Back to Journals » Patient Preference and Adherence » Volume 17
Validation of the Korean Version of Patient-Centered Care Tool: For Outpatients
Received 17 March 2023
Accepted for publication 3 June 2023
Published 29 June 2023 Volume 2023:17 Pages 1525—1540
DOI https://doi.org/10.2147/PPA.S411109
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Yeo Ju Kim,1,2 Gunjeong Lee,1 Sunyeob Choi1
1College of Nursing, Ewha Womans University, Seoul, South Korea; 2Inje University Ilsan-Paik Hospital, Goyang, Gyeonggi-do, South Korea
Correspondence: Sunyeob Choi, College of Nursing, Ewha Womans University, 52, Ewhayeodae-Gil, Seodaemun-Gu, Seoul, 03760, South Korea, Tel +82-2-3277-2873, Fax +82-2-3277-2850, Email [email protected]
Aim: The objective of this study was to assess the validity and reliability of the Korean version of the patient-centered care (K-PCC) instrument for outpatients. The study was conducted due to the absence of a measurement tool specifically designed to evaluate patient-centered care for outpatients.
Design: This study is a methodological study to verify the validity and reliability of the Korean version of Patient-Centered Care (K-PCC) to measure patient-centeredness for outpatients.
Methods: As a first step for the evaluation of the tool, the content validity was verified by expert panel. Then, a total of 400 outpatients were recruited, and construct validity was verified through confirmatory factor analysis (CFA) as the second step for the evaluation of the tool. The convergent and discriminant validity of the tool was verified by calculating the standardized factor loads, construct reliability (CR), and average variance extracted (AVE), and calculating the correlation square between the factors as the third and fourth steps for the evaluation of the tool. And as a fifth step for the evaluation of the tool, criterion validity was evaluated by comparing the correlation with the patient-centeredness measurement tool for inpatients (PEx-inpatient). In estimating reliability, internal consistency reliability coefficients were calculated.
Results: The confirmatory factor analysis supported good fit for the Korean patient-centered care instrument (K-PCC), and the eight-factor structure was validated. The scale comprises 21 items across eight factors: patient preferences (4 items), physical comfort (2 items), coordination of care (2 items), continuity and transition (3 items), emotional support (2 items), access to medical care (3 items), information and education (2 items), and family and friends (3 items). The Cronbach’s alphas ranging between 0.73 and 0.88.
Conclusion: The Korean patient-centered primary care instrument is a valid and reliable scale to measure patient-centered care for outpatients in the Korean medical environment.
Keywords: instrumentation, factor analysis, statistical, patient-centered care, patient experience
Introduction
In 2001, the Institute of Medicine (IOM) announced six key elements as requirements for quality healthcare.1 Among the six key elements, patient-centeredness is a concept that establishes a shared relationship between healthcare providers, patients, and their families to respect patient preferences in the decision-making process and ensure they receive the education and support they need to participate in their care.1 Patient-centeredness is an intangible value, which makes it challenging to define and measure the concept. Furthermore, it presents a limitation as it is not readily captured by existing administrative data.2 Nevertheless, in the United States and the United Kingdom, patient-centeredness has been measured since the early 2000s, reflected in the evaluation of the quality of care, and compensated through a value-based payment systems. Patient-centeredness, based on respect and partnership between patients and service providers, nurses and other clinical staff, is at the heart of quality primary care and is associated with positive health outcomes.3 Patient-centeredness in interactions between patients and medical staff is considered to lead to positive results by increasing patient trust in medical staff and facilitating shared decision-making,4 and is an essential competency for medical staff.5–7
In 2012, the Organization for Economic Cooperation and Development (OECD) recommended the need to establish the patient experience evaluation system in South Korea through the “OECD Health Care Quality Review” report,8 and the 2015 parliamentary audit also pointed out the need for efforts to do so.9 With this as an opportunity, the Health Insurance Review and Assessment Service conducted a study on the “patient-centered evaluation model” for inpatients and developed an evaluation tool,10 and the first evaluation began in 2017 and is set for the fourth evaluation in 2023.11 In the case of South Korea, although medicine has made rapid progress, consideration of patient-centeredness is insufficient in that patient-centeredness is considered as an characteristics and personalities of individual doctors rather than competency of medical institutions.2 The Korean Medical Association has highlighted certain concerns regarding patient experience evaluation, stating, “Since individual preferences, needs, and values vary based on personal inclinations and criteria for judgment, the results may differ even after receiving the same service”.12 Furthermore, they oppose the implementation of patient experience evaluation, asserting that the ranking of medical institutions based on evaluation scores lacks objectivity and reliability. They argue that the evaluation items are subjective and that the Health Insurance Review and Assessment Service seeks to exert control over medical institutions under the guise of institutional improvement.13 Conversely, medical consumer groups argue that some form of hospital evaluation should be conducted as South Korea’s healthcare system still primarily revolves around healthcare providers.13 Korea has the highest ratio of the average number of outpatient treatments per doctor in any OECD country, and doctors see the average 14.6 outpatients per day which is twice the OECD average of 6.8. Accordingly, patients have been found to have negative experiences of waiting for a long time and receiving short treatments during outpatient treatment.2 According to the OECD’s comparison of healthcare quality among member countries, disease management in Korea is lower quality for chronic compared with acute diseases.2,14 Although there is continued opposition to the patient experience evaluation by the opening doctors, given that patients with chronic diseases require frequent outpatient treatment, a tool needs to be developed that can measure the patient-centeredness outpatients experience in the Korean medical environment. In medical technology evaluation, the participation of patients and citizens themselves helps to secure procedural legitimacy by strengthening stakeholder participation and improving transparency. In addition, it is urgent to develop a patient experience evaluation tool for outpatients from a positive perspective that provides a specific and practical basis for treatment experience and quality of life.15
As a result of reviewing the literature, similar tools have recently been developed to measure patient-centeredness in South Korea, such as the Patient-Centered Healthcare Services Evaluation Scale,16 Patient-Centered Nursing Culture Scale for Hospitals17 and the Korean version of Person-centered Practice Inventory-Staff for nurses.18 However, these instruments cannot be regarded as tools that reflect patient preferences, which are the basis of patient-centeredness. The Person-centered Care Assessment (P-CAT), a human-centered care measurement tool, has also been developed by modifying tools created abroad; however, it has limitations in measuring the patient-centeredness of outpatient care, because it was developed for older adults with dementia, families, and nursing providers in elder care facilities. In addition, a survey was conducted in Korea on patient satisfaction with medical institutions; however, questions were raised about the validity, as various measurement tools were used.10 Thus, research and tools for measuring patient-centeredness for outpatients are still in their early stages in Korea, a standardized Korean version of patient-centered medical measurement tools need to be developed that can assess properties of patient-centeredness based on theoretical grounds.
Research on tool development has been more active abroad than in Korea,19 such as the Individualized Care Instrument (ICI), Patient-centered Family-focused Care (PCFC), Person-centered health care for older adults (PCHC), P-CAT, and Person-directed care assessment tool (PDC).19 However, since many of the developed tools are used in combination without separating inpatients and outpatients, there is a limit to reflecting the experience of outpatients in Korea, where outpatient treatment hours are generally less than 5 minutes.
The Patient-Centered Primary Care instrument (PCPC), developed in the Netherlands in collaboration with Harvard University and the Picker Institute, is a tool that has been verified for reliability and validity by applying the Patient-Centered Care (PCC) tool to the primary care environment.20 The PCC is one of the three most influential models in the United States that form the basis for patient-centered care,21 and its benefits have been demonstrated through several studies22–28 and measured in patients to reflect their values and preferences. Therefore, the PCPC tool based on PCC needs to be evaluated and applied after being modified to suit the Korean medical environment, where tools for measuring patient-centeredness for outpatients are lacking.
Methods
Aim
This study aimed to verify the validity and reliability of the Korean version of the PCPC, a patient-centered medical measurement tool developed by Cramm and Nieboer.20
Research Design
This study is a methodological study to verify the validity and reliability of the Korean version of the PCPC to measure patient-centered medical care in primary care settings.
Participants
The participants in this study were aged 19 years or older, receiving outpatient treatment at university hospitals, and able to communicate by reading and writing. Foreign, psychiatric, and pediatric patients were excluded from the study. For confirmatory factor analysis, the sample size should be at least ten times the number of questions,29 and the number of participants should be at least 360 participants. Therefore, the number of participants necessary for this study was calculated at 420, considering a 15% dropout rate. Excluding 20 collected questionnaires, including those with insufficient responses, 400 completed questionnaires were included in the final analysis.
Instrument
The PCPC was developed by Cramm and Nieboer20 to measure patient-centered care for primary care patients in eight dimensions, based on the concept of patient-centeredness identified by the Picker Institute. The PCPC consists of 36 items across eight dimensions, including patient preferences (7 items), physical comfort (5 items), coordination of care (4 items), continuity and transition (4 items), emotional support (4 items), access to care (5 items), information and education (4 items), and family and friends (3 items). The PCPC is measured on a five-point Likert scale (1 = totally disagree, 5 = totally agree). The higher the average score, the more patient-centered medical care is considered to have been provided. Regarding reliability at the time of development, Cronbach’s α of the eight dimensions ranged from 0.72 to 0.92 and was 0.89 for the entire scale.
Research Process
The process of this study was shown in Figure 1. In Item construction stage, the translation and back-translation process was conducted and the content validity was verified. The researchers used a CVI (Content Validity Index) cut-off of 0.8 to verify the content validity of the study. In pilot study stage, a preliminary survey was conducted with 10 outpatients. Based on the pilot study results, modifications were made to the PCPC questionnaire. In main study stage, data collection was conducted with 400 outpatient patients, and based on the results, the construct validity, criterion validity, and reliability of PCPC were verified. The factor loading cut-off was 0.6. The convergent and discriminant validity of the questionnaire were verified by calculating the standardized factor loadings, construct reliability (CR), and average variance extracted (AVE). CR should be greater than or equal to 0.70 and less than or equal to 0.95, and the AVE should be greater than or equal to 0.50.30 In reliability the Cronbach’s α 0.7 was the cut-off value.
 |
Figure 1 The process of the study. |
Item Construction Stage
Translation and Back-Translation of PCPC
The translation process was conducted in accordance with the linguistic validation process recommended by the Mapi Research Trust31 after obtaining approval for the tool’s translation and use from the PCPC’s developer.20 The linguistic validity process has four phases through which the translated tool is conceptually equivalent to the original tool when translated into another language and is consistent with the cultural context and easy for users to understand. In Phase 1 (forward translation), two researchers fluent in both Korean and English independently translated the PCPC. Subsequently, the researchers asked the professional translator, who was fluent in Korean and English and had a master’s degree in English literature, to faithfully translate the PCPC based on the original interpretation after explaining the tool’s purpose. Version 1 was created after comparing the consistency between the tools translated by the researcher and that of translated by the translator. Version 1 was verified by a panel of eight experts, including two nursing professors, three senior nurses, one head nurse in an integrated nursing care unit who provides direct care, and two head nurses in the general ward.
In Phase 2 (backward translation), version 2 was created by comparing the content with revised version 1 after requesting a foreign professional translator who was fluent in Korean and was not familiar with the original PCPC.
In Phase 3 (patient testing) was conducted to check whether the revised version 2 was suitable and comprehensible for outpatients, who were the PCPC’s intended respondents. A preliminary survey was conducted with 10 outpatients to determine whether there were any difficulties in understanding the survey’s content.
In Phase 4 (proofreading), the first version of the tool with 28 items was confirmed after checking for spelling and grammatical errors with a Korean literature scholar.
Content Validity
The version 1 PCPC was created after comparing the consistency between the tools translated by the researcher and that of translated by the translator. Version 1 was verified by a panel of eight experts, including two nursing professors, three senior nurses, one head nurse in an integrated nursing care unit who provides direct care, and two head nurses in the general ward. Tests showed that the CVI was 0.75 for three items, including Items 23 (“I was made aware of the possibilities for more intensive emotional support”), 32 (“I had easy access to my own data (lab results, medication overview, and referrals)”), and 34 (“With my consent, relatives were involved in my treatment”); however, the total CVI was 0.94. As a result of a discussion on items that did not meet the standard CVI value of 0.8, some items were removed or changed to create a revised version 1. For Item 23, the meaning of the phrase ‘more intensive emotional support’ was ambiguous, and Item 32 was found to be inadequate in Korea’s outpatient environment; thus, both items were excluded. For Item 34, “relatives” was revised to “family and guardians”, because in Korea, family members mainly makes decisions based on family-centeredness.32
The version 2 PCPC was created by comparing the content with revised Version 1 after requesting a foreign professional translator who was fluent in Korean and was not familiar with the original PCC. In this process, four items (4,16, 24, 33) were found to have overlapping meanings due to cultural differences. Specifically, Items 4 (“The influence of treatment that may have upon my life was taken into account”) and 24 (“There was a concern for the influence of my health upon my daily life (family, relative, work, social life, etc.)”) and Items 16 (“I could easily contact someone with questions”) and 33 (“I could ask questions whenever I wanted”) were interpreted as having the same meaning to respondent. After discussions between the researchers, Items 4 and 16 were deleted. As a result of reviewing these overlapping items, a revised version 2 was created, and a second content validity verification was conducted on two nursing professors, two head nurses, and one senior nurse. The total CVI was 0.97, and the CVI of items 15 and 33 were less than that of CVI 0.80. Items 15 (“I knew who was adjusting my treatment”) and 33 (“I could ask questions whenever I wanted”) were deleted.
Pilot Study and Questionnaire Modification
Pilot study was conducted to check whether the revised version 2 was suitable and comprehensible for outpatients, who were the PCPC’s intended respondents. A preliminary survey was conducted with 10 outpatients to determine whether there were any difficulties in understanding the survey’s content. As a result of examining the validity of the revised items, Item 5 (“I was helped to determine my own treatment purpose”) and 6 and Item 17 (“I knew where and why I should go when being referred to other healthcare providers (expert/nutritionist/physical therapist)”) and 18 (“All my information was delivered accurately in the case of a request and forwarding”) were considered to mean the same thing to respondents. After discussion between two researchers, Items 5 and 18 were deleted.
Main Study
Data Collection
The study period was from November 16, 2022 to January 3, 2023. Data were collected using face-to-face and non-face-to-face methods, and 400 questionnaires were collected in total. In the sampling process, convenience sampling was employed. Face-to-face data were collected with written consent from those who agreed to participate after receiving an explanation of the purpose of the study. These participants were patients who were waiting for or had completed outpatient treatment at a university-affiliated hospital in Gyeonggi Province, South Korea. Non-face-to-face data collection was performed using an online questionnaire platform to present the study’s purpose and procedure, participation method, consent to provide information, and questionnaire content. Data were then collected by obtaining approval from four online communities frequently used by outpatients and posting online addresses for surveys, along with recruitment posters for research participants. Respondents who participated in the study in a non-face-to-face manner read the explanation and participated in the survey and could withdraw from the study at any time. All participants received a reward.
Data Analysis
The collected data were analyzed using IBM SPSS 25.0 and AMOS 23.0. The participants’ demographic and sociological characteristics were analyzed by frequency and percentage, mean, and standard deviation. Item analysis, which identifies the item-domain correlation of each item, was conducted to confirm the contribution of each item to the concept.
Construct Validity
The original PCPC has already been verified for construct validity thus confirmatory factor analysis is appropriate for verifying the relationships between items and factors by applying previously verified tools to other population groups.33 Therefore, in this study, a confirmatory factor analysis was conducted to verify the construct validity of the Korean version of the PCPC. An absolute fit index was used to evaluate the overall model fit, a relative fit index was used to evaluate the differences between the model and the actual data, and a parsimonious fit index was used to evaluates the model’s complexity. The absolute fit index was confirmed using the chi-squared test, root mean square error of approximation (RMSEA), and adjusted goodness of fit index (AGFI). The chi-squared test is an indicator of a model’s suitability under the assumption of normal distribution; the model is suitable only when the p-value is greater than 0.05, but model fit is not necessarily low even if the p-value is less than 0.05. To compensate for this, the chi-squared statistic divided by the degree of freedom (normed chi-square [NC]) is less than or equal to 3.0, which is considered appropriate. RMSEA 0.05~.10 is considered an appropriate model.29,30 The AGFI is a value adjusted by the degree of freedom and is considered to indicate very good model if it is greater than or equal to 0.90.
The relative fit index (normal fit index [NFI]) and comparative fit index [CFI]) were confirmed, as was the brief fit index (Akaike information criterion [AIC]). The NFI and CFI are also considered very good if they are 0.90 or higher, and are evaluated as an appropriate level if they are between 0.70 to 0.90. For the AIC, the complexity of the model increases as the value increases; therefore, the lower the value, the better the model.
The convergent and discriminant validity of the questionnaire were verified by calculating the standardized factor loadings, construct reliability (CR), and average variance extracted (AVE), and calculating the correlation square between the factors.
Criterion Validity
The criterion validity verification of the Korean version of the PCPC confirmed the correlations between the patient-centeredness measurement tool for inpatients (PEx-inpatient) developed by the Health Insurance Review and Assessment Service.11
Reliability Assessment
The reliability of the tool was determined using Cronbach’s α, confirming internal consistency.
Results
Participants Characteristics
Demographic characteristics of the participants are presented in Table 1. The mean age of the participants in this study was 40 ± 15.1; 57.0% of those under the age of 40 years, and 43.0% were over. Of these, 78.8% were women, 47.8% were married, 62.0% were revisiting outpatients, and 51.0% had a bachelor’s degree.
 |
Table 1 General Characteristics of the Participants (N=400) |
Item Analysis
As a result of the item analysis of the Korean version of the PCPC with 28 items, the mean of each item was distributed between 2.88 and 4.21, and the standard deviation was in the range of 0.75 to 1.20. The Item 29 (“I can easily request a receipt”) was the highest with 4.21 points, and Item 28 (“I did not have to wait long for my turn when I visited”) was the lowest with 2.88 points. The skewness ranged from −1.12 to 0.04 and the kurtosis ranged from −1.06 to 0.98; thus, the normality test was satisfied with skewness below 3 and kurtosis below 10. As a result of confirming the correlation coefficient between the items and factors, Factor 1 (patient preferences) was 0.69~.82, Factor 2 (physical comfort) was 0.64~.74, Factor 3 (coordination of care) was 0.86~.92, Factor 4 (continuity and transition) was 0.81~.86, Factor 5 (emotional support) was .73~.90, Factor 6 (access to care) was 0.60~.80, Factor 7 (information and education) was 0.89~.91, and Factor 8 (family and friends) was 0.81~.87 (Table 2).
 |
Table 2 Item Analyses of the Korean Version of the PCC (28 Items) (N=400) |
Validity and Reliability of the Korean Version of the PCPC
Validity
Content validity
An item analysis was conducted before the confirmatory factor analysis. As a result of confirming the correlation coefficient between the items and subfactors for the item-level content validity (item-level content validity index [I-CVI]), items with an I-CVI value of 0.70 or higher were selected. Five items (Items 7, 8, 9, 12, and 29) had an I-CVI value of less than 0.70, and three were considered necessary, while two were deleted. The two deleted question were Item 7 (“I was advised on what I could actually do”; I-CVI = 0.69) and Item 29 (“I could easily request a receipt”; I-CVI = 0.60). Item 29 could be interpreted as inappropriate for the Korean medical environment where receipts are provided after treatment without the need for a separate request. In addition, Item 7 was interpreted as inappropriate in the Korean medical environment. This can be interpreted from the perspective of the outpatient medical environment in South Korea, where a large number of patients are seen within a short period of time. The number of outpatient visits per physician per day in South Korea is twice the average of OECD countries,2 resulting in patients receiving services within a time frame of 5 minutes.34 As a result, patients utilize medical services under the guidance of healthcare professionals, and there is limited time available for seeking advice. As a result of confirming the item-level content validity, a correlation of moderate or higher was generally accepted, and finally, 26 items were extracted for the second version of the tool.
Construct Validity
The results of the confirmatory factor analysis to test the construct validity of the Korean version of the PCPC with 26 items are shown in Table 3. As a result of analyzing the suitability of the confirmatory factor analysis of the Korean version of the PCPC, the chi-squared statistic was 1052.38 (df =271, p <0.001), and NC was 3.88. However, with RMSEA = 0.09, AGFI = 0.77, NFI = 0.79, and CFI = 0.84, the AGFI values were found to not meet the recommended criteria.
 |
Table 3 Model Fit of the Korean Version of the PCC (N=400) |
Accordingly, to increase the model fit, the standardized coefficients of Items 10, 11, 12, 24, and 28 with low explanatory power and a factor loading below 0.60, were removed. We compared and analyzed the suitability of Model 1 including all 26 items and Model 2 with Items 10, 11, 12, 24, and 28, with a factor load of less than 0.60, removed.
Regarding the results of Model 2 with 21 items, the chi-squared static was 386.18 (df =161, p < 0.001); however, NC was 2.40, which met the standard of NC < 3.0; NFI = 0.90, CFI = 0.94, and RMSEA=0.06 showed a significant increase over Model 1 to a suitable level, the AGFI also met the recommended criteria with a suitable level of 0.88, and the simple name suitability index, AIC, decreased from 1212.38 to 526.18, making the model more parsimonious (Table 3). The significance (CR) value was 11.20-19.88 in the relationships with each factor of Model 2, which removed five items from Model 1, and all factors were significantly explained from the constituent variables based on a significance level of 0.05. Thus, the Korean version of the PCPC (hereinafter K-PCC) with 21 items was adopted as the final tool (Table 4).
 |
Table 4 Results of the CFA and Analyses of Discriminant Validity of the Korean Version of PCC (21 Items) (N=400) |
Convergent and Discriminant Validity
The results of verifying the convergent validity of the K-PCC with 21 items finally adopted through confirmatory factor analysis are shown in Table 4. To verify the convergent validity, the standardized factor load (β) should be greater than or equal to 0.60, the CR should be greater than or equal to 0.70 and less than or equal to 0.95, and the AVE should be greater than or equal to 0.50.35 The results of this study verified the convergent validity of the K- PCC, because the β value of all items was 0.65~.89, CR was 0.77~.88, and AVE was 0.53~.78. The results of verifying the discriminant validity of the K-PCC with 21 through confirmatory factor analysis are shown in Table 4. Discriminant validity was verified when the two subfactors (AVE values were all larger than the square (R2) of the correlation coefficient (r) between factors.35 As shown in Table 4, the discriminant validity was verified, in that the value of AVE was larger than the square of the correlation coefficient.
Criterion Validity
This study analyzed the correlation between the K-PCC and the patient-centeredness measurement tool for inpatients (PEx-inpatient) developed by the Health Insurance Review and Assessment Service to verify the criterion validity of the K-PCC (Table 5). The PEx-inpatient10 was developed by combining HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) of AHRQ (Agency for Healthcare Research and Quality) of United States and the Inpatient Adult Survey of United Kingdoms. The tool consists of five domains, nurse area, doctor area, medication and treatment process, hospital environment, patient rights guarantee, and two questions regarding overall satisfaction and recommendation intention. The higher the score, the higher the patient-centered medical care. At the time of development, Cronbach’s α ranged from 0.79 to 0.94.10 A correlation analysis showed a significant positive correlation between the K-PCC and PEx-inpatient (r = 0.64, p < 0.001). All subfactors of the K-PCC showed significant positive correlations with the PEx-inpatent. Accordingly, the criterion validity of the K-PCC was verified.
 |
Table 5 Correlations Among the K-PCC and PEx-Inpatient (N=400) |
Reliability
The K-PCC with verified validity comprises 21 items across the following domains: patient preferences (4 items), physical comfort (2 items), coordination of care (2 items), continuity and transition (3 items), emotional support (2 items), access to medical care (3 items), information and education (2 items), and family and friends (3 items). The mean scores of the subfactors were as follows: patients’ preferences (factor 1) = 3.62±0.71, physical comfort (factor 2) = 3.68±0.85, coordination of care (factor 3) = 3.63±0.76, continuity and transition (factor 4) = 3.90±0.66, emotional support (factor 5) = 3.43±0.99, access to medical care (factor 6) = 3.67±0.85, information and education (factor 7) = 3.81±0.76, and family and friends (factor 8) = 3.42±0.85. The reliability of the factors was as follows: patients’ preferences (factor 1) = 0.79, physical comfort (factor 2) = 0.75, coordination of care (factor 3) = 0.73, continuity and transition (factor 4) = 0.79, emotional support (factor 5) = 0.88, access to medical care (factor 6) = 0.76, information and education (factor 7) = 0.77, and family and friends (factor 8) = 0.78 (Table 6). The K-PCC is shown in Table 7.
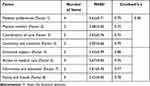 |
Table 6 Reliability of Korean Version of PCC (21 Items) (N=400) |
 |
Table 7 The Final Version of K-PCC |
Discussion
This study verified the validity and reliability of Korean version of PCPC for outpatients. This study clearly showed that the 21-item K-PCC is valid and reliable instrument to measure the patient-centeredness. Creating a patient-centered medical culture in which patient-centered medical service provision and positive medical service experiences improve patient symptom relief and treatment compliance.34 Accordingly, in South Korea, patient experience is being investigated for inpatients since 2017, as part of the establishment of a patient-centered care culture.11 The Picker Institute in the United States presented eight conceptual components of patient-centered care through various qualitative research studies to identify the definition and components of patient-centeredness,36 which greatly contributed to constructing the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) and National Health Service (NHS) Inpatient Survey, which are the cornerstones of patient experience evaluation in South Korea.2 However, a national tool for measuring patient-centered care have not yet been developed and surveys have not been conducted for outpatients in South Korea. On the other hand, South Korea has a higher percentage of outpatients than hospitalized or emergency patients.37 In particular, since 2020, the number of outpatients has increased further due to the prevalence of various infectious diseases, such as COVID-19,38 so it is urgent to investigate the patient experience for outpatients. Therefore, this methodological study verified the validity and reliability of the PCPC tool developed by Cramm and Nieboer20 into Korean to measure the level of patient-centered care for outpatients. The K-PCC developed in this study is a tool consisting of 21 items across eight factors: patients’ preferences, physical comfort, coordination of care, continuity and transition, emotional support, access to medical care, information and education, and family and friends, and the discussion of the tool is as follows.38
The biggest reason why the developed K-PCC tool deleted 15 items (items 4, 6, 7, 10, 11, 12, 15, 16, 18, 23, 24, 28, 29, 32, and 33) from the PCPC tool, which consists of 36 items, is South Korea’s care delivery system and the low compensation health insurance policy,39 which differs from developed countries. The care delivery system in South Korea is based on the Medical Act and the National Health Insurance Act, and medical institutions are divided into clinics, general hospitals including university hospitals, and tertiary general hospitals. However, there are no restrictions on the utilization of medical care, and the burden of using tertiary general hospitals and university hospitals is not significant. Additionally, there is no separate cost associated with seeking medical treatment at a tertiary general hospital, and due to an increase in loss insurance subscription, out-of-pocket expenses have often been very small. Therefore, most patients in South Korea have come to prefer general hospitals or advanced general hospitals with large and famous doctors and expensive equipment.40 Due to the concentration of outpatients in general hospitals, a general hospital that treats 10,000 outpatients per day is like a marketplace.39 According to OECD data, the number of outpatient treatments per person in South Korea was 16.6, nearly twice that of OECD countries.41 In the 2021 medical service survey, 56.9% of the respondents stated that the actual time they received outpatient treatment was 1 to 5 minutes.34 Additionally, there is a reason why university hospitals cannot guarantee profits solely from the treatment of natural suitable diseases due to the low health insurance rate policy in South Korea. This is why certain questions were excluded from the medical environment in South Korea, which is challenging for patient-centered communication because university hospital doctors treat at least 30 to 70 outpatients during the morning or afternoon. Therefore, it is imperative to assess the reliability and validity of PCPC within the specific cultural and healthcare context before implementing it in different cultural and healthcare environments.
The first component, the patient preferences dimension, involves maintaining dignity and treating patients by considering their preferences and motivating them to set and achieve their own treatment goals. To provide patient-centered medical care, it is important to relieve physical symptoms, such as patient pain or difficulty breathing and provide safety, which corresponds to the second factor of PCPC, physical comfort. With the recent emphasis on multidisciplinary healthcare, patient information should be properly transmitted, shared, and coordinated, among medical staff, as various medical providers such as doctors, nurses, pharmacists, and physical therapists, are involved in providing patient care. This aspect corresponds to the PCPC’s third factor, adjustment, and fourth factor, continuity. The fifth dimension of PCPC is emotional support which is, similar to what has been found in previous studies, in that it is necessary to involve emotional support because illness is often accompanied by anxiety and depression, which affects patients’ social relationships privacy.42,43 Patients should also be able to easily schedule and access treatment, which correspond to accessibility, the sixth dimension of the PCPC. The patients themselves are the subjects of disease management, and in the current medical environment, where patient participation in medical care is emphasized, patients must be aware of all aspects of treatment, which can be seen as in line with PCPC’s seventh dimension of information and education. Finally, individuals’ disease transitions affect their family members and other around them; thus, it is necessary to address their needs and questions and provide adequate support to engage family members in the treatment process.20 The K-PCC, which includes all the above components, is the tool to measure the composition concept of patient-centeredness, and this study is meaningful in that it has been adapted and verified the PCPC for the first time for use with Korean populations.
The model fit of original tool developed by Cramm and Nieboer20 was suitable of 36 items with CFI = 0.99, RMSEA = 0.05, and SRMR = 0.08, and the K-PCC was confirmed to be suitable with Model 2, with 21 items, through a model suitability verification process. Although 15 items were deleted from the original tool, the K-PCC was verified as an assessment of the overall concept of patient-centeredness and the suitability of the model was confirmed to be similar to that reported in previous studies. Model 2 was analyzed after removing five items (10, 11, 12, 24, and 29) with a factor load below 0.60 because the AGFI value was 0.77, and the model suitability index was improved to NFI = 0.90, CFI = 0.94, and RMSEA = 0.06, compared were Model 1.
It is hard to compare the convergent and discriminant validity between the original PCPC and K-PCC, since the original PCPC did not report the convergent and discriminant validity. However, the 21-item K-PCC tool verified the construct validity through intensive validity and discriminant validity verification. As a result, the standardized factor loading was at least 0.50, the CR was at least 0.70, and the AVE was at least 0.50; thus, it is a methodologically more valid than previous studies.
To verify the criterion validity of the K-PCC, correlations with the PEx-inpatient developed by the Health Insurance Review and Assessment Service10 were analyzed and there was a statistically significant correlation between the two tools. The analysis showed significant positive correlations in all subfactors (r = 0.21~.54, p < 0.001). When testing the reference validity, a correlation coefficient between 0.4 to 0.8 is recommended.44 In this study, the correlation coefficient was confirmed to be 0.4 or higher except for family and friends (Factor 8). This was found to have a relatively low correlation coefficient because the patient-centered tool for inpatients does not include questions related to family and friends, unlike the K-PCC. In the case of Korea, the K-PCC can be said to reflect Korean culture well in that many family opinions are reflected in medical decisions.32
As a result of confirming the internal consistency to verify the reliability of the K-PCC, patients’ preferences. Physical comfort, coordination of care, continuity and transition, emotional support, access to medical care, information and education, and family and friends had Cronbach’s α values of 0.79, 0.75, 0.73, 0.79, 0.88, 0.76, 0.77, and 0.78 respectively, which were similar to those of all original tools, 0.92, 0.72, 0.82, 0.87, 0.74, 0.80, 0.78, and 0.92, respectively. In this study, although the number of items was reduced from 36 in the original tool to 21 in the K-PCC, the overall reliability increased from 0.89 to 0.90. Therefore, the K-PCC can be evaluated as a tool with excellent reliability for measuring patient-centered medical care for outpatients.
This study is meaningful in that the validity and reliability of patient centeredness, which is increasing in the Korean medical environment where the proportion of outpatients is high, were measured by applying an adapted version of the PCC to the Korean outpatient environment. As a result of the analysis, the K-PCC a 21-item tool with confirmed validity and reliability. Therefore, is the K-PCC is expected to be useful for assessing patient-centered medical care perceived by patients who receive outpatient treatment at university hospitals. In addition, this study was able to select participants from more diverse age groups and situations by collecting data in parallel with written and online surveys. Using this mixed method is meaningful in that it was possible to increase the likelihood the research results can be generalized of generalization by increasing the representativeness of the sample.45 The research findings have confirmed that K-PCC is a tool with validity and reliability in the healthcare environment of South Korea. Therefore, it is necessary to utilize K-PCC to examine the concept and meaning of patient-centeredness as perceived by patients. Through this, it is important to assess the current healthcare environment in South Korea and establish a patient-centered healthcare environment. By doing so, patients will be able to receive high-quality medical services that align with their values and preferences.
Limitations of the Study
This study collected data by combining non-face-to-face and face-to-face methods. Given that non-face-to-face collection accounted for 75% of the participants, the average age of the participants was 40 years, which was lower than that of the original tool, which had a mean participant age of 74 years. Therefore, the necessity for expanded research is suggested by diversifying the age groups of the participants in the future. It is necessary to verify the K-PCC tool through repeated studies in Korea in that there may be problems with cultural differences and translation meaning in that K-PCC translated tools developed in Western cultures.
Conclusion
This study developed a K-PCC tool in accordance with the Korean medical environment by translating a PCPC tool that measures patient-centered care into Korean to assess the level of patient-centered care delivery for outpatients. The developed K-PCC tool is a 5-point Likert scale, consisting of 8 factors with 21 items.
In this study, statistical analyses were conducted to verify the content validity, construct validity, convergent and discriminant validity, and criterion validity of the K-PCC tool. The results demonstrated high reliability of the tool. Therefore, it was concluded that the K-PCC tool is a valid and reliable instrument for evaluating patient-centeredness among outpatients in South Korea. It is anticipated that the utilization of the K-PCC tool will contribute to assessing and promoting patient-centered care in the Korean medical environment.
Ethical Approval
Prior to face-to-face data collection, the research was approved by the review board of Inje University Ilsan Paik Hospital which the researcher belonged (ISPAIK 2022-09-038-001). Prior to non face-to-face data collection, the research was approved by the reivew board of Ewha Womans Universtiy which the researcher belonged (ewha-202212-0023-01). Our study complies with the Declaration of Helsinki.
Acknowledgment
We would like to thank Editage (www.editage.co.kr) for English language editing.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
All authors declare no conflicts of interest in this work.
References
1. Wolfe A. Institute of Medicine report: crossing the quality chasm: a new health care system for the 21st century. Policy Polit Nurs Pract. 2001;2(3):233–235. doi:10.1177/152715440100200312
2. Do YK. Improving patient-centeredness through patient experience evaluation: evidence, significance, and challenges. HIRA Policy Trend. 2017;11(3):7–24.
3. Etz RS, Zyzanski SJ, Gonzalez MM, Reves SR, O’Neal JP, Stange KC, et al. A new comprehensive measure of high-value aspects of primary care. Ann Fam Med. 2019;17(3):221–230. doi:10.1370/afm.2393
4. Wong EC, Collins RL, Breslau J, et al. Associations between provider communication and personal recovery outcomes. BMC Psychiatry. 2019;19(1):102. doi:10.1186/s12888-019-2084-9
5. Han J, Park J. A case study of medical communication education program for improving patient-centered communication skill program: focusing on the andragogy course model, andragogy today. Int J Adult Continu Educ. 2021;24(1):191–223. doi:10.22955/ace.24.1.202102.191
6. Kim SJ, Kim B. Effects of communication empowerment program based on situated learning theory for nursing students. J Korean Acad Nurs. 2018;48(6):708–719. doi:10.4040/jkan.2018.48.6.708
7. Kuehn BM. Patient-centered care model demands better physician-patient communication. J Am Med Assoc. 2012;307(5):441–442. doi:10.1001/jama.2012.46
8. OECD. OECD Health Care Quality Review: Korea, Assessment and Recommendations. Paris: OECD; 2012. doi:10.1787/9789264173446-4-en
9. Seo S. Introduction of patient experience assessment to measure patient-centeredness. HIRA Policy Trend. 2017;11(3):25–28.
10. Do YK, Kim JE, Lee JY, et al. Study on the development of patient-centeredness assessment model. Health Insurance Review & Assessment Service, Seoul National University Research and Development Business Foundation. 2015; Report no: G000E70-2015-87.
11. Health Insurance Review & Assessment Service. Gangwon-do: detailed implementation plan for patient experience evaluation in 2021; 2021. Available from https://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA020002000100&brdScnBltNo=4&brdBltNo=8734&pageIndex=1&pageIndex2=1#none.
12. Lee JW. Patient experience evaluation that breaks trust between doctors and patients must be stopped immediately. Medical Newspaper; 2022. Available from: http://www.bosa.co.kr/news/articleView.html?idxno=2178353.
13. Roh CJ. Who dares to see doctors? reasons for opposing HIRA’s ‘patient experience evaluation’. Insight Korea; 2022. Available from: https://www.insightkorea.co.kr/news/articleView.html?idxno=98082.
14. OECD indicators. Health at a Glance 2017. Paris: OECD Publishing; 2017:3216. doi::3216. doi:10.1787/health_glance-2017-en
15. Lee WY. Review on the patient and public involvement in health technology appraisals at NICE. J Crit Soc Welf. 2012;34:47–75.
16. Lee SR, Yang NY. Development of patient-centered healthcare services evaluation Scale. Korean Acad Community Health Nurs. 2020;27(2):198–209. doi:10.22705/jkashcn.2020.27.2.198
17. Shin E, Yoon SH. Development of the patient-centered nursing culture scale for hospitals. J Korean Acad Nurs. 2019;49(5):613–630. doi:10.4040/jkan.2019.49.5.613
18. Kim S, Tak SH. Validity and reliability of the Korean version of person-centered practice inventory–staff for nurses. J Korean Acad Nurs. 2021;51(3):363–379. doi:10.4040/jkan.21027
19. Son YJ, Yoon HK. A Concept analysis on patient-centered care in hospitalized older adults with multimorbidity. J Korean Criti Care Nurs. 2019;12(2):61–72. doi:10.34250/jkccn.2019.12.2.61
20. Cramm JM, Nieboer AP. Validation of an instrument for the assessment of patient-centered care among patients with multimorbidity in the primary care setting: the 36-item patient-centered primary care instrument. BMC Fam Pract. 2018;19(1):143. doi:10.1186/s12875-018-0832-4
21. Shaller D. Patient-Centered Care: What Does It Take? Commonwealth Fund New York; 2007.
22. Chen TT, Chueh KH, Chen KC, Chou CL, Yang JJ. The satisfaction with care of patients with schizophrenia in Taiwan: a cross-sectional survey of patient-centered care domains. J Nursi Res. 2023;31(2):e268. doi:10.1097/jnr.0000000000000549
23. Sestito SF, Rodriguez KL, Hruska KL, et al. A photo-elicitation study of homeless and marginally housed Veterans’ experiences with patient-centered care. Pat Exp J. 2018;5(3):123–148. doi:10.35680/2372-0247.1279
24. Williams JS, Walker RJ, Smalls BL, et al. Patient-entered care, glycemic control, diabetes self-care, and quality of life in adults with type 2 diabetes. Diabetes Technol Ther. 2016;18(10):644–649. doi:10.1089/dia.2016.0079
25. Harrison R, Walton M, Kelly P, et al. Hospitalization from the patient perspective: a data linkage study of adults in Australia. Int J Qual Health Care. 2018;30(5):358–365. doi:10.1093/intqhc/mzy024
26. Davis K, Schoenbaum SC, Audet AM. A 2020 vision of patient-centered primary care. J Gen Intern Med. 2005;20(10):953–957. doi:10.1111/j.1525-1497.2005.0178.x
27. Wolf A, Vella R, Fors A. The impact of person-centred care on patients’ care experiences in relation to educational level after acute coronary syndrome: secondary outcome analysis of a randomised controlled trial. Eur J Cardiovasc Nurs. 2019;18(4):299–308. doi:10.1177/1474515118821242
28. Cramm JM, Nieboer AP. Validation of an instrument to assess the delivery of patient-centred care to people with intellectual disabilities as perceived by professionals. BMC Health Serv Res. 2017;17(1): 1–11. doi:10.1186/s12913-017-2424-8
29. Lee YJ. Understanding factor analysis. Seoul: Suckjung; 2002.
30. DeVellis RF. Scale Development: Theory and Applications.
31. MAPI Group. Linguistic Validation Guidance of a Clinical Outcome Assessment (COA). France: Mapi Research Trust. 2018.
32. Lee JK, Keam B, An AR, et al. Surrogate decision-making in Korean patients with advanced cancer: a longitudinal study. Supportive Care in Cancer. 2013;21(1):72–91. doi:10.1037/a0032138
33. Geldhof GJ, Preacher KJ, Zyphur MJ, et al. Reliability estimation in a multilevel confirmatory factor analysis framework. Psychological methods. 2014;19(1):72–91. doi:10.1037/a0032138
34. Shin J, Cho BH, Choi BR, et al. Survey on the experience with healthcare service in 2020. Korea Institute for Health and Social AffairsPolicy Report Grant No: 2020-88. Supported by Ministry of Health and Welfare. 2020;181.
35. Hair JF, Hult GTM, Ringle CM, et al. A primer on partial least squares structural equation modeling (PLS-SEM). New York: Sage publications; 2021.
36. Scholl I, Zill JM, Härter M, et al. An integrative model of patient-centeredness – a systematic review and concept analysis. PLoS One. 2014;9(9):e107828. doi:10.1371/journal.pone.0107828
37. Kim JO. Recognition and related factors of outpatient medical service safety management. Korean J Safe Cult. 2022;15:273–288. doi:10.52902/kjsc.2022.15.273
38. Lee AY, Yu JW, Lee SH, et al. A Study on factors affecting outpatient care satisfaction according to the types of medical institution: findings from the health care experience survey 2019. J Korean Acad. 2021;22(9):505–513. doi:10.5762/KAIS.2021.22.9.505
39. Yum HK. Current status and improvement of university hospitals in the medical delivery system. Healthcare Policy Forum. 2022;20(1):8–13.
40. Kim YS. Improvement plan of healthcare delivery system in Korea. Korean J Med. 2020;95(3):129–133. doi:10.3904/kjm.2020.95.3.129
41. Kim YM. A Study on the Patient-centered medical delivery system - focusing on EU examples of strengthening primary care -. J Korean Soc Law Med. 2019;20(3):235–262. doi:10.29291/kslm.2019.20.3.235
42. Kuipers SJ, Nieboer AP, Cramm JM. Views of patients with multi-morbidity on what is important for patient-centered care in the primary care setting. BMC Fam Pract. 2020;21(1). doi:10.1186/s12875-020-01144-7
43. Read JR, Sharpe L, Modini M, et al. Multimorbidity and depression: a systematic review and meta-analysis. J Affect Disord. 2017;221:36–46. doi:10.1016/j.jad.2017.06.009
44. Lee K, Shin S. Validity of instrument development research in Korean nursing research. J Korean Acad Nurs. 2013;43(6):697–703. doi:10.4040/jkan.2013.43.6.697
45. Seo J, Lee M. Structural equation model for psychosocial adjustment of breast cancer survivors based on family resilience model. Korean J Adult Nurs. 2022;34(2):178–195. doi:10.7475/kjan.2022.34.2.178
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
