Back to Journals » Therapeutics and Clinical Risk Management » Volume 18
Updated Perspectives on the Management of Drug-Induced Parkinsonism (DIP): Insights from the Clinic
Authors Feldman M, Marmol S, Margolesky J
Received 20 August 2022
Accepted for publication 7 December 2022
Published 20 December 2022 Volume 2022:18 Pages 1129—1142
DOI https://doi.org/10.2147/TCRM.S360268
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Matthew Feldman,* Sarah Marmol,* Jason Margolesky
Department of Neurology, University of Miami Miller School of Medicine, Miami, FL, USA
*These authors contributed equally to this work
Correspondence: Jason Margolesky, Department of Neurology, University of Miami Miller School of Medicine, 1150 NW 14th St, Miami, FL, 33136, USA, Email [email protected]
Abstract: Parkinsonism refers to the clinical combination of bradykinesia, rigidity, tremor, and postural instability. Parkinsonism is often neurodegenerative, but it can be secondary or iatrogenic, as in drug-induced parkinsonism (DIP), which is the topic of this review. We review the pathophysiology of DIP, differentiate DIP and idiopathic Parkinson’s disease (PD), list culprit medications in the development of DIP, discuss the diagnosis of DIP as well as the motor and nonmotor signs and symptoms that can help with differentiation of DIP and PD, and detail the management of DIP.
Keywords: drug-induced parkinsonism, neuroleptic-induced parkinsonism, Parkinson’s disease
Introduction
Parkinsonism refers to the clinical combination of bradykinesia, rigidity, tremor, and postural instability. Parkinsonism can be due to a primary neurodegenerative disorder, as in Parkinson’s disease; or it can be secondary, as can be seen in metal deposition diseases (like manganese toxicity or Wilson’s disease). Parkinsonism can also be iatrogenic, which is the topic of this review.
The use of neuroleptics, such as typical and atypical antipsychotics (among other drug classes), can cause an acute to subacute drug-induced parkinsonism (DIP) or may unmask underlying idiopathic Parkinson’s disease (PD). DIP was first described in 1954 in patients treated with chlorpromazine and reserpine.1 Symptoms can manifest within days of medication initiation, with the vast majority emerging by 3 months.2 A second peak of symptom onset at 12 months of exposure has been reported, mainly with the use of calcium channel blockers.3 The parkinsonism tends to be bilateral and symmetric, but this is not a rule.
Typical antipsychotics are found to bind more tightly than dopamine to the D2 receptor and have lower dissociation constants. In contrast, atypical antipsychotics are found to bind more loosely than dopamine, with higher dissociation constants, adding to the “fast-off” hypothesis.4 One pharmacokinetic study showed that the typical antipsychotic haloperidol had 6.4- and 3.9-times slower rates of dissociation compared to the atypical antipsychotics clozapine and quetiapine, respectively.5 Additionally, clozapine exerts its therapeutic effect primarily by D1 receptor antagonism, whereas typical antipsychotics such as haloperidol exert their effects via D2 receptor blockade.6 This difference in dopamine receptor affinity may contribute to the increased risk of extrapyramidal side effects.
With discontinuation of the offending medication, most cases of parkinsonism will reverse within days to months – strongly suggesting DIP.2 About two-thirds of patients recover within 7 weeks, some persist for up to 18 months.7 Alternatively, symptoms may persist and slowly progress or cease only to recur with time. When symptoms persist and worsen with time, idiopathic PD (which was preclinical at the time of neuroleptic exposure) should be suspected. The term tardive parkinsonism has been used for patients with persistent symptoms after discontinuation, but pathologic evidence suggests that most cases of tardive parkinsonism are really unmasked PD.8 Pre mortem, these entities can be differentiated with a dopamine transporter (DAT) scan – which will be normal in drug induced or tardive parkinsonism.9
In the clinic, a neurologist may be asked to help differentiate drug-induced parkinsonism from idiopathic PD. While ancillary tests, such as metaiodobenzylguanidine (MIBG) cardiac scans10 and DAT scans can be confirmatory, a proper history, with a focus on medication review, nonmotor features, and physical exam can help guide one towards the correct diagnosis. Early recognition and management are important and have long-term implications as DIP is a treatable condition, and without appropriate management can lead to falls, nursing home placement and increased mortality.11 Recognition will lead to early withdrawal of culprit agents and negate the need for dopaminergic therapies.
In this manuscript, we differentiate DIP and idiopathic PD, list culprit medications in the development of DIP, discuss motor and nonmotor signs and symptoms that can help with differentiation, and detail the management of DIP.
Diagnostic Criteria
In the DSM-V, DIP is defined as:
Parkinsonian tremor, muscular rigidity, akinesia (i.e., loss of movement or difficulty initiating movement), or bradykinesia (i.e., slowing movement with decremental response) developing within a few weeks of starting or raising the dosage of a medication (e.g., a neuroleptic) or after reducing the dosage of a medication used to treat extrapyramidal symptoms.12
It is important to note that unlike the diagnostic criteria for Parkinson’s disease, bradykinesia is not required for the diagnosis of DIP.
Pathophysiology
The classical schematic of the basal ganglia circuit is useful in understanding the pathophysiology of drug-induced parkinsonism. Neuroleptics, including antipsychotics, antiemetics, and other dopamine antagonists block D2 dopamine receptors in the striatum. Reduction of dopamine transmission in the striatum leads to disinhibition of the indirect pathway via GABA- and Enkephalin-containing striatal neurons. The subthalamic nucleus is disinhibited, leading to excitation of the globus pallidus and substantia nigra pars reticulata. In turn, the thalamocortical projections are further inhibited. Bradykinesia and other signs of parkinsonism are the manifestations of this biochemical cascade and subsequent imbalance in the direct and indirect pathways.13 The delay in improvement after withdrawal of the medication may be due to long half-lives and the persistence of neuroleptic agents in body tissue. Older neuroleptics are highly surface-active and fat-soluble and readily concentrated in cell membranes.
The disruption in the dopaminergic-cholinergic balance caused by neuroleptics may explain why parkinsonism occurs, and why anticholinergics are beneficial in addressing these symptoms. Neuroleptics cause an increase in dopamine turnover which persists following destruction of the strio-nigral pathway. Anticholinergics antagonize the increase in dopamine turnover caused by neuroleptics by decreasing activity of tyrosine hydroxylase. Anticholinergics such as benztropine can also inhibit reuptake of dopamine into nerve terminals.14
Causative Drugs
DIP has been described as the sequela of neuroleptics including typical and atypical antipsychotic medications, though the risk is low with quetiapine and clozapine. A summary of culprits is listed in Table 1.
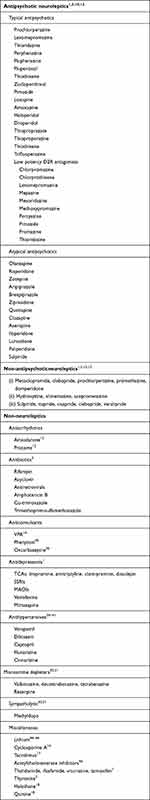 |
Table 1 Potentially Causative Agents in the Development of DIP |
Antipsychotics
Antipsychotic agents cause DIP by antagonizing central dopamine receptors as described above. A recent meta-analysis suggests that the pooled prevalence of extrapyramidal symptoms in patients taking antipsychotics is as high as 20%.19 Another study involving every resident of Piedmont, Italy, older than 39 years suggests that the risk of Parkinsonism is threefold higher in residents who were taking antipsychotics.20 The data also indicated that typical antipsychotics were more likely than atypical antipsychotics to put the patient at risk for parkinsonism. A significant caveat is that it is not clear how many of the patients studied had underlying idiopathic PD, which was simply unmasked by exposure to the medication.
Nonetheless, literature such as this underscores the significant burden of parkinsonism in patients taking both first- and second-generation antipsychotics. It is also crucial to understand the differential risk for DIP the two generations carry, which is rather nuanced.
Typical (also known as first-generation) antipsychotics have a higher affinity for central D2 receptors than atypical (second-generation) antipsychotics.20 The preference of atypical antipsychotics to antagonize serotonin receptors rather than D2 receptors is thought to contribute to the lower overall incidence of extrapyramidal symptoms compared to typical antipsychotics.21 Additionally, it is thought that the more rapid dissociation from D2 receptors contributes to the overall lower risk.22
However, the difference likely depends on the dose and also the dopamine receptor affinity. For example, a meta-analysis of all randomized controlled trials comparing second-generation antipsychotics with first-generation antipsychotics at lower doses indicated that the difference was not significant.23 In corollary to this, a retrospective cohort study shows that high-dose second-generation antipsychotics have a similar risk of developing DIP to first-generation antipsychotics.24 In particular, only the typical agents with the highest potency (haloperidol, perphenazine, and thiothixene) were found overall to pose a higher risk than the atypical antipsychotics.
There are additional differences in risk between the different second-generation antipsychotics. One meta-analysis of 54 studies suggests that patients on risperidone were more likely to require treatment for parkinsonism than patients taking ziprasidone, who were more likely to require treatment than patients taking olanzapine, quetiapine, and zotepine. All of these populations were more likely to need treatment than patients taking clozapine.3 Usage in the elderly further brings out the differences between second-generation antipsychotics. To date, only clozapine and quetiapine have evidence of lower DIP rates in the elderly.25
Non-Antipsychotic Neuroleptics
Certain antihistamines are known to increase the risk of DIP.3 In fact, the first-generation antihistamines portend a much higher risk, which is thought to be due to the fact that these drugs are phenothiazine derivatives.3 Phenothiazine is a peripheral and central D2 antagonist, which is why it is classified in this review as a neuroleptic.
Certain antiemetics are also known to increase the risk of DIP, particularly those with dopaminergic antagonism. These anti-emetics are listed in Table 1 and are metoclopramide, clebopride, promethazine, and domperidone. Although domperidone, for example, is known to cross the blood–brain barrier less easily,26 this relative restriction is less of a factor in children and the elderly. This is one of the reasons why it is suspected that these antiemetics have a higher risk of creating DIP in children and the elderly compared to the remaining population.3
The benzamide derivatives are neuroleptic medications used for various indications including Huntington’s chorea (tiapride) and as a gastroprokinetic (cisapride). They have central anti-D2 receptor action and have been observed less frequently, to put patients at risk for DIP; therefore, the risk exists, but is much lower.3
Non-Neuroleptics
Numerous other medications without clearly denoted dopamine-receptor blockade in the literature are reported to cause DIP. Of particularly high risk for inducing the development of DIP are the agents designed to deplete central dopamine storage or synthesis.1 These medications include α-methyldopa, tetrabenazine, deutetrabenazine, valbenazine, and reserpine.32,33 This can lead to many challenges when treating, amongst other disorders, patients with Huntington’s Disease.
One area of some controversy is the relation of antidepressants to DIP. Although in general the mechanism of the medications should have no relation to parkinsonism, the reports in the literature are not infrequent. In the previously mentioned French pharmacovigilance study spanning 17 years, there were 21 reports of parkinsonism after using antidepressants, which constituted 8% of all reports. 12/21 reports were from patients taking SSRIs, 3 were from imipraminics (1 amitriptyline, 1 clomipramine, and 1 dosulepin), 5 were from patients taking venlafaxine, and 1 was from a patient taking mirtazapine. A different pharmacologic review found that starting serotonergic antidepressants in patients already using L-dopa was followed by a more rapid increase in antiparkinsonian drugs.34 One case series in 2001 compiled about 100 cases of extrapyramidal symptoms associated with SSRI use.35 That same report estimates that the annual incidence is about 1–2 cases per 1000 patients. One study of a 5-HT1A agonist, Sarizotan, was found to worsen symptoms of parkinsonism.36 Serotonergic antidepressants have been shown in animals to decrease the concentration of dopamine in the striatum.37 Therefore, some low-level evidence exists for a pathophysiological link, and a low but nontrivial rate of case reports suggests that antidepressants should be considered low but non-zero risk for causing DIP.
Of the antiepileptics, valproic acid and (less frequently) phenytoin38 and per one case report oxcarbazepine39 in particular have been reported to cause DIP. A collection of studies suggests that as high as 5% of patients taking valproic acid suffer from drug-induced parkinsonism.31,40,41 The mechanism is yet unknown, but some authors suggest that oxidative stress and mitochondrial dysfunction are known to occur with valproate-induced toxicity, and note that this is also implicated in Parkinson's Disease.23
Two calcium channel blockers, flunarizine and cinnarizine, have a long history with ties to DIP27 and are widely reported to the point where in most sources it has its own name: FCIP, flunarizine-cinnarizine induced parkinsonism. The presence of pre-existing essential tremor and older age appear to be independent risk factors.28 The majority of patients tend to be female, as high as 89% in one study with 74 patients.29 The mechanism is not fully understood, but the hypotheses are important to understand in order to contrast these medications with other calcium-channel blockers, which appear to have a lower risk of DIP. Some authors believe that FCIP is caused by loss of dopamine precursor depletion as well as postsynaptic dopamine blockade.27 Flunarizine and cinnarizine differ from other calcium-channel blockers in that they carry a piperazine nucleus, which is known to interfere with dopamine storage, release, and dopamine receptor functionality.30 The presentation of FCIP tends to be an asymmetric akinetic-rigid syndrome, whereas traditional DIP caused by other agents is more frequently symmetric.31
Outside of cinnarizine and flunarizine, discussed above, calcium-channel blocker antihypertensives are considered low-risk for DIP. Verapamil and diltiazem are implicated in just a few case reports to date.42–44 There is a case report of captopril-induced DIP,45 despite a 2013 study suggesting that captopril protects nigrostriatal dopamine neurons in animal models of parkinsonism.46 No other blood pressure agents appear to have been associated with DIP to date.
One non-neuroleptic mood stabilizer that has appeared in the literature related to DIP is lithium. Lithium is notorious, like many of the drugs mentioned above, for drug–drug interactions. Interestingly, a few of the reports of extrapyramidal symptoms related to lithium use were linked to pharmacokinetic interactions with bromocriptine in patients who already had pre-existing PD.3 Other cases have been published in patients who developed apparent DIP despite no prior symptoms.46–48 The incidence appears infrequent, but underscores the importance of considering drug–drug interactions in the genesis of DIP.
Another rare but interesting class of medications associated with DIP is the cholinesterase inhibitors. This compound is already known to exacerbate symptoms of Parkinson's disease.49 One author notes that one of the hypotheses behind why lithium may cause DIP is that it has some anticholinesterase activity.50 Of note, this medication class (including donepezil, rivastigmine, and galantamine) shares a common piperazine nucleus, which is also true of flunarizine and cinnarizine as mentioned above.13 Despite this, anticholinergic medication has not yet shown clear evidence of benefit in DIP patients.51
Other miscellaneous medications that have been rarely reported to cause DIP are listed in Table 1. These medications include antiarrhythmics, some antibiotics, some immunosuppressants, and endocrine agents.
Epidemiology and Risk Factors
The accuracy of DIP prevalence is limited by misdiagnosis and myriad of criteria, leading to a lack of a single universally accepted criteria.1 There are likely several reasons for underdiagnosis including focus on the illness for which the culpable agent has been started, and a propensity to underestimate the likelihood of newer neuroleptics to cause DIP, albeit in lower frequency. Additionally, in other missed cases, motor features may have been mild, asymptomatic, or delayed.1 Conversely, there is evidence of overdiagnosis, namely in one academic center where only 1 of 24 referral for DIP ultimately retained the diagnosis.11 Therefore, prevalence data are highly variable between studies. Population studies attempting to identify what percentage of patients with parkinsonian symptoms had a diagnosis of DIP yield numbers such as 22% in Central Spain,52 20% in Olmsted, MN,53 37% in Bambui, Brazil,54 and 5% of all cases in a collaborative study across Europe.55 The disease skews towards women and the elderly, potentially due to the frequency of comorbidities, conditions requiring neuroleptics, hormonal influences, and medication interactions.3 Other independent risk factors include baseline extra-pyramidal signs, type of neuroleptic, severity of dementia,56 family history of parkinsonism,57 drug dosing,3 prior brain injury,58 severity of psychiatric disease,59 unexplained hyposmia60 and HIV infection.61 Careful history taking should elicit potential drug exposure and other risk factors.
Clinical Manifestations/Diagnosis
Motor manifestations in DIP can be indistinguishable from idiopathic PD. The prevalence of certain motor features in DIP can be gleaned by published series of patients. Hassin-Baer et al reported the motor characteristics of 75 patients with PD.62 In this cohort, most, 61%, of patients had symmetrical symptoms. Tremor, including rest and action tremor, was present in 44%. Gait disorders were mild in this cohort, and freezing of gait was rare (seen in only 2 of 75 patients). A similar prevalence of asymmetric symptoms was reported by Sethi and Zamrini, in 60% of 20 patients.63
The presence of associated signs and symptoms can help make a clinical distinction between DIP and PD. A diagnosis of DIP is supported by the co-occurrence of tardive syndromes.2 These syndromes include the classic oral-buccal lingual and other facial dyskinesia, respiratory dyskinesia, akathisia, humming, dystonia, myoclonus, tics, and chorea.11 Considering the non-motor symptom sphere can be helpful. Kim et al found that when compared to DIP patients, PD patients had significantly higher scores on the Non-Motor Symptoms Scale (NMSS). Urinary symptoms, sleep disturbances, concentration issues, and anosmia were significantly associated with PD compared to DIP.64 Morley et al compared 97 patients with DIP and 97 age-matched control with PD and determined that abnormal olfaction, sexual dysfunctional, and constipation were significantly more common in PD, present in 88%, 49%, and 47%, respectively, compared to 57%, 30% and 30% in DIP patients.65 Up to 60% of patient with PD have REM sleep behavior disorder (RBD),6 compared to less than 1% in the general population;10 and RBD is more prevalent in PD compared with DIP.65 Sialorrhea has long been recognized as an extrapyramidal side effect of neuroleptic medications,66 but can be seen in both PD and DIP, and the comparative prevalence has not been studied to our knowledge.
The diagnosis of DIP is grounded on the patient’s history of exposure to neuroleptics, or other culprit medications. The motor features of DIP and PD can be identical. Nonmotor symptoms should be elicited, and the absence of RBD, anosmia, or constipation are very pertinent negatives in the review of symptoms. Among the nonmotor symptoms, hyposmia may serve as a potential biomarker, assessable at the bedside, to distinguish DIP from an underlying degenerative synucleinopathy. In one study, among 16 DIP patients, those who had reduced tracer binding on DAT scans were also found to have abnormal olfactory function, suggesting a neurodegenerative etiology of their parkinsonism.60 In another study, among patients with DIP, lower age- and sex-adjusted olfactory scores and higher rates of anosmia were found in patients with abnormal DAT scans.67 Additionally, olfactory impairment may be able to predict response to drug withdrawal. In one study among 13 DIP patients, not only was hyposmia significantly more common in the underlying PD group but in 11 of 13 patients this was able to correctly predict symptomatic recovery after drug removal.68 While nonmotor features provide suggestive clues, they do not provide diagnostic certainty.
Resolution of parkinsonism with discontinuation of medication is diagnostic. If you cannot wait, then Dopamine Transporter (DAT) imaging can provide rapid clarity, with abnormal imaging suggesting underlying idiopathic PD.69 It is important to point out that DAT scans evaluate pre-synaptic terminal density, but it is the post-synaptic receptors that are typically stimulated by dopamine-receptor blocking agents. This is the core mechanism behind the scan’s utility in distinguishing DIP from PD. The use of DAT imaging has provided us with interesting retrospective data. Patients diagnosed with DIP who then go on to have positive DAT scans may differ clinically to those who go on to have negative scans. One article studied a population of 34 US veterans diagnosed with DIP, 12 of whom were later found to have nigrostriatal degeneration on DAT scan.70 In the population with degeneration, there was a significantly higher burden of gait abnormalities and non-motor symptoms. Specifically, lower performance in olfactory function (also reported elsewhere), the Timed Up and Go test, and total nonmotor symptom burden was a significant predictor of an abnormal DAT scan in this population.63 A similar retrospective study analyzed 51 patients at a movement disorders specialty center for whom a DAT scan was ordered to differentiate DIP and PD.71 The analysis noted that patients with greater than 2 cardinal manifestations of parkinsonism (tremor, rigidity, akinesia, postural instability) were significantly more likely (63.89% vs 93.33%, p = 0.04) to have a positive DAT scan, but that otherwise the syndromes were clinically similar. An interesting investigation of early-onset vs late-onset DIP, in relationship to neuroleptic initiation, notes that early-onset patients were more likely to have DAT abnormalities.72 This lends credence to the discussion that many patients diagnosed with DIP already have an underlying susceptibility to develop parkinsonism. Overall, these data suggest that some DAT-positive and DAT-negative patients undergoing workup for DIP vs PD may have distinct clinical features. These features are likely not sufficiently specific to make a diagnosis on their own, but still merit consideration for use alongside the other available clinical data when making practical management decisions.
Treatment
Prevention of DIP may be achieved by clinical monitoring of parkinsonism during the initial titration of culprit medications in order to determine the “neuroleptic threshold.”73 Signs of DIP may be detected as early as within 24 to 48 hours of neuroleptics in young patients, and within 96 hours in the elderly.74 Frequency of clinical monitoring can be decreased after the first three months post initiation or increase in dosage of a neuroleptic, as most cases of DIP present themselves within this time period.75,76
Treatment of DIP can be achieved by dose reduction, discontinuation of the causative agent, or switching to an alternative agent. This process should be done in conjunction with the patient’s treating psychiatrist. Discontinuation of the causative drug is advised when feasible while maintaining the risk of relapse in mind.1 For patients in whom their symptoms are stabilized, neuroleptic dose reduction would be a viable option. As noted above, due to the long half-lives of neuroleptic medications, the improvement of parkinsonism will not be immediate. With both dose reduction and discontinuation, there is a risk of withdrawal-emergent dyskinesia.
Transitioning to a drug with a lower affinity to D2 receptors is suggested if psychiatric symptoms worsen on a lower dose. Only quetiapine and clozapine have been shown not to worsen parkinsonism, with clozapine receiving Level A evidence in one review.77 Of note, patients transitioning to clozapine must be monitored for the development of agranulocytosis and be warned about the potential development of hypersalivation, which can occur in up to 54% of those receiving this medication.78
Anticholinergics such as trihexyphenidyl and benztropine are commonly used to treat DIP. Benztropine was found to effectively treat extrapyramidal symptoms in DIP at a dose of 4mg per day.79 These medications should be avoided in the elderly due to their central effects of cognitive impairment, hallucinations, delusions, and delirium in addition to their peripheral side effects of tachycardia, dry mouth, urinary retention, and constipation. Use of anticholinergics may also lead to a decrease in the plasma concentration of neuroleptics.80 Additionally, one review found that the use of benztropine hindered the efficacy of neuroleptic drugs among patients with schizophrenia, leading to worsening of positive symptoms.81 For these reasons, use of preventive anticholinergics in patients taking neuroleptics is discouraged.82
Amantadine, including the extended-release formulation Osmolex, has FDA approval for the treatment of DIP. It may be a better option in elderly patients with DIP or in patients who cannot tolerate anticholinergic side effects. In a double-blind placebo-controlled crossover study, amantadine at a dose of 100mg twice daily was as effective as trihexyphenidyl 4mg twice daily in treating DIP and produced fewer side effects.51 One double-blind crossover study found no difference in efficacy between amantadine and benztropine.83 In another double-blind study, amantadine was found to have fewer side effects than and comparable efficacy to benztropine in treating DIP, with the exception of benztropine having a greater effect on rigidity.84 Additionally, a systematic review provided Level C evidence for the use of amantadine in tardive syndromes.85
Regarding dopaminergics, levodopa is not commonly used for the treatment of DIP, and caution is encouraged in patients with psychosis.86 One study found that among patients whose DIP symptoms were controlled by anticholinergics, when switched to levodopa, they experienced worsening of tremor, rigidity, ataxia, diaphoresis, anxiety, lethargy, and depression.87 In another study, patients with parkinsonism and abnormal SPECT treated with levodopa experienced improvement in motor UPDRS scores over a three-month period, while patients with normal SPECT did not. However, this group with abnormal SPECT scan and levodopa responsiveness likely had idiopathic PD unmasked by neuroleptics, as this combination of findings would suggest an underlying degenerative cause for the observed parkinsonism rather than DIP.88 One study showed positive results with levodopa: 15 patients with DIP due to antipsychotics were treated with levodopa (doses of 300–1000mg) for up to four years; most did not experience adverse effects: only one patient had worsening of their psychiatric state and two patients developed dyskinesia. However, of these patients, eight experienced either no or slight improvement in motor symptoms as measured by the Webster score. Only two of the patients who had the culprit drug withdrawn in this study experienced either complete or transiently complete (12 months) resolution of extrapyramidal symptoms.89 Another study evaluated the use of the dopamine agonist rotigotine in patients with DIP due to antipsychotics. Twenty patients were treated with 3–8mg of rotigotine and were found to have a significant improvement in total UPDRS, UPDRS Part III, Simpson-Angus Scale, and Barnes Akathisia Rating Scale scores; this improvement was sustained for at least one month. All patients except one tolerated rotigotine well without worsening of psychotic symptoms.90
Electroconvulsive therapy (ECT) has also been found to improve the motor symptoms of DIP. In one randomized control trial, fourteen of twenty-five patients experienced transient improvement in their parkinsonism and psychosis after ECT.91 ECT has also been found useful in elderly patients with DIP, with improvement in motor symptoms noted up to six months after treatment.92
Though exercise has been found to be beneficial in PD, with improvements in disease symptoms, mobility, balance, gait and quality of life, studies have not proven its efficacy in DIP.93 Despite lack of evidence, exercise and physiotherapy should be part of the treatment regimen for patients with DIP.
Prognosis
Symptoms of DIP should resolve by six months after discontinuation of the causative medication.53 However, one case series found persistent parkinsonism nine months after discontinuation of medication in patients with a normal DAT scan, suggesting a longer period of surveillance of up to one year is required.94 One study found that the majority of patients who had been receiving treatment for DIP did not experience relapse of symptoms once the anti-parkinsonism treatment was discontinued after 3 months. The minority of patients who required resumption of treatment experienced return of symptoms within two to four weeks.95 Another study found a low risk (8%) of relapse among patients with DIP treated with anticholinergics.96
Discontinuation of the medication may lead to no change in symptoms. In one study, 16 weeks after the discontinuation of phenothiazine antipsychotics, no change in parkinsonism was observed; of note, 28% of patients in this study experienced relapse in psychiatric symptoms.97
In a large retrospective study, patients receiving either typical or atypical antipsychotics were three times as likely as unexposed subjects to develop either PD or atypical parkinsonism in the period of 18 months after initiation of drug use to two years after cessation of treatment. This risk decreased by about one-third after two years post-cessation of treatment.19 Another prospective cohort study found an increased risk of developing incident PD among patients exposed to neuroleptics of 3.16 for benzamides and 2.59 for phenothiazines.98 In one case series, two young patients (both age 35) treated with neuroleptics developed parkinsonism, which persisted and progressed after discontinuation of the medication; additionally, their symptoms were responsive to levodopa. The authors propose a potential mechanism of unmasking of idiopathic PD by neuroleptic use: neuroleptics are cytotoxic,99,100 leading to creation of free radicals, which leads to membrane and cell damage;101 concurrently, neuroleptics lead to increased firing, and increased dopamine synthesis and release in nigrostriatal dopaminergic neurons.102,103 This effect would be enhanced in a vulnerable population of neurons, such as those in patients with underlying PD, and may explain increased susceptibility to DIP.104
Transcranial sonography has been found helpful in distinguishing between DIP and suspected neurodegenerative parkinsonism; patients with suspected degenerative parkinsonism were found to have significantly higher substantia nigra echogenicity. Additionally, normal echogenicity was associated with complete recovery after drug withdrawal.105
One prospective study found shortest onset of DIP among patients treated with typical neuroleptics (1.2 ± 0.7 months), while those treated with calcium channel blockers (CCB), flunarizine or cinnarizine, had the longest time to onset (6 ± 1.4 months). The duration of parkinsonism was also longest in the CCB group (3.2 years).106
A history of prior extrapyramidal syndromes, in addition to age, sex, and medication dose may be predictive of future extrapyramidal syndromes.107 One study found that pre-treatment levels of dopamine and its metabolites correlated with development of akinesia, rigidity, and extrapyramidal symptoms; patients who excreted less free dopamine were found to develop more extrapyramidal symptoms.108
Our Approach
Our clinical approach to a patient with parkinsonism and potential DIP begins with a focus on the history. This includes a detailed medication exposure history and the duration of exposure (do not forget to ask about metoclopramide), eliciting risk factors for DIP or PD (eg, family history of PD), and considering the presence or absence of non-motor symptoms suggestive for PD (eg, RBD, constipation, and anosmia). Remember, that the physical exam, including the MDS-UPDRS part 3, may not help distinguish DIP vs PD, DIP can manifest with asymmetric or tremulous presentations, and comorbid tardive syndrome is a clue supporting DIP.
We are wary of parkinsonism or tremor (and other movement disorders) that develop after the use of non-classic culprit medications—including those implicated from the realm of case reports. Neuroleptics and VMAT inhibitors inducing parkinsonism, however, are well established and make pathophysiologic sense. Cases where symptoms develop acutely and persistent after short-term exposure of a medication are also suspect—functional movement disorders should be considered in these cases.
Stopping the potentially offending agent can be diagnostic and therapeutic. This should be done in conjunction and in conversation with psychiatry. Quetiapine or clozapine are the ideal alternatives to other neuroleptics in these scenarios. Both DIP and PD patients can benefit motorically from discontinuation of dopamine blocking agents. Then, watch and wait. Short- and long-term follow-up of the offending agent will help clarify the diagnosis. Without patience and time, DIP and PD unmasked by neuroleptics can be indistinguishable, and a DAT scan (or perhaps sympathetic cardiac scintigraphy) can quickly differentiate. DAT scan requires holding certain mood regulating medications for variable lengths of time (eg 45 days for fluoxetine), which is not always ideal or possible. A levodopa trial can be considered to aid in diagnosis, but one must use caution in patients with psychosis.
Amantadine (including its extended-release formulations) or anticholinergic agents (trihexyphenidyl, benztropine) can be considered for bothersome motor symptoms in DIP. If all goes well with the discontinuation of culprit agents, then motor treatment may not be necessary long term. Physical, occupational, and speech therapy can be utilized. Botulinum toxin injection can be used for bothersome sialorrhea. Anticholinergics being prescribed for motor symptoms can serve a dual purpose in also mitigating sialorrhea, employing their antimuscarinic and drying side effect. Similarly, amantadine can help with concurrent oro-buccal-lingual dyskinesia.
Drug-induced parkinsonism can be comorbid with other neurologic disorders. Parkinsonism can develop in a patient with Huntington’s disease using a VMAT inhibitor for chorea. Or, in an adolescent with Tourette syndrome using risperidone (or any one of many other neuroleptics) for tics. Remember to monitor for the development of parkinsonism for such patients after initiating neuroleptics for any indication.
Future Perspective
Clinicians and patients would benefit from the identification of cost-effective biomarkers to aid in the diagnosis of DIP and its differentiation from PD. Early and accurate diagnosis will facilitate discussions about prognosis and guide treatment. Skin biopsies for phosphorylated synuclein have yielded positive results in diagnosing synucleinopathies, with sensitivity and specificity >90% in differentiating idiopathic PD from controls.109 Abnormal biopsies results could help rule out DIP and would portend a worse prognosis and less expected improved with culprit drug discontinuation. DAT scan offers high sensitivity (98%), but lower specificity (67%) in early PD.110 Skin biopsy may be more cost-effective than DAT scan, and the biopsy specimen can be shipped to central processing labs, whereas patients need to travel to the DAT scan (which may not be locally available).
The Movement Disorders Society has published diagnostic criteria, intended to be utilized for research purposes, for prodromal PD.111 As a patient’s risk factors accumulate, including non-motor symptoms (particularly RBD), environmental exposures, family history, personal genetic information, and imaging biomarkers (DAT scan), the likelihood of having prodromal PD increases. Perhaps, this scoring system (or a similar one) could be applied to patients with suspected DIP to help differentiate neuroleptic induced unmasked PD, in a previously prodromal patient, from true DIP. Future studies could focus on identifying additional clinical diagnostic biomarkers discriminating PD from DIP.
There are no recent studies regarding therapeutics for DIP. Can we do better than anticholinergics or amantadine? And what should we do for patients with normal DAT scans and who do not improve after suspected culprit drug discontinuation? Is there a “tardive” parkinsonism with expected permanent deficits, similar to the oro-buccal-lingual tardive dyskinesia that persists after medication discontinuation? Better understanding of the pathophysiology that differentiates these syndromes can lead to more targeted therapy and perhaps prevention of DIP.
Conclusions
Drug-induced parkinsonism is common with prolonged neuroleptic exposure and can mimic idiopathic PD. Expeditious recognition of this syndrome can lead to timely treatment (discontinuation of the culprit medication) and thus minimize morbidity. If the patient is not improving in the months following drug discontinuation, then one must consider a case of unmasked idiopathic PD—DAT scan, levodopa trial, and perhaps skin biopsy for synuclein can arbitrate.
Author Contributions
All authors significantly contributed to the writing of this manuscript, including literature review, organization and writing the initial draft, and revisions of the non-final drafts leading to submitted manuscript. All authors have agreed to the journal to which the article is being submitted and have reviewed and agreed on submitting the manuscript as written. We agree to take responsibility and be accountable for the contents of the article.
Funding
Dr. Jason Margolesky receives funding from NINDS(NINDSU10 NS 077423) and Parkinson’s Foundation, but the funding is not related to this manuscript. Drs. Matthew Feldman and Sarah Marmol have no funding sources to declare.
Disclosure
The authors have no competing interests to declare.
References
1. Blanchet P, Kivenko V. Drug-induced parkinsonism: diagnosis and management. Res Rev Parkinsonism. 2016;6:83–91.
2. Shuaib UA, Rajput AH, Robinson CA, et al. Neuroleptic-induced Parkinsonism: clinicopathological study. Mov Disord. 2016;31(3):360–365. doi:10.1002/mds.26467
3. Bondon-Guiton E, Perez‐Lloret S, Bagheri H, Brefel C, Rascol O, Montastruc JL. Drug-induced parkinsonism: a review of 17 years’ experience in a regional pharmacovigilance center in France. Mov Disord. 2011;26:2226–2231. doi:10.1002/mds.23828
4. Seeman P. Atypical antipsychotics: mechanism of action. Can J Psychiatry. 2002;47(1):27–38. doi:10.1177/070674370204700106
5. Sahlholm K, Zeberg H, Nilsson J, et al. The fast-off hypothesis revisited: a functional kinetic study of antipsychotic antagonism of the dopamine D2 receptor. Eur Neuropsychopharmacol. 2016;26(3):467–476. doi:10.1016/j.euroneuro.2016.01.001
6. Ellenbroek BA, Artz MT, Cools AR. The involvement of dopamine D1 and D2 receptors in the effects of the classical neuroleptic haloperidol and the atypical neuroleptic clozapine. Eur J Pharmacol. 1991;196(1):103–108. doi:10.1016/0014-2999(91)90414-L
7. Marsden CD, Jenner P. The pathophysiology of extrapyramidal side-effects of neuroleptic drugs. Psychol Med. 1980;10(1):55–72. doi:10.1017/S003329170003960X
8. Frei K, Truong DD, Fahn S, et al. The nosology of tardive syndromes. J Neurol Sci. 2018;389:10–16. doi:10.1016/j.jns.2018.02.008
9. Vijayakumar D, Jankovic J. Drug-induced dyskinesia, part 2: treatment of tardive dyskinesia. Drugs. 2016;76(7):779–787. doi:10.1007/s40265-016-0568-1
10. Lee PH, Yeo SH, Yong SW, et al. Odour identification test and its relation to cardiac 123I-metaiodobenzylguanidine in patients with drug induced parkinsonism. J Neurol Neurosurg Psychiatry. 2007;78(11):1250–1252. doi:10.1136/jnnp.2007.121285
11. Esper CD, Factor SA. Failure of recognition of drug-induced parkinsonism in the elderly. Mov Disord. 2008;23(3):401–404. doi:10.1002/mds.21854
12. American Psychiatric Association. Association, AP. Diagnostic and Statistical Manual of Mental Disorders.
13. Shin HW, Chung SJ. Drug-induced parkinsonism. J Clin Neurol. 2012;8(1):15–21. doi:10.3988/jcn.2012.8.1.15
14. Young RG. The interactions of cholinergic and anticholinergic drugs with nigro-neostriatal dopaminergic neurons; 1977.
15. Werner EG, Olanow CW. Parkinsonism and amiodarone therapy. Ann Neurol. 1989;25(6):85–89. doi:10.1002/ana.410250618
16. Wasserstein PH, Honig LS. Parkinsonism during cyclosporine treatment. Bone Marrow Transplant. 1996;18(3):649–650.
17. Gmitterova K, Minár M, Žigrai M, et al. Tacrolimus-induced parkinsonism in a patient after liver transplantation – case report. BMC Neurol. 2018;18(1):44. doi:10.1186/s12883-018-1052-1
18. Ugoya SO, Agaba EI, Daniyam CA. Parkinsonism caused by adverse drug reactions: a case series. J Med Case Rep. 2011;5(1):105. doi:10.1186/1752-1947-5-105
19. d’Errico A, Strippoli E, Vasta R, et al. Use of antipsychotics and long-term risk of parkinsonism. Neurol Sci. 2021;4:2545–2553.
20. Abou-Setta AM. In first-generation versus second-generation antipsychotics in adults: comparative effectiveness. Rockville (MD); 2012.
21. Kapur S, Seeman P. Does fast dissociation from the dopamine D 2 receptor explain the action of atypical antipsychotics?: a new hypothesis. Am J Psychiatry. 2001;158(3):360–369. doi:10.1176/appi.ajp.158.3.360
22. Leucht S, Wahlbeck K, Hamann J, et al. New generation antipsychotics versus low-potency conventional antipsychotics: a systematic review and meta-analysis. Lancet. 2003;361(9369):1581–1589. doi:10.1016/S0140-6736(03)13306-5
23. Rochon PA, Stukel TA, Sykora K, et al. Atypical antipsychotics and parkinsonism. Arch Intern Med. 2005;165(16):1882–1888. doi:10.1001/archinte.165.16.1882
24. Rummel-Kluge C, Schwarz KK, Hunger H, et al. Second-generation antipsychotic drugs and extrapyramidal side effects: a systematic review and meta-analysis of head-to-head comparisons. Schizophr. 2012;1:167–177. doi:10.1093/schbul/sbq042
25. Ali T, Sisay M, Tariku M, et al. Antipsychotic-induced extrapyramidal side effects: a systematic review and meta-analysis of observational studies. PLoS One. 2021;16(9):e0257129. doi:10.1371/journal.pone.0257129
26. Montastruc JL, Llau ME, Rascol O, et al. Drug-induced parkinsonism: a review. Fundam Clin Pharmacol. 1994;8(4):293–306. doi:10.1111/j.1472-8206.1994.tb00808.x
27. Gimenez-Roldan S, Mateo D. Cinnarizine-induced parkinsonism. Susceptibility related to aging and essential tremor. Clin Neuropharmacol. 1991;14(2):156–164. doi:10.1097/00002826-199104000-00005
28. Marti-Masso JF, Poza JJ. Cinnarizine-induced parkinsonism: ten years later. Mov Disord. 1998;13(3):453–456. doi:10.1002/mds.870130313
29. Mena MA, de Yebenes JG. Drug-induced parkinsonism. Expert Opin Drug Saf. 2006;5(6):759–771. doi:10.1517/14740338.5.6.759
30. Chouza C, Caamaño JL, Aljanati R, et al. Parkinsonism, tardive dyskinesia, akathisia, and depression induced by flunarizine. Lancet. 1986;327(8493):1303–1304. doi:10.1016/S0140-6736(86)91223-7
31. Onofrj M, Thomas A, Paci C. Reversible parkinsonism induced by prolonged treatment with valproate. J Neurol. 1998;245(12):794–796. doi:10.1007/s004150050288
32. Akbar U, Kim DS, Friedman JH. Valbenazine-induced parkinsonism. Parkinsonism Relat Disord. 2020;70:13–14. doi:10.1016/j.parkreldis.2019.11.021
33. Teive HAG, Troiano AR, Germiniani FMB, et al. Flunarizine and cinnarizine-induced parkinsonism: a historical and clinical analysis. Parkinsonism Relat Disord. 2004;10(4):243–245. doi:10.1016/j.parkreldis.2003.12.004
34. van de Vijver DA, Roos RAC, Jansen PAF, et al. Start of a selective serotonin reuptake inhibitor (SSRI) and increase of antiparkinsonian drug treatment in patients on levodopa. Br J Clin Pharmacol. 2002;54(2):168–170. doi:10.1046/j.1365-2125.2001.01491.x
35. Prescrire's Editorial Staff. Extrapyramidal effects of SSRI antidepressants. Prescrire Int. 2001;10(54):118–119.
36. Olanow CW, Damier P, Goetz CG, et al. Multicenter, open-label, trial of sarizotan in Parkinson disease patients with levodopa-induced dyskinesias (the SPLENDID Study). Clin Neuropharmacol. 2004;27(2):58–62. doi:10.1097/00002826-200403000-00003
37. Dewey SL, Smith GS, Logan J, et al. Serotonergic modulation of striatal dopamine measured with positron emission tomography (PET) and in vivo microdialysis. J Neurosci. 1995;15(1 Pt 2):821–829. doi:10.1523/JNEUROSCI.15-01-00821.1995
38. Ertan S, Ulu MO, Hanimoglu H, et al. Phenytoin-induced parkinsonism. Singapore Med J. 2006;47(11):981–983.
39. Morgan JC, Sethi KD. Drug-induced tremors. Lancet Neurol. 2005;4(12):866–876. doi:10.1016/S1474-4422(05)70250-7
40. Easterford K, Clough P, Kellett M, et al. Reversible parkinsonism with normal β-CIT-SPECT in patients exposed to sodium valproate. Neurology. 2004;62(8):1435–1437. doi:10.1212/01.WNL.0000121228.32913.00
41. Jamora D, Lim S-H, Pan A, et al. Valproate-induced Parkinsonism in epilepsy patients. Mov Disord. 2007;22(1):130–133. doi:10.1002/mds.21188
42. Padrell MD, Navarro M, Faura CC, et al. Verapamil-induced parkinsonism. Am J Med. 1995;99(4):436. doi:10.1016/S0002-9343(99)80195-8
43. Dick RS, Barold SS. Diltiazem-induced parkinsonism. Am J Med. 1989;87(1):95–96. doi:10.1016/S0002-9343(89)80491-7
44. Graham DF, Stewart-Wynne EG. Diltiazem-induced acute parkinsonism. Aust N Z J Med. 1994;24(1):70. doi:10.1111/j.1445-5994.1994.tb04434.x
45. Sandyk R. Parkinsonism induced by captopril. Clin Neuropharmacol. 1985;8(2):130–133. doi:10.1097/00002826-198506000-00013
46. Sonsalla PK, Coleman C, Wong LY, et al. The angiotensin converting enzyme inhibitor captopril protects nigrostriatal dopamine neurons in animal models of parkinsonism. Exp Neurol. 2013;250:376–383. doi:10.1016/j.expneurol.2013.10.014
47. Kane J, Rifkin A, Quitkin F, Klein DF. Extrapyramidal side effects with lithium treatment. Am J Psychiatry. 1978;135(7):851–853.
48. Tyrer P, Alexander MS, Regan A, et al. An extrapyramidal syndrome after lithium therapy. Br J Psychiatry. 1980;136(2):191–194. doi:10.1192/bjp.136.2.191
49. Lecamwasam D, Synek B, Moyles K, Ghose K. Chronic lithium neurotoxicity presenting as Parkinsonʼs disease. Int Clin Psychopharmacol. 1994;9(2):127–129. doi:10.1097/00004850-199400920-00010
50. Prescrire's Editorial Staff. Cholinesterase inhibitors: tremor and exacerbation of Parkinson’s disease. Prescrire Int. 2007;16(91):197–198.
51. Fann WE, Lake CR. Amantadine versus trihexyphenidyl in the treatment of neuroleptic-induced parkinsonism. Am J Psychiatry. 1976;133(8):940–943.
52. Benito‐León J, Bermejo‐Pareja F, Rodríguez J, et al. Prevalence of PD and other types of parkinsonism in three elderly populations of central Spain. Mov Disord. 2003;18(3):267–274. doi:10.1002/mds.10362
53. Bower JH, Maraganore DM, McDonnell SK, et al. Incidence and distribution of parkinsonism in Olmsted County, Minnesota, 1976–1990. Neurology. 1999;52(6):1214. doi:10.1212/WNL.52.6.1214
54. Barbosa MT, Caramelli P, Maia DP, et al. Parkinsonism and Parkinson’s disease in the elderly: a community-based survey in Brazil (the Bambuí study). Mov Disord. 2006;21(6):800–808. doi:10.1002/mds.20806
55. de Rijk MC, Rocca WA, Anderson DW, et al. A population perspective on diagnostic criteria for Parkinson’s disease. Neurology. 1997;48(5):1277–1281. doi:10.1212/WNL.48.5.1277
56. Caligiuri MP, Lacro JP, Jeste DV. Incidence and predictors of drug-induced parkinsonism in older psychiatric patients treated with very low doses of neuroleptics. J Clin Psychopharmacol. 1999;19(4):322–328. doi:10.1097/00004714-199908000-00007
57. Myrianthopoulos NC, Kurland AA, Kurland LT. Hereditary predisposition in drug-induced parkinsonism. Arch Neurol. 1962;6(1):5–9. doi:10.1001/archneur.1962.00450190007002
58. Demars JP. Neuromuscular effects of long-term phenothiazine medication, electroconvulsive therapy and leucotomy. J Nerv Ment Dis. 1966;143(1):73–79. doi:10.1097/00005053-196607000-00008
59. Chakos MH, Mayerhoff DI, Loebel AD, et al. Incidence and correlates of acute extrapyramidal symptoms in first episode of schizophrenia. Psychopharmacol Bull. 1992;28(1):81–86.
60. Bovi T, Antonini A, Ottaviani S, et al. The status of olfactory function and the striatal dopaminergic system in drug-induced parkinsonism. J Neurol. 2010;257(11):1882–1889. doi:10.1007/s00415-010-5631-3
61. Hriso E, Masdeu KT, Grundman M. Extrapyramidal symptoms due to dopamine-blocking agents in patients with AIDS encephalopathy. Am J Psychiatry. 1991;148(11):1558–1561.
62. Hassin-Baer S, Sirota P, Korczyn AD, et al. Clinical characteristics of neuroleptic-induced parkinsonism. J Neural Transm. 2001;108(11):1299–1308. doi:10.1007/s007020100006
63. Sethi KD, Zamrini EY. Asymmetry in clinical features of drug-induced parkinsonism. J Neuropsychiatry Clin Neurosci. 1990;2(1):64–66.
64. Kim JS, Youn J, Shin H, et al. Nonmotor symptoms in drug-induced parkinsonism and drug-naïve Parkinson disease. Can J Neurol Sci. 2013;40(1):36–41. doi:10.1017/S0317167100012920
65. Morley JF, Pawlowski SM, Kesari A, et al. Motor and non-motor features of Parkinson’s disease that predict persistent drug-induced Parkinsonism. Parkinsonism Relat Disord. 2014;20(7):738–742. doi:10.1016/j.parkreldis.2014.03.024
66. Simpson GM, B. M, B. GH, Angus JWS, P. FRC, M. DP. A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl. 1970;45(S212):11–19. doi:10.1111/j.1600-0447.1970.tb02066.x
67. Morley JF, Cheng G, Dubroff JG, et al. Olfactory impairment predicts underlying dopaminergic deficit in presumed drug-induced Parkinsonism. Mov Disord Clin Pract. 2017;4(4):603–606. doi:10.1002/mdc3.12458
68. Morley JF, Duda JE. Use of hyposmia and other non-motor symptoms to distinguish between drug-induced parkinsonism and Parkinson’s disease. J Parkinsons Dis. 2014;4(2):169–173. doi:10.3233/JPD-130299
69. Olivares Romero J, Arjona Padillo A. Diagnostic accuracy of 123 I-FP-CIT SPECT in diagnosing drug-induced parkinsonism: a prospective study. Neurologia. 2013;28(5):276–282. doi:10.1016/j.nrl.2012.05.005
70. Aamodt WW, Dubroff JG, Cheng G, et al. Gait abnormalities and non-motor symptoms predict abnormal dopaminergic imaging in presumed drug-induced Parkinsonism. NPJ Parkinsons Dis. 2022;8(1):53. doi:10.1038/s41531-022-00309-8
71. Yomtoob J, Koloms K, Bega D. DAT-SPECT imaging in cases of drug-induced parkinsonism in a specialty movement disorders practice. Parkinsonism Relat Disord. 2018;53:37–41. doi:10.1016/j.parkreldis.2018.04.037
72. Chung SJ, Yoo HS, Moon H, et al. Early-onset drug-induced parkinsonism after exposure to offenders implies nigrostriatal dopaminergic dysfunction. J Neurol Neurosurg Psychiatry. 2018;89(2):169–174. doi:10.1136/jnnp-2017-315873
73. Mamo DC, Sweet RA, Keshavan MS. Managing antipsychotic-induced parkinsonism. Drug Saf. 1999;20(3):269–275. doi:10.2165/00002018-199920030-00006
74. McEvoy JP, Hogarty GE, Steingard S. Optimal dose of neuroleptic in acute schizophrenia. A controlled study of the neuroleptic threshold and higher haloperidol dose. Arch Gen Psychiatry. 1991;48(8):739–745. doi:10.1001/archpsyc.1991.01810320063009
75. Coyle JT. Early onset neuroleptic-induced extrapyramidal reactions: a second survey. In: Neuroleptics: Neurochemical, Behavioural, and Clinical Perspectives. Raven Press; 1983:75–92.
76. Sweet RA, Pollock BG. Neuroleptics in the elderly: guidelines for monitoring. Harv Rev Psychiatry. 1995;2(6):327–335. doi:10.3109/10673229509017153
77. Friedman JH. Parkinson disease psychosis: update. Behav Neurol. 2013;27(4):469–477. doi:10.1155/2013/645429
78. Prljaca E, Bećirović E, Hasanović M, et al. Clozapine-induced hypersalivation treated with sulpiride - is it a solution? Psychiatr Danub. 2021;33(Suppl 4):1230–1232.
79. Chouinard G, Annable L, Ross-Chouinard A, et al. Ethopropazine and benztropine in neuroleptic-induced parkinsonism. J Clin Psychiatry. 1979;40(3):147–152.
80. Gautier J, Jus A, Villeneuve A, et al. Influence of the antiparkinsonian drugs on the plasma level of neuroleptics. Biol Psychiatry. 1977;12(3):389–399.
81. Miller R. Dose-response relationships for the antipsychotic effects and Parkinsonian side-effects of typical neuroleptic drugs: practical and theoretical implications. Prog Neuropsychopharmacol Biol Psychiatry. 1997;21(7):1059–1094. doi:10.1016/S0278-5846(97)00099-7
82. World Health Organisation. Prophylactic use of anticholinergics in patients on long-term neuroleptic treatment: a consensus statement. Br J Psychiatry. 1990;156(3):412. doi:10.1192/bjp.156.3.412
83. Kelly JT, Zimmermann RL, Abuzzahab FS, et al. A double-blind study of amantadine hydrochloride versus benztropine mesylate in drug-induced parkinsonism. Pharmacology. 1974;12(2):65–73. doi:10.1159/000136523
84. DiMascio A, Bernardo DL, Greenblatt DJ, Marder JE. A controlled trial of amantadine in drug-induced extrapyramidal disorders. Arch Gen Psychiatry. 1976;33(5):599–602. doi:10.1001/archpsyc.1976.01770050055008
85. Bhidayasiri R, Jitkritsadakul O, Friedman JH, et al. Updating the recommendations for treatment of tardive syndromes: a systematic review of new evidence and practical treatment algorithm. J Neurol Sci. 2018;389:67–75. doi:10.1016/j.jns.2018.02.010
86. Moskovitz C, Moses H 3rd, Klawans HL. Levodopa-induced psychosis: a kindling phenomenon. Am J Psychiatry. 1978;135(6):669–675.
87. Yaryura-Tobias JA, Wolpert A, Dana L, et al. Action of L-dopa in drug induced extrapyramidalism. Dis Nerv Syst. 1970;31(1):60–63.
88. Tinazzi M, Morgante F, Matinella A, et al. Imaging of the dopamine transporter predicts pattern of disease progression and response to levodopa in patients with schizophrenia and parkinsonism: a 2-year follow-up multicenter study. Schizophr Res. 2014;152(2–3):344–349. doi:10.1016/j.schres.2013.11.028
89. Hardie RJ, Lees AJ. Neuroleptic-induced Parkinson’s syndrome: clinical features and results of treatment with levodopa. J Neurol Neurosurg Psychiatry. 1988;51(6):850–854. doi:10.1136/jnnp.51.6.850
90. Di Fabio R, De Filippis S, Cafariello C, et al. Low doses of rotigotine in patients with antipsychotic-induced parkinsonism. Clin europharmacol. 2013;36(5):162–165. doi:10.1097/WNF.0b013e3182a2ce3f
91. Moellentine C, Rummans T, Ahlskog JE, et al. Effectiveness of ECT in patients with parkinsonism. J Neuropsychiatry Clin Neurosci. 1998;10(2):187–193. doi:10.1176/jnp.10.2.187
92. Sadananda SK, Holla B, Viswanath B, et al. Effectiveness of electroconvulsive therapy for drug-induced parkinsonism in the elderly. J ECT. 2013;29(1):e6–e7. doi:10.1097/YCT.0b013e3182611563
93. Grazina R, Massano J. Physical exercise and Parkinson’s disease: influence on symptoms, disease course and prevention. Rev Neurosci. 2013;24(2):139–152. doi:10.1515/revneuro-2012-0087
94. Lim TT, Ahmed AA, Itin I, et al. Is 6 months of neuroleptic withdrawal sufficient to distinguish drug-induced parkinsonism from Parkinson’s disease? Int J Neurosci. 2013;123(3):170–174. doi:10.3109/00207454.2012.732976
95. Orlov P, Kasparian G, DiMascio A, Cole JO. Withdrawal of antiparkinson drugs. Arch Gen Psychiatry. 1971;25(5):410–412. doi:10.1001/archpsyc.1971.01750170026005
96. Fleischhauer J. Sind Anticholinergika in der Langzeittherapie des Neuroleptika-induzierten Parkinson-Syndroms unverzichtbar? Eine Entzugsstudie [Are anticholinergics indispensable in the long-term therapy of neuroleptic-induced Parkinson syndrome? A withdrawal study (author’s transl)]. Arzneimittelforschung. 1976;26(6):1183–1184. German.
97. Hershon HI, Kennedy PF, McGuire RJ. Persistence of extra-pyramidal disorders and psychiatric relapse after withdrawal of long-term phenothiazine therapy. Br J Psychiatry. 1972;120(554):41–50. doi:10.1192/bjp.120.554.41
98. Foubert-Samier A, Helmer C, Perez F, et al. Past exposure to neuroleptic drugs and risk of Parkinson disease in an elderly cohort. Neurology. 2012;79(15):1615–1621. doi:10.1212/WNL.0b013e31826e25ce
99. Christensen E, Moller JE, Faurbye A. Neuropathological investigation of 28 brains from patients with dyskinesia. Acta Psychiatr Scand. 1970;46(1):14–23. doi:10.1111/j.1600-0447.1970.tb02097.x
100. Nielsen EB, Lyon M. Evidence for cell loss in corpus striatum after long-term treatment with a neuroleptic drug (flupenithixol) in rats. Psychopharmacology. 1978;59(1):85–89. doi:10.1007/BF00428036
101. Pall HS, Blake D, Williams A, et al. Evidence of enhanced lipid peroxidation in the cerebrospinal fluid of patients taking phenothiazines. Lancet. 1987;330(8559):596–599. doi:10.1016/S0140-6736(87)92987-4
102. Bunney BS, Walters JR, Roth RH, et al. Dopaminergic neurons: effect of antipsychotic drugs and amphetamine on single cell activity. J Pharmacol Exp Ther. 1973;185(3):560–571.
103. Scatton B, Garret C, Julou L. Acute and subacute effects of neuroleptics on dopamine synthesis and release in the rat striatum. Naunyn Schmiedebergs Arch Pharmacol. 1975;289(4):419–434. doi:10.1007/BF00508415
104. Melamed E, Achiron A, Shapira A, et al. Persistent and progressive parkinsonism after discontinuation of chronic neuroleptic therapy: an additional tardive syndrome? Clin Neuropharmacol. 1991;14(3):273–278. doi:10.1097/00002826-199106000-00013
105. Lopez-Sendon Moreno JL, Alonso-Cánovas A, Buisán Catevilla J, et al. Substantia nigra echogenicity predicts response to drug withdrawal in suspected drug-induced Parkinsonism. Mov Disord Clin Pract. 2016;3(3):268–274. doi:10.1002/mdc3.12281
106. Munhoz RP, Bertucci Filho BFD, Teive HAG. Not all drug-induced parkinsonism are the same: the effect of drug class on motor phenotype. Neurol Sci. 2017;38(2):319–324. doi:10.1007/s10072-016-2771-y
107. Keepers GA. Use of neuroleptic-induced extrapyramidal symptoms to predict future vulnerability to side effects. Am J Psychiatry. 1991;148(1):85–89.
108. Crowley TJ, Hoehn MM, Rutledge CO, et al. Dopamine excretion and vulnerability to drug-induced parkinsonism: schizophrenic patients. Arch Gen Psychiatry. 1978;35(1):97–104. doi:10.1001/archpsyc.1978.01770250099010
109. Gibbons CH, Garcia J, Wang N, et al. The diagnostic discrimination of cutaneous α-synuclein deposition in Parkinson disease. Neurology. 2016;87(5):505–512. doi:10.1212/WNL.0000000000002919
110. de la Fuente-Fernandez R. Role of DaTSCAN and clinical diagnosis in Parkinson disease. Neurology. 2012;78(10):696–701. doi:10.1212/WNL.0b013e318248e520
111. Berg D, Postuma RB, Adler CH, et al. MDS research criteria for prodromal Parkinson’s disease. Mov Disord. 2015;30(12):1600–1611. doi:10.1002/mds.26431
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
