Back to Journals » International Journal of Women's Health » Volume 15
Using the WHO Self-Reporting Questionnaire-20 (SRQ-20) to Detect Symptoms of Common Mental Disorders among Pregnant Women in Vietnam: a Validation Study
Authors Do TTH , Bui QTT , Ha BTT , Le TM , Le VT, Nguyen QCT, Lakin KJ , Dang TT, Bui LV, Le TC, Tran ATH, Pham HTT, Nguyen TV
Received 16 January 2023
Accepted for publication 6 April 2023
Published 14 April 2023 Volume 2023:15 Pages 599—609
DOI https://doi.org/10.2147/IJWH.S404993
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Trang Thi Hanh Do,1 Quyen Thi Tu Bui,2 Bui Thi Thu Ha,3 Thi Minh Le,3 Vui Thi Le,3 Quynh-Chi Thai Nguyen,3 Kimberly Joyce Lakin,4 Tung Thanh Dang,5 Loi Van Bui,5 Thien Cong Le,5 An Thi Ha Tran,5 Hien Thi Thu Pham,5 Tuan Van Nguyen5
1Faculty of Environmental and Occupational Health, Hanoi University of Public Health, Hanoi, Vietnam; 2Faculty and Fundamental Sciences, Hanoi University of Public Health, Hanoi, Vietnam; 3Faculty of Social and Behavioral Sciences, Hanoi University of Public Health, Hanoi, Vietnam; 4Nossal Institute for Global Health, Melbourne School of Population and Global Health, Melbourne, Victoria, Australia; 5The National Institute of Mental Health, Bach Mai Hospital, Hanoi, Vietnam
Correspondence: Quyen Thi Tu Bui, Department of Biostatistics, Faculty of Fundamental Sciences, Hanoi University of Public Health, 1A Duc Thang Street, Bac Tu Liem District, Hanoi, Vietnam, Tel +84 912 225 245, Fax +84 24 6266 2385, Email [email protected]
Purpose: Detection of antenatal common mental disorders in low-resource settings like Vietnam is important and requires a reliable, valid and practical screening tool. Currently, there is no such tool validated for use among pregnant women in Vietnam. This study aims to assess the validity of the Vietnamese version of the 20-item Self Reporting Questionnaire (SRQ-20) by evaluating its reliability, factorial structure, and performance in detecting common mental disorder (CMD) symptoms, thereby identifying the optimum cut-off score for CMD screening among pregnant women in Vietnam.
Participants and Methods: A total of 210 pregnant women from four rural communes participated in a face-to-face interview using the Vietnamese version of the SRQ-20, followed by a clinical diagnostic interview based on ICD-10 diagnostic criteria of CMDs. The reliability of the SRQ-20 was assessed by calculating the scale’s Cronbach’s alpha to measure internal consistency. Factor analyses were undertaken to examine the factor structure of the instrument. The Receiver Operating Characteristic (ROC) curve analysis was performed to assess the performance of the SRQ-20 against the clinical diagnosis and to identify the optimum cut-off score.
Results: Internal consistency was good, with a Cronbach’s alpha of 0.87. Factor analyses resulted in a 4-factor solution. The area under the ROC curve (AUC) for detection of CMDs was 0.90. The optimum cut-off score of the SRQ-20 for detection of CMD symptoms among Vietnamese pregnant women was 5/6.
Conclusion: The Vietnamese version of the SRQ-20 has the capacity to detect CMDs among pregnant women effectively and is recommended for use as a screening tool for CMDs in antenatal care settings in Vietnam.
Keywords: SRQ-20, screening, common mental disorders, pregnant women, Vietnam
Introduction
The mental health of women during pregnancy and in the year after birth has been well documented in high-income countries (HICs). In this context, research suggests that 10% of pregnant women experience some type of mental disorder.1,2 However, a review by Fisher et al revealed that approximately 15% of women in low- and middle-income countries (LMICs) experience common mental disorders (CMDs), such as depression, anxiety and adjustment disorders, antenatally and 20% postnatally.1 Despite the disproportionate burden of CMDs among pregnant women in LMICs, the perinatal mental health of women in such contexts has received significantly less scholarly attention. Childbearing women in LMICs are at risk of developing CMDs if they are socioeconomically disadvantaged, have an unintended pregnancy, are unmarried, experience intimate partner violence, or have a history of mental health problems.1 Notably, women who experience CMDs during pregnancy are less likely to attend antenatal care and more likely to report substance misuse and lower than expected weight gain.2 This may not only result in adverse obstetric outcomes for the woman, such as intrauterine growth restriction, but can have adverse consequences for the child. Wachs et al have shown that children of depressed mothers living in LMICs experience cognitive and motor delay, as well as undernutrition and stunting.3 The far-reaching consequences of CMDs emphasize the importance of early detection of symptoms among pregnant women, particularly those in living resource-constrained settings.
As a consequence of rapid social and economic development, Vietnam is in an epidemiological transition with increasing rates of non-communicable diseases, including mental health disorders.4 Bao Giang et al found that in a rural area in Vietnam, the prevalence of mental distress was 5.4%, with only 42% of the individuals receiving treatment.5 In their study, Fisher et al revealed that 33% of the women visiting health clinics in Ho Chi Minh City were depressed after giving birth.6 Moreover, multiple studies in Vietnam have highlighted the association between intimate partner violence, including emotional abuse and physical and sexual violence, and an increase in CMD symptoms among women during and after pregnancy.7–11 Another study revealed that women with fetal abnormalities also had a high risk of developing antenatal depression. As a result, Hue et al call for implementing formal screening programs into standardized perinatal care in Vietnam to enable early detection of psychological disorders.12 Until 2004, Vietnam’s national plan of action only focused on treating schizophrenia and epilepsy in hospitals, with no health promotion or primary care-based policies addressing mental health. Recently, the Vietnamese government developed a five-year national plan of action (2006–2010), which incorporates mental health issues, and proposes to screen pregnant women and children for mental illnesses.13 Nevertheless, challenges remain in improving Vietnam’s health system to respond to the needs of those with mental illnesses, particularly vulnerable populations such as pregnant women.
The World Health Organization (WHO) has developed numerous screening tools for psychiatric disorders; however, most require trained personnel for administration, are time-consuming and cannot be feasibly implemented at the primary care level. This prompted the development of the Self-Reporting Questionnaire (SRQ-20), a 20-item mental disorder screening tool for patients in primary healthcare settings.14,15 The SRQ-20 instrument contains 20 questions in simple language, which ask respondents about symptoms and problems associated with CMDs. Each question requires a yes/no response and is accordingly scored a “0” or “1”, with a score of “1” indicating that the symptom was present in the past month, and a score of “0” suggesting that the symptom was absent.14 Though studies have found that the SRQ-20 has high face and criterion validity, is cost-effective, and can be administered by a lay health worker, the cut-off score, validity, and reliability of the instrument varies across settings,15 and the literature recommending a cut-off score for screening for CMDs among pregnant women is currently very limited. Therefore, implementation of the SRQ-20 at the community- or primary care-level for a specific population requires validation of the screening tool in that setting.15 Several studies have assessed the validity of the SRQ-20 instrument at the primary care level in LMICs. These studies reveal that cut-off, validity, and reliability can not only vary between contexts but are also influenced by the gender, age, language, and culture of the population.15,16 For instance, Netsereab et al found that while the SRQ-20 had good internal reliability in primary care settings in Eritrea, the cut-off scores were different for women and men.15 In the context of Vietnam, Giang et al have adapted and validated the SRQ-20 in a rural district hospital setting, assessing the tool’s performance in different sociodemographic groups.17 The instrument was found to perform significantly better for those who were single, as well as those aged between 18 and 24 years, though only face validity and criterion validity of the instrument were assessed in this study. For future use of the SRQ-20 tool in Vietnam, Giang et al stressed the need to identify the optimal cut-off points for different sociodemographic groups.17 However, to date, only one study has used the SQR-20 tool to assess CMDs specifically among pregnant women in Vietnam, using a cut-off score of 7 to classify women into two groups, ie, with low or high levels of common mental disorder,18 based on the results of the validation study by Giang et al.17 Early detection of symptoms among pregnant women in low-resource settings, such as Vietnam, is essential to prevent adverse consequences of CMDs for both mother and child.3 However, a reliable and practical screening tool has not yet been validated to detect mental health disorders among pregnant women in Vietnam. In light of this, this study aims to assess the validity of the SRQ-20 by evaluating its reliability, factorial validity, and its performance in detecting CMD symptoms, thereby identifying the optimum cut-off score for CMD screening among pregnant women in Vietnam.
Materials and Methods
Study Design
A cross-sectional design was used for this study.
Study Setting and Population
The study was conducted in four communes with the highest number of pregnant women in Hiep Hoa – a rural district in Bac Giang province, which was purposely selected based on the population booklets managed by Hiep Hoa District Health Center. Hiep Hoa district has an area of 102 km2 and a population of 252,122 people, among which 92% are farmers, and is 60 km from Hanoi, the capital city of Vietnam.19 All 321 pregnant women living in the four selected communes were sampled for the study, and 210 actually participated. This sample size is sufficient for factor analysis, considering the rule of thumb in calculating sample size for factor analysis, being that the ratio of participants to variables should be no less than 10 to 1.20,21
The 20-Item Self Reporting Questionnaire
The 20-item Self Reporting Questionnaire (SRQ-20) was developed to screen for non-psychotic disorders. It consists of 20 yes/no questions asking respondents about symptoms and problems likely to occur in people with neurotic disorders in the past 30 days.22 Each item is scored either 1 if the answer is “yes”, or 0 if the answer is “no”; therefore, the possible maximum score of the scale is 20.22 This study used the Vietnamese version of the SRQ-20, which underwent a back translation process with involvement of bilingual public health researchers and psychiatrists. Pilot testing of the questionnaire was also undertaken with community people.17 These steps prompted some modification of wording in the final translated version compared to the first translated version to make the instrument understandable to people from a rural setting without changing the meaning of the items in the original questionnaire.17
Data Collection
Data were collected in June 2022. We obtained a list of all pregnant women residing the four select communes based on the communes’ population booklets. The population booklets consist of various information about the commune’s population such as the number of households, demographic characteristics of each member of the household, changes in the household including the number of new-born children, women’s pregnancy history, death of household members, and migration history of household members. The information is updated monthly by trained population collaborators as required by the Vietnam Ministry of Health. It provides the most comprehensive and up-to-date information for obtaining the pregnant women sampling frame, capturing all pregnant women in the communes at the time of the study.
All pregnant women living in the four selected communes were invited to their nearest commune health center to be involved in a face-to-face interview using the SRQ-20 with trained research assistants who were junior academic staff from Hanoi University of Public Health. A half-day training was conducted to equip these interviewers with research interview skills and ethical conduct of the research. In this training, issues related to confidentiality and privacy during interviewing participants were emphasized. The SRQ-20 interview was followed by a clinical mental diagnosis session with qualified psychiatrists from the National Institute of Mental Health. Identification of cases through in-depth clinical interviews was based on ICD-10 diagnostic criteria of any depressive disorders (major depressive disorder, depressive episode) or anxiety disorders (generalized anxiety disorder, panic disorder, phobias, social anxiety disorder, obsessive-compulsory disorder, and post-traumatic stress disorder). In total, 210 pregnant women participated in the interviews and clinical diagnosis. Every SRQ-20 interview and clinical diagnosis session at the commune health centers was conducted in a private room to ensure privacy and confidentiality. Each SRQ-20 interview took about 5 minutes, while the average time to complete a clinical diagnostic interview was 50 minutes. The psychiatrists were completely blind to the results of the SRQ-20 assessment. The language of the questionnaire administration and clinical diagnosis was Vietnamese. Each participant was reimbursed 50,000 VND (about 2 USD) for their time and effort spent on participation in the SRQ-20 interview and the clinical assessment. This type and amount of incentive is common for community-based surveys in Vietnam.
Statistical Analysis
Data were analysed with STATA software version 14.1. The demographic characteristics of the participants were reported by descriptive analyses. The reliability of the SRQ-20 was assessed by calculating the scale’s Cronbach’s alpha to measure internal consistency. A Cronbach’s alpha value equal to or higher than 0.7 indicates good reliability.23 Factorial validity was assessed by performing an exploratory factor analysis (EFA) and then a confirmatory factor analysis (CFA). EFA was conducted using principal component analysis with varimax rotation. All factors with an eigenvalue equal to or greater than 1 were extracted, and items with a loading factor equal to or larger than 5 after rotation remained in the factor. The scree plots were also examined to identify the optimal number of factors to be extracted. For CFA, a range of fit indices, including Chi-square (χ2), root mean square error of approximation (RMSEA), the Tucker Lewis Index (TLI), the comparative fit index (CFI), and the standardized root mean square residual (SRMR) were used to assess model fit. An RMSEA less than 0.05 demonstrates good fit, between 0.05 and 0.08 acceptable fit, between 0.08 and 1.00 marginal fit, and greater than 1 poor fit.24 In addition, a good fit of data is also obtained when a CFI is close to 0.90, a TLI is close to 0.90, and an SRMR is close to 0.08.25–27 Chi-square statistic (χ2) has also been used as an index to assess model fit in factor analysis. As χ2 is sensitive to sample size with larger sample sizes increasing the power to reject the null hypothesis even though there may only be a trivial misfit.28 Therefore, the ratio χ2/df was used instead of χ2 to assess model fit, with a ratio less than 5 indicating an acceptable model fit.26 Based on the results of the EFA, a 4-factor model was tested.
To assess the performance of the SRQ-20 in detecting CMDs symptoms, the receiver operating characteristic (ROC) curve was plotted to compare the performance of the scale with the results of the clinical diagnosis. The area under the curve (AUC), a metric associated with the ROC, was assessed. This statistic reflects the probability that two cases, one from each group of the sample selected randomly, will both be correctly classified. An AUC value of 1 demonstrates 100% sensitivity and 100% specificity at all cut-off scores, while an AUC value of 0.5 indicates a test’s inability to discriminate between cases and non-cases. The accuracy of the test increases when the AUC value gets closer to 1. The optimum cut-off score of the SRQ-20 was determined based on the optimum combination of sensitivity and specificity (ie, when the balance between sensitivity and specificity is obtained) as well as on the proportion of the sample correctly classified by the SRQ-20 (scale efficiency) at that cut-off score.29
Results
Characteristics of the Study Sample
Table 1 presents some characteristics of the participants related to socio-demographic information, obstetric history, and mental health history. The mean age of the 210 pregnant women participating in the study was 28.9 (± 6.3) years. The participants’ age ranged from 18 to 49 years. Most of the participants (99.5%) were married. The percentage of pregnant women in trimesters 1, 2 and 3 was 25.2%, 40.5%, and 34.3%, respectively. Most participants reported high school education or above. Half of the study sample reported having finished high school, and 21.9% reported completing tertiary education. Most of the pregnant women (85.7%) had a job at the time of the interview. Median perceived social status, measured by asking the participants to rate their family’s social status (including economical, educational, and occupational status) based on a 10-rung ladder corresponding to scores from 1 to 10; the top rung indicates the highest social status, and the bottom rung indicates the lowest social status, was 5 (ranging from 1 to 10). Only 8.0% of the participants reported having a family history related to mental health problems, and 1.0% had been diagnosed with mental illness before the interview. About half of the women said that their pregnancy was planned. Nearly 20% reported having had pregnancy-related problems.
 |
Table 1 Characteristics of the Participants (n=210) |
Reliability
The Vietnamese version of the SRQ-20 had a Cronbach’s alpha of 0.87, which indicates good internal consistency.
Factorial Validity
Before factor analyses were conducted, the adequacy of factor analysis was assessed. The Kaiser-Meyers-Olkin (KMO) measure for sampling adequacy of the SRQ-20 was 0.81, much higher than the recommended value of 0.60,30 and Bartlett's test of sphericity of the scale was significant (p<0.5), demonstrating the suitability of the data for factor analysis.
Results of the EFA showed that four factors were retained, and these four factors explained 62.20% of the variance in the sample. The item loadings on each factor are presented in Table 2.
 |
Table 2 EFA Factor Loadings for the SRQ-20 |
All items of the SRQ-20 had a factor loading higher than 0.5; therefore, no item was excluded from the scale (Table 2). No cross-loading, where one item loads on two or more factors, was observed.
CFA was undertaken with a 4-factor model suggested by the EFA. Results of the CFA showed that all fit indices satisfied the recommended threshold for acceptable model fit with a CFI of 0.88, a TLI of 0.86, an RMSEA of 0.08, a SRMR of 0.07, and a χ2/df of 2.41. These results of CFA indicate that the data complied with the 4-factor structure suggested by the EFA results. With this factor structure, loadings of the items on the factors ranged from 0.58 to 0.89.
Performance of the SRQ-20 in Detecting CMDs (ROC Analysis)
As shown in Figure 1, the receiver operating characteristic (ROC) analysis resulted in an area under the curve (AUC) of 0.90. This indicates that the SRQ-20 is highly effective in detecting CMDs.
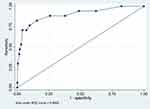 |
Figure 1 ROC curve of the SRQ-20. Abbreviations: ROC, receiver operating characteristic; AUC, area under the curve. |
It can be seen from Table 3 that the optimum cut-off score of the SRQ-20 is 5/6, where there is a balance between sensitivity and specificity. This means that pregnant women having an SRQ-20 score equal or greater than 6 can be classified as having symptoms suggestive of a CMD diagnosis. At this optimum cut-off score, the scale has a sensitivity of 82.35% and a specificity of 84.46%, and the proportion of the sample correctly classified is 84.29%. When using the SRQ-20 with a cut-off score of 5/6, the proportion of pregnant women identified as having symptoms suggestive of a CMD diagnosis was 20.95%. The prevalence of CMDs based on the ICD-10 clinical diagnosis was 8.09%.
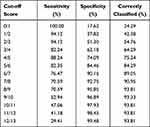 |
Table 3 Sensitivity, Specificity, and Proportion Correctly Classified at Different Cut-off Scores of the SRQ-20 |
Discussion
This study aimed to validate the Vietnamese version of the SRQ-20 in a community sample of pregnant women in rural Vietnam. We assessed the instrument’s reliability, factor structure, and performance in detecting CMDs among pregnant women.
Our study findings revealed that the SRQ-20 had good reliability, with a Cronbach’s alpha of 0.87. Good internal consistency of the SRQ-20 has also been widely reported in other countries in both primary care and community settings.31–33 Our study is the first to examine the factorial validity of the Vietnamese version of the SRQ-20. Results of EFA and CFA in our study suggest a 4-factor solution for the instrument, yielding four theoretically meaningful factors, which indicates that the SRQ-20 is a potential tool for screening for CMDs among Vietnamese pregnant women. From our point of view, the latent structure of the SRQ-20 is represented by the factors including “somatic symptoms” (items 1, 2, 3, 5, 7, 19), “anxiety and sadness” (items 4, 6, 9, 10), “lethargy” (items 8, 11, 12, 13, 18, 20), and “depressive thoughts” (items 14–17). Our factor structure of the Vietnamese version of SRQ-20 is very similar to the factor solution reported by Iacoponi and Mari for the Portuguese version of the SRQ-20 administered to people attending primary care in Sao Paulo city, Brazil.34 Data of this study resulted in four factors included Decreased Energy (items 8, 11, 12, 13, 18, 20), Somatic Symptoms (items 1, 2, 7, 19), Depressive Mood (items 6, 9, 10), and Depressive Thoughts (items 14–17).34 However, the factor structure of the SRQ-20 in our study differed from factor structures reported elsewhere. The number of factors of the SRQ-20 reported in the literature could range from 2 to 722,31,32,34,35 and we have not found any published study examining the factor structure of the SRQ-20 in pregnant women. The inconsistent findings of the factor structure of the SRQ-20 to date emphasize the need for further studies on the psychometric properties of the instrument in pregnant women. Researchers/practitioners using the Vietnamese version of the SRQ-20 at this stage may consider using the instrument as an overall scale instead of using the factors as separate subscales.
ROC curve analysis has been considered as one of the most common methods to examine the effectiveness of a test.36 In our study, the ROC analysis revealed that the Vietnamese SRQ-20 is highly effective in discriminating between cases and non-cases of CMDs among pregnant women, with an AUC statistic of 0.90. This is consistent with the results of studies using the SRQ-20 in a rural, antenatal population37 and with women in a primary care setting.15 One important purpose of this study is to identify the most appropriate cut-off score for case identification. The optimum cut-off score recommended in our study is 5/6, where there is a balance between maximum sensitivity and specificity. This criterion for identifying the optimum cut-off score has been the most widely used.38 At this cut-off score, the SRQ-20 presented both good sensitivity (82.35%) and specificity (84.46%). There is considerable variation in the optimum cut-off score of the SRQ-20 among studies.16,39–41 This may result from heterogeneity in the gold standard diagnosis instrument used, the study population (antenatal versus postnatal), the interested mental health problems (depression only versus common mental disorders), and the cultural setting. It has been argued that the expression of mental symptoms can be influenced by the culture and language of the respondent.42,43 Rahman et al discussed the translation and cultural adaptation of health questionnaires, using the SRQ-20 adaptation in the context of Pakistan as an example. They pointed out that in the local language, there were many words that could depict worry, tension and nervousness associated with anxiety and mood disorders, while no exact substitutes for some phrases such as “clear thinking” or “work suffering” could be identified. In addition, gender-based differences in the interpretation of certain items, as well as high level of sensitiveness of some issues such as “suicide” could make the respondents feel reluctant to provide their response.42 Therefore, cultural context can be an important factor affecting the performance of mental health measures. Our recommended cut-off score was higher than the cut-off score of 4/5 found in a study examining the performance of the SRQ-20 in detecting antenatal depression in Malawi.40 Although examining the performance of the SRQ-20 in a similar population (pregnant women), the fact that the Malawi study addressed different mental disorders (depression only), used DSM-IV major and major-or minor depressive episode as the gold standard diagnoses, determined with the Structured Clinical Interview for DSM-IV (SCID), and the different cultural context may explain this difference in the optimum cut-off score between the two studies.
In comparison with other studies with Vietnamese samples, our optimum threshold was equal to that recommended for detecting mental disorders in the adult population attending district hospitals but lower than the cut-off score of 6/7 recommended for screening for mental health problems in the general community population.17 This result is probably explained by the fact that pregnant women or people in health care settings are at higher risk of having psychological morbidity than the general population;44,45 therefore, the cut-off value in these groups should be lower than in the general population.38 The variation in the test characteristics of the SRQ-20 across different populations confirmed the need for studies examining different optimal cut-off scores to detect cases in different target groups, which has been previously mentioned by researchers.17,46
Our study has some limitations. The study was conducted with pregnant women from four rural communes in a northern province of Vietnam; therefore, the study sample may not represent all Vietnamese pregnant women. Consideration should be taken when generalizing the study findings to pregnant women in other communities, such as those in urban areas or less developed, mountainous areas in the country. In addition, formal inter-rater reliability of the SRQ-20 was not undertaken. To minimize inter-rater variation, a standard interview guide for the SRQ-20 was developed, and all interviewers were trained on interview techniques and ethical conduct of research before data collection. Moreover, literature has pointed out that mental health symptoms can vary through different gestational periods and can be affected by a range of factors including history of mental health problems, unplanned pregnancy, multiparity, and family relationship.47,48 It might be worthwhile to examine whether the SRQ-20 scores vary among different groups of pregnant women (ie, being at different gestational periods or having planned versus having unplanned pregnancy, etc). However, due to resource constraint, we did not obtain a large enough sample size of pregnant women that allows adequate power to detect differences in mental health status of pregnant women with various characteristics known to be more sensitive to mental health problems. Larger-scale studies may be needed to investigate further into the validity of the Vietnamese version of the SRQ-20 by assessing the instrument’s performance in different groups of pregnant women.
Limitations notwithstanding, the study’s findings suggest the potential for using the SRQ-20 as a screening tool for CMDs among pregnant women in Vietnam. Given that the instrument is reliable, valid, brief (completed within 5 minutes), simple, easy to administer, and that 97% of pregnant women in Vietnam attend antenatal care services,49 the instrument might be of potential use in antenatal care services as a means to detect CMDs among pregnant women. This is crucial in a resource-limited country like Vietnam, where antenatal mental illnesses have not been adequately detected and treated,12 and where there is no current formal screening program for CMDs in perinatal care settings. The appropriateness of using the SRQ-20 in an antenatal care setting in low-resource countries has also been previously reported.40 This recommendation is in line with global initiatives, including the World Health Organization Mental Health Gap Action Program,50 The Grand Challenges in Global Mental Health,51 and the United Nations Sustainable Goal52 that support prioritization of routine CMD detection within primary care and community care settings.41,51
Conclusion
Our study provides evidence of the validity and reliability of the Vietnamese version of the SRQ-20. Although the SRQ-20 cannot be a substitute for a clinical diagnostic examination, this instrument can effectively detect CMDs among pregnant women. It is recommended as a screening tool for CMDs in antenatal care settings in Vietnam.
Data Sharing Statement
The raw data supporting the conclusions of this manuscript will be made available by the authors, without undue reservation, to any qualified researcher.
Ethics Approval and Informed Consent
All procedures performed in the study involving human participants comply with the Declaration of Helsinki and were in accordance with the ethical standards of the Ethical Review Board for Biomedical Research at Hanoi University of Public Health (Ethics approval decision number 33/2022/YTCC-HD3, dated 7 February 2022). Written informed consent was obtained from all participants. All information on the original dataset was collected confidentially.
Acknowledgment
The authors would like to thank staff from Bac Giang Center for Disease Prevention and Control and Hiep Hoa District Health Center for their assistance in organizing data collection. In addition, the authors are grateful to all research participants who contributed their time and efforts to this project.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The work received funding from the Joint MRC/ESRC/DFID/Wellcome Health Systems Research Initiative (grant ref: MR/T023481/1). The views are of the authors only and do not necessarily represent those of the funders.
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Fisher J, Cabral de Mello M, Patel V, et al. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bull World Health Organ. 2012;90(2):139g–149g. doi:10.2471/BLT.11.091850
2. Stocker R, Nguyen T, Tran T, et al. Social and economic development and pregnancy mental health: secondary analyses of data from rural Vietnam. BMC Public Health. 2020;20(1):1001. doi:10.1186/s12889-020-09067-9
3. Wachs TD, Black MM, Engle PL. Maternal depression: a global threat to children’s health, development, and behavior and to human rights. Child Dev Perspect. 2009;3(1):51–59. doi:10.1111/j.1750-8606.2008.00077.x
4. van der Ham L, Wright P, Van TV, Doan VDK, Broerse JEW. Perceptions of mental health and help-seeking behavior in an urban community in Vietnam: an explorative study. Community Ment Health J. 2011;47(5):574–582. doi:10.1007/s10597-011-9393-x
5. Bao Giang K, Viet Dzung T, Kullgren G, Allebeck P. Prevalence of mental distress and use of health services in a rural district in Vietnam. Glob Health Action. 2010;3(1):2025. doi:10.3402/gha.v3i0.2025
6. Fisher JRW, Morrow MM, Nhu Ngoc NT, Hoang Anh LT. Prevalence, nature, severity and correlates of postpartum depressive symptoms in Vietnam. BJOG. 2004;111(12):1353–1360. doi:10.1111/j.1471-0528.2004.00394.x
7. Fisher J, Tran TD, Biggs B, Dang TH, Nguyen TT, Tran T. Intimate partner violence and perinatal common mental disorders among women in rural Vietnam. Int Health. 2013;5(1):29–37. doi:10.1093/inthealth/ihs012
8. Nhị TT, Hạnh NTT, Gammeltoft TM. Emotional violence and maternal mental health: a qualitative study among women in northern Vietnam. BMC Womens Health. 2018;18(1):58. doi:10.1186/s12905-018-0553-9
9. Van Ngo T, Gammeltoft T, Nguyen HTT, Meyrowitsch DW, Rasch V. Antenatal depressive symptoms and adverse birth outcomes in Hanoi, Vietnam. PLoS One. 2018;13(11):e0206650. doi:10.1371/journal.pone.0206650
10. Hoang TN, Van TN, Gammeltoft T, Meyrowitsch D, Nguyen Thi Thuy H, Rasch V. Association between Intimate partner violence during pregnancy and adverse pregnancy outcomes in Vietnam: a prospective cohort Study. PLoS One. 2016;11(9):e0162844. doi:10.1371/journal.pone.0162844
11. Vung ND, Ostergren P-O, Krantz G. Intimate partner violence against women, health effects and health care seeking in rural Vietnam. Eur J Public Health. 2009;19(2):178–182. doi:10.1093/eurpub/ckn136
12. Hue MT, Nguyet Van NH, Nha PP, et al. Factors associated with antenatal depression among pregnant women in Vietnam: a multisite cross-sectional survey. Health Psychol Open. 2020;7(1):2055102920914076. doi:10.1177/2055102920914076
13. Niemi M, Thanh HT, Tuan T, Falkenberg T. Mental health priorities in Vietnam: a mixed-methods analysis. BMC Health Serv Res. 2010;10(1):257. doi:10.1186/1472-6963-10-257
14. Beusenberg M, Orley JH; World Health Organization. Division of Mental H. A User’s Guide to the Self Reporting Questionnaire (SRQ / Compiled by M. Beusenberg and J. Orley. Geneva: World Health Organization; 1994.
15. Netsereab TB, Kifle MM, Tesfagiorgis RB, Habteab SG, Weldeabzgi YK, Tesfamariam OZ. Validation of the WHO self-reporting questionnaire-20 (SRQ-20) item in primary health care settings in Eritrea. Int J Ment Health Syst. 2018;12(1):61. doi:10.1186/s13033-018-0242-y
16. van der Westhuizen C, Wyatt G, Williams JK, Stein DJ, Sorsdahl K. Validation of the self reporting questionnaire 20-item (SRQ-20) for use in a low- and middle-income country emergency centre setting. Int J Ment Health Addict. 2016;14(1):37–48. doi:10.1007/s11469-015-9566-x
17. Giang KB, Allebeck P, Kullgren G, Tuan NV. The Vietnamese version of the self reporting questionnaire 20 (SRQ-20) in detecting mental disorders in rural Vietnam: a validation study. Int J Soc Psychiatry. 2006;52(2):175–184. doi:10.1177/0020764006061251
18. Nguyen PH, Saha KK, Ali D, et al. Maternal mental health is associated with child undernutrition and illness in Bangladesh, Vietnam and Ethiopia. Public Health Nutr. 2014;17(6):1318–1327. doi:10.1017/S1368980013001043
19. Hiep Hoa Distrct People’s Committee. Geographic and demographic characteristics. Hiep Hoa District People’s Committee; 2022. Available from: https://hiephoa.bacgiang.gov.vn/chi-tiet-tin-tuc/-/asset_publisher/gFj0vhwEUNmh/content/-ieu-kien-tu-nhien-cua-huyen-hiep-hoa.
20. Mundfrom DJ, Shaw DG, Ke TL. Minimum sample size recommendations for conducting factor analyses. Int J Test. 2005;5(2):159–168. doi:10.1207/s15327574ijt0502_4
21. Arrindell WA, van der Ende J. An empirical test of the utility of the observations-to-variables ratio in factor and components analysis. Appl Psychol Meas. 1985;9:165–178. doi:10.1177/014662168500900205
22. World Health Organization. A User’s Guide to the Self Reporting Questionnaire (SRQ). Geneva: World Health Organization; 1994.
23. Coaley K. An Introduction to Psychological Assessment and Psychometrics. Los Angeles: SAGE; 2009.
24. Fabrigar LR, Wegener DT, MacCallum RC, Strahan EJ. Evaluating the use of exploratory factor analysis in psychological research. Psychol Methods. 1999;4(3):272–299. doi:10.1037/1082-989X.4.3.272
25. Hu L, Bentler PM. Cut-off criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model. 1999;6:1–55. doi:10.1080/10705519909540118
26. Li J, Yuan L, Wu Y, Luan Y, Hao Y. The Chinese version of the Pediatric Quality Of Life Inventory™ (PedsQL™) healthcare satisfaction generic module (version 3.0): psychometric evaluation. Health Qual Life Outcomes. 2013;11(1):113. doi:10.1186/1477-7525-11-113
27. Hooper D, Coughlan J, Mullen M. Structural equation modelling: guidelines for determining model fit. Electron J Bus Res Methods. 2008;61(1):53–60.
28. Alavi M, Visentin DC, Thapa DK, Hunt GE, Watson R, Cleary M. Chi-square for model fit in confirmatory factor analysis. J Adv Nurs. 2020;76(9):2209–2211. doi:10.1111/jan.14399
29. Akobeng AK. Understanding diagnostic tests 3: receiver operating characteristic curves. Acta Paediatr. 2007;96(5):644–647. doi:10.1111/j.1651-2227.2006.00178.x
30. Cerny BA, Kaiser HF, Study A. Of A measure of sampling adequacy for factor-analytic correlation matrices. Multivariate Behav Res. 1977;12(1):43–47. doi:10.1207/s15327906mbr1201_3
31. Bell SA, Lori J, Redman R, Seng J. Psychometric validation and comparison of the self-reporting questionnaire-20 and self-reporting questionnaire-suicidal ideation and behavior among Congolese refugee women. J Nurs Meas. 2015;23(3):393–408. doi:10.1891/1061-3749.23.3.393
32. Scholte WF, Verduin F, van Lammeren A, Rutayisire T, Kamperman AM. Psychometric properties and longitudinal validation of the self-reporting questionnaire (SRQ-20) in a Rwandan community setting: a validation study. BMC Med Res Methodol. 2011;11(1):116. doi:10.1186/1471-2288-11-116
33. Chen S, Zhao G, Li L, Wang Y, Chiu H, Caine E. Psychometric properties of the Chinese version of the Self-Reporting Questionnaire 20 (SRQ-20) in community settings. Int J Soc Psychiatry. 2009;55(6):538–547. doi:10.1177/0020764008095116
34. Iacoponi E, de Jesus Mari J. Reliability and factor structure of the Portuguese version of self-reporting questionnaire. Int J Soci Psychiatry. 1989;35(3):213–222. doi:10.1177/002076408903500301
35. Rasmussen A, Ventevogel P, Sancilio A, Eggerman M, Panter-Brick C. Comparing the validity of the self reporting questionnaire and the Afghan symptom checklist: dysphoria, aggression, and gender in transcultural assessment of mental health. BMC Psychiatry. 2014;14:206. doi:10.1186/1471-244X-14-206
36. de Jesus Mari J, Williams P, Validity A. Study of a psychiatric screening questionnaire (SRQ-20) in primary care in the city of Sao Paulo. Br J Psychiatry. 1986;148(1):23–26. doi:10.1192/bjp.148.1.23
37. Stewart RC, Kauye F, Umar E, et al. Validation of a Chichewa version of the self-reporting questionnaire (SRQ) as a brief screening measure for maternal depressive disorder in Malawi, Africa. J Affect Disord. 2009;112(1–3):126–134. doi:10.1016/j.jad.2008.04.001
38. Habibzadeh F, Habibzadeh P, Yadollahie M. On determining the most appropriate test cut-off value: the case of tests with continuous results. Biochem Med. 2016;26(3):297–307. doi:10.11613/BM.2016.034
39. de Graaff AM, Cuijpers P, Leeflang M, et al. A systematic review and meta-analysis of diagnostic test accuracy studies of self-report screening instruments for common mental disorders in Arabic-speaking adults. Glob Ment Health. 2021;8:e43. doi:10.1017/gmh.2021.39
40. Stewart RC, Umar E, Tomenson B, Creed F. Validation of screening tools for antenatal depression in Malawi—A comparison of the Edinburgh postnatal depression scale and self reporting questionnaire. J Affect Disord. 2013;150(3):1041–1047. doi:10.1016/j.jad.2013.05.036
41. Larsen A, Pintye J, Bhat A, et al. Is there an optimal screening tool for identifying perinatal depression within clinical settings of sub-Saharan Africa? SSM Ment Health. 2021;1:100015. doi:10.1016/j.ssmmh.2021.100015
42. Rahman A, Iqbal Z, Waheed W, Hussain N. Translation and cultural adaptation of health questionnaires. J Pak Med Assoc. 2003;53(4):142–147.
43. Bhui K, Mohamud S, Warfa N, Craig TJ, Stansfeld SA. Cultural adaptation of mental health measures: improving the quality of clinical practice and research. BrJ Psychiatry. 2003;183(3):184–186. doi:10.1192/bjp.183.3.184
44. Arzamani N, Soraya S, Hadi F, Nooraeen S, Saeidi M. The COVID-19 pandemic and mental health in pregnant women: a review article. Front Psychiatry. 2022;13:949239. doi:10.3389/fpsyt.2022.949239
45. Ohrnberger J, Fichera E, Sutton M. The relationship between physical and mental health: a mediation analysis. Soc Sci Med. 2017;195:42–49. doi:10.1016/j.socscimed.2017.11.008
46. Matthey S. Is validating the cutoff score on perinatal mental health mood screening instruments, for women and men from different cultures or languages, really necessary? Int J Environ Res Public Health. 2022;19:7. doi:10.3390/ijerph19074011
47. Woldetsadik AM, Ayele AN, Roba AE, Haile GF, Mubashir K. Prevalence of common mental disorder and associated factors among pregnant women in South-East Ethiopia, 2017: a community based cross-sectional study. Reprod Health. 2019;16(1):173. doi:10.1186/s12978-019-0834-2
48. Truijens SEM, Spek V, van Son MJM, Guid Oei S, Pop VJM. Different patterns of depressive symptoms during pregnancy. Arch Womens Ment Health. 2017;20(4):539–546. doi:10.1007/s00737-017-0738-5
49. General Statistics Office of Viet Nam, United Nations Children’s Fund (UNICEF) Viet Nam Country Office. Survey Measuring Viet Nam Sustainable Development Goal Indicators on Children and Women 2020–2021. Hanoi: General Statistics Office of Viet Nam; 2021.
50. World Health Organization. mhGAP Intervention guide for mental, neurological, and substance use disorders in non-specialized health settings. World Health Organization; 2016. Available from: https://apps.who.int/iris/bitstream/handle/10665/250239/9789241549790-eng.pdf?sequence=1&isAllowed=y.
51. Collins PY, Patel V, Joestl SS, et al. Grand challenges in global mental health. Nature. 2011;475(7354):27–30. doi:10.1038/475027a
52. United Nations. Transforming our world: the 2030 agenda for sustainable development. United Nations; 2015. Available from: https://sustainabledevelopment.un.org/content/documents/21252030%20Agenda%20for%20Sustainable%20Development%20web.pdf.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
