Back to Journals » Clinical Ophthalmology » Volume 17
Validity of an Ocular Emergency Triage System Compared to the Existing Grading System at the Emergency Unit of a Tertiary Eye Hospital in Saudi Arabia
Authors AlSamnan M, AlAmry M, aldossari S, Talea M, Khandekar R , AlGhadeer H
Received 15 November 2022
Accepted for publication 18 January 2023
Published 8 February 2023 Volume 2023:17 Pages 527—534
DOI https://doi.org/10.2147/OPTH.S397504
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mazen AlSamnan,1 Mohammed AlAmry,1 Saif aldossari,2 Mohammed Talea,2 Rajiv Khandekar,3 Huda AlGhadeer1
1Emergency Department, King Khaled Eye Specialist Hospital, Riyadh, Saudi Arabia; 2Ophthalmology Department, King Khaled Eye Specialist Hospital, Riyadh, Saudi Arabia; 3Research Department, King Khaled Eye Specialist Hospital, Riyadh, Saudi Arabia
Correspondence: Huda AlGhadeer, Emergency Department, King Khaled Eye Specialist Hospital, PO Box 7191, Riyadh, 11462, Saudi Arabia, Tel +966 1 4821234 ext. 2500, Email [email protected]
Purpose: To assess true ocular emergencies based on the ocular emergency triage system compared to the existing method of serving patients “first come first serve” by attending ophthalmology resident and review the validity of the triage system by ophthalmic subspecialty.
Methods: In this cross-sectional study of validity, new patients attending the ocular emergency department of a tertiary eye hospital in 2021– 2022 were examined by ophthalmology resident. The time required for registration, an eye exam, and total time in the emergency unit was determined. Using ophthalmic triage criteria, same patients were reviewed by senior ophthalmologist to categorize them as “top emergencies”, “emergencies”, and “not an emergency.” The reviewer was masked about grading by an ophthalmology resident. The agreement rate for true emergencies by both methods of grading was calculated by subspecialty.
Results: One thousand patients with ocular emergencies were evaluated. The median overall time spent in the emergency unit was 92 minutes [interquartile range (IQR): 56; 142]. The revised triage system estimated 85% were “true emergencies.” Using both the revised triage and conventional methods, 172 (17.2%) patients were not considered as having an ocular emergency. The difference in patients grouped into “emergencies” (34.3% vs 21.4%) and “top emergencies” (46.5% vs 60.4%) was significant (P< 0.001) between methods. Uveitis (72%) had the lowest agreement between methods and pediatric ophthalmology (100%) had the highest agreement.
Conclusion: The revised ophthalmic triage system seems to be more efficient than existing method. Subspecialist ophthalmologists may provide quicker and better treatment if ophthalmic emergency patients are prioritized utilizing the proposed redesigned triage method.
Keywords: emergency, eye, ophthalmic, triage
Introduction
The term “triage” is derived from the French word “trier”, which means to choose or sort.1 A significant number of patients presenting to ophthalmic accident and emergency (A&E) departments have non-acute conditions that would be better treated in an ophthalmic outpatient department.2–4 In the absence of a patient prioritizing system, individuals requiring immediate medical and/or surgical attention would be missed among the enormous number of patients waiting in a busy trauma unit. Due to the vast range in the severity of presenting cases and the high patient volume, many ophthalmic units have implemented a triage system that assigns patients to an appropriate category of urgency. An effective triage system can be a cost-effective method for lowering patient wait times while maintaining a high standard of care.5–7 The effectiveness of patient prioritization is dependent upon the training of ophthalmic specialists and the existence of defined criteria for each color-coded emergency eye disease.3,4
A triage system provides a basic framework for dividing all arriving patients into groups using a standard urgency rating scale or structure to expedite the treatment of those with the most serious conditions.1–3 The implementation of a standard triage system facilitates quality improvement in emergency departments by allowing comparisons of important performance indicators (i.e., time-to-treatment by triage category) both within and across emergency departments.8,9 The current study was performed at a tertiary eye hospital in central Saudi Arabia. In the existing system, patients are registered at an emergency unit, attended by an ophthalmology resident on “first come, first serve” basis, and emergency eye care services are provided by experienced eye care specialists. If assistance is needed, the senior ophthalmologist requests the help of subspecialists for further management.
We present the validity of a redesigned triage process in an emergency department compared to the conventional method for ocular emergencies. We also present the perceived ophthalmic emergency score and its determinants as determined by the attending eye care provider.
Methods
The Institutional Review Board of the King Khaled Eye Specialist Hospital approved this research, and this study adhered to the tenets of the Declaration of Helsinki. This research includes patients who presented to the emergency department between June 2021 and June 2022. The study comprised the first five and last five patients on each day of the week, as well as the first 10 patients on weekends, who visited the hospital's emergency department for the first time. It is believed that care differs during different times of the day when ophthalmologists are on duty. To ensure that both fresh-on-duty and tired-on-duty ophthalmologists giving care were adequately covered, we decided to take the first and last few cases of the day. Patients seeking follow-up care at the emergency department were excluded from this study. To calculate the sample size for a cross-sectional study, we estimated that 21% of self-referrals to the eye emergency unit had a real ocular emergency according to the Rome Eye Scoring System for Urgency and Emergency (RESCUE).9 To achieve 95% confidence interval, 3% acceptable error margin and designing factor of 1.5, at least 993 ≅ 1000 participants were required for the study. Open epi software was used to calculate the sample size for this cross-sectional validity study.10
In existing assessment and care system, based on presenting symptoms (mainly pain, redness, and decreased visual acuity), the attending ophthalmology resident classifies the ocular emergency as either a true emergency or a non-emergency. They are supervised by trainee fellow ophthalmologist of different subspecialities. Non-emergent cases are encouraged to visit a regular ophthalmology clinic. The rate of true emergencies by ophthalmic subspecialty (anterior segment, glaucoma, neuro-ophthalmology, oculoplastic, pediatric ophthalmology, uveitis, and vitreoretinal) was also calculated. The ophthalmology resident obtained the patient's history, evaluated the perceived severity of an ophthalmic emergency, and sought assistance from superiors.
In the proposed ophthalmic triage system, the senior ophthalmologist graded same patients retrospectively and assigned a color designation according to the patients estimated ocular severity: red for the most urgent cases, green for semi-urgent, blue for those awaiting availability, and white for non-emergent (non-ER) cases. The reviewer ophthalmologist was masked about the status of ophthalmic emergency as defined by the attending ophthalmology resident. Conditions under the “red” category that warranted urgent attention included, perforating eye injuries,blunt trauma, severe trauma, alkali burns, severe ocular pain, and total hyphema. Patients who have experienced complete/partial loss of visual acuity during the previous 48 hours, are considered to have an urgent ophthalmic presentation and require immediate attention.
Scoring was as follows: a white “non-ER” category was assigned a score of 0 or 1, the semi-urgent blue category was 2; green category was assigned a score of 3 and red was assigned a score of 4 or higher. Only complaints with a duration of 1 week or less were included in the triage procedure for calculating an overall score. Complaints longer than 1 week were excluded. Scores for redness and pain comprised none (0), moderate (1), and severe (2). Vitreoretinal triage was also used for conditions involving the posterior segment of the eye Table 1.
 |
Table 1 Vitreoretinal Triage Adopted in Ophthalmic Emergency Care |
A flow chart explains how two methods of grading ophthalmic emergency were compared in the present study Figure 1.
 |
Figure 1 Flow chart showing the existing system for patients with ocular emergencies and the proposed ophthalmic triage implementation. |
The total waiting time was noted for each patient and group of patients in each color code category. Table 2 presents the times for eye care delivery in these groups, as well as the types of ocular emergencies.
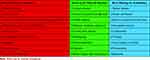 |
Table 2 Ocular Emergency Triage System Proposed for Validity Testing |
To study the internal validation of triaging, 10% of the cases were assessed by two ophthalmologists who graded ocular emergencies without consulting each other. The agreement in grading ocular emergencies was 98%.
Data were collected from the electronic health record of each patient and entered into an Excel® spreadsheet (Microsoft Corp., Redmond, WA, USA). After verification and removal of identifiable patient information, the data were transferred to Statistical Package for Social Studies (SPSS 25; IBM Corp., Armonk, NY, USA) spreadsheet. The number and percentage proportion and 95% confidence intervals were calculated for true ocular emergencies. Normally distributed determinants are presented as mean and standard deviation. Small sample or skewed distributions are presented as median and interquartile range (IQR). The agreement and disagreement rate of the two triaging methods for determining grades of ocular emergencies along with the kappa value were estimated. The nonparametric method and two-sided Kruskal Wallis P value were used to compare time spent in the emergency department by category of ocular emergency. P < 0.05 was considered statistically significant.
Results
The study sample was comprised of 1000 ocular emergency patients. Figure 2 presents the percentage of ocular emergencies by ophthalmic subspecialty. Three-fourth of them were of anterior segment subspeciality. Around 10% emergencies were related to vitro-retinal subspeciality. Hardly 1% of total ocular emergencies were related to pediatric ophthalmology.
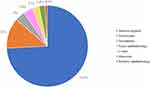 |
Figure 2 Distribution of ocular emergency patients by ophthalmic subspecialties. |
The median wait time for patient registration was 14.4 minutes (IQR 9.5; 19.3). The median duration of an eye exam was 15.5 minutes (IQR 11.2; 20.2). The total median duration in the emergency unit was 92 minutes (IQR 56; 142). Table 3 presents the median and IQR of wait times based on ocular emergency codes. The time spent in the emergency unit was longest for patients graded as non-emergency, while patients with top emergencies spent the shortest time in the ER. We correlated the time spent for registration, examination, and total time in emergency by three grades of emergencies defined by triage system. The time spent in the emergency department varied greatly based on the type of emergency (Kruskal Wallis P = 0.018).
 |
Table 3 Time for Registration, Eye Examination, and Total Time (in Minutes) Spent in the Emergency Unit, as Determined by the Ocular Emergency Triage Coding System |
Table 4 presents the agreement of emergency grading by ophthalmology resident using the existing method to the ophthalmologist’s grading using the revised ophthalmic triage system. The percentage of agreement was 85.1% (95% CI: 82.9–87.3). The rate of disagreement was 13.9% (95% CI: 11.8–16.0) (Kappa = 0.768). The conventional grading method seems effective in identifying non-emergent ophthalmic conditions. The proposed triage proved useful for distinguishing between the most urgent situations and emergencies.
 |
Table 4 Comparison of Grading Emergency Patients Using Ophthalmic Emergency Triage Coding System and Existing Method of Grading Ocular Emergency |
Table 5 presents the agreement, disagreement, and kappa value of grading ocular emergency with both methods based on the subspeciality. Details of validity of anterior segment and vitreoretinal subspeciality are presented in Table 6. The difference in patients grouped into “emergencies” (34.3% vs 21.4%) and “top emergencies” (46.5% vs 60.4%) was significant (P<0.001). Uveitis (72%) had the lowest agreement and pediatric ophthalmology (100%) had the highest agreement.
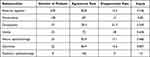 |
Table 5 Agreement of Ocular Emergency Grading by Revised Triage and the Existing Method Among Subspecialties of Ophthalmology |
 |
Table 6 Agreement of Ocular Emergency Grading by Revised Triage and Existing Method for Anterior Segment and Vitreoretinal Subspecialities |
Discussion
The outcomes of this study indicate that using a triage coding method for classifying ophthalmic emergencies allowed for the reclassification of one of every eight emergencies previously classified as top emergencies using the existing system. We found that in the emergency unit of a tertiary eye hospital, the identification of non-emergent patients using the triage coding method and the conventional method was similar. The time spent in the emergency department by patients with ophthalmic conditions varied significantly depending on the ophthalmic emergency triage code. The validity of the ophthalmic triage coding system was highest in pediatric ophthalmology emergencies and lowest in patients with uveitis emergencies.
In the modern era of gaining information via the internet, eye patients and their families seek subspecialist ophthalmologists for eye treatment.11,12 This may also be the case for ocular emergencies arriving at a tertiary eye hospital. Prior research has shown the efficacy of ophthalmic triage.13–17 However, this may be the first research study with a large sample size to emphasize the necessity of subspecialty ophthalmic units being involved in ocular triage coding. Incorporating this ocular triage, particularly for vitreoretinal cases, in addition to anterior segment emergencies, would be useful for ophthalmology residents and ophthalmic nurses working in the emergency units.
In our research, there was 85% agreement between the triage coding system and the conventional system. By using both methods, all non-emergent cases were identified. There was a difference in the classification of emergencies into high emergencies and emergencies. In a study conducted at a different facility in the same city, using a Rome Eye Scoring System for Urgency and Emergency (RESCUE) triage coding system, it was reported that the triaging system had 99% sensitivity and 90% specificity in differentiating urgent and semi-urgent conditions from non-urgent conditions.16 D’Oria et al13 used an alphabetical triage score for ophthalmology (ATSO) and reported 91.4% sensitivity and 98.8% specificity indicating the reliable prediction of ocular emergencies. Rossi et al9 analyzed up to 160,936 ocular emergencies and reported that the Rome Eye System for Scoring Urgency and Emergency (Rescue) was highly reliable for grading ocular emergencies and determining admission for further care.
In our study, the ocular emergency coding system for patients with anterior segment and vitreoretinal disorders was 75% and 80%, respectively. Management of ocular emergencies by subspeciality experts has become easier and more common.8 Consequently, the validity of such a subspecialty triage system is essential for establishing protocols and enhancing education on ophthalmic emergencies. Examples of triage systems to prioritize emergency patient treatment include brain injuries in children and patients at two United Kingdom emergency rooms.18,19
Previous studies indicate that participation of a senior resident in triage significantly improves the emergency department’s performance.20 However, the initiative’s cost-effectiveness must be examined before it can become standard operating practice.20 Although ophthalmologists were engaged in subspecialty eye care in our study, ophthalmologists and subspecialty fellows provided treatment of the main emergency.
The length of patient stays in the emergency unit of our eye hospital was more for non-emergency patients than those with top emergencies. This emphasizes the need to resolve non-emergent cases more rapidly via the rigorous implementation of standard operating procedures. To expedite treatment, we suggest that top emergencies should be exempt from the registration process.
Increasing the number of personnel and resources available to respond to emergencies might minimize waiting times for examination and initial assistance. At the Mayo Clinic in the United States during the COVID-19 pandemic, telephone triage for ocular crises shortened wait times by 43 minutes.21
In another Saudi Arabian facility, a trial incorporation of RESCUE to simplify emergent ophthalmic care of patients, resulted in lowering emergency department wait times from a median of 46 minutes to 33 minutes.16 However, caution is recommended when incorporating initiatives that shorten emergency department wait times. Emergency patients should not be rushed through a comprehensive eye examination, particularly of the contralateral eye.
In all cases of ophthalmic emergency at our institutions, it is difficult to determine the reason for extended waiting and registration times. This is a rich area for study that might potentially save time. There is a propensity for eye patients, particularly those who arrive late for their appointments, to seek eye treatment in emergency departments.
The administration should be strict and encourage eye care professionals to transfer these patients to clinics so that emergency personnel may devote their entire attention and care to patients with actual ocular emergencies.
Due to the cross-sectional nature of this study, there are inherent limitations to be considered. One must be cautious when demonstrating the causal link between an outcome and its determinants. The subsample of subspecialty ocular emergencies was small; thus, it should be considered a trend regarding the validity of ophthalmic triage coding for these subgroups.
Conclusion
We noted that proposed triage system enables eye care providers to differentiate emergencies from top emergencies more effectively. Providing state-of-the-art services in a tertiary eye hospital, particularly in emergency situations, is challenging. Training ophthalmologists, mid-level eye care professionals, and supporting personnel to include adequate explanation and practical training, followed by monitoring and corrective measures, would further improve emergency eye care. Emergency personnel and patients anticipate timely treatment from subspecialists. Implementing subspecialty triage will be aided by more research with larger sample sizes.
Ethical Statement
The study was authorized by the King Khaled Eye Specialist Hospital’s Institutional Review Board and followed the Helsinki Declaration’s tenets. All participants/guardians have provided written informed consent to participate in this study.
Acknowledgment
We would like to thank the research coordinator Mr Faisal Al Hamidi for his help in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Banerjee S, Beatty S, Tyagi A, et al. The role of ophthalmic triage and the nurse practitioner in an eye-dedicated casualty department. Eye. 1998;12(Pt 5):880–882. doi:10.1038/eye.1998.222
2. Bhatt R, Sandramouli S. Evidence-based practice in acute ophthalmology. Eye. 2007;21(7):976–983. doi:10.1038/sj.eye.6702374
3. Bhopal RS, Parkin DW, Gillie RF, et al. Pattern of ophthalmological accidents and emergencies presenting to hospitals. J Epidemiol Community Health. 1993;47(5):382–387. doi:10.1136/jech.47.5.382
4. Chiapella AP, Rosenthal AR. One year in an eye casualty clinic. Br J Ophthalmol. 1985;69(11):865–870. doi:10.1136/bjo.69.11.865
5. Edwards RS. Ophthalmic emergencies in a district general hospital casualty department. Br J Ophthalmol. 1987;71(12):938–942. doi:10.1136/bjo.71.12.938
6. Fenton S, Jackson E, Fenton M. An audit of the ophthalmic division of the accident and emergency department of the Royal Victoria Eye and Ear Hospital, Dublin. Ir Med J. 2001;94(9):265–266.
7. Kirkwood BJ, Pseudovs K, Loh RS, et al. Implementation and evaluation of an ophthalmic nurse practitioner emergency eye clinic. Clin Experiment Ophthalmol. 2005;33(6):593–597. doi:10.1111/j.1442-9071.2005.01101.x
8. Rossi T, Boccassini B, Cedrone C, et al. Testing the reliability of an eye-dedicated triaging system: the RESCUE. Eur J Ophthalmol. 2008;18(3):445–449. doi:10.1177/112067210801800321
9. Rossi T, Boccassini B, Iossa M, et al. Triaging and coding ophthalmic emergency: the Rome Eye Scoring System for Urgency and Emergency (RESCUE): a pilot study of 1000 eye-dedicated emergency room patients. Eur J Ophthalmol. 2007;17(3):413–417. doi:10.1177/112067210701700324
10. Dean AG, Sullivan KM, Soe MM. OpenEpi: open source epidemiologic statistics for public health, version. Available from: www.OpenEpi.com.
11. Subburaman GB, Hariharan L, Ravilla TD, et al. Demand for tertiary eye care services in developing countries. Am J Ophthalmol. 2015;160(4):619–627. doi:10.1016/j.ajo.2015.06.005
12. Kilduff CL, Thomas AA, Dugdill J, et al. Creating the Moorfields’ virtual eye casualty: video consultations to provide emergency teleophthalmology care during and beyond the COVID-19 pandemic. BMJ Health Care Inform. 2020;27(3):125.
13. D’Oria F, Bordinone MA, Rizzo T, et al. Validation of a new system for triage of ophthalmic emergencies: the alphabetical triage score for ophthalmology (ATSO). Int Ophthalmol. 2020;40(9):2291–2296. doi:10.1007/s10792-020-01413-5
14. Marsden J. An evaluation of the safety and effectiveness of telephone triage as a method of patient prioritization in an ophthalmic accident and emergency service. J Adv Nurs. 2000;31(2):401–409. doi:10.1046/j.1365-2648.2000.01285.x
15. Eijk ES, Busschbach JJ, Monteban H, et al. Towards patient self‐triage in the ophthalmic emergency department: sensitivity and specificity of a self‐triage instrument. Acta Ophthalmol. 2014;92(7):697–700. doi:10.1111/aos.12342
16. AlSamnan MS, Mousa A, Al-Kuwaileet S, AlSuhaibani AH. Triaging self-referred patients attending ophthalmic emergency room. Saudi Med J. 2015;36(6):678–684. doi:10.15537/smj.2015.6.11302
17. Deaner JD, Amarasekera DC, Ozzello DJ, et al. Accuracy of referral and phone-triage diagnoses in an eye emergency department. Ophthalmology. 2021;128(3):471–473. doi:10.1016/j.ophtha.2020.07.040
18. de Magalhães-Barbosa MC, Robaina JR, Prata-Barbosa A, et al. Validity of triage systems for paediatric emergency care: a systematic review. Emerg Med J. 2017;34(11):711–719. doi:10.1136/emermed-2016-206058
19. Hinson JS, Martinez DA, Cabral S, et al. Triage performance in emergency medicine: a systematic review. Ann Emerg Med. 2019;74(1):140–152. doi:10.1016/j.annemergmed.2018.09.022
20. Abdulwahid MA, Booth A, Kuczawski M, et al. The impact of senior doctor assessment at triage on emergency department performance measures: systematic review and meta-analysis of comparative studies. Emerg Med J. 2016;33(7):504–513. doi:10.1136/emermed-2014-204388
21. Shah SM, Khanna CL. Ophthalmic emergencies for the clinician. Mayo Clin Proc. 2020;95(5):1050–1058. doi:10.1016/j.mayocp.2020.03.018
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
