Back to Journals » Therapeutics and Clinical Risk Management » Volume 16
Vancomycin in ICU Patients with Gram-Positive Infections: Initial Trough Levels and Mortality
Authors Alshehri N, Ahmed AE, Yenugadhati N , Javad S, Al Sulaiman K , Al-Dorzi HM , Aljerasiy M , Badri M
Received 18 June 2020
Accepted for publication 6 September 2020
Published 14 October 2020 Volume 2020:16 Pages 979—987
DOI https://doi.org/10.2147/TCRM.S266295
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Garry Walsh
Nadiyah Alshehri,1,2 Anwar E Ahmed,3 Nagarajkumar Yenugadhati,2,4 Sundas Javad,2,4 Khalid Al Sulaiman,1 Hasan M Al-Dorzi,5 Majed Aljerasiy,4 Motasim Badri2,4
1Pharmaceutical Care Department, Ministry of National Guard- Health Affairs, Riyadh, Saudi Arabia; 2Department of Epidemiology & Biostatistics, College of Public Health and Health Informatics, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia; 3Henry M. Jackson Foundation for the Advancement of Military Medicine, Bethesda, MD, USA; 4King Abdullah International Medical Research Center, King Saud Bin-Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia; 5Intensive Care Department, College of Medicine King Saud Bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia
Correspondence: Nadiyah Alshehri
Department of Epidemiology & Biostatistics, College of Public Health and Health Informatics, King Saud bin Abdulaziz University for Health Sciences, P.O. Box: 47323, Riyadh 11552, Saudi Arabia
Email [email protected]
Background: Vancomycin is one of the most common therapeutic agents for treating gram-positive infections, particularly in critically ill patients. The aim of this study was to identify factors associated with initial therapeutic vancomycin trough levels and mortality in a tertiary-care intensive care unit (ICU).
Methods: This retrospective study evaluated 301 adult ICU patients admitted to King Abdulaziz Medical City in Riyadh between October 1, 2017 and December 31, 2018 with confirmed gram-positive infections and received intravenous vancomycin. Vancomycin trough levels of 15– 20 mg/L for severe infections and 10– 15 mg/L for less severe infections were considered therapeutic.
Results: The patients were relatively older with a mean age of 60 (SD ± 20) years. Initial vancomycin trough levels were therapeutic in 168 (55.8%). Factors associated with initial therapeutic vancomycin trough levels were female gender (adjusted odds ratio [aOR]=2.575), older age (aOR=1.024), receiving a loading dose (aOR=2.445), having bacteremia (aOR=2.061), and high platelet count (aOR=1.003). On the other hand, the increase of estimated glomerular filtration rate (eGFR) (aOR=0.993) and albumin levels (aOR=0.944) were associated with lower odds of initial therapeutic vancomycin trough levels. Factors associated with higher mortality were female gender (adjusted hazard ratio [aHR]=2.630), increased body weight (aHR=1.021), cancer (aHR=3.451), and high APACHE II score (aHR=1.068).
Conclusion: The study identified several factors associated with achieving initial therapeutic vancomycin trough levels (i.e. older age, female gender, receiving a loading dose, bacteremia, high platelets count, low eGFR and albumin level). These factors should be considered in the dosing of vancomycin in critically ill patients with gram-positive infections.
Keywords: vancomycin dosage, pharmacokinetics, renal function, serum trough levels, mortality
Introduction
Vancomycin, a glycopeptide antibiotic, is frequently used for treating severe infections caused by gram positive bacteria in critically ill patients. These infections include bacteremia, pneumonia, skin and soft tissue infections, and other methicillin-resistant Staphylococcus aureus-induced sepsis or septic shock.1 According to the Infectious Diseases Society of the United States of America (IDSA), the initial dose for adult patients ranges from 15–20 mg/kg of actual body weight, and dosing frequency depends on creatinine clearance.2 The recent guidelines recommended an initial dose is 25–30 mg/kg as loading dose in treating complicated infections in the critically ill.3 Physicians/clinical pharmacists should also consider age, sex, disease status, and volume of distribution. These factors can lead to variations in the pharmacokinetics of vancomycin and should be considered to provide the appropriate dose and achieve therapeutic effectiveness.
The recommendations suggest that trough vancomycin levels should be checked at steady-state conditions before the fourth dose (without a loading dose) and before the third dose (with loading dose).4,5 A higher vancomycin target trough level is required for selected infections (ie, sepsis, pneumonia, meningitis, osteomyelitis, and endocarditis) of 15–20 mg/L and 10–15 mg/L for less severe infections, respectively.6,7 New guidelines recommended the trough vancomycin level to be 15–20 mg/L.3 Under-dosing of vancomycin might contribute to antimicrobial resistance and failure of treatment, while over-dosing leads to toxicity such as nephrotoxicity and ototoxicity.8 Nephrotoxicity remains the most severe vancomycin adverse effect and is reversible. Studies showed that vancomycin trough 20 ≥ mcg/mL was an independent predictor of nephrotoxicity.9,10 Vancomycin-associated nephrotoxicity is associated with increased length of hospital stay, costs, and mortality.11 Results from a recent systematic review and meta-analysis revealed that the implementation of the recommended therapeutic levels for vancomycin resulted in improved clinical outcomes and lowers the risk of nephrotoxicity.12
Studies have shown that up to 40% of ICU patients receiving vancomycin did not reach the initial therapeutic trough level.13,14 This alarming prevalence rate necessitates understanding of factors that increase the odds of therapeutic vancomycin trough levels and mortality in critically ill patients with gram positive infections. This has become more important as studies have demonstrated increased use of vancomycin in the ICUs, including those in Saudi Arabia.15 A standardized loading dose can be considered as a simple and sustainable intervention that can enhance the achievement of therapeutic vancomycin levels in critically ill patients.16–18 In these patients, 30-day mortality is associated with age, malignancy, increased illness severity scores, residence in long-term care facilities, and chronic renal failure.19,20
To our knowledge there has not been any recent study conducted in Saudi Arabia to determine the factors affecting reaching therapeutic levels of vancomycin and mortality rate in ICU patients. The aim of this study was to identify factors associated with initial therapeutic vancomycin trough levels and mortality in the intensive care unit (ICU) at King Abdulaziz Medical City-Riyadh (KAMC-R).
Materials and Methods
A retrospective study was conducted in adult ICU patients (aged ≥18 years) who had confirmed gram-positive infections and received intravenous vancomycin between October 1, 2017 and December 31, 2018 at KAMC-R. The ICU at KAMC-R followed the closed unit concept, admitted a variety of medical, surgical and trauma patients, and were covered by board-certified intensivists 24/7. Clinical pharmacists were part of the multidisciplinary rounds during the weekdays. The IRB of King Abdullah International Medical Research Center approved the study (IRB SP19/025/R) and waived informed consent due to the study nature. Ethical standards complied with the Declaration of Helsinki.
The study data were obtained from BESTCare, the hospital information system, and included data on vancomycin trough level after the fourth dose (without a loading dose) and the third dose (with loading dose), demographic characteristics (height, body-weight, age, and gender), clinical characteristics (type of comorbidities, Gram-positive organisms, the associating chronic diseases, admission category, hemodialysis, renal function, creatine serum, loading dose and the fluid balance alongside that of vancomycin antibiotics, date of administration vancomycin, therapeutic levels, length of ICU stay, shock types, source of bloodstream infection, recurrence of disease, duration of vancomycin, vancomycin trough concentrations, death, date of death, the Glasgow coma scale the Vasoactive-Inotropic and APACHE-II Score). Vancomycin therapeutic trough levels of 15–20 mg/L for severe infections (ie, sepsis, pneumonia, meningitis, osteomyelitis, and endocarditis) and 10–15 mg/L for less severe infections was considered therapeutic.2 All of the patients received 15–20 mg/kg (as actual body weight) as an initial dose and some patients received a loading dose of vancomycin 25–30 mg/kg (based on actual body weight).5 The outcomes of the study were 1) achieving therapeutic level in the initial trough level of vancomycin and 2) all cause 30-day mortality.
A total of 456 ICU patients presented between the study period (Figure 1). As per the study subject definition, the authors excluded 109 patients who had vancomycin treatment for less than 3 days, 44 no vancomycin trough levels readings, and two who had contaminated samples from the Microbiology lab report. Hence, 301 were eligible and therefore included in the analysis.
 |
Figure 1 The inclusion and exclusion criteria used during the screening process. |
Statistical Analysis
Data were analyzed using SAS software for Windows version 9.4 (SAS Corp., Cary, NC, USA). Data were summarized as means with standard deviations (SD) and frequencies with percentages as appropriate. Chi-square test will be reported to test whether severity of infection is associated with achieved initial vancomycin trough levels. A stepwise binary logistic regression model was performed to identify factors associated with initial vancomycin trough levels. The effect estimate was reported as odds ratio (OR) and adjusted odds ratio (aOR). The Hosmer-Lemeshow test was used to assess the goodness-of-fit of the final model. A stepwise Cox proportional hazards regression model was constructed to identify factors associated with 30-day mortality and an effect estimate was reported as a hazard ratio (HR) and adjusted hazard ratio (aHR). All tests were two-sided and a P≤0.05 was considered significant.
Results
A total 301 critically ill patients with gram-positive infections were included in the analysis. The characteristics of the study patients are presented in Table 1. Briefly, 66.1% were males, mean (SD) age was 60 (20) years, mean weight was 69 kg (21.5), and 60.5% had at least one preexisting comorbidity. At baseline, mean (SD) APACHE II score was 15.9 (7.11), GCS score 9.2 (4.7), and 64.8% received invasive mechanical ventilation. The majority of patients (n=168, 55.8%) achieved initial therapeutic vancomycin trough levels (61 patients had severe infection, 107 had other infection); and 133 patients (44.2%) did not achieve initial therapeutic trough levels (39 patients had severed infection, 94 had other infection) (P=0.201). The bar chart in Figure 2 describes patients who reached initial therapeutic trough level by age groups.
 |
Table 1 Sample Characteristics (n=301) |
 |
Figure 2 Patient who reached the target trough in initial vancomycin trough by age groups. |
Table 2 depicts the results of the bivariate analysis of factors associated with the initial therapeutic vancomycin trough levels (within range). More importantly, the factors associated with initial vancomycin therapeutic trough levels on the multivariable logistic regression analysis were female gender (aOR=2.575, 95% CI=1.371–4.834), age (aOR=1.024, 95% CI=1.007–1.040), receiving a loading dose (aOR=2.445, 95% CI=1.112–5.377), having bacteremia (aOR=2.061, 95% CI=1.139–3.729), and platelet count (aOR=1.003, 95% CI=1.001–1.005) (Table 3). Additionally, estimated glomerular filtration rate (aOR=0.993, 95% CI=0.987–1.000) and albumin levels (aOR=0.944, 95% CI=0.902–0.988) were associated with lower odds of initial therapeutic vancomycin trough levels (Table 3). The goodness-of-fit indicates that the model fits the data well (P-value of Hosmer and Lemeshow test=0.820).
 |
Table 2 Bivariate Analyses of Factors Associated with the Initial Vancomycin Trough Levels (Within Range) |
 |
Table 3 Multivariate Analysis of Factors Associated with Achieve Initial Vancomycin Trough Levels (Within Range) |
The 30-day mortality rate of the patients were 57 (18.9%). Bivariate analysis of factors associated with the risk of 30-day mortality are shown in Table 4. On multivariate analysis, factors associated with the risk of 30-day mortality were: female gender (aHR=2.630, 95% CI=1.446–4.782), weight (aHR=1.021, 95% CI=1.010–1.031), cancer (aHR=4.429, 95% CI=2.259–8.684), and APACHE II score (aHR=1.068, 95% CI=1.027–1.110) (Table 5). Failure to achieve therapeutic level was associated with an increased 30-day mortality risk only on the bivariate analysis. According to the Kaplan Meier analysis (Figure 3), the probability of survival differed significantly by cancer.
 |
Table 4 Bivariate Analyses of Factors Associated with the Risk of 30-Day Mortality in Patients Who Received Vancomycin |
 |
Table 5 Multivariate Analysis of Factors Associated with the Risk of 30-Day Mortality in Patients Who Received Vancomycin |
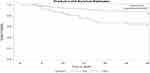 |
Figure 3 30-day survival curves by cancer. |
Discussion
This research outlines the potential benefit of early vancomycin individualized dose in critically ill adult patients with gram positive infections. In the present study, being female, age, loading dose, bacteremia, low eGFR, high platelets, and low albumin were associated with achieving initial therapeutic vancomycin trough levels. Also, being female, weight, cancer, and APACHE II (increased illness severity scores) were associated with 30-day mortality.
The failure to achieve a therapeutic level of vancomycin is common and may be associated with treatment failure.21 Walraven et al22 found that in MRSA bacteremia caused by endocarditis or pneumonia, vancomycin failure was common, reaching 48.2%. Moise et al23 also illustrated that MRSA bloodstream isolates could have decreased sensitivity to vancomycin in vitro in patients previously treated with vancomycin within 30 days. A study suggested that initial vancomycin dose with a loading dose for MRSA bacteremia may decrease clinical failures without increasing toxicity.24 We found that the initial vancomycin trough level was within the target range in 55.8% of patients in the ICU with gram positive infections.
A standardized loading dosage can be used as a simple and safe way that can improve the acquisition of therapeutic vancomycin levels in critically ill patients.16–18 However, there are factors that may affect vancomycin dosing in the ICU. Legal and Wan25 illustrated that young patients require more frequent administration of the vancomycin dosage than older patients. The findings also indicated that females had more chances to reach the therapeutic level as compared with males, which was confirmed by O’Donnell et al's26 results. A study found patients with severe hypoalbuminemia (<25 g/L) may not require a loading dose to achieve the therapeutic vancomycin level as they had high vancomycin trough levels after vancomycin loading.27 Besides, a lower estimated glomerular filtration rate has been associated with elevated vancomycin level.28 A recent review shows an association between the highest trough level of vancomycin and thrombocytopenia.29 However, the platelet counts might be a surrogate of organ dysfunction or disease severity.30 Aubron et al31 indicated that peak and trough concentration was lower in patients with severe organ dysfunction. In this current study, we found that female gender, increasing age, receiving a loading dose, having bacteremia, platelet count, lower estimated glomerular filtration rate, and albumin levels were associated with initial therapeutic vancomycin trough levels.
We found that female gender, weight, cancer, and APACHE II score were associated with 30-day mortality in ICU patients with gram positive infections. Female gender has been found to be an independent predictor of ICU mortality for patients with severe sepsis.32 Having an initial therapeutic vancomycin level was not associated with 30-day mortality. There are many potential explanations for this finding. First, we only evaluated the initial vancomycin level; second, only one quarter of our patients had MRSA; and, third, patients may already had been on another antibiotic (such as a beta lactam) to which the bacteria were susceptible.
There are several limitations in this study. These include that a small sample size was used; the research was conducted at a single center and was further limited to only adult ICU population; and a retrospective design without control group was employed. Besides, data on concomitant antibiotics were absent, vancomycin peak levels were not performed, and there were a lot of monitoring skips. However, the current study is important as it marks the first recent study on factors affecting reaching therapeutic vancomycin levels in Saudi Arabia. Therefore, future research should consider investigating the same research objectives but with a broader scope, that is using a larger sample size and multiple sites. Researchers can also examine the pathogen relationship with vancomycin level and also calculate the daily area under the curve and further reassessit with the identified factors.
Conclusion
Our study found that achieving an initial therapeutic vancomycin trough level in critically ill patients with gram positive infection was associated with older age, female gender, loading dose, bacteremia, high platelets count, low estimated glomerular filtration rate, and low albumin level. Factors associated with 30-day morality for patients who received vancomycin with gram positive infection were being female, weight, cancer, and increased APACHE II score. Markedly, cancer had the highest impact on the patient’s survival rate. These factors should be considered in management of critically ill patients with severe infections caused by gram positive bacteria. Further studies with a larger sample size and multiple sites are required to confirm our findings.
Abbreviations
VIS, vasoactive-inotropic score; APACHE, Acute Physiology Assessment and Chronic Health Evaluation II; MV, mechanical ventilation; MRSA, methicillin-resistant staphylococcus aureus; MSSA, methicillin-susceptible staphylococcus aureus; GCS, Glasgow coma scale.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
This research was approved by King Abdullah International Medical Research Center IRB; SP19/025/R. All patient data accessed complied with relevant data protection and privacy regulations.
Acknowledgments
The authors would like to acknowledge Nadin Al-Anazi (Pharmacist in King Abdulaziz Medical City, Riyadh) for helping in collecting the research data.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research did not receive any funding.
Disclosure
The authors declare that they have no competing interests for this work.
References
1. Hammes WP, Neuhaus FC. On the mechanism of action of vancomycin: inhibition of peptidoglycan synthesis in Gaffkya homari. Antimicrob Agents Chemother. 1974;6(6):722–728. doi:10.1128/AAC.6.6.722
2. Martin JH, Norris R, Barras M, et al. Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society Of Infectious Diseases Pharmacists. Clin Biochem Rev. 2010;31(1):21.
3. Rybak MJ, Le J, Lodise TP, et al. Therapeutic monitoring of vancomycin for serious methicillin-resistant Staphylococcus aureus infections: A revised consensus guideline and review by the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, the Pediatr. Am J Heal Pharm. 2020;77(11):835–864.
4. Álvarez R, Cortés LEL, Molina J, Cisneros JM, Pachón J. Optimizing the clinical use of vancomycin. Antimicrob Agents Chemother. 2016;60(5):2601–2609.
5. Rybak M, Lomaestro B, Rotschafer JC, et al. Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Am J Heal Pharm. 2009;66(1):82–98. doi:10.2146/ajhp080434
6. Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis. 2011;52(3):e18–e55.
7. Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43(3):304–377.
8. Koliha K, Falk J, Patel R, Kier K. Comparative evaluation of pharmacist-managed vancomycin dosing in a community hospital following implementation of a system-wide vancomycin dosing guideline. J Pharm Pharmacol. 2017;5:607–615.
9. Barceló-Vidal J, Rodríguez-García E, Grau S. Extremely high levels of vancomycin can cause severe renal toxicity. Infect Drug Resist. 2018;11:1027. doi:10.2147/IDR.S171669
10. de Almeida CDC, Silva ACS, de Queiroz OJA, et al. Vancomycin-associated nephrotoxicity in non-critically ill patients admitted in a Brazilian public hospital: A prospective cohort study. PLoS One. 2019;14(9):9. doi:10.1371/journal.pone.0222095
11. Jeffres MN. The whole price of vancomycin: toxicities, troughs, and time. Drugs. 2017;77(11):1143–1154. doi:10.1007/s40265-017-0764-7
12. Ye Z-K, Tang H-L, Zhai S-D. Benefits of therapeutic drug monitoring of vancomycin: a systematic review and meta-analysis. PLoS One. 2013;8(10):10. doi:10.1371/journal.pone.0077169
13. Mahmoodian A, Abbasi S, Farsaei S. A new approach to Vancomycin utilization evaluation: A cross-sectional study in intensive care unit. J Res Pharm Pract. 2016;5(4):279. doi:10.4103/2279-042X.192453
14. Obara VY, Zacas CP, de Maio Carrilho CMD, Delfino VDA. Currently used dosage regimens of vancomycin fail to achieve therapeutic levels in approximately 40% of intensive care unit patients. Rev Bras Ter Intensiva. 2016;28(4):380. doi:10.5935/0103-507X.20160071
15. Dib JG, Al-Tawfiq JA, Al Abdulmohsin S, Mohammed K, Jenden PD. Improvement in vancomycin utilization in adults in a Saudi Arabian Medical Center using the Hospital Infection Control Practices Advisory Committee guidelines and simple educational activity. J Infect Public Health. 2009;2(3):141–146. doi:10.1016/j.jiph.2009.07.002
16. Wang J-T, Fang C-T, Chen Y-C, Chang S-C. Necessity of a loading dose when using vancomycin in critically ill patients. J Antimicrob Chemother. 2001;47(2):246. doi:10.1093/jac/47.2.246
17. Truong J, Levkovich BJ, Padiglione AA. Simple approach to improving vancomycin dosing in intensive care: a standardised loading dose results in earlier therapeutic levels. Intern Med J. 2012;42(1):23–29. doi:10.1111/j.1445-5994.2011.02459.x
18. Reardon J, Lau TTY, Ensom MHH. Vancomycin loading doses: a systematic review. Ann Pharmacother. 2015;49(5):557–565. doi:10.1177/1060028015571163
19. van Hal SJ, Jones M, Gosbell IB, Paterson DL. Vancomycin heteroresistance is associated with reduced mortality in ST239 methicillin-resistant Staphylococcus aureus blood stream infections. PLoS One. 2011;6(6):6. doi:10.1371/journal.pone.0021217
20. Holmes NE, Turnidge JD, Munckhof WJ, et al. Vancomycin AUC/MIC ratio and 30-day mortality in patients with Staphylococcus aureus bacteremia. Antimicrob Agents Chemother. 2013;57(4):1654–1663. doi:10.1128/AAC.01485-12
21. Shahrami B, Najmeddin F, Mousavi S, et al. Achievement of vancomycin therapeutic goals in critically ill patients: early individualization may be beneficial. Crit Care Res Pract. 2016;2016.
22. Walraven CJ, North MS, Marr-Lyon L, Deming P, Sakoulas G, Mercier R-C. Site of infection rather than vancomycin MIC predicts vancomycin treatment failure in methicillin-resistant Staphylococcus aureus bacteraemia. J Antimicrob Chemother. 2011;66(10):2386–2392. doi:10.1093/jac/dkr301
23. Moise PA, Smyth DS, El-Fawal N, et al. Microbiological effects of prior vancomycin use in patients with methicillin-resistant Staphylococcus aureus bacteraemia. J Antimicrob Chemother. 2008;61(1):85–90. doi:10.1093/jac/dkm445
24. Ortwine JK, Zasowski EJ, Pogue JM, et al. Relationship Status between Vancomycin Loading Dose and Treatment Failure in Patients with MRSA Bacteremia: it’s Complicated. Infect Dis Ther. 2019;8(4):627–640. doi:10.1007/s40121-019-00268-3
25. Legal M, Wan M. Influence of age on frequency of vancomycin dosing. Can J Hosp Pharm. 2010;63(1):13.
26. O’Donnell JN, Rhodes NJ, Miglis CM, et al. Doses, durations, and gender predict vancomycin-induced kidney injury in pre-clinical studies. Int J Antimicrob Agents. 2018;51(2):239. doi:10.1016/j.ijantimicag.2017.08.012
27. Kovacevic T, Miljkovic B, Mikov M, et al. The Effect of Hypoalbuminemia on the Therapeutic Concentration and Dosage of Vancomycin in Critically Ill Septic Patients in Low-Resource Countries. Dose-Response. 2019;17(2):1559325819850419. doi:10.1177/1559325819850419
28. Zonozi R, Wu A, Shin J-I. et al., Elevated vancomycin trough levels in a tertiary health system: frequency, risk factors, and prognosis. In: Mayo Clinic Proceedings. Vol. 94. Elsevier; 2019:17–26.
29. Mohammadi M, Jahangard-Rafsanjani Z, Sarayani A, Hadjibabaei M, Taghizadeh-Ghehi M. Vancomycin-induced thrombocytopenia: a narrative review. Drug Saf. 2017;40(1):49–59. doi:10.1007/s40264-016-0469-y
30. Greco E, Lupia E, Bosco O, Vizio B, Montrucchio G. Platelets and multi-organ failure in sepsis. Int J Mol Sci. 2017;18(10):2200. doi:10.3390/ijms18102200
31. Aubron C, Corallo CE, Nunn MO, Dooley MJ, Cheng AC. Evaluation of the accuracy of a pharmacokinetic dosing program in predicting serum vancomycin concentrations in critically ill patients. Ann Pharmacother. 2011;45(10):1193. doi:10.1345/aph.1Q195
32. Sakr Y, Elia C, Mascia L, et al. The influence of gender on the epidemiology of and outcome from severe sepsis. Crit Care. 2013;17(2):R50. doi:10.1186/cc12570
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
