Back to Journals » International Journal of Women's Health » Volume 12
Utilization Rate and Factors Associated with Non-Utilization of Non-Pneumatic Anti-Shock Garment in the Management of Obstetric Hemorrhage in Public Health Care Facilities of Northern Ethiopia: A Cross-Sectional Study
Authors Desta AA , Berhane M, Woldearegay TW
Received 17 June 2020
Accepted for publication 12 October 2020
Published 30 October 2020 Volume 2020:12 Pages 943—951
DOI https://doi.org/10.2147/IJWH.S266534
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Abraham Aregay Desta,1 Mentsegeba Berhane,2 Tewolde Wubayehu Woldearegay3
1Public Health Research, Tigray Health Research Institute, Mekelle, Tigray, Ethiopia; 2Maternal Care, Mekelle Hospital, Mekelle, Tigray, Ethiopia; 3Tigray Health Research Institute, Mekelle, Tigray, Ethiopia
Correspondence: Abraham Aregay Desta
Public Health Research, Tigray Health Research Institute, P.O. Box 1547, Mekelle, Tigray, Ethiopia
Email [email protected]
Background: Obstetric hemorrhage (OH) causes more than 25% of the maternal deaths across the world annually. A significant number of these deaths can essentially be prevented with a skilled birth attendant and having all-inclusive emergency obstetric care technologies. One of these promising technologies is to utilize non-pneumatic anti-shock garment (NASG). Despite this fact, there are limited studies on the utilization of NASG in Ethiopia.
Objective: The aim of this study was to assess the utilization rate and factors associated with non-utilization of NASG in the management of obstetric hemorrhage in public healthcare facilities of Northern Ethiopia.
Methods: An institution-based cross-sectional study was conducted from December 2017 to February 2018 involving 338 randomly selected healthcare providers working in the maternity healthcare facilities. Data were collected using pre-tested and self-administered questionnaires. Data were entered and analyzed using STATA version 14.0 statistical software package. The result was displayed using descriptive, bivariate, and multivariable logistic regression analysis to identify independent predictors of non-utilization of NASG at a P-value≤ 0.05.
Results: About 121 (35.80%; 95% CI=30.68– 41.16%) of the health workers did not utilize NASG, and 217 (64.20%; 95% CI=58.84– 69.32%) utilized NASG. Being females, with adjusted odds ratio (AOR)=2.21 (95% CI=1.06– 4.63), use of NASG in previous works to manage OH, with AOR=0.1 (95% CI=0.02– 0.48), having perceived skill to use the garment in the facility, with AOR=0.10 (95% CI=0.01– 0.79), were significantly associated with the non-utilization of NASG.
Conclusion: There was a lower rate of NASG utilization among the healthcare providers for the management of obstetric hemorrhage. Being a male care provider, having no experience of using NASG to manage PPH, and having perceived skill to use the garment in the healthcare facility were significantly associated factors for the non-utilization of the NASG. Due emphasis should be given to the utilization of NASG to manage obstetric hemorrhage by addressing the identified modifiable factors for non-utilization of NASG by healthcare workers.
Keywords: maternal and child health, non-pneumatic anti-shock garment, Ethiopia
Plain Language Summary
Globally, more than 25% of the maternal deaths are caused by obstetric hemorrhage. Postpartum hemorrhage accounts for more than 30% of all maternal deaths. NASG is a part of the resuscitation measures to help control the sequelae of bleeding. Evidence proved that it is very important to stabilize mothers with obstetric hemorrhage and hypovolemic shock. Even though utilization of NASG is proven at reducing the sequelae of obstetric hemorrhage, little is known about the utilization rate and factors associated with non-utilization among the healthcare providers in Tigray. Respondents were asked about the utilization of NASG for the management of obstetric hemorrhage. Knowledge and attitude of obstetric hemorrhage and NASG-related questions were assessed and determined quantitatively. Of the 338 healthcare workers, only 217 (64.20%; 95% CI=58.84–69.32%) reported that they did utilize NASG for the management of obstetric hemorrhage. There were a high number of healthcare providers who did not utilize NASG for management of obstetric hemorrhage.
Due emphasis should be given to utilization of NASG to manage obstetric hemorrhage by addressing the identified modifiable factors for non-utilization of NASG by healthcare workers.
Introduction
Worldwide, about five million maternal deaths are attributed to pregnancy related complications.1 Three Asian (India, Pakistan, Afghanistan) and three African (Nigeria, Ethiopia, and the Democratic Republic of Congo) countries alone covered more than 50% of the maternal deaths all over the world.2,3 Over 99% of maternal deaths occurred in developing countries, where pregnant women live in rural areas or have numerous barriers to promptly reaching skilled care.4 In Ethiopia, regardless of marked enhancements in the utilization of maternal health services, the Maternal Mortality Rate (MMR) remains high.5–7
Annually, obstetric hemorrhage alone causes more than 25% of maternal deaths across the world.8–10 It is the largest direct cause of maternal mortality worldwide11 and it is estimated to have killed around 500,000 women as a result of hemorrhage within a few hours of delivery.12 The proportion of maternal deaths attributable to PPH varies considerably between developed and developing countries.13 Proper management of PPH can save many lives, though it depends on a number of factors, like the accessibility and availability of healthcare facilities, skilled birth attendant, timely diagnosis, treatment, and adequacy of blood transfusion services.14,15
A significant number of maternal deaths can essentially be prevented using skilled birth attendants and having all-inclusive emergency obstetric care technologies16,17 and provision of comprehensive emergency obstetrical care (CEmOC).18 One of the promising technologies is the use of NASG, otherwise known as “life wrap”.16 The International organization of the Global Library of Women’s Medicine (GLOWM), International Federation of Gynecology and Obstetrics (FIGO), and World Health Organization (WHO) all recommend the use of the NASG. NASG is a first aid device and resuscitation measure to help control the sequelae of bleeding. Evidence proved that it is very important to stabilize women experiencing hypovolemic shock secondary to obstetric hemorrhage.19–21 The NASG is applicable for obstetric hemorrhage, which includes antepartum, intrapartum, and postpartum hemorrhages.22 Evidence suggests that NASG is essential to keep women stable while waiting for blood transfusion and surgeries at sophisticated referral facilities or to manage hemorrhage in delays and transports to referral healthcare facilities.23
In Ethiopia, NASG was introduced as a pilot project in Oromia and Tigray regions in 2011 by the Clinton Health Access Initiative (CHAI) and later on it was scaled up to many other health facilities in Ethiopia.24 However, ensuring the availability of NASG alone cannot guarantee its use in the management of the obstetric hemorrhage. Rather, proper utilization of NASG is mandatory to reduce maternal mortality. In line with the scale up of the NASG, there were limited data on the utilization of NASG in Ethiopia in general and in Tigray region in particular. Hence, this study aimed to assess the utilization rate and factors associated with the non-utilization of NASG in the management of obstetric hemorrhage by the healthcare providers working in maternal healthcare facilities of Mekelle city, Northern Ethiopia. This study may reflect the context of northern Ethiopia and other regions of Ethiopia.
Materials and Methods
Study Setting and Design
The study was conducted in public healthcare facilities in Mekelle city by using an institution-based cross-sectional study design from December 2017 to February 2018. Mekelle city is located 780 km from the capital city of Ethiopia, Addis Ababa. The city had around 586,897 residents in 2015 and had seven sub-cities and 10 health centers, two public general hospitals, and one referral hospital.25
Study Population
All selected healthcare providers working in maternity care of the selected public healthcare facilities.
Eligibility Criteria
Inclusion Criteria
- Healthcare providers registered in the human resources of the healthcare facility who have been working in the maternity services.
Exclusion Criteria
Healthcare providers who had been on leave at the time of data collection time.
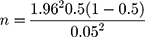
Sample Size Determination
The sample size was calculated using a single population proportion formula.
where, Zα/2 = critical value of the normal distribution at α/2, p is the expected proportion of utilizing NASG, q is the expected proportion of NASG non-utilization, and d is the marginal error.
n<10,000 so, the final sample size (nf) was calculated as nf =
384*1,550/384+1,550=307=742,656/1,934=308
After including 10% of non-responsiveness, the final total sample size was 338.
Sampling Procedure
The sampling technique was simple random sampling. To come up with the sample, all the registered maternal care providers in 13 public healthcare facilities (three hospitals and 10 health centers) were accessed and listed in an excel spreadsheet. Finally, using their employee identification as a sampling frame, the required sample size was selected using simple random sampling by lottery method (Figure 1).
 |
Figure 1 Schematic presentation of sampling procedure for NASG utilization among the healthcare providers working in the public healthcare facilities in Mekelle city. |
Variables
Dependent Variable
- Utilization of NASG
Independent Variables
- Sociodemographics
- Age
- Professional category
- Work experience in years
- Gender
- Health system factors
- Availability of NASG
- Trained on using NASG
- Availability of other ways of treating PPH
- Availability of funds supporting to use NASG
- Perceived as having skill of using NASG
- Knowledge of NASG
- Attitude towards NASG
Operational Definitions
- NASG Utilization: Use of NASG for the management of obstetric hemorrhage.
- Good knowledge: A score greater than 50% from the provided knowledge questions.
- Healthcare provider: Skilled healthcare provider working in the departments of maternity care.
- Favorable attitude: Feeling and thoughts about utilizing NASG and obstetric hemorrhage with a score of greater than 50% of the provided attitude questions.
- Having perceived skill to use the garment in the facility: Self-report of having skill to use NASG in the healthcare facility.
- Lack of experience: Having no experience in applying the NASG during emergency to manage obstetric hemorrhage.
- Trained human power at the facility: Presence of healthcare provider trained on NASG in the respective healthcare facility.
Data Collection Methods
Instruments
A structured questionnaire was used to collect the data using an interviewer. The questionnaires contained questions to capture information on socio-demographic, perceived skill of using NASG, availability of NASG, knowledge, and attitude towards utilization of the NASG. The questionnaire was prepared from various literature considering the study area situation. The questionnaire was standardized by senior program experts and researchers on maternal health. The questionnaire was initially established in English and then translated to the local language, Tigrigna.
Data Collection Process
Eight diploma midwives who have experience in data collection but not working in the selected healthcare facilities were recruited and trained in data collection. In addition, two supervisors were recruited to supervise all activities in the data collection. Fully completed questionnaires were entered into STATA version 14.
Data Quality Assurance
To confirm data quality and validity, the questionnaires were designed from different literature. Both English and Tigrigna versions of the questionnaire were crosschecked by an independent bilingual expert. To maintain the quality of the questionnaire, about 5% of the total sample size was piloted by a similar population in Wukro public general hospital. Data in the questionnaires were checked daily for their consistency and completeness by the supervisors. Respondents were re-interviewed for any incomplete and inconsistent information to ensure quality.
Data Management and Analysis
A Likert scale was created by presenting respondents with a series of negative and positive attitude statements with five possible responses. For positive statements, responses including agree and strongly agree were labeled as “favorable”, and strongly disagree, disagree, and undecided were labeled as “unfavorable”. For negative statements, responses including agree, strongly agree, and undecided were labeled as “unfavorable”, and disagree and strongly disagree were labeled as “favorable” responses.
Data were analyzed using STATA version 14. Data were cleaned by running frequencies to each variable to check outliers, inconsistencies, and missed values for accuracy purposes. The normality of the continuous variables was checked using scatter plots. Descriptive statistics were done on different demographic variables and NASG utilization.
The outcome variable was utilization; those who utilized NASG were coded as “0” and those who did not utilize were coded as “1”. Variables significant at a P-value≤0.05 in the unadjusted (bivariate) analysis were entered into multivariable logistic regressions to identify the independent predictors. Adjusted Odds Ratio (AOR) estimates were obtained and interpreted at 95% CI. As the prediction of the outcome was using a logistic regression model, goodness of fit was tested using the Hosmer–Lemeshow test (HL test).
Results
Socio-Demographic Characteristics
About 250 (74%) of the respondents were female care providers, and 53% of them were nurses. About 26.6% and 14.2% of them were midwives and doctors, respectively. The average age of the care providers was 35.29 years, with a standard Deviation (SD) of ±8.87 years. Similarly, the average years of experience of the care providers was 10.24 years with SD of ±9.31 (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Healthcare Providers Working in Public Healthcare Facilities in Mekelle City, North Ethiopia, February 2018 (N= 338) |
Utilization of NASG
About 121 (35.80%; 95% CI=30.68–41.16%) of the healthcare providers reported that they did not utilize NASG and 217 (64.20%; 95% CI=58.84–69.32%) of them reported that they did utilize NASG for the management of obstetric hemorrhage (Figure 2).
 |
Figure 2 Utilization of NASG among healthcare providers working in public healthcare facilities in Mekelle city, North Ethiopia, February 2018 (n= 338). |
Factors Affecting NASG Non-Utilization
Bivariate Analysis
In the unadjusted analysis, being female with a Crude Odds Ratio (COR)=2.50 (95% CI=1.42–4.41), age with COR=1.04 (95% CI=1.02–1.07), being a BSc nurse with COR=5.06 (95% CI=2.28–11.21), being a diploma nurse with COR=4.33 (95% CI=1.65–11.37), year of work experience with COR=1.03 (80% CI=1.01–1.05), use of NASG to manage obstetric hemorrhage in previous works with COR=0.05 (95% CI=0.01–0.23), and having perceived skill to use the garment in the facility with COR=0.17 (95% CI=0.04–0.72) were statistically significant factors for the non-utilization of the NASG (Table 2).
Multivariate Analysis
In the adjusted analysis of the multivariate logistic regression, females with AOR=2.21 (95% CI=1.06–4.63), use of NASG in previous works to manage PPH with AOR=0.1 (95% CI=0.02–0.48), and having perceived skill to avail use the garment in the facility with AOR=0.10 (95% CI=0.01–0.79) were significantly associated with the non-utilization of the NASG (Table 2).
Discussion
This study was aimed to assess the utilization rate and factors associated with non-utilization of NASG in the management of obstetric hemorrhage in public healthcare facilities of Northern Ethiopia. This study revealed that there were 64.20% (95% CI=58.84– 69.32%) healthcare providers who were utilizing NASG for the management of obstetric hemorrhage. In the adjusted analysis; males, non-utilization of NASG in previous works to manage obstetric hemorrhage, and perceived to avail garment in the healthcare facility were the identified factors associated with the non-utilization of the NASG.
The utilization of NASG in this study was lower compared to a study conducted in Nepal in 2014 which reported all nurses and midwives used NASG in the management of obstetric hemorrhage.26 This difference may be attributed to the limited experience in the use of NASG to manage obstetric hemorrhage in healthcare facilities of Tigray, Ethiopia. However, the utilization of NASG in this study was better compared to a study reported from primary healthcare, Jos North LGA of Plateau state, Nigeria (14.1%),27 Jimma public hospitals (36.2%),28 Ibadan, Nigeria, and Sokoto State Specialist Hospital (35%) in both study areas25,29 and Bayelsa State Nigeria (46.4%) and Benin Central Hospital (42%) of the respondents used NASG in the management of obstetric hemorrhage.30,31 These differences might be attributed to the study setting or study designs. Similarly, different healthcare providers may have different levels of practice. For example, midwives may have a better level of utilization since they are mostly involved with the management of obstetric hemorrhage. The other reason for the variation of NASG utilization might be due to country-to-country difference in scaling up and awareness creation among the healthcare providers. Increasing the utilization and coverage of the NASG requires the involvement of local NASG champions, greater NASG awareness among policymakers and clinicians, as well as a strong advocacy and political will,32 which all have a significant impact on NASG utilization among the healthcare providers working in maternity care.
In the adjusted analysis, it has been shown that the odds of non-utilization of NASG to manage obstetric hemorrhage was almost 2-times higher among female care providers compared to males, while all other variables were kept constant with AOR=2.21 (95% CI=1.06–4.63). There were no accessed studies that showed an association between sex and non-utilization of the NASG. On the other hand, use of NASG in previous works to manage obstetric hemorrhage was a significant predictor of non-utilization of the NASG. The odds of non-utilization of NASG was 90% less likely among care providers who had no experience in the use of NASG to manage OH compared with care providers who did not have the experience to use NASG for the management of obstetric hemorrhage while all other variables were kept constant, with AOR=0.10 (95% CI=0.02–0.48). Even though there were no previous studies which describe the strength of association of non-utilization of NASG with the previous works of experience to manage OH; there were cross-sectional studies in 2017 in primary healthcare, Nigeria, which showed that non-availability and inexperience of the garment were the main hindrances of NASG utilization.13,33 This is because having no experience on utilization of NASG in previous works may have lower reinforcement on the current utilization of the NASG.
Having perceived skill to use the garment in the facility was also a significant predictor of non-utilization of NASG among the maternal healthcare providers. The odds of non-utilization of NASG was 90% less likely among care providers who have perceived to avail garment compared to those who did not perceive to avail garment at the healthcare facility, while all other variables were kept constant with AOR=0.10 (95% CI=0.02–0.48). The finding of this study was similar to the study conducted in Ondo-State, in primary healthcare, Nigeria, which found that awareness about the existence of NASG was high among the respondents.27 Availing NASG does not suffice, but additionally creating awareness and skill of utilization of NASG in the healthcare facilities is crucial.
Strengths and Limitations of the Study
The tool was piloted in a similar facility to validate the research tool. As this is a cross-sectional study, it is not possible to establish causation between the independent and dependent variables.
Conclusions
There was a lower rate of NASG utilization among the healthcare providers for the management of obstetric hemorrhage. Being a male care provider, having no experience of using NASG to manage PPH, and having perceived skill to use the garment in the facility were significantly associated factors for the non-utilization of the NASG. Due emphasis should be given to utilization of NASG to manage obstetric hemorrhage by addressing the identified modifiable factors for non-utilization of NASG by healthcare workers.
Abbreviation
AOR, Adjusted Odds Ratio; CEmOC, Comprehensive Emergency Obstetrical Care; CHAI, Clinton Health Access Initiative; CI, Confidence Interval; COR, Crude Odds Ratio; DALYs, Disability Adjusted Life Years; FIGO, Federation of Gynecology and Obstetrics; GLOWM, Global Library of Women’s Medicine; HL, Hosmer–Lemeshow; M, Kilometer; MMR, Maternal Mortality Ratio; MU, Mekelle University; NASG, Non-pneumatic Anti-Shock Garment; OH, Obstetric Hemorrhage; PPH, Post-Partum-Hemorrhage; SD, Standard Deviation; WHO, World Health Organization.
Data Sharing Statement
The data used to support the findings of this study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
Ethical approval and clearance were obtained from the ethical review committee of the School of Nursing, Mekelle University (MU). Institutional permission was obtained from the Tigray Regional Health Bureau (TRHB) and Mekelle city health office after communicating with a formal letter from the school of nursing, MU. All participants were informed about the purpose of the study and written consent was obtained from the respondents to participate in the study. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. There were no personal identifiers in the data collection and report synthesis.
Acknowledgments
We wish to extend our acknowledgement to MU for financing the study. We would also like to thank the data collectors and healthcare providers in the public healthcare facilities in Mekelle city.
Author Contributions
All authors made a significant contribution to the conception, study design, execution, acquisition, analysis, and interpretation. All authors were involved in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by a non-for-profit sector, MU for research and community services.
Disclosure
The authors declare that they have no competing interests.
References
1. World Health Organization (WHO). World health report 2005: make every mother and child count. Geneva: WHO; 2005. Available from: www.who.int/whr/2005/whr2005_en.pdf.
2. Hogan MC, Foreman KJ, Naghavi M, et al. Maternal mortality for 181 countries, 1980–2008: a systematic analysis of progress towards millennium development goal 5. The institute of health metrics and evaluation (IHME) at the University of Washington in Seattle, USA. Lancet. 2010;375:1609–1623. doi:10.1016/S0140-6736(10)60518-1
3. WHO, UNICEF, UNFPA and The World Bank estimates. Trends in maternal mortality: 1990 to 2010. Available from: http://whqlibdoc.who.int/publications/2012/97892415.
4. Kassebaum NJ, Bertozzi-Villa A, Coggeshall MS, et al. Global, regional, and national levels and causes of maternal mortality during 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2014;384(9947):980–1004.
5. Homer C, Clements V, Donnell NM, Peek M. Elizabeth sullivan: maternal mortality: what can we learn from stories of post partumhaemorrhage. WomenandBirth. 2009;22:97–104.
6. Central Statistics Agency. Ethiopian demographic and health survey. 2000
7. Central Statistics Agency. Ethiopian demographic and health survey. 2005
8. Mourad-Youssif M, Ojengbede OA, Meyer CD, Fathalla M, Galadanci H. Can the non-pneumatic anti-shock garment (NASG) reduce adverse maternal outcomes from postpartum hemorrhage? Evidence from Egypt and Nigeria. J Reprod Health. 2010;7:24.
9. Ngwenya S. Post partum hemorrhage: incidence, risk factors, and out comes in a low-resource setting. Int J Women’s Health. 2016;8:647–650. doi:10.2147/IJWH.S119232
10. Alkema L, Chou D, Hogan D, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenariobased projections to 2030: a systematic analysis by the UN maternal mortality estimation inter-agency group. Lancet. 2016;387(10017):462–474. doi:10.1016/S0140-6736(15)00838-7
11. McCarthy J, Maine D. A framework for analyzing the determinants of maternal mortality. Stud Fam Plann. 1992;23:23–33. doi:10.2307/1966825
12. Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Global Health. 2014;2(6):e323–e333. doi:10.1016/S2214-109X(14)70227-X
13. Lydia B, Ramyil S, Ogundeko O, et al. Knowledge and management of post partumhaemorrhage among skilled birth attendants in primary health centres of Jos North LGA, Plateau State. Public Health Int. 2017;2(4):124–130.
14. Demeke Z. Non-pneumatic anti-shock garment pilot in Ethiopia to reduce maternal mortality secondary to obstetric hemorrhage.
15. Naume C. Traditional and skilled birth attendants in zimbabwe: a situational analysis and some policy considerations. J Anthropol. 2015;2015:11.
16. Knight M, Callaghan WM, Berg C, Alexander S, Bouvier-Colle MH, Ford JB. Trends in postpartum haemorrhage in high resource countries: a review and recommendations from the international postpartum haemorrhage collaborative group. BMC Pregnancy Childbirth. 2009;9:1–10. doi:10.1186/1471-2393-9-55
17. Berhan Y, Berhan B. Review of maternal mortality in Ethiopia: a story of the past 30 years. Ethiop J Health Sci. 2014;24:3–14. doi:10.4314/ejhs.v24i0.2S
18. United Nations. The millennium development goals report 2007. New York; 2007.
19. Stenson AL, Miller S, Lester F. The mechanisms of action of the nonpneumatic anti-shock garment.
20. WHO. Non-pneumatic anti-shock garment. Available from: http://www.who.int/medical_devices/innovation/new_emerging_tech_30.pdf.
21. Miller S, Morris JL, Fathalla MMF, Ojengbede O, Mourad-Youssif M, Hensleigh P. Chapter 38: non-pneumatic anti-shock garments: clinical trials and results. In: International Federation of Obstetrics and Gynecology (FIGO) Book, Postpartum Hemorrhage: New Thoughts, New Approaches. Sapiens Publications; 2012.
22. Roberts S. Chapter 40: hypovolemic and cardiac shock. In: Belfort MA, Saade G, Foley MR, Phelan JP, Dildy GA, editors. Critical Care Obstetrics.
23. Miller S, Fathalla MM, Ojengbede OA, et al. Obstetric hemorrhage and shock management: using the low technology non-pneumatic antishock garment in Nigerian and Egyptian tertiary care facilities. BMC Pregnancy Childbirth. 2010;10:64. doi:10.1186/1471-2393-10-64
24. Hailu S, Enqueselassie F, Berhane Y. Health facility-based maternal death audit in Tigray, Ethiopia. Ethiop J Health Dev. 2010;23(2). doi:10.4314/ejhd.v23i2.53226
25. Kolade A, Tijani A, Oladeji O, Ajibade L. Midwives’ knowledge and utilization of anti-shock garment in prevention of postpartum haemorrhage shock at the University College Hospital, Ibadan Nigeria. J Nurs Health Sci. 2014;3(1):9–16. doi:10.9790/1959-03140916
26. El Ayadi AM, Butrick E, Geissler J, et al. Combined analysis of the non-pneumatic anti-shock garment on mortality from hypovolemic shock secondary to obstetric hemorrhage. BMC Pregnancy Childbirth. 2013;13:208. doi:10.1186/1471-2393-13-208
27. Ohaeri B, Ogbeye GB. Assessment of utilisation of non-pneumatic anti shock garment (NASG) in the control of post-partum haemorrhage among midwives in selected hospitals in Ondo-State, Nigeria. Int J Caring Sci. 2017;10(1):327.
28. Bekele G, Terefe G, Sinaga M, Belina S. Utilization of non-pneumatic anti-shock garment and associated factors for postpartum hemorrhage management among health care professionals’ in public hospitals of Jimma zone, south-West Ethiopia, 2019. Reprod Health. 2020;17:37. doi:10.1186/s12978-020-0891-6
29. Kombo SA, Shehu SB, Farooq MA, Yunusa A. Knowledge and utilization of anti-shock garment in prevention of postpartum hemorrhagic shock in specialist hospital Sokoto, Sokoto State Nigeria. DUJOPAS. 2018;4(2):236–244.
30. Onasoga OA, Duke E, Danide IU, Jack-Ide IO. Midwives ’ knowledge and utilization of non pneumatic anti shock garment in reducing complication of postpartum hemorrhage is selected health care facilties in Bayelsa state Nigeria. IntJ Reproductive Contraceptive Obstet Gynecol. 2015;4:977–981. doi:10.18203/2320-1770.ijrcog20150410
31. Enuku C, Adeyemo F. Knowledge and use of anti-shock garment among midwives in central hospital, Benin City, Edo state. Lautech J Nurs. 2018;23.
32. Jordan K, Butrick E, Yamey G, Miller S, Roy JK. Barriers and facilitators to scaling up the non-pneumatic anti-shock garment for treating obstetric hemorrhage: a qualitative study. PLoS One. 2016;11(3):e0150739. doi:10.1371/journal.pone.0150739
33. Kerr NL, Hauswald M, Tamrakar SR, Wachter DA, Baty GM. An inexpensive device to treat postpartum hemorrhage: a preliminary proof of concept study of health provider opinion and training in Nepal. BMC Pregnancy Childbirth. 2014;14:81. doi:10.1186/1471-2393-14-81
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.