sample t-test, a sub-sample of 220 Morwell and 165 Sale participants was required to complete FMD testing. Recruitment was by mailed invitation, with up to two reminders and follow up phone contact attempted for non-responders. Recruitment and testing continued until target sample sizes were reached or exceeded, after which non-responders were not pursued.
Air Pollution Exposure
Due to limitations in the ground level air pollution monitoring during the early days of the mine fire period, the CSIRO Oceans and Atmosphere undertook modelling of the mine fire-related PM2.5 concentrations in the Latrobe Valley and surrounding area.12 The model incorporated variables such as weather information including wind direction, speed and temperature and calculations of the amount of PM2.5 released per unit mass of burning coal.12 It was found that the National Environment Protection Measure was exceeded on 23 days in southern Morwell and 12 days in eastern Morwell.
The town of Sale was estimated to have usual background levels (average PM2.5 concentration 6µg/m3) without any elevation in PM2.5 concentrations and the air quality limits were not exceeded.21 Within Sale, 16 statistical areas Level 1 (SA1s) were selected which had comparable median age, household size, Socio-Economic Indexes For Areas (SEIFA) and population stability as Morwell. By limiting recruitment in Sale to these SA1s, this comparison population was as similar to Morwell as practically possible, with the exception of Hazelwood mine fire smoke exposure. CSIRO’s modelled 12-hourly mine fire-related PM2.5 concentrations were mapped to participants’ time-location diaries which had been collected as part of the Adult Survey, to estimate each participant’s average, and peak, daily level of mine fire-related PM2.5 exposure over the six-week duration of the fire. The time-location diaries included participant’s residential addresses, work addresses and any addresses to which they relocated, on each day and each night of the 6 week mine fire period.
Outcomes and Covariates
FMD was obtained on the right brachial artery via a Vivid Q ultrasound system with a 12 MHz linear probe (GE Healthcare, Haifa, Israel) at a standardised room temperature of 22–26°C. Any smoking or consumption of food, vitamin supplements, caffeine or alcohol in the four hours prior to assessment, and any moderate to vigorous physical activity in the 48 hours prior, were documented. Baseline brachial artery images were obtained after 10–15 minutes of supine rest. The duration of cuff occlusion was five minutes. Following cuff deflation, images were obtained at 30-, 60-, 90-, 120- and 180-second time intervals. The average diameter (mm) of the brachial artery over six R waves was measured at each interval and deducted from the baseline diameter to obtain the relative change as a percentage of the baseline diameter.22 The maximal relative change was used as the FMD (%) value in the analysis. The primary outcome was FMD (%) with time to reach peak diameter as the secondary outcome.
Other markers of vascular health, such as hsCRP23 and evidence of ischaemic heart disease based on 12-lead electrocardiograph (ECG), were also assessed. A sample of blood was taken from a peripheral vein of unfasted participants and hsCRP level was measured via the immunoturbidimetric method. A standard ECG was acquired using a portable ECG Machine (Philips TC50, China) and then validated by a cardiologist (SB). Evidence of underlying ischaemic heart disease, i.e., left bundle branch block, previous infarction, ST depression, T or Q wave abnormalities, was documented. Abnormal results were communicated, with the participants’ permission, to their regular general practitioners for further management as appropriate.
In order to assess the cardiovascular risk of the participants, the Framingham Risk Score was calculated based on age, cigarette smoking, total cholesterol, high-density lipoprotein cholesterol, measurement of systolic blood pressure and treatment for hypertension.24,25 Participants’ characteristics such as age, gender, ethnicity, education, employment status, body mass index (BMI), smoking status, alcohol consumption, physical activity, occupational exposure, history of CVD, diabetes mellitus, hypertension, hypercholesterolaemia, family history of heart attack or stroke, and medications were obtained by self-report questionnaire (See Table S1 for cardiovascular health, smoking, alcohol, physical activity and ethnicity questions, and Table S2 for medications and corresponding ATC codes).
Smoking status was coded as either Non-smoker (<100 cigarettes in entire lifetime), Current smoker (≥ 100 cigarettes and smoking on a regular basis) or Ex-smoker (≥100 cigarettes in entire lifetime, but no longer smoking). Alcohol consumption was assessed using the Alcohol Use Disorders Identification Test - Consumption (AUDIT-C) tool, with a score of 0 implying Non-drinker, a score of 1–2 for females and 1–3 for males indicating Low risk, and a score ≥3 for females or ≥4 for males considered High risk.26
Adequate physical activity was defined as any vigorous physical activity or at least 150 minutes of moderate physical activity for the previous seven days.27 Past history of CVD was defined as a self-reported doctor-diagnosis of myocardial infarction, coronary artery disease, stroke and/or peripheral vascular disease. Participants who self-reported a doctor-diagnosis of type 2 diabetes, were taking oral hypoglycaemic medications or insulin, or had a HbA1c ≥6.5% were coded as having diabetes mellitus. Medications were recorded with associated WHO Anatomical Therapeutic Chemical Classification System (ATC) codes (see Table S2 for a list of ATC codes).28 Occupational exposure was defined as having worked as an emergency responder, or in a coal mine or power station, or in any job for at least six months where the air contained a lot of dust, fumes, smoke, gas, vapour or mist.
Statistical Analyses
Demographic characteristics and health-related risk factors were compared using descriptive statistics. Weighting methods were used to correct for over sampling of participants with a history of CVD, as well as possible selection bias in the HHS Adult Survey. Categorical variables were analysed with weighted Pearson χ2 tests, while continuous variables were compared using weighted t-tests. Simple descriptive statistics were used to compare outcomes between Sale (unexposed) and tertiles of mine fire related daily PM2.5 exposure in Morwell (low, medium or high).
Linear regression was used to evaluate associations between mine fire-related PM2.5 exposure level and FMD (%) controlling for key confounding factors including demographics, smoking and drinking status, as well as factors related to underlying risk of cardiovascular diseases such as Framingham Risk Score and family history. Average baseline diameter of brachial artery was also included as a confounding factor. Regression models were estimated with, or without, township (Morwell vs Sale) as a potential confounder, to evaluate any residual confounding by township when estimating the dose-response relationship between PM2.5 exposure and FMD %. Ordinal logistic regression was used to evaluate associations between exposure and time to peak FMD, controlling for key confounding factors. The proportional odds assumption of ordinal logistic regression was evaluated using approximate likelihood-ratio test.29 All regression analyses accounted for post-stratification and sampling weights, sampling stratification (Morwell vs Sale) and clustering at household level. Statistical analyses were performed using Stata version 15 (Stata Corporation, College Station, Texas 2015).
Ethics Committee Approval and Consent
The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki, the Monash University Human Research Ethics Committee granted approval for this research (Project number 1078) and each participant signed an informed consent statement prior to commencement.
Results
Description of Participants
Recruitment concluded when 336 Morwell residents and 162 Sale residents (n=498; 45%) had participated, of whom 387 (225 Morwell and 162 Sale) underwent FMD measurement (refer Figure S1). Exposed Morwell participants comprised 78 categorised as low PM2.5 exposure, 73 medium exposure, and 74 high exposure. The mean and peak daily PM2.5 levels for each exposure category are provided in Table 1. Participants were generally well matched across the PM2.5 exposure groups, including Framingham Risk Score, age, gender, employment status, education level, body mass index, alcohol consumption, occupational exposure, past medical history, and family history of heart attack or stroke. However, fewer participants who had medium exposure were Caucasian (p=0.031) and more participants who had low exposure were current smokers (p=0.029). In addition, there were fewer participant in Sale who were physically inactive (p=0.005) and took aspirin (p=0.01) or lipid modifying agents (p=0.002) as regular medications, as described in Table 1.
 |
Table 1 Demographic and Clinical Profile of the Study Sample (N=387) Across Exposure Levels |
Outcomes
Table 2 shows crude comparisons between unexposed, low, medium and high exposure participants. There was no evidence of a difference in the average baseline diameter of brachial artery (0.48mm vs 0.48mm vs 0.47mm vs 0.46mm; p=0.56), peak brachial artery diameter (0.49mm vs 0.50mm vs 0.49mm vs 0.48mm; p=0.50), FMD absolute value (0.018mm vs 0.019mm vs 0.018mm vs 0.018mm; p=0.86), or FMD % (3.98% vs 4.02% vs 4.06% vs 4.09%; p=0.99). In terms of other markers of vascular health, there was also no evidence of a difference in the average hsCRP level (3.19 vs 3.54 vs 3.75 vs 2.78mg/L; p=0.46) or the proportions with ischaemic ECG changes (15% vs 21% vs 29% vs 12%; p=0.11), as shown in Table 2. However, there were more unexposed participants who reached peak diameter of brachial artery within 30 seconds of cuff deflation compared to low, medium, and high exposure participants (36% vs 13%, 22% and 23% respectively, p=0.002). The distributions of FMD % and time to peak diameter are shown in Figures 1 and 2, respectively.
 |
Table 2 Crude Comparison of Study Outcomes Between Unexposed, Low, Medium and High Exposure Levels |
 |
Figure 1 Comparison of FMD (%) distribution (A) between Morwell and Sale, and (B) between exposure levels. Note: Statistical weighting not applied. |
 |
Figure 2 Comparison of time to peak diameter distribution (A) between Morwell and Sale and (B) between exposure groups. Note: Statistical weighting not applied. |
In multivariable regression models, neither PM2.5 exposure level nor residential township were associated with FMD % after controlling for other confounding factors (refer Table 3). Males were found to have higher FMD % (Coef=2.12, 95% CI:1.12, 3.12). Having a larger baseline brachial artery diameter (Coef=−17.05, 95% CI: −21.9, −12.2), being employed (Coef=−0.92, 95% CI: −1.44, −0.40) and being an ex-smoker (Coef=−0.92, 95% CI: −1.44, −0.40) were found to be associated with lower FMD %, as shown in Table 3.
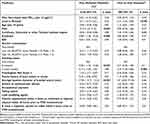 |
Table 3 Potential Predictive Factors for Flow Mediated Dilatation and Time to Peak Diameter |
Table 3 also summarises ordinal logistic regression models for time to peak diameter. Although individual level of PM2.5 exposure was not associated with time to peak diameter, living in the exposed town, Morwell, during the mine fire period was associated with delayed time to peak diameter (ORadj 2.71, 95% CI: 1.56, 4.69). Similar associations were also shown for participants who were current smokers (ORadj 2.55, 95% CI: 1.39, 4.66) or had higher education (ORadj 1.53, 95% CI: 1.03, 2.26). Both regression models showed that differences between participants in medications, such as aspirin and lipid modifying agents, did not seem to affect FMD % or time to peak diameter, as described in Table 3.
Most participants (95% of the study sample) either had vitamin supplements or a meal/ cigarette/ alcohol/ coffee within four hours prior to FMD measurement, or had undertaken moderate to vigorous physical activity within 48 hours prior. However, the impact on FMD results or time to peak diameter between exposure levels seemed to be minimal as shown in the regression analyses in Table 3.
Discussion
The key findings of this study were that level of exposure to PM2.5 from the six-week Hazelwood coal mine fire smoke was not associated with impaired FMD results, elevated hsCRP or ischaemic ECG changes four years later in older adults. Delayed time to peak diameter was observed in participants living in the most exposed town, Morwell, however this was not associated with PM2.5 exposure category. That may mean that any level of PM2.5 during the 6-week mine fire was sufficient to elicit this impairment. Alternatively, the difference between the two towns was caused by residual unknown confounders which require further investigation.
These findings build upon previous HHS research showing increased dispensing of cardiovascular medications during the mine fire,13 increased risk of cardiovascular-related deaths during the 6 months after the mine fire,15 increased vascular stiffness in young children three years after exposure,16 increased ambulance call outs for cardiovascular-related causes during the 3.5 years after the fire,17 but no increase in a number of cardiovascular markers in adults four years after the fire.18 Combined, these findings suggest that adverse cardiovascular effects of the mine fire smoke may have not persisted in older adults four years after exposure.
Both short- and long-duration exposures to PM2.5 have been related to reduced vascular response through impaired endothelium-dependent vasodilation.1,2,30,31 Several mechanisms have been proposed involving systemic oxidative stress, inflammation and autonomic imbalance.1,2,32 Nonetheless, the most harmful aspect of PM to vascular function and cardiovascular health may not be best quantified by mass concentration alone. PM has a heterogeneous and dynamic chemical composition,33 which can have independent and potentially synergistic or antagonistic effects with each constituent.1
Our study provided unique insights into the impact of high concentration, medium duration coal mine fire PM2.5 exposure on vascular function. Whilst we might expect abnormal vascular responses in exposed participants, we were unable to convincingly demonstrate endothelial dysfunction among older adults approximately four years after exposure to smoke from the Hazelwood coal mine fire. Our study showed endothelial function measured by FMD was not significantly different between the four groups at different exposure levels. After adjustment for potential confounders, the FMD results were still not influenced by the coal mine fire PM2.5 exposure level. This lack of an observed impact on vascular function is further supported by the lack of differences in the hsCRP levels and lack of evidence of changes in underlying ischaemic heart disease on ECG.
Considering our analysis was conducted almost four years following a medium-duration exposure, there is a possibility that an acute association between the exposure and decreased vascular response was missed. Our previous findings of increased dispensing of cardiovascular medications during the mine fire,13 and increased risk of cardiovascular-related deaths during the 6 months after the mine fire,15 support this possibility. The increase in cardiovascular-related deaths within a few months of the fire could have contributed to a “harvesting” effect whereby some of the residents most vulnerable to a reduced vascular response subsequently died and were, therefore, excluded from this four-year followup study.
The increased dispensing of cardiovascular medications may reflect the possibility that residents with known chronic heart conditions took precautionary and protective measures. It was also possible that some residents with known chronic heart conditions relocated from the smoke-effected areas. Both of these protective measures would potentially reduce the likelihood of finding an association between level of PM2.5 exposure and vascular function four years later. Most previous studies measured vascular response within a few days or weeks of the exposure.2,34–36 It is also possible that improvement in the air quality after the exposure would lead to gradual improvement of endothelial function. One study suggested impaired endothelial function could be favourably influenced by reducing indoor PM2.5 in a woodsmoke-impacted community.37
The multivariable analysis of the FMD identified average baseline brachial artery diameter as the strongest predictor of reduction in FMD, followed by former smoking and being employed. On the other hand, male gender was associated with greater FMD. These findings are consistent with previous studies where FMD correlated positively with male gender, but negatively with baseline brachial artery diameter.38,39 In contrast, being an ex-smoker and being employed as negative predictors of FMD still remain unexplained.
Measurement of time to peak diameter as a potential marker of vascular response has attracted interest. One study demonstrated that individuals with metabolic syndrome had preserved FMD, but delayed time to peak diameter.40 It was suggested that time to peak diameter may provide new insights into the vascular phenotype.40 Although Liuni et al41 interpreted the time to peak diameter as at least partially nitric oxide independent, their study also revealed there was a significant positive correlation between age and time to peak diameter. Similarly, Black et al42 demonstrated a significant difference between time to peak diameter in cohorts of young and older healthy subjects, suggesting that these findings may have been due to the decrease in arterial compliance that was associated with advanced age. As a result, those studies might support the hypothesis that arterial stiffness might delay time to peak diameter, but not reduce FMD %.41
In our study, there was a significant difference in time to reach peak diameter between exposed and unexposed participants. After adjustment for known potential confounders, current smoking and living in Morwell, but not PM2.5 exposure level, were strong independent predictors of delayed time to peak diameter. While it has previously been documented that smoking increases arterial stiffness,43–45 the association between delayed time to peak diameter and living in Morwell is not fully explained. It is possibly due to residual unknown confounders, such as diet, physical activity or occupation. Further longitudinal population studies of participants living in Morwell or similar towns would be required to verify those potential unknown confounders.
Study Strengths and Limitations
Our study provides unique insights into the impact of a medium duration exposure to coal mine fire emissions on vascular responses in older adults. When combined with our previously reported findings which were based on longitudinal administrative health datasets13,15,17 and clinical studies in infants,16 these detailed clinical data from older adults exposed to the mine fire provide a comprehensive overview of the impacts of mine fire smoke on the effected community’s cardiovascular health. A further strength of this study is its use of detailed individual daily PM2.5 exposure estimates drawing upon sophisticated modelling techniques12 and participant’s detailed time-location diaries. Additionally, our study looked into the potential utility of time to peak diameter measurement in real life cases and our findings suggest it could be a useful adjunctive measure of vascular status.
However, this study has some limitations that need to be acknowledged. Firstly, this was a cross-sectional analysis and temporality could not be established. Secondly, FMD measurements during or immediately after the exposure were not available. Those measurements might have provided a better reflection of the short-term impact of coal mine fire smoke on vascular endothelial function. Thirdly, there were potential unknown confounders that might have influenced the time to peak diameters.
Conclusions
Medium-duration exposure to high concentration coal mine fire smoke was not associated with reduced FMD or delayed time to peak diameter four years later in older adults. Combined with previous findings, these data suggest that adverse cardiovascular effects of the mine fire smoke observed during the first 3 years or so after the event, have not persisted in older adults after four years. However, future linkages with healthcare utilisation data may confirm the longer-term cardiovascular effects in this community. This is an important topic, not just because the incidence of coal mine fires is increasing across the globe46 but also because mega wildfires such as those in South-eastern Australia,10,47 the west coast of the US11 and Greece48 have exposed large communities to smoke for weeks and months. Our research should assist governments and policy makers to make an appropriate public health response to similar events in the future.
Acknowledgments
The Victorian Department of Health funded the Hazelwood Health Study. However, the paper presents the views of the authors, not the Department. We would like to acknowledge Brigitte Borg, Sharon Harrison, Karen Kilpatrick, Shantelle Allgood, Susan Denny, Sylvia Pomeroy, Melanie Reeves, Kylie Sawyer and Kristina Thomas for their assistance with project management, procurement, recruitment and data collection.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by the Victorian Department of Health. The paper presents the views of the authors and does not represent the views of the Department.
Disclosure
Michael J Abramson holds investigator-initiated grants for unrelated research from Pfizer, Boehringer-Ingelheim, Sanofi and GSK. He has also undertaken an unrelated consultancy for Sanofi and received a speaker’s fee from GSK. Danny Liew has undertaken unrelated consultancies for AbbVie, Astellas, AstraZeneca, Bristol-Myers Squibb, CSL-Behring, Novartis, Pfizer and Sanofi. Dion Stub undertakes unrelated research supported by a National Heart Foundation fellowship. The remaining authors report no relationships that could be construed as a conflict of interest in this work.
References
1. Brook RD, Rajagopalan S, Pope CA
2. Krishnan RM, Adar SD, Szpiro AA, et al. Vascular responses to long- and short-term exposure to fine particulate matter: mesa Air (Multi-Ethnic Study of Atherosclerosis and Air Pollution). J Am Coll Cardiol. 2012;60(21):2158–2166.
3. Newby DE, Mannucci PM, Tell GS, et al. Expert position paper on air pollution and cardiovascular disease. Eur Heart J. 2015;36(2):83–93b.
4. Franklin BA, Brook R, Arden pope C
5. Thijssen DHJ, Bruno RM, van Mil A, et al. Expert consensus and evidence-based recommendations for the assessment of flow-mediated dilation in humans. Eur Heart J. 2019;40(30):2534–2547.
6. Hurlimann D, Forster A, Noll G, et al. Anti-tumor necrosis factor-alpha treatment improves endothelial function in patients with rheumatoid arthritis. Circulation. 2002;106(17):2184–2187.
7. Celermajer DS, Sorensen KE, Gooch VM, et al. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet. 1992;340(8828):1111–1115.
8. Charakida M, Masi S, Luscher TF, Kastelein JJ, Deanfield JE. Assessment of atherosclerosis: the role of flow-mediated dilatation. Eur Heart J. 2010;31(23):2854–2861.
9. World Health Organization Regional Office for Europe. Health Effects of Particulate Matter. Policy Implications for Countries in Eastern Europe, Caucasus and Central Asia. World Health Organization; 2013.
10. Johnston FH, Borchers-Arriagada N, Morgan GG, et al. Unprecedented health costs of smoke-related PM2.5 from the 2019–20 Australian megafires. Nature Sustainability. 2021;4(1):42–47.
11. Rice MB, Henderson SB, Lambert AA, et al. Respiratory Impacts of Wildland Fire Smoke: future Challenges and Policy Opportunities. An Official American Thoracic Society Workshop Report. Ann Am Thorac Soc. 2021;18(6):921–930.
12. Luhar A, Emmerson K, Reisen F, Williamson G, Cope M. Modelling smoke distribution in the vicinity of a large and prolonged fire from an open-cut coal mine. Atmos Environ. 2020;229:117471.
13. Johnson AL, Dipnall JF, Dennekamp M, et al. Fine particulate matter exposure and medication dispensing during and after a coal mine fire: a time series analysis from the Hazelwood Health Study. Environ Pollut. 2019;246:1027–1035.
14. Johnson AL, Gao CX, Dennekamp M, et al. Coal-mine fire-related fine particulate matter and medical-service utilization in Australia: a time-series analysis from the Hazelwood Health Study. Int J Epidemiol. 2020;49(1):80–93.
15. Dimitriadis C, Gao CX, Ikin JF, et al. Exposure to mine fire related particulate matter and mortality: a time series analysis from the Hazelwood Health Study. Chemosphere. 2021;285:131351.
16. Zhao B, Johnston FH, O’Sullivan T, et al. Early life exposure to coal mine fire and tobacco smoke affect subclinical vascular function. Arch Dis Child. 2019;105(6):539–544.
17. Broder J, Gao CX, Abramson MJ, et al. Long-term impact of exposure to coalmine fire emitted PM2.5 on emergency ambulance attendances. Chemosphere. 2022;288(1):132339.
18. Betts JM, Dewar EM, Stub DA, et al. Markers of cardiovascular disease among adults exposed to smoke from the Hazelwood coal mine fire. Int J Environ Res Public Health. 2021;18(4):1587.
19. Ikin J, Carroll M, Walker J, et al. Cohort Profile: the Hazelwood Health Study Adult Cohort. Int J Epidemiol. 2020;49(6):1777–1778.
20. Inaba Y, Chen JA, Bergmann SR. Prediction of future cardiovascular outcomes by flow-mediated vasodilatation of brachial artery: a meta-analysis. Int J Cardiovasc Imaging. 2010;26(6):631–640.
21. Emmerson K, Reisen F, Luhar A, Cope M, Williamson G. Air Quality Modelling of Smoke Exposure from the Hazelwood Mine Fire. CSIRO; 2016.
22. Liang YL, Teede H, Kotsopoulos D, et al. Non-invasive measurements of arterial structure and function: repeatability, interrelationships and trial sample size. Clin Sci (Lond). 1998;95(6):669–679.
23. Carrero JJ, Franko MA, Obergfell A, Gabrielsen A, Jernberg T. hsCRP Level and the Risk of Death or Recurrent Cardiovascular Events in Patients With Myocardial Infarction: a Healthcare‐Based Study. J Am Heart Assoc. 2019;8(11):e012638.
24. Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837–1847.
25. Sytkowski PA, Kannel WB, D’Agostino RB. Changes in Risk Factors and the Decline in Mortality from Cardiovascular Disease. N Eng J Med. 1990;322(23):1635–1641.
26. Fujii H, Nishimoto N, Yamaguchi S, et al. The Alcohol Use Disorders Identification Test for Consumption (AUDIT-C) is more useful than pre-existing laboratory tests for predicting hazardous drinking: a cross-sectional study. BMC Public Health. 2016;16(1):379.
27. Australian Institute of Health and Welfare. Insufficient physical activity. AIHW. Available from: https://www.aihw.gov.au/reports/risk-factors/insufficient-physical-activity.
28. World Health Organization. ATC Classification Index with DDDs, 2020. Oslo, Norway: WHO Collaborating Centre for Drug Statistics Methodology; 2019.
29. Wolfe R, Gould W. An approximate likelihood-ratio test for ordinal response models. Stata Technical Bulletin. 1998;42:24-27.
30. Rundell KW, Hoffman JR, Caviston R, Bulbulian R, Hollenbach AM. Inhalation of ultrafine and fine particulate matter disrupts systemic vascular function. Inhal Toxicol. 2007;19(2):133–140.
31. Briet M, Collin C, Laurent S, et al. Endothelial function and chronic exposure to air pollution in normal male subjects. Hypertension. 2007;50(5):970–976.
32. Pope CA
33. Health effects of particulate matter. World Health Organization. Policy implications for countries in Eastern Europe, Caucasus and Central Asia Web site; 2013. Available from: http://www.euro.who.int/__data/assets/pdf_file/0006/189051/Health-effects-of-particulate-matter-final-Eng.pdf?ua=1.
34. O’Neill MS, Veves A, Zanobetti A, et al. Diabetes enhances vulnerability to particulate air pollution-associated impairment in vascular reactivity and endothelial function. Circulation. 2005;111(22):2913–2920.
35. Liu L, Ruddy TD, Dalipaj M, et al. Influence of personal exposure to particulate air pollution on cardiovascular physiology and biomarkers of inflammation and oxidative stress in subjects with diabetes. J Occup Environ Med. 2007;49(3):258–265.
36. Schneider A, Neas L, Herbst MC, et al. Endothelial dysfunction: associations with exposure to ambient fine particles in diabetic individuals. Environ Health Perspect. 2008;116(12):1666–1674.
37. Allen RW, Carlsten C, Karlen B, et al. An air filter intervention study of endothelial function among healthy adults in a woodsmoke-impacted community. Am J Respir Crit Care Med. 2011;183(9):1222–1230.
38. Maruhashi T, Soga J, Fujimura N, et al. Relationship between flow-mediated vasodilation and cardiovascular risk factors in a large community-based study. Heart. 2013;99(24):1837.
39. Mizia-Stec K, Gasior Z, Mizia M, et al. Flow-mediated dilation and gender in patients with coronary artery disease: arterial size influences gender differences in flow-mediated dilation. Echocardiography. 2007;24(10):1051–1057.
40. Fernandes IA, Sales AR, Rocha NG, Silva BM, Vianna LC, da Nobrega AC. Preserved flow-mediated dilation but delayed time-to-peak diameter in individuals with metabolic syndrome. Clin Physiol Funct Imaging. 2014;34(4):270–276.
41. Liuni A, Luca MC, Lisi M, et al. Observations of time-based measures of flow-mediated dilation of forearm conduit arteries: implications for the accurate assessment of endothelial function. Am J Physiol Heart Circ Physiol. 2010;299(3):H939–945.
42. Black MA, Cable NT, Thijssen DH, Green DJ. Importance of measuring the time course of flow-mediated dilatation in humans. Hypertension. 2008;51(2):203–210.
43. Doonan RJ, Hausvater A, Scallan C, Mikhailidis DP, Pilote L, Daskalopoulou SS. The effect of smoking on arterial stiffness. Hypertens Res. 2010;33(5):398–410.
44. Camplain R, Meyer ML, Tanaka H, et al. Smoking Behaviors and Arterial Stiffness Measured by Pulse Wave Velocity in Older Adults: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Hypertens. 2015;29(11):1268–1275.
45. Wei Y, Liu H, Liu B. Impact of smoking and smoking cessation on arterial stiffness in healthy individuals. Heart. 2011;97(Suppl 3):A107.
46. Melody SM, Johnston FH. Coal mine fires and human health: what do we know? Int J Coal Geol. 2015;152:1–14.
47. Borchers Arriagada N, Palmer AJ, Bowman DM, Morgan GG, Jalaludin BB, Johnston FH. Unprecedented smoke-related health burden associated with the 2019-20 bushfires in eastern Australia. Med J Aust. 2020;1:543.
48. Palaiologou P, Kalabokidis K, Troumbis A, Day MA, Nielsen-Pincus M, Ager AA. Socio-Ecological Perceptions of Wildfire Management and Effects in Greece. Fire. 2021;4(2):18.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
