Back to Journals » Clinical Interventions in Aging » Volume 18
Validation of Three Tools for Estimating the Risk of Primary Osteoporosis in an Elderly Male Population in Beijing
Authors Lin J, Guo S, Zuo W, Wu H, Li Y, Yang X, Yang Y, Fei Q
Received 27 February 2023
Accepted for publication 10 May 2023
Published 24 May 2023 Volume 2023:18 Pages 845—853
DOI https://doi.org/10.2147/CIA.S410239
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Jisheng Lin,1,* Sijia Guo,1,* Weiyang Zuo,1,* Hao Wu,2 Yongjin Li,3 Xiuquan Yang,4 Yong Yang,1 Qi Fei1,*
1Department of Orthopedics, Beijing Friendship Hospital, Capital Medical University, Beijing, People’s Republic of China; 2Fangzhuang Community Health Service Center, Beijing, People’s Republic of China; 3Tuanjiehu Community Health Service Center, Beijing, People’s Republic of China; 4Wangzuo Community Health Service Center, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Qi Fei, Tel +86 10 6313 8353, Fax +86 10 8391 1029, Email [email protected]
Purpose: This cross-sectional study estimated three clinical tools including the Osteoporosis Self-Assessment Tool for Asians (OSTA), Body Mass Index (BMI), and Beijing Friendship Hospital Osteoporosis Self-assessment Tool for Elderly Male (BFH-OSTM) for identifying primary osteoporosis and found optimal cut-off values in an elderly Han Beijing male population.
Materials and Methods: We conducted a cross-sectional study, enrolling 400 community-dwelling elderly Han Beijing males aged ≥ 50 from 8 medical institutions. Osteoporosis was diagnosed as a T-score of − 2.5 standard deviations or lower than that of the average young adult in different diagnostic criteria [lumbar spine (L1-L4), femoral neck, total hip, WHO]. BFH-OSTM, OSTA, and BMI were assessed for predicting OP by receiver operating characteristic (ROC) curves. Sensitivity, specificity, and areas under the ROC curves (AUC) were determined. Ideal thresholds for the omission of screening BMD were proposed.
Results: The prevalence of osteoporosis ranged from 9.25% to 19.0% according to different diagnostic criteria. The present study indicated the highest discriminating ability was BFH-OSTM in different criteria. The AUCs of OSTA and BMI were 0.748 and 0.770 in WHO criteria, which suggested limiting predictive value for identifying OP in elderly Beijing males. The AUC of BFH-OSTM to predict OP based on WHO criteria was 0.827, yielding a sensitivity of 65.8% and specificity of 82.7%, respectively. With a cost of missing 6.5% of osteoporosis patients, BFH-OSTM could reduce 73.5% of participants in screening BMD tests.
Conclusion: BFH-OSTM may be a simple and effective tool for identifying OP in the elderly male population in Beijing to omit BMD screening reasonably.
Keywords: male, osteoporosis, osteoporosis self-assessment tool for Asians, OSTA, Beijing friendship hospital osteoporosis self-assessment tool for elderly male, BFH-OSTM, body mass index, BMI
Introduction
Osteoporosis (OP) is defined as a metabolic bone disease, characterized by low bone mass and micro architectural deterioration, which has rapidly become a critical health problem because of bone fragility and a higher risk of future fractures.1 Although OP has become a major threat to aging women in terms of morbidity and mortality, it has not been widely recognized as a significant health issue in the aging male population.2 The majority of elderly men who have a previous fragility fracture are not aware of participating in screening bone mineral density (BMD) tests or receiving medical treatment.3 Male osteoporosis is largely neglected in the People’s Republic of China. It is valued to predict the risk of developing OP in elderly males and prevent the first fracture from happening.
A previous study indicates 1% of BMD losses yearly in men since the sixth decade.4 With the development of the economy and medical treatment, the average life expectancy has increased. More and more elderly males are susceptible to osteoporotic fractures. Considering the high prevalence of mortality and disability in men after fractures, early diagnosis and prevention of osteoporosis are crucial to future medication.5
BMD measurement using dual-energy X-ray absorptiometry (DXA) is the current gold standard for diagnosing osteoporosis. According to the World Health Organization (WHO), osteoporosis is defined as a BMD value of less than 2.5 standard deviations (SD) below the mean value at any site of the lumbar spine (L1-L4), femoral neck, or total hip.6 However, there is no uniform standard for diagnosis of male OP currently, previous study has found that BMD at the lumbar spine site declines with age in women, but it does not apply to men.7 Therefore, some scholars hold the opinion that the femoral neck can reflect the bone mineral density of males more precisely.8 Some previous studies have shown that BMD of the femoral neck is better than the lumbar spine to discriminate OP from normal, because calcification of the abdominal aorta and osteoarthritis of the spine can influence BMD at the lumbar spine site.9 However, some guidelines also suggest that the lumbar spine is the preferred site for therapeutic assessment.10 Besides, BMD measurement is expensive and invasive. Some guidelines recommend that men at high risk of OP (aged 70 and above or men aged 50–69 with risk factors) are supposed to take BMD testing by central dual-energy x-ray absorptiometry.11 Considering the great population in China, OP is an important public health problem cause of its high incidence, high mortality, and heavy economic and social burden. So it is necessary to obtain a better method to estimate the risk of OP in the People’s Republic of China. Various OP screening tools have been developed by multiple organizations, such as Osteoporosis Self-assessment Tool for Asians (OSTA), and weight-based criterion.
The Osteoporosis Self-Assessment Screening Tool for Asians (OSTA) is simple and effective screening tools for identifying osteoporosis for post-menopausal women, which also performances well in elderly males.12,13 Although OSTA only includes two factors (age and weight), some validation studies show that compared to other complicated tools, OSTA is more effective. Some researchers have proven that OSTA is useful for diagnosing osteoporosis in Beijing elderly men, especially at the femoral neck site.14
Body Mass Index (BMI) has been used to assess obesity and health in individuals with an international standard. Some studies show that BMI is related to osteoporotic fracture risk.15–17 The results of previous research suggested that low BMI (<20kg/m2) should go for a DXA in women less than 60-year-old.18 The results of many studies have suggested a correlation between BMI and BMD in postmenopausal women.19–22 However, there is not enough evidence to confirm whether BMI is a useful tool in predicting OP in elderly men.
We have developed a clinical screening tool, named Beijing Friendship Hospital Osteoporosis Self-assessment Tool for Elderly Male (BFH-OSTM), based on two clinical risk factors including weight, and the history of fragility fracture. Our previous study has confirmed that it can well identify male osteoporosis, the BFH-OSTM index (cut-off value = 70) has a sensitivity of 85% and specificity of 53% for identifying osteoporosis according to the WHO criteria, with an area under the ROC curve of 0.763.23
Hence, our goal is to compare the validation of BFH-OSTM, OSTA, and BMI in predicting primary osteoporosis, and find suitable thresholds to omit BMD testing reasonably in a community-dwelling elderly male population in Beijing.
Materials and Methods
The Ethics Committee of Beijing Friendship Hospital, Capital Medical University approved this cross-sectional study, and all subjects provided signed informed consent. Our study complied with the Declaration of Helsinki. The flow diagram of the study is shown in Figure 1.
Study Population
The population of this study included Chinese men aged ≥50 years who did not exhibit typical clinical symptoms. Volunteers were recruited and screened out via inclusion and exclusion criteria as follows.
Inclusion criteria: (1) Chinese men aged ≥50 years. (2) Volunteer for this study after the researcher explained the purpose. (3) Conscious, verbal, readable, and able to communicate with investigators without difficulties. (4) Han nationality, and have lived in Beijing for more than 20 years.
Exclusion criteria: (1) History of anti-bone resorptive drugs (ie bisphosphonate, calcitonin, and estrogen) and/or osteogenic drugs (ie fluoride and parathyroid hormone) therapies. (2) History of malignant tumor, bone metastatic tumor, or other endocrine and bone metabolism diseases (eg rheumatoid arthritis, hyperthyroidism, and adrenal diseases). (3) History of severe liver and kidney disease, immobilization for more than 3 months. (4) History of a bilateral hip replacement or fracture. (5) Patients with mental disorders or cognitive impairment.
BMD and T-Score Measurements
All enrolled participants were measured BMD scores at the hip and spine site with DXA equipment by an experienced technologist in the Osteoporosis Clinic of Beijing Friendship Hospital. A well-designed questionnaire was filled out by enrolled participants and necessary information was asked by a trained interviewer. Data about demographics and clinical risk factors were added to the questionnaire properly. Height was measured with a stadiometer (Mahr GmbH, Gottingen, Germany) and weight was measured using an electronic balance (Tanita, Tokyo, Japan). All enrolled participants were wearing light-weight indoor clothing and no shoes during the measurement process.
A DXA equipment (Discovery Wi, QDR series, Hologic, Waltham, MA, USA) was operated by a well-trained technologist to measure the BMD score of the lumbar spine (L1–L4) and left femur (ie the femoral neck, trochanter, Ward’s triangle, and total hip). BMD score of the right femur was measured as a substitution if the left side was previously undergone surgery or fractured. A quality assurance scan was performed every day before each test to standardize measurement. To minimize subjective error, the same well-trained technologist was asked to perform the DXA scan process in this study. The BMD T-score was calculated by software of DXA equipment automatically.
The database was established by two researchers and checked by the senior researcher to confirm its credibility and quality. According to the WHO standards, participants whose BMD T-score at any site (L1–L4, femoral neck, or total hip sites)≤-2.5 was diagnosed with OP, and that between −1 and −2.5 was diagnosed as low bone mass. Diagnosis of OP at each site and whole body were made, respectively.
OSTA Score
The OSTA was calculated based on age and body weight using the following formula:24 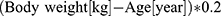 .
.
The decimal digits of the calculation results were then disregarded. For example, 60-year-old men with 48kg weight would have an OSTA index of −2.
BMI
The BMI was calculated based on weight and height using the following formula: 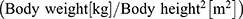 .
.
BFH-OSTM Score
In our previous study, a multivariate regression model was built based on weight and history of the previous fracture, we named it Beijing Friendship Hospital Osteoporosis Self-assessment Tool for Elderly Male (BFH-OSTM). According to the result, the BFH-OSTM may perform well for identifying elderly males at increased risk for osteoporosis, and applying it would result in the more prudent use of BMD measurement by DXA, especially for Han Chinese males. The model was finally calculated using the following formula:23 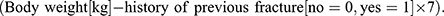
Statistical Analysis
Initial data input and calculation were conducted with Microsoft Excel software ver.2019. Basic descriptive statistical analysis was performed. And the independent-samples Student’s t-test, non-parametric test, and one-way analysis of variance were used for single-factor analysis via SPSS software ver.22.0 (IBM Corporation, Armonk, NY, USA). BMD T-scores at each site were summarized. Then, the performances of three tests (OSTA score, BMI, and BFH-OSTM score) for predicting OP at each site were compared. A receiver operating characteristic (ROC) curve was constructed and the 95% confidence interval (CI) was estimated by MedCalc software ver.11.5.0.0 (MedCalc Software, Ostend, Belgium). The predictive value of the three tools was determined according to the AUC as follows: perfectly predictive, AUC =1; highly predictive, 1>AUC≥0.9; moderately predictive, 0.9>AUC≥0.7; less predictive, 0.7>AUC≥0.5; and non-predictive, AUC<0.5.25 A p-value of <0.01 was considered statistically significant in all statistical analyses.
Results
In our study, 400 participants were selected according to the inclusion and exclusion criteria. The characteristics of the participants are shown in Table 1.
 |
Table 1 Summary of Descriptive Characteristics of the OP and Health Groups (n=400) |
Several differences were detected between OP and non-OP individual groups, including age, weight, height, BMI, alcohol drinking history, and fracture history. Specifically, the mean age was higher and weight was lower in the osteoporosis group. And osteoporosis individuals presented higher rates of history of fractures. Interestingly, the rate of alcohol drinking and smoking history was significantly lower in the osteoporosis group, which may be affected by the small sample size or living habits of the volunteers.
BMD T-Score Analysis and ROC Curves
BMD T-scores of different sites are compared in Table 2. According to the WHO criteria, 19% (n=76) subjects were diagnosed with OP and 42.5% (n=170) subjects were diagnosed with low bone mass. OP morbidity at the total hip, femoral neck, and L1-L4 was 9.25%, 14.0%, and 14.25%, respectively. Three tools were used to predict OP prevalence at a different site and the results are shown in Table 3. At all three sites, the AUC of BFH-OSTM is significantly larger than the others (p<0.01). There is no statistical difference in AUC for estimating the risk of osteoporosis between BMI and OSTA (p=0.8332).
 |
Table 2 OP Diagnosis at Each Site |
 |
Table 3 Cut-off Value and AUC of Three Tools in Predicting OP at Different Sites |
ROC Curve Outcomes
The ROC curves of the three tools for identifying OP in WHO criteria were compared in software shown in Figure 2. AUCs of all three tools were moderately predictive (0.9>AUC>0.7, p<0.01). The cut-off value of the three tools was 63 for BFH-OSTM, 22.49 for BMI, and −1 for OSTA, respectively. BFH-OSTM score showed the highest sensitivity and BMI showed the highest specificity at their cut-off point. In Figure 2, the AUC of BFH-OSTM was significantly larger than that of BMI and OSTA, respectively (BFH-OSTM~BMI: 5.66%, p = 0.0006, BFH-OSTM~OSTA:7.69%, p = 0.0012). AUCs of BMI and OSTA showed no significant difference (BMI~OSTA:2.03%, p = 0.4476).
Lower Thresholds Results
Considering the prevalence of OP in each criteria and previous research reports, we chose the cut-off value in WHO criteria, so they were set as the optimal thresholds. The low-risk thresholds were set at 63 for BFH-OSTM, −1 for OSTA, and 22.49 for BMI. Test performances at those thresholds are summarized in Table 4. As shown in Table 4, compared to the sensitivity and negative predictive value of BMI and OSTA, BFH-OSTM performed better. In WHO criteria, BFH-OSTM had the best predictive value yielding an AUC of 0.827, sensitivity of 65.8%, specificity of 82.7%, negative predictive value of 91.2% and osteoporosis missed of 6.5%.
 |
Table 4 Test Performance in Predicting Osteoporosis at Defined Low-Risk Thresholds |
Discussion
This study compared the performance of BMI, OSTA, and BFH-OSTM for predicting OP in Chinese men aged 50 years or higher, and defined the optimal thresholds so that unnecessary BMD measurement could be avoided as much as possible. In this study, the prevalence of osteoporosis in men ranged from 9.25% to 19.0% according to the different criteria. This is consistent with what has been previously reported. The high prevalence of OP in Chinese elderly men suggests that we urgently need a reliable and easily feasible screening tool to identify the high-risk population of osteoporosis in elderly males.26
There were significantly lower mean height, weight, and BMI in the osteoporosis group than in the non-osteoporosis group as shown in Table 1 (P<0.01). Nevertheless, older average age and a higher number of previous fragility fractures were found in the OP group than in the non-OP group. This was in accordance with the viewpoint of former studies. Further, our results showed lower body height among participants with OP compared to non-OP controls. This could be explained by height loss following vertebral fracture resulting from osteoporosis.
It has been reported that a low BMI was a well-documented risk factor for osteoporotic fracture whereas a body weight increase was considered a protective factor against osteoporosis.27,28 The AUCs of BMI ranged from 0.767 to 0.804 in this study and its predictive efficacy was acceptable. The optimal cut-off value was calculated to be 22.49 according to the WHO standard, yielding a sensitivity of 56.6% and a specificity of 85.8%. When BMI was applied to screen osteoporosis in elderly men, its positive likelihood ratio (+LR) was 3.99, negative likelihood ratio (-LR) was 0.51 and diagnostic odds ratio (DOR) was 9.29. These results indicate that BMI has limited value in predicting osteoporosis in elderly men in Beijing, is not sufficiently reliable and valid, and a tool with a higher sensitivity was required to predict osteoporosis.
OSTA is a simple and effective screening tool for predicting postmenopausal osteoporosis based on weight and age.29 It has been reported to be used in predicting elderly male osteoporosis.30,31 OSTA performed inefficiently in osteoporosis prediction whose AUCs ranged from 0.706 to 0.801 and had the highest levels of identification of osteoporosis in the femoral neck (0.801) better than that in lumbar vertebrae (0.706). The best cut-off value was calculated to be −1, which was same with WHO recommendation, yielding the sensitivity of 61.8% and specificity of 76.9% based on the WHO standard. Its +LR was 2.47, and -LR was 0.45 with a DOR of 5.49. Depending on race or region, the results might differ, and local practice suggested revalidating this tool by tailoring the cut-off values to increase prediction potency.
BFH-OSTM is a tool for osteoporosis prediction in elderly men developed by Beijing Friendship Hospital. In this study, it has the best predictive efficiency compared with BMI and OSTA (p<0.001) whose AUCs range from 0.813 to 0.857. It had 65.8% sensitivity and 82.7% specificity according to WHO criteria. BFH-OSTM also had a high +LR (3.81) a low -LR (0.41) and the highest DOR (9.29). Significant differences in AUCs were observed between BFH-OSTM and OSTA or BMI in predicting OP. These findings illustrate that BFH-OSTM has a robust prediction efficiency in screening OP in elderly males.
Our study suggested that with a cost of missing 6.5% osteoporosis patients, BFH-OSTM could reduce 73.5% participants in screening BMD tests. Based on horizontal comparison of the various diagnostic criteria, sensitivity, osteoporosis missed and BMD measurement saved for BFH-OSTM were significantly better when we set WHO criteria as gold diagnosis standard of male OP. BFH-OSTM performed well at identifying individuals who were not necessary to take BMD measurement with high specificity. The results were consistent with the purpose of our study that elderly males should receive appropriate treatment.
The present study included several strengths: A cross-sectional study rather than a retrospective one was conducted in this study. Participants were elderly males whose information was collected from 8 distinct medical institutions. Our study implemented strict inclusion and exclusion criteria to eliminate selection bias as much as possible. This study may have some referential meaning for the development of possible diagnoses against OP and would be valuable for physicians in screening osteoporotic populations at primary hospitals or community health centers.
Conclusions
In conclusion, a comparison of three clinical tools for predicting primary osteoporosis was performed, and suitable thresholds for omitting BMD measurements were determined. Based on our cross-sectional study, BFH-OSTM outperformed OSTA and BMI, and BFH-OSTM was the most valuable tool for identifying primary osteoporosis in male. Benefit in terms of cost and reduction of unnecessary radiation exposure, we suggest men over age 50 years with BFH-OSTM score < 63 to take a BMD screening test.
Acknowledgment
The study was funded by Beijing Municipal Commission of Health promotion project (NO: 2018-TG-44).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wysocki MA, Doyle ST. Advancing osteoporosis evaluation procedures: detailed computational analysis of regional structural vulnerabilities in osteoporotic bone. J Pers Med. 2023;13(2):321. doi:10.3390/jpm13020321
2. Mo X, Zhao S, Wen Z, et al. High prevalence of osteoporosis in patients undergoing spine surgery in China. BMC Geriatr. 2021;21(1):361. doi:10.1186/s12877-021-02313-8
3. Shen ZW, Wei YX, Yu CQ, et al. 中国10个地区成年人骨折住院率的描述性分析 [Descriptive analysis of fracture hospitalization rate in adults from 10 regions of China]. Zhonghua Liu Xing Bing Xue Za Zhi. 2021;42(5):771–779. Chinese. doi:10.3760/cma.j.cn112338-20200619-00862
4. Melton LJ 3rd, Khosla S, Achenbach SJ, O’Connor MK, O’Fallon WM, Riggs BL. Effects of body size and skeletal site on the estimated prevalence of osteoporosis in women and men. Osteoporos Int. 2000;11(11):977–983. doi:10.1007/s001980070037
5. Kweon SM, Sohn DH, Park JH, et al. Male patients with rheumatoid arthritis have an increased risk of osteoporosis: frequency and risk factors. Medicine. 2018;97(24):e11122. doi:10.1097/MD.0000000000011122
6. Pinheiro MB, Oliveira J, Bauman A, Fairhall N, Kwok W, Sherrington C. Evidence on physical activity and osteoporosis prevention for people aged 65+ years: a systematic review to inform the WHO guidelines on physical activity and sedentary behaviour. Int J Behav Nutr Phys Act. 2020;17(1):150. doi:10.1186/s12966-020-01040-4
7. Looker AC, Melton LJ 3rd, Borrud LG, Shepherd JA. Lumbar spine bone mineral density in US adults: demographic patterns and relationship with femur neck skeletal status. Osteoporos Int. 2012;23(4):1351–1360. doi:10.1007/s00198-011-1693-z
8. Winzenrieth R, Ominsky MS, Wang Y, Humbert L, Weiss RJ. Differential effects of abaloparatide and teriparatide on Hip cortical volumetric BMD by DXA-based 3D modeling. Osteoporos Int. 2021;32(3):575–583. doi:10.1007/s00198-020-05806-1
9. Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ 3rd, Khaltaev N. A reference standard for the description of osteoporosis. Bone. 2008;42(3):467–475. doi:10.1016/j.bone.2007.11.001
10. Compston J, Cooper A, Cooper C, et al. UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos. 2017;12(1):43. doi:10.1007/s11657-017-0324-5
11. Watts NB, Adler RA, Bilezikian JP, et al. Osteoporosis in men: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2012;97(6):1802–1822. doi:10.1210/jc.2011-3045
12. An N, Lin JS, Fei Q. Beijing Friendship Hospital Osteoporosis Self-Assessment Tool for Elderly Male (BFH-OSTM) vs Fracture Risk Assessment Tool (FRAX) for identifying painful new osteoporotic vertebral fractures in older Chinese men: a cross-sectional study. BMC Musculoskelet Disord. 2021;22(1):596. doi:10.1186/s12891-021-04476-2
13. Zhang X, Lin J, Yang Y, et al. Comparison of three tools for predicting primary osteoporosis in an elderly male population in Beijing: a cross-sectional study. Clin Interv Aging. 2018;13:201–209. doi:10.2147/CIA.S145741
14. Zha XY, Hu Y, Pang XN, Chang GL, Li L. Diagnostic value of osteoporosis self-assessment tool for Asians (OSTA) and quantitative bone ultrasound (QUS) in detecting high-risk populations for osteoporosis among elderly Chinese men. J Bone Miner Metab. 2015;33(2):230–238. doi:10.1007/s00774-014-0587-5
15. Paik JM, Rosen HN, Katz JN, et al. BMI, waist circumference, and risk of incident vertebral fracture in women. Obesity. 2019;27(9):1513–1519. doi:10.1002/oby.22555
16. Gutwerk A, Müller M, Crönlein M, et al. Analyse steigender Behandlungskosten bei erhöhtem BMI von Patienten mit proximaler Femurfraktur [Analysis of rising treatment cost of elevated BMI in patients with proximal femoral fracture]. Unfallchirurgie. 2022. German. doi:10.1007/s00113-022-01187-8
17. Wynkoop A, Ndubaku O, Fras A, Walter N, Eekhoff J, Atkinson T. Ankle fracture patterns in drivers are associated with femoral fracture, higher BMI, and advanced age. Traffic Inj Prev. 2016;17(5):530–534. doi:10.1080/15389588.2015.1120296
18. Bergkvist D, Hekmat K, Svensson T, Dahlberg L. Obesity in orthopedic patients. Surg Obes Relat Dis. 2009;5(6):670–672. doi:10.1016/j.soard.2009.05.014
19. Bachmann KN, Bruno AG, Bredella MA, et al. Vertebral strength and estimated fracture risk across the BMI spectrum in women. J Bone Miner Res. 2016;31(2):281–288. doi:10.1002/jbmr.2697
20. Jia L, Cheng M. Correlation analysis between risk factors, BMD and serum osteocalcin, CatheK, PINP, β-crosslaps, TRAP, lipid metabolism and BMI in 128 patients with postmenopausal osteoporotic fractures. Eur Rev Med Pharmacol Sci. 2022;26(21):7955–7959. doi:10.26355/eurrev_202211_30147
21. Głogowska-Szeląg J. Ocena związku między gęstością mineralną kości (BMD) a wskaźnikiem masy ciała (BMI) u kobiet z osteoporozą po menopauzie [Assessment of the relationship between BMD and body mass index BMI in women with postmenopausal osteoporosis]. Wiad Lek. 2018;71(9):1714–1718. Polish.
22. Strugala C, Sobala W, Szubert Z, Hanke W. Ocena Ryzyka Złamań Osteoporotycznychw Populacji Kobiet W Wieku Powyżej 50 Latanaliza Wskaźników FRAX® BMI I FRAX® BMD [Evaluation of osteoporotic fractures in the group of woman over 50 years of age--comparison of tools FRAX BMD versus FRAX BMI]. Med Pr. 2013;64(3):327–333. Polish.
23. Lin J, Yang Y, Zhang X, et al. BFH-OSTM, a new predictive screening tool for identifying osteoporosis in elderly Han Chinese males. Clin Interv Aging. 2017;12:1167–1174. doi:10.2147/CIA.S140553
24. Koh LK, Sedrine WB, Torralba TP, et al. A simple tool to identify asian women at increased risk of osteoporosis. Osteoporos Int. 2001;12(8):699–705. doi:10.1007/s001980170070
25. Greiner M, Pfeiffer D, Smith RD. Principles and practical application of the receiver-operating characteristic analysis for diagnostic tests. Prev Vet Med. 2000;45(1–2):23–41. doi:10.1016/S0167-5877(00)00115-X
26. Mao Y, Xu L, Xue T, et al. Novel nomogram for predicting the 3-year incidence risk of osteoporosis in a Chinese male population. Endocr Connect. 2021;10(9):1111–1124. doi:10.1530/EC-21-0330
27. Tang H, He JH, Gu HB, et al. The different correlations between obesity and osteoporosis after adjustment of static mechanical loading from weight and fat free mass. J Musculoskelet Neuronal Interact. 2021;21(3):351–357.
28. Wang L, Yu W, Yin X, et al. Prevalence of osteoporosis and fracture in China: the china osteoporosis prevalence study. JAMA Netw Open. 2021;4(8):e2121106. doi:10.1001/jamanetworkopen.2021.21106
29. Kiswanjaya B, Bachtiar-Iskandar HH, Yoshihara A. Correlations of the Osteoporosis Self-Assessment Tool for Asians (OSTA) and three panoramic indices using Quantitative Ultrasound (QUS) bone densitometry. Dent J. 2023;11(2):34. doi:10.3390/dj11020034
30. Zhang J, Zhou R, Luo X, et al. Routine chest CT combined with the osteoporosis self-assessment tool for Asians (OSTA): a screening tool for patients with osteoporosis. Skeletal Radiol. 2022;52:1169–1178. doi:10.1007/s00256-022-04255-7
31. Subramaniam S, Chan CY, Soelaiman IN, et al. The performance of osteoporosis self-assessment tool for Asians (OSTA) in identifying the risk of osteoporosis among Malaysian population aged 40 years and above. Arch Osteoporos. 2019;14(1):117. doi:10.1007/s11657-019-0666-2
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


