Back to Journals » Clinical Interventions in Aging » Volume 13
Utility of the Care Dependency Scale in predicting care needs and health risks of elderly patients admitted to a geriatric unit: a cross-sectional study of 200 consecutive patients
Authors Doroszkiewicz H, Sierakowska M , Muszalik M
Received 11 December 2017
Accepted for publication 7 March 2018
Published 8 May 2018 Volume 2018:13 Pages 887—894
DOI https://doi.org/10.2147/CIA.S159511
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Richard Walker
Halina Doroszkiewicz,1 Matylda Sierakowska,2 Marta Muszalik3
1Department of Geriatrics, Medical University of Bialystok, Bialystok, Poland; 2Department of Integrated Medical Care, Medical University of Bialystok, Bialystok, Poland; 3Department and Clinic of Geriatrics, Nicolaus Copernicus University, Collegium Medicum in Bydgoszcz, Bydgoszcz, Poland
Objective: The aim of the study was to evaluate the usefulness of the Polish version of the Care Dependency Scale (CDS) in predicting care needs and health risks of elderly patients admitted to a geriatric unit.
Methods: This was a cross-sectional study of 200 geriatric patients aged ≥60 years, chronologically admitted to a geriatrics unit in Poland. The study was carried out using the Polish version of the CDS questionnaire to evaluate biopsychosocial needs and the level of care dependency.
Results: The mean age of the participating geriatric patients was 81.8±6.6. The mean result of the sum of the CDS index for all the participants was 55.3±15.1. Detailed analysis of the results of evaluation of the respondents’ functional condition showed statistically significant differences in the levels of care dependency. Evaluation of the patients’ physical performance in terms of the ability to do basic activities of daily living (ADL) and instrumental ADL (I-ADL) showed statistically significant differences between the levels of care dependency. Patients with high dependency were more often prone to pressure ulcers – 13.1±3.3, falls (87.2%), poorer emotional state – 6.9±3.6, mental function – 5.1±2.8, and more often problems with locomotion, vision, and hearing. The results showed that locomotive disability, depression, advanced age, and problem with vision and hearing are connected with increasing care dependency.
Conclusion: CDS evaluation of each admitted geriatric patient enables us to predict the care needs and health risks that need to be reduced and the disease states to be improved. CDS evaluation should be accompanied by the use of other instruments and assessments to evaluate pressure ulcer risk, fall risk, and actions toward the improvement of subjective well-being, as well as correction of vision and hearing problems where possible and assistive devices for locomotion.
Keywords: Care Dependency Scale, care needs, health risks, elderly
Introduction
The process of population aging is deepening worldwide. Epidemiological studies demonstrate the deterioration of locomotive function, poorer health, and a number of diseases occurring in elderly people.1,2 The deteriorating health and poorer performance resulting from the aging process increase the need of care.3–5 It is observed that new measurements are being introduced to assess the care needs of elderly people.
The instrument that enables professional evaluation is the Care Dependency Scale (CDS) questionnaire including 15 items that refer to biopsychosocial needs that every person, whether healthy or ill, has and wants to satisfy, based on the assumptions of Virginia Henderson’s nursing theory.6
The scale shows to what extent the patient’s needs are not satisfied and in what areas they need assistance/support. It is worth emphasizing the advantages of practical application of the scale to assess patients’ needs, especially regarding those that are unable to communicate or have limited communication capabilities.
In her theory of nursing, Virginia Henderson identified 14 basic needs, which can only be satisfied with the help of other people.6 According to the author, nursing is professional assistance to the patient, whose goal is to restore independence as soon as possible and to provide care that the person needs. The essence of this concept is professional assistance of the caregiver, the goal of which is to “transfer” the patient from dependency to independency.
Patient evaluation using the CDS can be performed by a nurse at the first stage of the nursing process; it also enables us to plan further care and discussion as part of interdisciplinary consultations targeted at the diagnosis and intervention of different specialists. Evaluation of the patient’s nursing needs can be repeated, so that it may provide new information on the care-related situation and effectiveness of previous activities taken to reduce the patient’s level of dependency.7
The CDS is considered appropriate to evaluate patients in different fields of medicine, where it has been validated and developed since 1996, initially in the Netherlands by Ate Dijkstra and then in other countries, including Poland.8–10 Recommendations by the authors of previous studies concerning further development and implementation of CDS in preliminary evaluation of estimated care needs and establishing the scope and kind of help and support regardless of the place of providing care show that this study is justified.9,10
The aim of the study was to evaluate the usefulness of the Polish version of the CDS in predicting care needs and health risks of elderly patients admitted to a geriatric unit.
Patients and methods
Patients
The study involved 200 patients aged ≥60 years, chronologically admitted to a geriatrics unit in North-Eastern Poland. All patients who were involved in the study provided written informed consent to participate in the study. Most of the patients were referred to the hospital by general practitioners due to aggravation of chronic conditions or due to newly developed medical problems.
Measurements and procedure
The research involved a cross-sectional study. The study was carried out using the Polish version of the CDS questionnaire to evaluate biopsychosocial needs and the level of care dependency.8 The CDS consists of 15 items, including biopsychosocial needs that every person, whether healthy or ill, has and wants to satisfy, such as eating and drinking, continence, body, posture, mobility, day/night pattern, getting dressed and undressed, body temperature, avoidance of danger, hygiene, communications, contact with others, sense of rules and values, daily activities, recreational activities, and learning activities. Each item has a brief description and five care dependency criteria.
Five-point Likert scale was used to evaluate the items, where 1 means complete dependency on others’ care, 2 – high dependency, 3 – partial dependency, 4 – limited dependency, and 5 – the patient is almost independent of the care of others. After the interpretation of the scores in the scale, each patient was attributed to one of the three levels of dependency, where the 15–44 range means high level of care dependency, 45–59 – medium dependency, and 60–75 – low dependency. Accordingly, the lower the value, the more care dependent the patient is.12
Data concerning self-care performance, locomotive performance, emotional status, cognitive functions, evaluation of vision, hearing, the risk of development of pressure sores or falls, self-evaluation of the health status, and the sense of loneliness were collected from medical documentation based on the selected elements of Comprehensive Geriatric Assessment (CGA). The geriatric patients underwent CGA, which is a multidimensional and multidisciplinary diagnostic process with the purpose of planning and/or delivering care.11 CGA is being performed routinely at the geriatric unit by an interdisciplinary team of a physician, a nurse, a psychologist, and a physiotherapist.
The participants were divided into the following two groups on the basis of the median of distribution of the age variable – 83 years: group I were patients aged ≤82 years (n=98), and group II, patients aged ≥83 years (n=102).
Objective sociodemographic data
The sociodemographic characteristics involved the participants’ age, sex, marital status, and mode of dwelling (alone or with family).
Measures of subjective well-being
Sense of loneliness was assessed using the question “Do you feel lonely?” (answer options: never, sometimes, and often).
Self-rated health was evaluated using the question “How do you evaluate your health status?” (answer options: significantly worse, moderately worse, moderately better, and significantly better).
The geriatric patients’ emotional state was evaluated using Yesavage’s Geriatric Depression Scale (GDS), where the range 0–5 means no depression and 6–15, a growing risk of depression.12
Objective measures or states
The patients’ physical functional condition was evaluated using the Barthel scale, including eating and drinking, transfer from bed to chair and back/sitting down, personal hygiene, using the toilet, bathing, walking on flat surfaces, climbing up and down the stairs, getting dressed and undressed, and (urinary and fecal) continence. The total score of Barthel Index ranges from the minimum of 0 point (complete dependence) to the maximum of 100 points (complete independence).13
The instrumental functional status (instrumental activities of daily living [I-ADL]) was evaluated using Duke Older Americans Resources and Services Assessment.14 The six evaluated domains of functions covered housework (cleaning floors and other tasks, using the telephone, preparing their own meals, handling their own money, going shopping, and taking their medicines). The summary score ranges from 0 point (lowest function) to 12 points (highest function), with 9–12 points being the evidence of independence.
The assessment of the risk of development of pressure ulcers was evaluated using the Norton test, where a score of ≤14 points indicates the risk.15
Cognitive functions were evaluated using the Abbreviated Mental Test Score (AMTS) by Hodgkinson. The range of scores in the test is from 0 to 10, where higher scores mean better mental function.16
Balance and gait were evaluated with a short form of the Performance Oriented Mobility Assessment (POMA). The score ranged from the minimum of 0 point, indicating inability to perform any task, up to a maximum of 10 points, indicating full independence.17
Procedure and ethical considerations
The study was performed in 2017. The approval of the Bioethics Committee of the Medical University of Białystok was obtained for the study (resolution number R-I-002/177/2017).
Statistical analysis
The obtained results were subject to statistical analysis, in which the arithmetic mean and SD were calculated for quantitative variables, whereas the percentage distribution was calculated for qualitative variables.
The Mann–Whitney U-test was used for quantitative qualities to compare the selected groups, and in the case of a higher number of compared groups, the Kruskal–Wallis test was used. In the analysis, the Spearman’s rank correlation model was applied. The chi-square test was used to evaluate qualitative variables. The significance level of p<0.05 was assumed. Calculations were performed using Statistica statistical package.
Results
Table 1 shows the sociodemographic characteristics of the studied group of geriatric patients and the evaluation parameters of their functional performance in terms of three levels of care dependency. The mean result of the sum of the CDS index for all the participants was 55.3±15.1, and in each level of care dependency: high dependency, 33.2±8.2; medium dependency, 52.2±6.0; and low dependency, 67.5±4.6, respectively. The differences were statistically significant (p<0.000) (Table 1).
The mean age of the participating geriatric patients was 81.8±6.6. The vast majority of them were women (69.0%). About one-third of the respondents (35.0%) were married, and 38.0% lived alone. More than half of the elderly people (57.5%) assessed their health as poor.
Detailed analysis of the results of evaluation of the respondents’ functional condition showed statistically significant differences in the levels of care dependency. Evaluation of the people’s physical performance in terms of the ability to do basic ADL and I-ADL showed statistically significant differences between the levels of care dependency. Highly dependent patients had poorer ability to do ADL and I-ADL; the mean rate of ADL was 43.0±30.9 and of I-ADL was 2.2±2.5. People with high dependency were more often prone to pressure ulcers – 13.1±3.3, falls (87.2%), had poorer emotional state – 6.9±3.6, mental function – 5.1±2.8, and more often had problems with locomotion, vision, and hearing (Table 1).
Further in the study, 15 needs of the geriatric patients were evaluated using CDS (Table 2). Detailed analysis of needs within each level showed that the highest level of care dependency was associated with satisfying needs such as recreational activities (1.14), daily activities (1.59), learning activities (1.78), mobility (1.85), getting dressed and undressed (1.93), avoidance of danger (1.95), continence (2.14), contact with others (2.36), eating and drinking (2.36), body temperature (2.59), body posture (2.59), and day/night pattern (2.68) (Table 2).
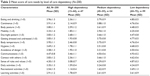  | Table 2 Mean score of care needs by level of care dependency (N=200) |
Table 3 shows the sociodemographic characteristics of the studied group of geriatric patients and the evaluation parameters of their functional performance in the age groups. The mean result of the sum of the CDS index was 58.0±14.9 (patients aged ≤82 years) and 52.7±14.9 (patients aged >83 years), respectively.
The differences were statistically significant (p<0.005) (Table 3). Detailed analysis of the results of evaluation of the respondents’ functional condition showed statistically significant differences between the age groups. Evaluation of the people’s physical performance in terms of the ability to do ADL and I-ADL showed statistically significant differences between the age groups.
Older patients had poorer ability to do ADL and I-ADL; the mean rate of ADL was 74.0 (vs patients aged ≤82 years – 80.1) and of I-ADL – 5.6 (vs 7.3). Older patients had poorer mental function – 5.8 (vs patients aged ≤82 years – 7.0), they were more often prone to falls (67.7% vs patients aged ≤82 years – 50.1%), and more often had problems with locomotion – 76.5% vs 61.2%, vision – 41.2% vs 38.7%, and hearing – 53.9% vs 31.6% (Table 3).
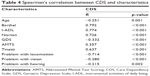
CDS showed negative correlation with locomotion (r=−0.714, p<0.001), emotional state (r=−0.332, p<0.001), patients’ age (r=−0.251, p=0.001), vision (r=−0.280, p<0.001), and hearing (r=−0.215, p=0.002). The results showed that locomotive disability, risk of depression, advanced age, and problems with vision and hearing are connected with increasing care dependency (Table 4).
Discussion
The problems of providing care for elderly people are currently one of the most common and difficult challenges for all health care and social care providers. The priority in caring for elderly people is to sustain as long as possible their full capabilities allowing independent functioning in their place of residence and to improve the quality of their lives.
This study involved the evaluation of the usefulness of the Polish version of the CDS in predicting health risks and care needs of geriatric patients admitted to a geriatric unit.
Half of the participants (50.5%) were patients who were dependent on the care of other people in satisfying their needs. A total of 23.5% of the patients represented high care dependency level and 27.0%, medium care dependency.
The analysis of the relationship between sociodemographic factors in the studied group showed an increase in care dependency with advancing age. Factors such as sex, marital status, or the living alone/with family did not have a statistically significant influence on the level of care dependency.
The analysis of the relationship between subjective well-being factors showed a significant influence of the participants’ health self-evaluation and emotional state on the level of care dependency.
In the category of highly care-dependent patients, the proportion of people who assessed their health as worse and had a higher average score of GDS was higher than among low-dependency patients. No relationship was observed between the sense of loneliness and the level of care dependency. Similar proportions of geriatric patients faced the problem of loneliness irrespective of the care category.
The analysis of functional capability of the participants showed a relationship between the results of the evaluation and the level of care dependency.
A higher level of care dependency was significantly correlated with poorer results of functional status in all the evaluated areas.
Patients from the high-dependency category presented significantly worse ability to do ADL (43.0 vs 93.4) and I-ADL (2.2 vs 9.0) compared to patients with a low level of dependency.
In addition, patients from the high-dependency category were more often exposed to the development of pressure ulcers (mean 13.1 vs 18.4), had poorer cognitive capacity (mean 5.1 vs 7.4), and significantly more often had problems with vision (57.4% vs 29.2%) and hearing (53.2% vs 31.3%). Problems with locomotion occurred statistically significantly more often in patients from the high-dependency category (94.0% vs 52.5%).
This study shows that advancing age and deteriorating functional condition of the studied geriatric patients is an important factors of the high level of care dependency.
The review of results of previous studies using CDS, published in many countries including Poland, shows that there is a relation between age, functional capabilities, and the level of care dependency.18–20
A study by Lohrmann et al18 carried out in German hospitals among 1,806 patients >60 years of age hospitalized in different units showed that most patients were independent in terms of care, and care dependency was growing with advancing age.
The results of other authors’ research point to a correlation between the level of care dependency (CDS) and performance (ADL). Higher level of care dependency was related to lower self-care performance in terms of ADL.19,20
In this study, we identified patients from the health risk group, ie, in advanced age, with locomotive disability, depression, as well as problems with vision and hearing.
This study shows that CDS is a useful instrument to be used by nurses in patient assessment. It should be stressed out that categorizing patients using CDS makes it possible to identify patients from the risk group, provides more information on varied care needs, allows more thorough evaluation of the needs, and can help better plan and implement care for those who are at risk of pressure ulcers, falls, and depression. Besides, it allows determination of the directions of intervention in order to improve the health status, overcome disability in elderly patients through activities such as providing equipment that facilitates locomotion (canes, crutches, and a wheelchair), treating depression, or correcting vision and hearing impairments. Potential correction of reversible conditions prevents the deepening of care dependency.
A study by Mertens et al concerning the usability of CDS in estimating the risk of fall among patients staying in hospital and in a nursing home showed that people at risk of falls were more often care dependent than were people without that risk.21
Moreover, in this study we estimated the needs in satisfying which elderly people needed the assistance of others. The highest level of care dependency was observed in the following needs: recreational activities, daily activities, learning activities, mobility, getting dressed and undressed, avoidance of danger, continence, contact with others, eating and drinking, body temperature, body posture, and day/night pattern.
A previous study carried out in Poland with the use of CDS among residents of elderly nursing homes and long-term care institutions showed significant reduction in independence among people >80 years of age, especially in the case of those with chronic somatic diseases and increased demand for care.22 Residents of nursing homes were completely or largely care dependent and had the greatest deficits in terms of personal hygiene, mobility, avoidance of dangers, and ADL.
Another study carried out in Poland among 227 elderly patients of Clinic of Geriatrics showed that the majority of respondents achieved high and medium levels of functional capability. The main problems associated with the fulfillment of needs were difficulties with the adoption of appropriate body posture, movement restrictions, and problems connected with participating in leisure activities, unassisted, outside the home. The most significant problems were related to sleep disorders, restrictions in freedom of movement. Good daily functioning of geriatric patients significantly depended on their intellectual and mental efficiency.23
The authors of this manuscript believe that elderly people need multidimensional and holistic approach to solving complex medical and social problems. When organizing and planning care for geriatric patients, individual assessment of biopsychosocial needs, age, and functional condition of the person should be considered. Only care that is based on individual recognition of needs can accurately address the scope of the needed assistance, improve the quality of life, rationalize the costs of care, assist allocation, and support the patient’s independence as long as possible.24
Evaluation of the needs of geriatric patients done by nurses could help caregivers provide the care for the patient at home, indicating areas of needs in which the patients really need assistance/support, ensure proper temporal organization of care, and prevent neglect or greater care dependency.25
CDS is a useful instrument to evaluate the needs of elderly, care-dependent people. It must be emphasized that further subjective and objective measurements for each patient categorized as care dependent are necessary to evaluate health risks such as pressure ulcers, falls, and depression, or to overcome disability by implementing interventions, ie, pressure ulcer prevention, anti-bedsore mattresses, equipment that facilitates mobility (canes, crutches, and a wheelchair), depression treatment, correcting vision impairment, or considering the use of hearing aids in people with hearing impairments.
Conclusion
CDS evaluation of each admitted geriatric patient enables us to predict the care needs and health risks that need to be reduced and the disease states to be improved. CDS evaluation should be accompanied by the use of other instruments and assessments to evaluate pressure ulcer risk, fall risk, and actions toward the improvement of subjective well-being, as well as correction of vision and hearing problems where possible and assistive devices for locomotion.
Limitations of the study
According to the authors, the main limitations of the study are the design (cross-sectional) and the study group, including only patients of a geriatric unit. The authors agree it is necessary to develop their research by increasing the number of participants and following the age cohort within, eg, 6 months ahead in order to track the stability of CDS and patients’ experiences in terms of overcoming disability or reducing health risk. The health risk needs to be monitored on the regular basis.
Acknowledgment
The study was financed in part by the Ministry of Science and Higher Education, grant number N/ST/ZB/17/002/3301.
Disclosure
The authors report no conflicts of interest in this work.
References
Pędich W, Wilmańska J, Bień B, et al. Niesprawność fizyczna, poznawcza i emocjonalna w populacji osób starszych a świadczenie opieki [Physical, cognitive and emotional disability in the elderly population vs the provision of care]. In: Sytuacja zdrowotna osób w starszym wieku w Polsce: aspekt medyczny i społeczno-demograficzny. Łódź, Poland: Wydawnictwo Szkoła Zdrowia Publicznego; 2000:149–156. Polish. | ||
Bień B, Wojszel ZB, Wilmańska J, et al. Starość pod ochroną. Opiekunowie rodzinni niesprawnych osób starych w Polsce. Porównawcze Studium Środowiska Miejskiego i Wiejskiego [Old Age Under Protection. Family Caregivers of Disabled Elderly People in Poland: A Comparative Study of Urban and Rural Environments]. Kraków, Poland: Oficyna Wydawnicza TEXT; 2001. Polish. | ||
Bień B. Stan zdrowia i sprawność ludzi starszych [Health and ability status of elderly people]. In: Synak B, editor. Polska Starość. Gdańsk, Poland: Wydawnictwo Uniwersytetu Gdańskiego; 2002:35–77. Polish. | ||
Wizner B, Skalska A, Klich-Rączka A, et al. Ocena stanu funkcjonalnego u osób w starszym wieku [Evaluation of the functional status of elderly people]. In: Mossakowska M, Więcek A, Błędowski P, editors. Aspekty medyczne, psychologiczne, socjologiczne i ekonomiczne starzenia się ludzi w Polsce. Poznań, Poland: Polsenior Termedia; 2012:81–94. Polish. | ||
Doroszkiewicz H, Bień B. Nursing care for the community dwelling people at advanced old age. Gerontol Pol. 2003;2(1):22–26. | ||
Henderson V. The concept of nursing. J Adv Nurs. 1978;3(2):113–130. | ||
Lohrmann C, Dijkstra A, Dassen T. Care dependency: testing the German version of the care dependency scale in nursing homes and on geriatric wards. Scand J Caring Sci. 2003;17(1):51–56. | ||
Dijkstra A, Buist G, Brown L, et al. An international psychometric testing of the nursing-care dependency (NCD) scale. J Adv Nurs. 2000;4:944–952. | ||
Dijkstra A, Coleman M, Tomas C, Välimäki M, Dassen T. Cross-cultural psychometric testing of the care dependency scale with data gathered in three countries. J Adv Nurs. 2003;43(2):181–187. | ||
Dijkstra A, Muszalik M, Kędziora-Kornatowska K, Kornatowski T. Care dependency scale – psychometric testing of the Polish version. Scand J Caring Sci. 2010;24(Suppl 1):62–66. | ||
Rubenstein LZ. An overview of comprehensive geriatric assessment. In: Rubenstein LZ, Wieland D, Bernabei R, editors. Geriatric Assessment Technology. The State of the Art. Milan: Editrice Kurtis; 1995:1–9. | ||
Sheikh JI, Yesavage JA. Geriatric depression scale (GDS): recent evidence and development of a shorter version. Clin Gerontol. 1986;5(1–2):165–173. | ||
Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J. 1965;14:61–65. | ||
Fillenbaum GG, Smyer MA. The development, validity and reliability of OARS multidimensional functional assessment questionnaire. J Gerontol. 1981;36(4):428–434. | ||
Norton D, McLaren R, Exton-Smith A. An Investigation of Geriatric Nursing Problems in Hospital. London: National Corporation for the Care of Old People; 1962. | ||
Grodzicki T, Kocemba J, Skalska A. Geriatria z elementami gerontologii ogólnej. Podręcznik dla lekarzy i studentów [Geriatrics with Elements of General Gerontology: Physician and Student Manual]. Kraków, Poland: Via Medica; 2006. Polish. | ||
Tinetti ME. Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc. 1986;34(2):119–126. | ||
Lohrmann C, Dijkstra A, Dassen T. The care dependency scale: an assessment instrument for elderly patients in German hospitals. Geriatr Nurs. 2003;24(1):40–43. | ||
Boggatz T, Farid T, Mohammedin A, Dijkstra A, Lohrmann C, Dassen T. Psychometric properties of the extended care dependency scale for older persons in Egypt. J Clin Nurs. 2009;18(23):3280–3289. | ||
Muszalik M, Marzec A, Zielińska-Więczkowska H. The selected aspects of geriatric patients functioning evaluation. Med Biol Sci. 2012;26(4):97–101. | ||
Mertens EI, Halfens RJG, Dassen T. Using the care dependency scale for fall risk screening. J Adv Nurs. 2007;58(6):594–601. | ||
Muszalik M, Kędziora-Kornatowska K, Kornatowski T. Care dependency scale as an assessment instrument for elderly patients in long care-term and social welfare-first research in Poland. In: Saracen A, editor. Holistic care of the elderly. Radom, Poland: Radomska Szkoła Wyższa, 2009:31–41. | ||
Muszalik M, Kornatowski T, Zielińska-Więczkowska H, Kędziora-Kornatowska K, Dijkstra A. Functional assessment of geriatric patients in regard to health-related quality of life (HRQoL). Clin Interv Aging. 2015;10:61–67. | ||
Cassel CK. Researching the health of elderly people. BMJ. 1994;308:1655–1656. | ||
Bień-Barkowska K, Doroszkiewicz H, Bień B. Silent strain of caregiving: exploring the best of distress in family carers of geriatric patients. Clin Interv Aging. 2017;12:263–274. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.