Back to Journals » Clinical, Cosmetic and Investigational Dentistry » Volume 12
Using Cone-Beam Computed Tomography to Determine the Prevalence of the Second Mesiobuccal Canal in Maxillary First Molar Teeth in a Sample of an Iraqi Population
Authors Al-Saedi A , Al-Bakhakh B, AL-Taee RG
Received 9 September 2020
Accepted for publication 29 October 2020
Published 16 November 2020 Volume 2020:12 Pages 505—514
DOI https://doi.org/10.2147/CCIDE.S281159
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Christopher E. Okunseri
Aqeel Al-Saedi,1 Bahaa Al-Bakhakh,2 Riad G AL-Taee3
1Oral Diagnosis Department, College of Dentistry, University of Basrah, Basrah, Iraq; 2Conservative Dentistry Department, College of Dentistry, University of Basrah, Basrah, Iraq; 3Oral and Maxillofacial Surgery Department, College of Dentistry, University of Basrah, Basrah, Iraq
Correspondence: Aqeel Al-Saedi Oral Diagnosis
Department, College of Dentistry, University of Basrah Kut Al-Hujaj, Basrah 61004, Iraq
Tel +964 7706910561
Fax +964 7700636421
Email [email protected]
Purpose: This study aimed to determine the prevalence of the second mesiobuccal canal in maxillary first molar teeth in a sample of population from Basrah city in the south of Iraq.
Patients and Methods: Cone-beam computed tomography (CBCT) images of 353 Iraqi patients from Basrah city were included in the study. These images revealed 691 maxillary first molars, but only 655 of them were included. The images were obtained using a Gendex (GXDP-7000) CBCT machine (Hatfield, PA, USA) and studied for the prevalence of second mesiobuccal canal in the mesiobuccal root canal configuration, according to Vertucci’s classification, by scrolling through the images. Pearson’s chi-square tests were used to correlate canal type distribution to gender and age. The distributions of canal type on the right and left sides were assessed using the Kendal tau correlation coefficient. A P-value < 0.001 was considered highly significant. For intra-examiner reliability analysis, Cohen’s kappa test was used.
Results: The second mesiobuccal canal was identified in 81.68% of the Iraqi population sample. The most common type was type II (44.58%), followed by type IV (31.30%). Type I occurred in 18.32% of cases. Other types were less frequent.
Conclusion: The second mesiobuccal canal occurred in most of the examined samples of the Iraqi population (81.68%), with the most common type being type II, followed by type IV.
Keywords: maxillary molars, root canal anatomy, Vertucci’s classification, mesiobuccal root
Introduction
The maxillary first molar (MFM) boasts the largest tooth volume and a very complex root canal anatomy and is considered to be the most treated yet least understood posterior tooth.1
Technological advances have enabled the application of various techniques to investigate the dental anatomy. Many clinical studies have provided evidence that cone-beam computed tomography (CBCT) is a crucial tool when assessing the root canal anatomy, such as for the identification of the second mesiobuccal (MB2) canal in maxillary molars.2 CBCT produces undistorted three-dimensional images of the maxillofacial skeleton, including the teeth and the surrounding tissues, with a relatively lower effective radiation dose than that of computed tomography.3 CBCT is therefore considered a valuable tool for detecting MB2 canals and could be used in the endodontic treatment of MFMs.4,5
In recent years, many studies have assessed the prevalence of the MB2 canal, most of which used CBCT, as shown in Table 1.
 |
Table 1 Previous Studies on Evaluation of the Prevalence of MB2 Canals in Different Populations |
Some of these studies have investigated canal configuration in the mesiobuccal root specifically according to Vertucci’s classification. For example, the most common canal morphology in the mesiobuccal roots of MFMs in a Thai population was reported as type I (36.4%), followed by type II (28.8%) and type IV (25.3%).14 Meanwhile, Rouhani et al assessed the canal configuration in an Iranian population according to Vertucci’s classification and reported that the most common configuration was type I (46.4%), followed by types VI and II (17.6% and 14.4%, respectively).16 Alrahabi and Zafar, when assessing extracted teeth from a Saudi population, found that the most common canal configuration per Vertucci’s classification in mesiobuccal roots was type II, followed by type I.6 Finally, Khademi et al also investigated the morphology of MFMs in Iranian patients and reported that the most common type in their study was Vertucci type II (53.1%), followed by type I.10
Untreated root canals, because of failure to identify the canals, would become a reservoir for pathogenic bacteria, leading to the inhibition of healing or initiation of new inflammatory lesions in the periapical tissues.18
Most of the population in southern Iraq descends from an Arabic origin, while the population of northern Iraq has a Kurdish origin, which necessitates highlighting these racial variations when studying dental anatomy among Iraqi patients. On searching previous literature, no studies were found to investigate the anatomy of maxillary molars in the population of southern Iraq. Therefore, in the present study, we aimed to analyze CBCT images in a sample of southern Iraqi population from Basrah city for the prevalence of the MB2 canal in MFMs.
Materials and Methods
The present study was approved by the Ethical Review Committee at the College of Dentistry, University of Basrah (Protocol no. PRN/120/12/OD), and written informed consent was obtained from all participants to use their data. The present study complied with the principles of the Declaration of Helsinki. In this study, CBCT images of 353 patients (92 men and 212 women), with an average age of 30 years and an age range of 18 to 56 years, were evaluated. The included sample was classified into four age groups (18–26, 27–36, 37–46, and 47–56 years) to evaluate the relationship between age and distribution of canal types. These images were requested for multiple clinical purposes, including orthodontics, oral surgery, endodontics, and implants in the time period from November 15, 2018, to September 30, 2019.
From a total of 353 individuals, 691 MFMs were assessed; among them, 655 canal concerns were identified and distributed as 339 right and 316 left ones, respectively (36 MFMs were excluded). The study exclusion criteria were as follows: (1) a history of trauma to the maxillary arch, (2) presence of an MFM restoration and/or root canal filling, (3) an MFM with an open apex in one or more of its roots, (4) a history of surgery in the posterior maxilla, (5) the presence of any periapical pathology and/or resorption that could complicate image interpretation, (6) the presence of a calcified canal and/or pulp stones, (7) an MFM with developmental anomalies that could interfere with the interpretation of CBCT images, and (8) collection of images with artifacts or technique errors affecting interpretation.
The examiners looked for the presence or absence of an MB2 canal by scrolling along the axial and coronal sections. If an MB2 canal was present, it was classified according to Vertucci’s classification (Figure 1).19
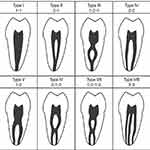 |
Figure 1 Diagrammatic representations of Vertucci’s classification for root canal morphology. |
Radiographic Technique
CBCT images were obtained using a Gendex (GXDP-7000) CBCT machine (Hatfield, PA, USA) operating at 90 kV and 10 mA with an exposure time of 13 s. The image dimensions used were 400 × 400 × 300 pixels IJK and the image resolution was 200 × 200 × 200 µm, while the image size (field of view) was 80.0 × 80.0 × 60.0 mm. The minimum slice thickness was 0.25 mm, with a slice interval of 0.5 mm. The detector resolution was 200 µm. Scanning procedures were performed according to the manufacturer’s protocol. All CBCT examinations were carried out by an oral radiologist with more than 10 years of experience using the minimum exposure parameters necessary for acceptable image quality according to the “as low as reasonably achievable” radiation protocol.
Evaluation of the Images
All CBCT images were analyzed with a software program (GxPicture; Kavo Dental, Biberach an der Riss, Germany) built into the Invivo 5 dental viewer (Anatomage, San Jose, CA, USA) and run on a 64-bit Windows 7 system (Microsoft Corporation, Redmond, WA, USA). All images were analyzed using a 19-inch LCD screen (Dell, Round Rock, TX, USA) with a resolution of 1366 × 768 pixels in a dark room. The contrast and brightness of the images were adjusted during analysis using the software’s image processing tools to obtain the optimal visualization conditions. The examiners scrolled through the axial, coronal, and sagittal views. A professional oral radiologist, endodontist, and maxillofacial surgeon evaluated all CBCT images separately. The obtained data were compared, and any inconsistent data were rechecked and evaluated by the examiners at the same time so as to achieve consensus between their radiographic findings. One month after the first round of assessments, a second group of readings was performed, including approximately 20% of the images selected randomly to assess intra-examiner reliability using Cohen’s kappa test.
Statistical Analysis
Statistics were recorded for the type of root canal configuration observed and patients’ sex and age. The relationships between canal type, sex, and age were assessed using Pearson’s chi-square tests. P-values <0.05 were considered statistically significant, while P-values <0.001 were considered to be highly significant. The distributions of canal type on both sides (right and left) were assessed using the Kendal tau correlation coefficient. Intra-examiner reliability was analyzed using Cohen’s kappa test. The Statistical Package for the Social Sciences version 22.0 for Windows software program (IBM Corporation, Armonk, NY, USA) was used to conduct the statistical analyses.
Results
The intra-examiner reliability was found to be perfect (kappa test value = 0.9). This study involved a total of 353 individuals, including 212 (60.1%) women and 141 (39.9%) men, with an age range of 18 to 56 years and an average age of 30 years. As seen in Table 2, female study participants were typically younger than the male participants; however, this difference was not statistically significant (p > 0.05).
 |
Table 2 Age and Sex Distribution of the Sample |
While 691 MFMs were studied, only 655 canal issues were identified (ie, 36 MFMs were excluded according to the exclusion criteria), divided as 339 right and 316 left teeth, respectively. Generally, type II was the most common canal type on both sides (44.58%), followed by type IV (31.30%). Type I seemed to occur to a similar degree on both the right and left sides (around 18%). Meanwhile, other types were less frequent (Figure 2). There was a fair correlation between the type of the canal on both right and left sides (Kendal tau correlation coefficient = 0.409), indicating that approximately 40% of the variability on one side can be explained by the variability on the other side (Table 3). Radiographic representation of different canal types is shown in Figure 3.
 |
Table 3 Types of Canals on Right and Left Sides |
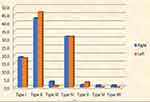 |
Figure 2 Graphical representation of canal types on the right and left sides. |
Types I, V, VI, and VII were found to appear more commonly in females, while type II was most prevalent in males. Type III and Type IV appeared more commonly on the right side in females, but they were seen in more ratios on the left side in males. As such, the distribution of right and left canals was significantly different between male and female patients (p < 0.05) (Table 4).
 |
Table 4 Distribution of Canal Type According to Gender |
The included sample was classified into four age groups (18–26, 27–36, 37–46, and 47–56 years) to evaluate the relationship between age and distribution of canal types. There was no statistically significant difference in the distribution of canal type according to age (p > 0.05) (Tables 5 and 6).
 |
Table 5 Distribution of Types of Canal on the RIGHT Side According to the Age Groups |
 |
Table 6 Distribution of Types of Canal on the LEFT Side According to the Age Groups |
Discussion
To achieve successful root canal therapy outcomes, dentists should have adequate knowledge of general dental anatomy and morphology of the root canal. Wide range of variations have been reported in both the shape and number of root canals in permanent teeth.
Because the root canal anatomy is related to genetics, similarities and variations in the root canal anatomy among populations could always be found. Variations in root canal configuration related to ethnicity have been reported in many studies. Therefore, evaluating the root canal anatomy of a certain population and comparing the results with those of other populations will help clinicians understand the population’s propensity in terms of root canal anatomy.8
Advancements in technology have made it possible to use techniques, such as CBCT, to investigate dental anatomy with greater precision and accuracy. Besides radiographic techniques, other methods have emerged for studying the root canal system, such as root canal sectioning, staining, and tooth-clearing techniques. Tooth-clearing techniques could be considered the gold standard for analyzing root canal morphology but can only be applied to extracted teeth (in vitro). The clinical methods used for analyzing the internal anatomy of teeth are radiographs, including conventional X-rays and tomograms. Research suggests that CBCT is superior to conventional radiographs.18 Meanwhile, Mirmohammadi et al concluded that CBCT sensitivity in detecting MB2 canal was 96%.21 Other research has reported findings of 89% sensitivity for CBCT versus 55% for periapical radiographs.22
In the present study, MB2 canals occurred in 81.68% of the population sample studied, showing a variety of types other than just type I (which constituted only 18.32% of cases). This finding supports the results of other researchers concerning the prevalence of MB2 canals. Coelho et al reported an overall prevalence rate of 75.91%,23 while Hiebert et al11 observed MB2 in 92% of their sample. Fernandes et al found MB2 prevalence rates of 92% and 87% on right and left sides, respectively, among a South African population,15 and Estrela et al reported the prevalence of MB2 in 76% of the evaluated Brazilian population.24 Meanwhile, in a worldwide study using CBCT to assess the MB2 canal prevalence, the ratio ranged from 48.0% in Venezuela to 97.6% in Belgium, with an average rate of 73.8%.25 Zhang et al found MB2 canals in 85.4% of their study sample.12 Finally, in a sample of 149 MFMs studied by Naseri et al using CBCT, 86.6% showed the presence of MB2 canal,26 while a similar prevalence rate was observed in the study by Shetty et al (86.36%) in an Indian population.2
However, some studies have reported lower prevalence rates for MB2 canal, such as the study by Su et al (45.9%).27 Furthermore, a study conducted by Tanvi et al in an Indian population reported a prevalence rate of 55.7%,28 while Zand et al reported a prevalence rate of 55.1% in Iranian study subjects.29 Finally, 64.9% prevalence rate of MB2 canal was revealed in 330 MFMs of Saudi patients in a report by Al-Shehri et al.30 These differences in the MB2 canal prevalence rate could be related to variations in sample size, racial variations, and/or the methodology used.
The most common canal type in our study was type II (44.58%), with no significant difference between its frequency on the right and left sides, followed by type IV (31.3%) and type I (18.32%). Other types also occurred but in small percentages: types III and V occurred in 2.29% and type VI and VII occurred in 0.61% of the study population. Meanwhile, type VIII was not observed in any of the examined teeth. These findings are in agreement with those of a previous study conducted in Saudi patients, which reported that Vertucci’s type II was the most frequent type (47%), followed by type I (29.4%) and types III and IV (11.8% each); no other types were observed in this study.6 Additionally, according to a study by Ghobashi et al conducted in an Egyptian population, it was found that the most common canal type per Vertucci’s classification was type II (45.6%), followed by type IV (27.27%) and type I (25.45%).9 Among 389 MFMs evaluated by Khademi et al, in a sample of Iranian population, where MB2 appeared in 70.2% of the sample, the most common canal type was type II (53.1%), followed by type I (29.8%).10 Naseri et al also evaluated an Iranian population and reported that type VI was the most common canal type in their study population (35.6%), followed by type II (32.9%).26 These ratios are close to, although not coinciding with, the results of the present study; the differences could be related to racial differences between the evaluated samples. In addition, using different types of CBCT machines and/or different fields of view could be a cause for variation in visibility and interpretation of MB2.5
We found no significant difference in the distribution of canal types according to age. This concurs with the findings of several other studies; for example, Fernandes et al reported no significant relationship between sex and age and the prevalence of MB2 canal.15 Additionally, Mordanov et al conducted a study in Russian patients and stated that no significant correlation could be found between sex, age, and race and the prevalence of MB2 canal.31 Using an operating microscope, Das et al discerned no significant difference in the prevalence rate of MB2 canal according to age, sex, or side.32 Falcão et al also reported no significant differences in the existence of MB2 canal according to age and sex.33
Meanwhile, Martins et al found no significant difference in the prevalence rate of MB2 canal between the two sexes but reported that younger patients more frequently presented with MB2 canal.25 On the contrary, Zhang et al reported no statistically significant difference in the incidence of MB2 canal between the left and right sides, but they noted a significant association between both sex and age and the presence of MB2 canal.12 In addition, Lin et al conducted a study in a Taiwanese population and observed a decrease in MB2 canal detection with increasing age.8 Although the findings of the studies that suggest a decreased prevalence of MB2 canal with increasing age seem to be rational, using different CBCT machines, voxel sizes, fields of views, and software programs could justify the variation in findings, which could be the cause of decreased ratios reported alongside differences in the race of the studied samples.8
The variation reported between the results of different studies can also be attributed to ethnicity, study type (in vivo or in vitro), size of the sample, and the techniques used to identify canal morphology.16
In their study in Saudi patients, Alrahabi et al attributed the high frequency of occurrence of two or more canals in the mesiobuccal root to factors such as racial ethnicity, population, and configuration.6
Although root canal treatment remains the treatment of choice for most teeth, with a predictable success rate, the failure of treatment in maxillary molar teeth may be related to a lack of knowledge regarding the true existence of MB2 canals and difficulty in locating them. Unlocated and consequently untreated MB2 canals are a source of persistent microbial infection and contamination, leading to endodontic treatment failure and later appearance of apical periodontitis.15
In the present study, only medium field of view (80.0 × 60.0 mm) CBCT images were studied to ensure imaging of bilateral MFMs. Visualization of the MB2 canal could be enhanced using a smaller field of view. Comparison of the results of in vivo and ex vivo studies using different methods to identify the root canal anatomy can provide more accurate findings for the prevalence of MB2 in different populations, including Iraqi patients descending from different ethnicities. This can enhance the knowledge regarding the effect of racial differences on root canal configuration.
The findings of the present study might be of clinical value for Iraqi endodontists in their routine practice, especially when treating MFMs, by making them aware of the high probability of occurrence of MB2 among Iraqi patients, thus minimizing the occurrence of posttreatment failure related to untreated canals. This study can also be a starting point for establishing a research base for root canal configurations among southern Iraqi patients.
Conclusion
MB2 canal was present in a majority of the examined southern Iraqi population samples (81.68%), with the most commonly appearing types being, in the given order, type II, type IV, and type I; other types occurred more rarely.
Ethics Approval and Informed Consent
The present study was approved by the Ethical Review Committee at the College of Dentistry, University of Basrah (Protocol no. PRN/120/12/OD), and written informed consent was obtained from all participants to use their data.
Acknowledgment
The authors appreciate the help of Dr Guillermo Concha for permission to reproduce and reuse a figure downloaded by him.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This research received no external funding.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Estrela C, Nunes CA, Guedes OA, et al. Study of anatomical relationship between posterior teeth and maxillary sinus floor in a subpopulation of the Brazilian central region using cone-beam computed tomography-part 2. Braz Dent J. 2016;27(1):9–15. doi:10.1590/0103-6440201600679
2. Shetty H, Sontakke S, Karjodkar F, Gupta P, Mandwe A, Banga KS. A Cone Beam Computed Tomography (CBCT) evaluation of MB2 canals in endodontically treated permanent maxillary molars. A retrospective study in Indian population. J Clin Exp Dent. 2017;9(1):e51.
3. Patel S, Brown J, Pimentel T, Kelly RD, Abella F, Durack C. Cone beam computed tomography in endodontics–a review of the literature. Int Endod J. 2019;52(8):1138–1152.
4. Bello MDC, Tibúrcio-Machado C, Londero CD, Barletta FB, Moreira CHC, Pagliarin CML. Diagnostic efficacy of four methods for locating the second mesiobuccal canal in maxillary molars. Iran Endod J. 2018;13(2):204.
5. Studebaker B, Hollender L, Mancl L, Johnson JD, Paranjpe A. The incidence of second mesiobuccal canals located in maxillary molars with the aid of cone-beam computed tomography. J Endod. 2018;44(4):565–570. doi:10.1016/j.joen.2017.08.026
6. Alrahabi M, Zafar MS. Evaluation of root canal morphology of maxillary molars using cone beam computed tomography. Pak J of Med Sci. 2015;31(2):426. doi:10.12669/pjms.312.6753
7. Aktan AM, Yildirim C, Culha E, Demir E, Ciftci ME. Detection of second mesiobuccal canals in maxillary first molars using a new angle of cone beam computed tomography. Iran J Radiol. 2016;13(4). doi:10.5812/iranjradiol.31155
8. Lin YH, Lin HN, Chen CC, Chen MS. Evaluation of the root and canal systems of maxillary molars in Taiwanese patients: a cone beam computed tomography study. Biomed J. 2017;40(4):232–238. doi:10.1016/j.bj.2017.05.003
9. Ghobashy AM, Nagy MM, Bayoumi AA. Evaluation of root and canal morphology of maxillary permanent molars in an Egyptian population by cone-beam computed tomography. J Endod. 2017;43(7):1089–1092. doi:10.1016/j.joen.2017.02.014
10. Khademi A, Naser AZ, Bahreinian Z, Mehdizadeh M, Najarian M, Khazaei S. Root morphology and canal configuration of first and second maxillary molars in a selected Iranian population: a cone-beam computed tomography evaluation. Iran Endod J. 2017;12(3):288.
11. Hiebert BM, Abramovitch K, Rice D, Torabinejad M. Prevalence of second mesiobuccal canals in maxillary first molars detected using cone-beam computed tomography, direct occlusal access, and coronal plane grinding. J Endod. 2017;43(10):1711–1715. doi:10.1016/j.joen.2017.05.011
12. Zhang Y, Xu H, Wang D, et al. Assessment of the second mesiobuccal root canal in maxillary first molars: a cone-beam computed tomographic study. J Endod. 2017;43(12):1990–1996. doi:10.1016/j.joen.2017.06.021
13. Martins JN, Gu Y, Marques D, Francisco H, Caramês J. Differences on the root and root canal morphologies between Asian and white ethnic groups analyzed by cone-beam computed tomography. J Endod. 2018;44(7):1096–1104. doi:10.1016/j.joen.2018.04.001
14. Ratanajirasut R, Panichuttra A, Panmekiate S. A cone-beam computed tomographic study of root and canal morphology of maxillary first and second permanent molars in a Thai population. J Endod. 2018;44(1):56–61. doi:10.1016/j.joen.2017.08.020
15. Fernandes NA, Herbst D, Postma TC, Bunn BK. The prevalence of second canals in the mesiobuccal root of maxillary molars: a cone beam computed tomography study. Aust Endod J. 2019;45(1):46–50. doi:10.1111/aej.12263
16. Rouhani A, Bagherpour A, Akbari M, Azizi M, Nejat A, Naghavi N. Cone-beam computed tomography evaluation of maxillary first and second molars in Iranian population: a morphological study. Iran Endod J. 2014;9(3):190.
17. Tzeng LT, Chang MC, Chang SH, Huang CC, Chen YJ, Jeng JH. Analysis of root canal system of maxillary first and second molars and their correlations by cone beam computed tomography. J Formos Med Assoc. 2020;119(5):968–973. doi:10.1016/j.jfma.2019.09.012
18. Olczak K, Pawlicka H. The morphology of maxillary first and second molars analyzed by cone-beam computed tomography in a polish population. BMC Med Imaging. 2017;17(1):68. doi:10.1186/s12880-017-0243-3
19. Vertucci FJ. Root canal anatomy of the human permanent teeth. oral surgery. Oral Med Oral Pathol Oral Radiol. 1984;58(5):589–599. doi:10.1016/0030-4220(84)90085-9
20. Torres A, Jacobs R, Lambrechts P, et al. Characterization of mandibular molar root and canal morphology using cone beam computed tomography and its variability in Belgian and Chilean population samples. Imaging Sci Dent. 2015;45(2):95–101. doi:10.5624/isd.2015.45.2.95
21. Mirmohammadi H, Mahdi L, Partovi P, Khademi A, Shemesh H, Hassan B. Accuracy of cone-beam computed tomography in the detection of a second mesiobuccal root canal in endodontically treated teeth: an ex vivo study. J Endod. 2015;41(10):1678–1681. doi:10.1016/j.joen.2015.06.011
22. Sousa TO, Haiter-Neto F, Nascimento EHL, Peroni LV, Freitas DQ, Hassan B. Diagnostic accuracy of periapical radiography and cone-beam computed tomography in identifying root canal configuration of human premolars. J Endod. 2017;43(7):1176–1179. doi:10.1016/j.joen.2017.02.021
23. Coelho MS, Parker JM, Tawil PZ. Second mesiobuccal canal treatment in a predoctoral dental clinic: a retrospective clinical study. J Dent Educ. 2016;80(6):726–730. doi:10.1002/j.0022-0337.2016.80.6.tb06135.x
24. Estrela C, Bueno MR, Couto GS, et al. Study of root canal anatomy in human permanent teeth in a subpopulation of Brazil’s center region using cone-beam computed tomography-part 1. Braz Dent J. 2015;26(5):530–536. doi:10.1590/0103-6440201302448
25. Martins JN, Alkhawas MBA, Altaki Z, et al. Worldwide analyses of maxillary first molar second mesiobuccal prevalence: a multicenter cone-beam computed tomographic study. J Endod. 2018;44(11):1641–1649. doi:10.1016/j.joen.2018.07.027
26. Naseri M, Safi Y, Baghban AA, Khayat A, Eftekhar L. Survey of anatomy and root canal morphology of maxillary first molars regarding age and gender in an Iranian population using cone-beam computed tomography. Iran Endod J. 2016;11(4):298.
27. Su CC, Huang RY, Wu YC, et al. Detection and location of second mesiobuccal canal in permanent maxillary teeth: a cone-beam computed tomography analysis in a Taiwanese population. Arch Oral Biol. 2019;98:108–114. doi:10.1016/j.archoralbio.2018.11.006
28. Tanvi M, Vimala N, Lalitagauri M. Evaluation of the root morphology of maxillary permanent first and second molars in an Indian subpopulation using cone beam computed tomography. J Dent Med Sci. 2016;15:51–56.
29. Zand V, Mokhtari H, Zonouzi HR, Shojaei SN. Root canal morphologies of mesiobuccal roots of maxillary molars using cone beam computed tomography and periapical radiographic techniques in an Iranian population. J Contemp Dent Pract. 2017;18(9):745–749. doi:10.5005/jp-journals-10024-2119
30. Al-Shehri S, Al-Nazhan S, Shoukry S, Al-Shwaimi E, Al-Shemmery B. Root and canal configuration of the maxillary first molar in a Saudi subpopulation: a cone-beam computed tomography study. Saudi Endod J. 2017;7(2):69.
31. Mordanov O, Khabadze Z, Daurova F, et al. Second mesiobuccal canal evaluation features with cone-beam computed tomography. Int J Dent. 2019;2019:1–4. doi:10.1155/2019/5856405
32. Das S, Warhadpande MM, Redij SA, Jibhkate NG, Sabir H. Frequency of second mesiobuccal canal in permanent maxillary first molars using the operating microscope and selective dentin removal: a clinical study. Contemp Clin Dent. 2015;6(1):74. doi:10.4103/0976-237X.149296
33. Falcão CA, Albuquerque VC, Amorim NL, et al. Frequency of the mesiopalatal canal in upper first permanent molars viewed through computed tomography. Acta Odontol Latinoam. 2016;29(1):54–59.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

