Back to Journals » Open Access Emergency Medicine » Volume 15
Validity of TIMI Risk Score and HEART Score for Risk Assessment of Patients with Unstable Angina/Non-ST Elevation Myocardial Infarction Presented to an Emergency Department in Jordan
Authors Ababneh MJ , Smadi MM , Al-Kasasbeh A, Jawarneh QA , Nofal M, El-Bashir M, Jarrah MI , Raffee LA
Received 9 September 2023
Accepted for publication 9 December 2023
Published 18 December 2023 Volume 2023:15 Pages 465—471
DOI https://doi.org/10.2147/OAEM.S439423
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Hans-Christoph Pape
Muhannad J Ababneh,1 Mahmoud Mustafa Smadi,2 Abdullah Al-Kasasbeh,1 Qutaiba Ali Jawarneh,3 Mohammad Nofal,3 Mohanad El-Bashir,4 Mohamad Ismail Jarrah,1 Liqaa A Raffee5
1Division of Cardiology, Department of Internal Medicine, Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan; 2Department of Mathematics and Statistics, Jordan University of Science and Technology, Irbid, Jordan; 3Department of Internal Medicine, Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan; 4Faculty of Nursing, Jordan University of Science and Technology, Irbid, Jordan; 5Department of Accident and Emergency Medicine, Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan
Correspondence: Muhannad J Ababneh, Division of Cardiology, Department of Internal Medicine, Faculty of Medicine, Jordan University of Science and Technology, P.O.Box 3030, Irbid, 22110, Jordan, Tel +962799964654, Fax +962 2 7095010, Email [email protected]
Purpose: To examine the validity and predictability of thrombolysis in myocardial infarction (TIMI) risk and HEART scores in patients presenting to the emergency department (ED) with chest pain in Jordan (representative of the Middle East and North Africa Region, MENA).
Patients and Methods: Risk scores were calculated for 237 patients presenting to the ED with chest pain. Patients were followed-up prospectively for the need for percutaneous coronary intervention, major adverse cardiovascular events, and all-cause mortality, looking for correlation and accuracy between the predicted cardiovascular risk from TIMI risk score and HEART score and the clinical outcome.
Results: Of the 237 patients, approximately 77% were diagnosed with unstable angina and 23% diagnosed with non-ST elevation myocardial infarction (NSTEMI). about two thirds of the study population were smokers and known to have hypertension and dyslipidaemia. In 50 patients, the primary outcome (need for percutaneous coronary intervention (PCI) and/or major adverse cardiovascular events (MACE) at days 14 and 40, all-cause mortality) was observed. Regarding the predictability of the TIMI score, a larger number of events were observed in the study population than predicted. Patients with TIMI scores of 3 to 5 have about a 5– 8% higher event rate than predicted.
Conclusion: Both TIMI and HEART risk scores were able to predict an elevated risk of major cardiovascular adverse events (MACE). The overall impression was that the TIMI risk score tended to underestimate risk in the study population.
Keywords: acute coronary syndrome, risk stratification, cardiovascular diseases, emergency department
Introduction
Cardiovascular diseases encompass a wide spectrum of disorders including coronary heart disease, cerebrovascular disease, peripheral arterial disease, rheumatic heart disease, congenital heart disease, deep vein thrombosis, and pulmonary embolism. Cardiovascular diseases are globally the leading cause of mortality, with approximately 85% of deaths attributed to acute coronary syndrome and cerebrovascular disease.1
Acute coronary syndrome (ACS) is a major presentation of coronary heart disease (CAD) which is further classified into unstable angina (UA), non-ST-elevation myocardial infarction (NSTEMI), and ST-elevation myocardial infarction (STEMI). All three entities commonly present with chest pain.
Chest pain remains one of the most common presenting symptoms in the emergency department (ED) and effective risk stratification plays a pivotal role in the management and prediction of patients in this context. The introduction of high-sensitivity cardiac troponin (hs-cTn) facilitated the identification of patients with different levels of risk for acute coronary syndrome; however, the implication of clinical risk scores alongside laboratory testing improved the risk stratification and allowed a faster triage of patients, particularly recognizing those with very low risk.2,3
Many clinical tools were designed to figure out patients with unfavorable outcomes. Risk score tools based on patient history and findings at presentation are commonly used in the setting of acute chest pain in the emergency department. Commonly used are GRACE (Global Registry of Acute Coronary Events), TIMI (Thrombolysis in myocardial infarction), and HEART (History, Electrocardiogram, Age, Risk factors, and Troponin) scoring systems to stratify the risk for adverse events and mortality in these patients.4
Thrombolysis in myocardial infarction (TIMI) and HEART scores for predicting major cardiac events are widely used for risk stratification and therapeutic decision-making.5 The validity of these scoring systems has been well-examined in several studies in North and South America, Europe, New Zealand, and Australia, but little is known about the validity of these risk scores in the Middle East and North Africa (MENA) region.
This study aims to evaluate the validity of TIMI and HEART risk scores in patients presenting with chest pain at the Emergency Department (ED) at King Abdullah University Hospital (KAUH) in northern Jordan. The objective includes a comparative analysis of both risk scores and an assessment of their predictive values in the study population.
TIMI score incorporates seven parameters: age >65, severe angina in the last 24 h, history of aspirin use in the last seven days, presence of at least three CAD risk factors (diabetes mellitus, hypertension, smoking, or a family history of heart disease), known CAD with stenosis >50%, electrocardiogram (ECG) changes, and positive cardiac enzymes.6 Each parameter corresponds to a single point. A score from zero to two was considered low risk, three to five was intermediate risk, and six or seven was considered high risk. Risk was calculated as the percentage of possible events (predicted major cardiovascular adverse events, MACE). This represents the possibility of myocardial infarction (new or recurrent) or severe ischemia requiring urgent revascularisation or death from any cause over the next 14 days.
The HEART score predicts the 6-week risk of major cardiovascular events. Based on history, ECG findings, age, risk factors, and initial troponin levels. Patients score 0–2 points for each parameter, with a maximum score of 10.
Regarding the HEART score, the sample was divided into three groups: low-, intermediate-, and high-risk. Risk group definition by HEART score: low-risk group (0–3 points), intermediate-risk group (4–6 points), and high-risk group (7–10 points).7
The follow-up endpoint is set at the 14th day for the TIMI score and on day 40 for the HEART score.
Materials and Methods
Participants
This prospective observational cohort study was conducted at King Abdullah University Hospital (KAUH) in north Jordan. After obtaining institutional IRB approval for this prospective observational study, each participant signed a consent form permitting the use of their data for study purposes. Patient enrolment was conducted from July 2021 to January 2022 and included 237 patients. KAUH is a general public health hospital and contains a specialised cardiac centre that provides 24 hour service for percutaneous coronary intervention (PCI) with cardiac surgery on board. The hospital serves as a referral tertiary hospital in four governorates in the north of Jordan, which serves about 3 million people (about one-third of Jordan’s total population), with about 400 patients visiting the emergency department daily.8
Any patient who presented to the ED with chest pain, aged >18 years, for whom an ECG was performed and cardiac enzymes were measured in the hospital were eligible for this study. Patients with STEMI and those who did not fulfil the criteria required to calculate the TIMI UA/NSTEMI and HEART scores were excluded.
Data Acquisition and Management
The following parameters were collected: patient age, sex, presenting complaint, duration, comorbidities, medication history, smoking habits, family history of CAD, physical examination with vital signs at the ED, outpatient clinics and inpatient wards, ECG findings, cardiac enzymes, HbA1c, lipid profile, previous cardiac catheterisation results (if applicable), serum creatinine level, medical record number of the patient, and contact details. On days 14 and 40, the patients were followed up for any complications throughout the study period, adverse cardiovascular events, the need for revascularization, and death.
These data were collected directly from the patients and their medical records. Patient follow-up was performed via phone calls to obtain information about hospitalisation in other hospitals, PCI, and the occurrence of major cardiovascular events. The primary endpoint was to compare the predicted risk scores with observed events. To compare the weight of each risk factor on the score and its correlation with the actual occurrence of events, the frequencies and percentages of each CAD risk factor for males and females, were calculated, namely, smoking, family history, diabetes mellitus (DM), hypertension (HTN), dyslipidaemia, and cerebrovascular accidents (CVA).
The counts for each TIMI scores (0–7) and MACE versus risk factors, and sex are presented in Table 1.
 |
Table 1 Counts Patients with the Primary Outcome (MACE at Day 14) for Every TIMI Score Value Vs Risk Factors and Gender |
Statistical Methodology
Statistical analysis were performed the Statistical Package for Social Sciences software, SPSS version 22 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were used to summarise and determine patient characteristics and the distribution of patient data. Among the descriptive statistics, we determined the range, mean, standard deviation (SD), and median for the continuous variables and counts, percentages, and cross-tabulation for the categorical variables. In addition, visual examination of the data was performed using clustered bar charts and side-by-side box plots. Inferential statistics were used to assess associations between categorical variables and group comparisons between quantitative variables.
Results
This study involved 237 patients who attended the ED with chest pain. Out of the total participants, 54 were female, constituting 22.8% of the sample, with an average age of 58.0 years. The remaining 183 participants were male, representing 77.2% of the sample, and had an average age of 52.8 years. Among the entire group, 77 (32.5%) individuals had a known history of coronary artery disease (CAD).
Table 2 shows the frequencies and percentages of cardiovascular risk factors in males and females (defined by TIMI score). Smoking, hypertension, and dyslipidemia were present in almost two-thirds of the patients. In contrast to smoking and dyslipidemia in male patients, hypertension and diabetes were more common in females.
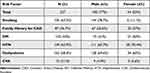 |
Table 2 Frequencies and Percentages of Cardiovascular Risk Factors as Defined by TIMI Score for Males and Females |
Table 3 shows frequencies and percentages of attributes defining the TIMI score. About 77% of the patients were diagnosed with UA and 23% were diagnosed with NSTEMI. Regarding TIMI risk score follow-up at 14 days, 5 patients were excluded due to follow-up loss. In 45 participants (19%) the primary endpoint was recorded (PCI, MACE, or death). Regarding deaths, two patients died on day 14, and one more death case during the 40-day observation period, their TIMI scores were higher than 4.
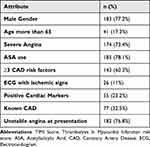 |
Table 3 Frequencies and Percentages of Attributes Defining the TIMI Score |
Out of the 106 patients who underwent catheterization, 11 belonged to the low-risk group, while 95 were in the high-risk group. The positive predictive value for coronary artery disease (CAD) was 2 in the low-risk group and 66 in the higher-risk group, corresponding to percentages of 4.9% and 32%, respectively. After 40 days of observation among the cohort with the primary outcome, 46 patients underwent percutaneous coronary intervention (PCI), and 4 underwent coronary artery bypass grafting (CABG), resulting in one mortality. In total, there were three recorded death cases. Patients with more than one outcome were counted once.
As predicted by the TIMI score, a direct correlation between the increasing score and primary outcome was observed. Table 1 shows the event rates (MACE) for each TIMI score for each cardiovascular risk factor and sex.
The rate of events correlated with TIMI score is shown in Figure 1.
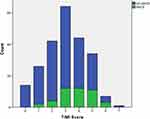 |
Figure 1 Side-by-side Box plot of the TIMI score for the primary outcome of MACE on day 14 compared to patients without events (no MACE). |
Seven patients were excluded from the HEART score, six of whom were lost to follow-up, and one patient lacked an electrocardiogram. By day 40, 50 patients experienced the primary outcome of Major Adverse Cardiac Events (MACE).
Among the categorized risk groups, 52 patients were classified as low risk (HEART scores 0–3), with only 1.9% encountering MACE. The intermediate-risk group, consisting of 135 patients with scores ranging from 4–6, exhibited a 19.9% incidence of MACE. In the high-risk category (HEART scores 7–10), comprising 42 patients, a significant 54.8% recorded positive outcomes related to MACE.
In Table 4 and Table 5, the occurrence of MACE in the study population is compared to the standard rates predicted by the TIMI risk score and HEART score, respectively.6,7
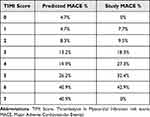 |
Table 4 Comparison of the Predicted Events Calculated by TIMI Score with the Events Recorded at 14 Days (MACE 14 Days) |
 |
Table 5 Comparison of the Predicted Events Calculated by HEART Score with the Events Recorded at 40 Days (MACE 40 Days) |
Discussion
The TIMI risk and heart scores have been widely used in clinical practice to aid physicians in managing patients presenting with chest pain and providing information about mortality and morbidity rates after presentation. Higher rates of adverse events in patients with acute coronary syndrome (ACS) with low TIMI scores were previously observed in the Middle Eastern population.9
The validity of these risk scores has been examined in different populations, but little is known about the validity of the MENA region population; therefore, in this study, we compared the statistics of the original studies with our study population.
The TIMI risk score was based on the age of the patient, severe angina in the last 24 hours, history of aspirin use in the last 7 days, presence of CAD risk factors, known CAD with stenosis >50%, ECG changes, and positive cardiac enzymes. These are the parameters that any physician will look for when dealing with patients presenting with chest pain, making this score an easy-to-use tool with great availability of needed information. The TIMI risk score was valid for predicting outcomes (death, MI, or revascularization) in our population. The recorded events in patients with TIMI score of 1–6 were slightly higher than the standard, indicating that the TIMI risk score probably underestimates the risk of MACE in this group of patients. For patients with TIMI scores of 0 and 7, the small sample size made the comparison unreliable.
The outcome of the HEART score was recorded 40 days after enrolment. The HEART score considers the patient’s age, history of presenting illness, presence of risk factors, ECG changes, and initial troponin levels. Three patients died during the observation period. The percentage of MACE in the three risk groups is shown in Table 5 and was comparable to the standard.
Another prospective study conducted on the Jordanian population concluded that patients with higher TIMI risk scores have an increased cardiac risk;9 however, a study conducted on the Saudi population to assess the validity of the TIMI risk score found no correlation between the increasing TIMI risk score and in-hospital mortality.10 Generally, the application of risk scores for chest pain patients in the Emergency Department (ED) has demonstrated reliability, with various scoring systems such as TIMI, HEART, and GRACE exhibiting differences in predictability.
Artificial intelligence systems have the potential to eliminate the necessity for traditional scores as they can provide more precise prognostic information. This paradigm shift is exemplified in the realm of AI and machine learning (ML) systems.11
It is crucial to emphasize that risk stratification scores and any emerging tools employed in cardiology for risk assessment should be utilized alongside clinical judgment and other pertinent information. These tools are intended to complement, not replace, the expertise and decision-making of a human doctor.
Limitations
Despite the limitations of the small sample size and the fact that the study was conducted at a single center, this study was able to provide insights into the reliability of both TIMI and HEART scores in predicting outcomes in patients with chest pain.
Conclusion
In our study, we found that both the TIMI risk score and HEART scores give physicians a quick and easy tool to deal with chest pain in the ED, and both are effective in predicting the outcome; however, when they are compared together, the TIMI score underestimates the risk of MACE in our population, while the HEART score emerges as a more reliable tool for determining subsequent patient management steps.
Cardiac causes of chest pain in low-risk patients, as defined by the HEART score, may be downgraded in the differential diagnoses, moderate-risk patients may need admission, and high-risk patients may benefit from early invasive measures.
Considering the use of the TIMI score in the ED to determine patients with a low risk for adverse events, we found that patients with a TIMI score of one or two points, perceived as low risk, were identified to be at high risk in this study population, emphasizing the need for careful consideration in risk stratification. For high-risk patients with a TIMI score greater than 4, the TIMI score proved reliable, indicating a higher rate of adverse events than anticipated. Furthermore, these findings suggest that patients with high TIMI risk scores may warrant more aggressive treatment, reinforcing the importance of individualized approaches to patient care based on robust risk assessments.
Ethics Statement
The collection and use of patients’ data was approved by the Institutional Review Board (IRB) of Jordan University of Science and Technology (JUST) and King Abdullah University Hospital (KAUH). Written informed consent for participation was obtained before recruitment in accordance with the national legislation and the institutional requirements. We explicitly confirm that our study adheres to the principles outlined in the Declaration of Helsinki.
Disclosure
All authors declare that they have no conflicts of interest.
References
1. Cardiovascular disease. Available form: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds).
2. Body R, Carley S, McDowell G, et al. Rapid exclusion of acute myocardial infarction in patients with undetectable troponin using a high-sensitivity assay. J Am Coll Cardiol. 2011;58(13):1332–1339. Erratum in: J Am Coll Cardiol. 2012 Sep 18;60(12):1122. PMID: 21920261. doi:10.1016/j.jacc.2011.06.026
3. Chapman AR, Hesse K, Andrews J, et al. High-sensitivity cardiac troponin i and clinical risk scores in patients with suspected acute coronary syndrome. Circulation. 2018;138(16):1654–1665. doi:10.1161/CIRCULATIONAHA.118.036426
4. Sakamoto JT, Liu N, Koh ZX, et al. Comparing HEART, TIMI, and GRACE scores for prediction of 30-day major adverse cardiac events in high acuity chest pain patients in the emergency department. Int J Cardiol. 2016;221:759–764. PMID: 27428317. doi:10.1016/j.ijcard.2016.07.147
5. Khan R, Zarak MS, Munir U, Ahmed K, Ullah A. Thrombolysis in Myocardial Infarction (TIMI) risk score assessment for complications in acute anterior wall ST elevation myocardial infarction. Cureus. 2020;12(6):e8646. doi:10.7759/cureus.8646
6. Antman EM, Cohen M, Bernink PJ, et al. The TIMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision making. JAMA. 2000;284(7):835–842. PMID: 10938172. doi:10.1001/jama.284.7.835
7. Six AJ, Backus BE, Kelder JC. Chest pain in the emergency room: value of the HEART score. Neth Heart J. 2008;16(6):191–196. doi:10.1007/BF03086144
8. Department of statistics. Available form: http://dosweb.dos.gov.jo/.
9. Hammoudeh A, Saleh A, Hamam I, et al. The prognostic implications of TIMI risk scores in Jordanian patients with acute coronary syndrome. results from the glucometabolic abnormalities in acute coronary Syndrome in Jordan (GLORY) Study. Jordan Med J. 2012;46:1.
10. Al-Bugami S, Al-Husayni F, Alamri S, et al. Thrombolysis in myocardial infarction (TIMI) risk score validation in Saudi Arabia. Curr Res Cardiol. 2018;5(1):4–8. doi:10.4172/2368-0512.1000101
11. Hayıroğlu Mİ, Altay S. The role of artificial intelligence in coronary artery disease and atrial fibrillation. Balkan Med J. 2023;40(3):151–152. PMID: 37025078. doi:10.4274/balkanmedj.galenos.2023.06042023
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
