Back to Journals » Journal of Multidisciplinary Healthcare » Volume 12
Use and preferences of information and communication technologies in patients with hypertension: a cross-sectional study in Ecuador
Authors Chérrez-Ojeda I , Vanegas E , Felix M , Mata VL, Gavilanes AWD, Chedraui P
Received 15 March 2019
Accepted for publication 4 July 2019
Published 24 July 2019 Volume 2019:12 Pages 583—590
DOI https://doi.org/10.2147/JMDH.S208861
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ivan Chérrez-Ojeda,1,2 Emanuel Vanegas,1,2 Miguel Felix,1,2 Valeria L Mata,1,2 Antonio WD Gavilanes,3,4 Peter Chedraui5,6
1Universidad Espíritu Santo, Samborondón, Ecuador; 2Respiralab Research Group, Guayaquil, Ecuador; 3Department of Pediatrics, Maastricht University Medical Center, Maastricht, the Netherlands; 4School of Oncology and Developmental Biology, Maastricht University, Maastricht, the Netherlands; 5Instituto De Investigación E Innovación En Salud Integral, Facultad De Ciencias Médicas, Universidad Católica De Santiago De Guayaquil, Guayaquil, Ecuador; 6Facultad De Ciencias De La Salud, Universidad Católica “Nuestra Señora De La Asunción”, Asunción, Paraguay
Objectives: This study was designed to assess the use and preferences for information and communication technologies (ICTs) among patients with hypertension in Ecuador.
Methods: We conducted an anonymous cross-sectional study during 2018, in which 207 patients with hypertension were surveyed using an adapted version of the Michigan questionnaire. The survey included 16 questions in total, in which patients were asked to quantify their use for each ICT, and their interest in using ICTs to receive information and communicate with health care providers. Adjusted binomial and multinomial regression analyses were performed.
Results: Of the surveyed population, 74.9% of patients reported owning a smartphone, while 79.2% of responders reported having access to the internet. In general, web-based internet (53.7%) remains the main source for obtaining information related to hypertension, followed by YouTube (39.5%) and Facebook (30.2%). WhatsApp and Facebook were rated with the highest interest for receiving and asking health-related information. Older age and lower educational levels were consistently associated with less interest and usage for most ICTs.
Conclusions: The widespread use of ICTs opens new possibilities for improving the care of patients with hypertension through self-management education strategies. Further studies should be conducted to demonstrate how to develop and promote interventions through ICTs more effectively, based on the studied patterns of use and preferences of ICTs for specific patients.
Keywords: information and communication technology, social media, hypertension, self-management, Latin America
Introduction
Hypertension is a chronic nontransmissible disease characterized by sustained systolic and/or diastolic blood pressure.1 In Latin America, it is responsible for 13% of deaths and 5.1% of disability-adjusted life years, representing the most important cardiovascular risk factor regarding the overall disease burden.2,3 Although numerous treatment strategies are often available, it is estimated that only a third of patients in Latin America have their blood pressure controlled.4 In Ecuador, hypertension-related complications are considered the second most common cause of death nationwide, with an estimated prevalence of 9.3% according to data provided by the National Health and Nutrition Examination Survey.5 Furthermore, the same study found that most Ecuadorians with blood pressure in the prehypertensive range have no knowledge about the risks related to hypertension, and roughly half of hypertensive patients had poor adherence to treatment.
Self-management education strategies through digital health interventions offer an opportunity to address this increasing health burden in a widespread and potentially cost-effective way.6 For example, a recent systematic review on the effectiveness, usability and user satisfaction of mobile apps to support self-management of hypertension concluded that mobile apps might be effective in lowering blood pressure and are accepted by most users.7 The use of technology can also aid to lessen the barriers associated with cultural diversity and decision-making, by simplifying global communications, thus facilitating self-management education programs.8 Still, there is a need for additional studies addressing security measures, effectiveness, usability, and the theoretical basis for implementation of mobile applications in the health care setting.9
ICTs, defined as technologies that use computing and mobile-type devices for communication and information purposes (eg, email, social media, text messaging, etc.) can provide a platform for the development and implementation of self-management programs.10 For example, participation in support groups and consulting with health professionals through ICTs assist patients in self-monitoring and decision-making.11 There is evidence that by using ICTs in developing countries, it is possible to reach large numbers of people to promote physical activity and healthy diets.12 Furthermore, there is a high proliferation and adoption of mobile technologies, with estimates suggesting that two-thirds of global internet users are based in developing countries.13,14 The end result is a unique scenario for the potential development and implementation of self-management programs designed to improved health-related outcomes in patients with hypertension through ICTs, particularly in developing countries. As such, we designed this study to fill the knowledge gap, by identifying the frequency, preferences, and interest in using ICTs among Ecuadorian patients with hypertension.
Methods
Ethical considerations
This study was approved by the Ethics Committee “Comité de Ética e Investigación en Seres Humanos” (CEISH). Every participant signed an informed consent before the beginning of the survey. The identity and data obtained from each of the patients were guaranteed not to be revealed.
Study design
We conducted an anonymous cross-sectional study which was carried out between the months of January and June in 2018, in which 207 Ecuadorian patients diagnosed with arterial hypertension were surveyed, where each of them rated themselves through questions assessing the frequency and preferences of use of ICTs. Participants were recruited in cardiology or internal medicine outpatient clinical centers and their background varied to include individuals coming from urban/inner city, suburban and rural areas. Patient demographics, such as gender, educational level, ethnicity, as well as patterns and preferences of use of ICTs were reported. To be included, patients from either public or private medical practice had to be diagnosed with hypertension and be at least 18 years old or more. Patients who had psychiatric diseases, had any form of language impairment or who found it difficult to visualize the survey were excluded.
Sample size
Sample size was calculated according to the most demanding analysis in this study. We used G*Power Version 3.0.10 (Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany) to calculate the sample size for goodness-of-fit tests, setting an effect size (w) of 0.3, α error probability of 0.05, a power of 0.08 and 2 degrees of freedom. With such parameters, the calculated sample size was 108, which was further expanded to 162 to overcome Type II errors as much as possible.
Procedures
To assess the patterns and preferences of use of ICTs, a Spanish version of the Michigan questionnaire was used, which was adapted for hypertension.15 Each patient was previously informed with the purpose of our study and then given the questionnaire, which they could fill by themselves or with the help of a previously trained person (eg, physician, nurse or intern).
Questionnaire
The survey included 16 questions in total and took roughly 8 mins to complete. The first 7 questions addressed general demographic and clinical information, as well as access to ICTs. If patients accomplished the clause of owning a cellphone and having access to internet, they could proceed to answer the rest of the questionnaire.
In the following section, patients were asked to quantify their use of each ICT (text messaging, Facebook, Twitter, LinkedIn, email, web browsers, WhatsApp, YouTube, Instagram, Skype and Blogs) under a scale assessing frequency (daily, at least once a week, at least once a month, less than once a month, never). Furthermore, patients were asked if they used such ICTs to obtain information about their disease in a dichotomic fashion (yes/no). Then, patients rated their interest level to receive information and ask health care providers about their disease through these ICTs under a designated scale (extremely, very, moderately and mildly interested and not interested).
Free text entries were solicited to determine how and why ICTs would be helpful as methods to approach patients with hypertension, or the reasons why they might not be interested in using such technologies for health-related purposes.
Statistical analysis
Of the surveyed population (n=207), 89.9% reported they owned a cellphone, of which 74.9% were smartphones, while only 79.2% responders reported having access to the internet. Based on the ICT access (owning a cellphone and having access to the internet), 45 patients could not complete the survey, whilst the remaining 162 patients that filled the whole questionnaire were part of the sample subject of statistical analysis.
For each ICT type, responses assessing the frequency of use were categorized into “high frequency” (daily and at least once a week), “low frequency” (at least once a month and less than once a month) and “never.” Age, gender, educational level and years since hypertension diagnosis were used as independent variables on each analysis. Whilst age and years since hypertension diagnosis were used as continuous variables, educational level was dichotomized into none or pretertiary and university/postgraduate. Gender was either male or female.
We performed binomial regression analyses between such independent variables and the use of each ICT to obtain information about hypertension. We further undertook multinomial regression analyses between the selected independent variables and the degree of interest (categorized into “very-extremely interested,” “mildly-moderately interested” and “not interested”) in receiving information or asking physicians about the disease through each technology. Analyses were adjusted for age, gender, educational level and years since diagnosis. For binomial analyses, the reference categories for gender and educational level were male and no education/pretertiary education, respectively. On the other hand, for multinomial analyses, the reference categories for gender and educational level were female and university/postgraduate, respectively.
All the data were analyzed using SPSS, version 24.0 software (SPSS Inc., Chicago, IL, USA). A p-value of less than 0.05 was considered statistically significant.
Results
Demographics, ICT access and frequency of use
From the 207 surveyed participants, 89.9% reported they owned a cellphone, of which 74.9% were smartphones. 79.2% responders reported having access to the internet.
For the purpose of the statistical analyses, 162 patients were selected, with a gender distribution of 58.6% females and 41.4% males. Most patients had secondary education level (35.2%), followed closely by university studies (34.6%). Most of the patients were Hispanic/Mestizo (90.7%). The mean age was 57.1 years, with an average of 8.4 years with hypertension (Table 1).
 |
Table 1 General characteristics of the surveyed population (n=162) |
Concerning frequency of use, WhatsApp (94.4%), followed by Facebook (77.8%) and YouTube (59.3%) were reported as the most used ICTs (Figure 1).
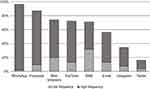 |
Figure 1 Frequency of use of information and communication technologies in patients with hypertension.Abbreviation: SMS, short message service. |
Use of ICTs to obtain information about hypertension
In general, web browsers (53.7%) were reported as the most used ICT to obtain information about hypertension, followed by YouTube (39.5%) and Facebook (30.2%) (Figure 2). Whilst a higher educational level was associated with a greater likelihood of using email (OR, 21.6), web browsers (OR, 3.05) and Facebook (OR, 2.26) to obtain information when compared to patients with pre-tertiary or no education, increasing age was associated with lesser odds of using email (OR, 0.94), web browsers (OR, 0.94) and YouTube (OR, 0.96) for such purposes (Tables S1 and S2).
 |
Figure 2 Use of ICTs to obtain information related to hypertension and interest in receiving health-related information and communicating with health care providers through ICTs. |
Interest in receiving and asking information related to hypertension through ICTs
Overall, WhatsApp was the single best rated ICT of interest to both receive information (68.5%) and ask physicians (75.9%) about hypertension, followed by Facebook (51.9% and 41.4%, respectively) (Figure 2).
Individuals with pretertiary or no education were more likely to be very/extremely interested in receiving information about hypertension through SMS (OR, 5.03) and WhatsApp (OR, 5.78) (Table 2), as well as asking physicians about their disease through SMS (OR, 2.67) and Facebook (OR, 2.90) (Table 3) when compared to patients with higher education (Table S3). However, they were also less likely to be mildly/moderately interested in receiving information about the disease through email (OR, 0.19) than those with higher education.
 |
Table 2 Interest in receiving information related to hypertension through ICTs |
 |
Table 3 Interest in asking health-related information through ICTs |
Increasing age was associated with less likelihood of being interested in asking and receiving information through email and web browsers. On the other hand, increasing years with disease and being male were factors associated with higher odds of being mildly/moderately interested in receiving information (OR, 1.09) and asking physicians (OR, 4.93) about hypertension through email, respectively (Table S4).
Discussion
ICTs can offer several benefits for patients. For instance, it can create networks with peers to share common experiences, increase problem-solving skills, and increase confidence in making life-improving changes.16 Thus, ICTs might serve as a potential platform for improving the care of patients with hypertension.
In our study, approximately 80% of patients with hypertension had internet access, while a slightly similar percentage reported owning a smartphone. Web-based internet was rated as the main source for obtaining information related to hypertension in approximately half of the patients. Still, there is a considerable proportion of patients that could miss potential intervention through ICTs. Recent data suggest that the use of ICTs, particularly the Internet, is proportional to the educational level of the individual. The higher the level of education, the higher the use rate of ICTs.17 In comparison to our study, in which not only educational level but also age appear to influence the use and interest for ICTs, older age and lower educational levels were consistently associated with less use of most ICTs, as well as less interest for receiving and asking health-related question through them.
Discussing specific ICTs, the instant messaging application WhatsApp was rated both as the most commonly used, as well as the platform with the highest interest for both receiving and asking health-related information. Not only text could be exchanged through this instant messaging platform, also images, videos and audio messages are available for no cost. Interestingly, usage of WhatsApp was found to be approximately two-thirds of all internet users in Latin America, in contrast to a lesser frequency among North Americans.18 Our results suggest that approximately two-thirds of our patients were highly interested in receiving information about hypertension and communicating with physicians using WhatsApp. This ICT could be particularly appropriate for patients with lower educational levels since they were approximately six times more likely to be highly interested in using this ICT for receiving health care-related information than responders with secondary or higher education. In some countries of Latin America, mobile phone operators are offering various mobile plans that usually include unlimited data for exclusive usage of WhatsApp and Facebook services. For this reason, WhatsApp presents higher penetration rates in many countries of Latin America when compared to other regions.18
With regard to the use of Facebook in Latin America, one study found that Argentina has the greatest user platform (32.14%), while Peru has the smallest (16%).19 However, we found in our Ecuadorian sample that 77.8% of responders were frequent Facebook users. Additionally, this ICT was rated second both regarding the general frequency of use and overall interest for communicating with health care providers and receiving relevant health-related information using this platform. While some patients may share their experiences with certain diseases, others spread messages of hope and many learn recent data from studies published, all thanks to the creation of support groups on Facebook. This may be one of the reasons why many patients were interested in this particular ICT.
In previous literature exploring the benefits that social media provides for chronic diseases among different studies, it was found that 45% of individuals identified a positive impact with regard to support (via blogs) and disease modification (via Facebook).20 However, a recent publication found that the number of English hypertension-related Facebook groups and their users was minor compared to the whole Facebook community, and the groups’ activity levels were low.21 There is limited information about the scientific accuracy of the information posted on Facebook group walls of Latin-American hypertension patients, but this could be advantageous if it leads to the development of strategies to provide sources of medical information supported by expert medical teams. Thus, Facebook groups might be useful to promote hypertension awareness in an assay of patients.
Moreover, our results suggest that YouTube was the second most commonly used ICT (39.5%) to obtain information about hypertension. This ICT may represent a viable channel for translating and disseminating hypertension-related patient education on topics such as medication management. However, many low-quality videos are posted on YouTube and many of them advocate unproven alternative treatments for hypertension, a condition that could affect patient safety.22 Health professionals have the responsibility to ensure the quality of information and that available comments are reliable. Thus, whenever a physician encourages patient education and recommends the patient to look online for hypertension-related information, it is necessary to ascertain which ICTs patients prefer and which of them represents a reliable source of data.20,21
There is a significant difference in the utilization of various forms of health information technology tools between rural and urban communities.23 There are research projects in Latin America focused to determine which technologies are appropriate to provide the best communication.24 The results provided by our study have potential implications for designing future interventions through ICTs, especially in low- and middle-income countries, since it is known that many patients suffering from chronic diseases, and living in rural or hard-to-reach areas usually present with poor control of their disease. The development of strategies and interventions has the additional advantage of having the potential to be highly personalized, based on the individual participant’s data, and engaging with interactive tools and graphically rich content. The appropriate use of ICTs in developing countries can bring notable benefits and improvements to current practice, such as support from health-care professionals and promotion of physical activity and healthy diets.12 However, more emphasis on process and methodology is necessary to determine which ICTs could be used correctly, especially in Latin-American countries.25
There are some limitations to our study, for instance, we do not know if the use of ICTs varied according to disease severity. Additionally, surveyed participants knew of the purpose of the study, which may have influenced the answers given by them. Last, our survey instrument, a modified version of the original Michigan Questionnaire, has not been validated yet, which could influence future replicability of this study. However, one strength of the study is that the sample included participants of different genders, age, and educational levels.
Conclusion
In conclusion, the use of ICTs appears to be increasing in Latin America, as ICTs are becoming a mainstream tool in assisting patients in self-management care. In our study, web-based internet remains the main source for obtaining information related to hypertension. WhatsApp and Facebook were rated with the highest interest for receiving and asking health-related information. Older age and lower educational levels were consistently associated with less interest and usage for most ICTs. High-quality studies should be conducted to demonstrate how to develop and promote ICT-based resources more effectively to engage patients with hypertension through self-management education programs in developing countries.
Ethics approval and consent to participate
This study was approved by the ethics committee Comité de ética e Investigación en Seres Humanos (CEISH), Guayaquil-Ecuador, in accordance to the principles established by the declaration of Helsinki.
Abbreviations
SME, self-management education; ICTs, information and communication technologies; SMS, short-message service.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
The authors acknowledge the guidance and knowledge imparted by the MECOR Program for this study, especially from Sonia Buist MD, Ana Menezes MD, and Juliana Ferreira M.D. Special thanks to Chelsea Chica, Jose Espinoza, and Maria Fernanda Vinueza, who participated in the data recollection process. Finally, we want to express our gratitude to Universidad Espiritu Santo for their continuous support.
Author contributions
The authors have made substantial contributions to conception and design, acquisition, analysis and interpretation of data, have been involved in drafting the manuscript or revising it critically for important intellectual content and have given final approval of the version to be published. ICO, VE, MF participated in the study design process. EV performed statistical analyses and results. MF drafted the tables and figures. EV, MF and VM interpreted the analyses and wrote the manuscript. All authors read and approved the final version.
Disclosure
The authors declare no conflicts of interest related to this work.
References
1. Council ES, Redon J, Narkiewicz K, et al. ESH/ESC guidelines for the management of arterial hypertension. Eur Heart J. 2013;34:2159–2219. doi:10.1093/eurheartj/eht151
2. Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. lancet. 2013;380(9859):2224–2260. doi:10.1016/S0140-6736(12)61766-8
3. Sanchez RA, Ayala M, Baglivo H, et al. Latin American guidelines on hypertension. J Hypertens. 2009;27(5):905–922. doi:10.1097/HJH.0b013e32832aa6d2
4. Prince MJ, Ebrahim S, Acosta D, et al. Hypertension prevalence, awareness, treatment and control among older people in Latin America, India and China: a 10/66 cross-sectional population-based survey. J Hypertens. 2012;30(1):177–187. doi:10.1097/HJH.0b013e32834d9eda
5. Ecuador MdSPdlRd. Encuesta Nacional de Salud y Nutrición. Ministerio de Salud Pública del Ecuador; 2013.
6. Murray E, May C, Mair F. Development and formative evaluation of the e-Health Implementation Toolkit (e-HIT). BMC Med Inform Decis Mak. 2010;10(1):61. doi:10.1186/1472-6947-10-61
7. Alessa T, Abdi S, Hawley MS, de Witte L. Mobile apps to support the self-management of hypertension: systematic review of effectiveness, usability, and user satisfaction. JMIR Mhealth Uhealth. 2018;6(7):e10723. doi:10.2196/10723
8. Shachaf P. Cultural diversity and information and communication technology impacts on global virtual teams: an exploratory study. Inf Manage. 2008;45(2):131–142. doi:10.1016/j.im.2007.12.003
9. Alessa T, Hawley MS, Hock ES, de Witte L. Smartphone apps to support self-management of hypertension: review and content analysis. JMIR Mhealth Uhealth. 2019;7(5):e13645. doi:10.2196/13645
10. Perron BE, Taylor HO, Glass JE, Margerum-Leys J. Information and communication technologies in social work. Adv Soc Work. 2010;11(2):67. doi:10.18060/241
11. Logan AG. Community hypertension programs in the age of mobile technology and social media. Am J Hypertens. 2014;27(8):hpu125.
12. Muller AM, Alley S, Schoeppe S, Vandelanotte C. The effectiveness of e-& mHealth interventions to promote physical activity and healthy diets in developing countries: a systematic review. Int J BehavNutr Phys Act. 2016;13. doi:10.1186/s12966-016-0434-2
13. Burke LE, Ma J, Azar KM, et al. Current science on consumer use of mobile health for cardiovascular disease prevention. Circulation. 2015;132(12):
14. Facts I. Figures-The World in 2015. Geneva: The International Telecommunication Union (ITU); 2015.
15. Baptist AP, Thompson M, Grossman KS, Mohammed L, Sy A, Sanders GM. Social media, text messaging, and email-preferences of asthma patients between 12 and 40 years old. J Asthma. 2011;48(8):824–830. doi:10.3109/02770903.2011.608460
16. Cline RJ, Haynes KM. Consumer health information seeking on the Internet: the state of the art. Health Educ Res. 2001;16(6):671–692. doi:10.1093/her/16.6.671
17. Pew Research Center. Internet Use by Education. In. Electronic version ed: Pew Research Center: Washington DC, USA; 2017.
18. Young K. WhatsApp usage highest in LatAm. In: GlobalWebIndex. Vol. 2017. The trends to watch in 2017 ed. Global Web Index: United Kingdom; 2016.
19. Henostroza W. Estadísticas de Facebook en Latinoamérica y España. Webespacio. [Published 2011; Updated May 28, 2015]. Available from: https://www.webespacio.com/facebook-latinoamerica-espana-analisis-estadisticas/.
20. Patel R, Chang T, Greysen SR, Chopra V. Social media use in chronic disease: a systematic review and novel taxonomy. Am J Med. 2015;128(12):1335–1350. doi:10.1016/j.amjmed.2015.06.015
21. Al Mamun M, Ibrahim HM, Turin TC. Peer reviewed: social media in communicating health information: an analysis of facebook groups related to hypertension. Prev Chronic Dis. 2015;12. doi:10.5888/pcd12.140535
22. Kumar N, Pandey A, Venkatraman A, Garg N. Are video sharing web sites a useful source of information on hypertension? J Am Soc Hypertens. 2014;8(7):481–490. doi:10.1016/j.jash.2014.05.001
23. Greenberg AJ, Haney D, Blake KD, Moser RP, Hesse BW. Differences in access to and use of electronic personal health information between rural and urban residents in the United States. J Rural Health. 2016;34.
24. Prieto-Egido I, Simó-Reigadas J, Liñán-Benítez L, García-Giganto V, Martínez-Fernández A. Telemedicine Networks of EHAS Foundation in Latin America. Frontiers in Public Health; 2014.
25. Diez-Canseco F, Zavala-Loayza JA, Beratarrechea A, et al. Design and multi-country validation of text messages for an mHealth intervention for primary prevention of progression to hypertension in Latin America. JMIR mHealth uHealth. 2015;3(1). doi:10.2196/mhealth.3949.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
