Back to Journals » International Journal of General Medicine » Volume 12
University students’ knowledge, attitudes, and practice regarding antibiotic use and associated factors: a cross-sectional study in the United Arab Emirates
Authors Jairoun A , Hassan N, Ali A, Jairoun O, Shahwan M , Hassali M
Received 7 January 2019
Accepted for publication 17 April 2019
Published 28 June 2019 Volume 2019:12 Pages 235—246
DOI https://doi.org/10.2147/IJGM.S200641
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Ammar Jairoun,1 Nageeb Hassan,1 Abdelazim Ali,1 Obaida Jairoun,2 Moyad Shahwan,1 Mohamed Hassali3
1College of Pharmacy and Health Sciences, Ajman University, Ajman, UAE; 2College of Dentistry, Ajman University, Ajman, UAE; 3Discipline of Social and Administrative Pharmacy, School of Pharmaceutical Sciences, Universiti Sains Malaysia, Penang, Malaysia
Purpose: Antibiotic resistance is one of the world’s most fatal health crises. Medical students are the antibiotic prescribers of tomorrow, so better understanding of their knowledge, attitudes, and practice (KAP) pertaining to antibiotic use is crucial.
Objectives: This study aimed to assess the KAP of antibiotics and associated factors among university students in the United Arab Emirates (UAE).
Methods: This was a descriptive cross-sectional study conducted among a random sample of undergraduate students from Ajman University in the UAE. A self-administered pretested questionnaire was used to collect data on students’ demographics and their KAP regarding antibiotic use. Data were analysed using STATA version 14.2. P<0.05 was considered statistically significant.
Results: This study showed that university students have a high rate of antibiotic self-medication. The average KAP score was 56% (95% CI 55%–57%). Statistical modeling showed that major, study year, age, and sex were strong determinants of KAP regarding antibiotic use.
Conclusion: There is a need to develop an effective and comprehensive antibiotic-stewardship program as part of undergraduate education. Moreover, reinforcing antibiotic-use policies, involving pharmacies, drug supply, distribution, and sale, are also urgently needed.
Keywords: antibiotic usage, behavior, KAP, self-medication
Introduction
Antibiotic resistance is absolutely one of the world’s most fatal health crises.1 Without prompt action, the yearly death toll could reach 10 million by 2050, which is definitely more than deaths resulting from cancer, measles, cholera, and traffic accidents combined.1 The phenomenon is not simple, because it involves certain microbial characteristics, technological developments that empower the transmission of drug-resistant organisms, selective strains of antimicrobial consumption, and demographic issues. Such infections are becoming practically untreatable, resulting in a boost in morbidity, mortality, and health-care expenses.2 Self-medication is defined as the use of medications or any pharmaceutical product by the public to treat common health problems, self-diagnosed disorders, or the intermittent or continued use of medications or chronic or recurrent disease or symptoms without being prescribed by a doctor.3 However, antibiotic self medication has become a global concern that has begun to worry researchers, because of its irrational use, especially among adolescents and college students. Antibiotic self-medication can result from many factors, such as public knowledge and attitudes toward antibiotics, unregulated sell of antibiotics at pharmacies, and relaxed policies concerning regulation of antibiotics. Overusing antibiotics or using them irrationally can easily result not only in the emergence of resistant bacterial strains but also in adverse reactions, and can also result in an economic burden on national health systems.4 According to a September 2013 report from the US Centers for Disease Control and Prevention, treatment of antibiotic-resistant infections adds $35 billion in health-care costs and 8 million hospital days per year in the US.5
One study was performed in 45 hospitals in the southeastern Mediterranean region using short-framed interviews in outpatient clinics or primary-health centers in Turkey, Egypt, Cyprus, Jordan, Lebanon, Jordan, Tunisia, and Libya. On average, 19% of patients were under the self-medication umbrella (<0.1% in Cyprus to 37% in Lebanon) and 48.4% of the whole group claimed that they stored antibiotics at home, with the highest percentage in Lebanon (60%).6 The evolution of antimicrobial resistance in Gulf Cooperation Council (GCC) countries may have occurred for a number of reasons. One is the ease of access and availability of broad-spectrum antibiotics, such as carbapenems and third- and fourth-generation cephalosporins and quinolones, in health-care settings. Most GCC countries lack the presence of antimicrobial-stewardship programs, especially in the inpatient setting, where broad-spectrum antimicrobial agents are used. The lack of clinical pharmacists and infectious disease specialists may be a major contributor to the current emergence of resistance.7
In the GCC region, Al Rasheed et al8 suggested that in Saudi Arabia in 2014, nearly 79% of the subjects of their cross-sectional survey of Al Wazarat Health Centre admitted self-medication.5 According to studies, even though over-the-counter trade of antibiotics is not allowed by law in GCC countries, 68% of pharmacies in Abu Dhabi, 78% in Riyadh, and 87 of 88 pharmacies in Saudi Arabia sold antibiotics without prescriptions issued.1 In the United Arab Emirates (UAE), similarly to other countries, there is spreading concern regarding the haphazard prescription of antibiotics and even self-administration for mild symptoms for which they may not be needed. This can lead to emerging antibiotic-resistant species of bacteria, thus hindering the effect of some antibiotics when they are needed to treat a certain infection.6 There has been growing concern regarding this issue in Saudi Arabia as well. New hospital species of resistant bacteria have emerged in the community. Some efficient steps have been considered to enhance local guidelines regarding the appropriate consumption of different antibiotics.9 In 2016, the GCC Infection Control Board established a new strategic plan to fight antimicrobial resistance disasters with a focus on four basic points pertaining to this issue, including the human aspect.10 Currently, there is legislations that prevents the dispensing of any antimicrobial product without a valid prescription in the UAE.
University students, especially medical students, are future antibiotic prescribers. Therefore, understanding of their knowledge, attitudes, and practice (KAP) in relation to public usage of antibiotics can greatly impact antibiotic-related issues. This highlights the importance of conducting this study to compile needed data for adequate decision-making. This study aimed to assess KAP pertaining to antibiotic self-medication and to explore significant risk factors.
Methods
Study setting and design
This study was a descriptive cross-sectional survey conducted among a random sample of undergraduate students from Ajman University in the UAE. It was conducted for 12 months from January to December 2017.
Target population
The study population consisted of undergraduates covering a broad range of disciplines, such as dentistry, pharmacy, medicine, engineering, management, information technology, and law.
Sample size and sampling technique
As the prevalence of antibiotic self-medication may range from 27% to 91.7% according to many previous studies, we assumed 63% prevalence of antibiotic self-medication among university students. The α-level was set at 5% so that we had a 95% CI. The precision of the 95% CI was fixed at 5% so that the interval's width will be at maximum 10%. According to these assumptions above, we needed a sample of 1,183 participants if we assume a nonresponse rate around 70%. The Admission and Registration Department of Ajman University provided an Excel sheet of information including student names, college, study year, and email addresses. Simple random-sample selection was used for sampling, where the study population was randomly selected according to their ID numbers and stratified according to college and study year. The final sample size chosen was 1,200 students. The questionnaire was distributed to the students who had been preselected according to the random sample chosen from the admission and registration Excel sheet. The questionnaires were handed to students during lectures (at the end of their classes) before the examination period. The nature and objectives of the research were explained to the students on the first page of the questionnaire, and students willing to participate were requested to sign the consent form provided prior to filling the questionnaire. Participation was voluntary, and no benefits or incentives were given to participants.
Research-instrument development
After investigation of previous similar studies KAP regarding antibiotic use in the literature, a structured self-administered questionnaire was designed and adapted to cover all the main key points of the research and in a way that suited the local UAE population.
The questionnaire was then reviewed and assessed by subject experts for its content, design, relevance, readability, and comprehension. The questionnaire was validated by seven clinical pharmacy lecturers at Ajman University after assessment of its content relevance and appropriateness. Minor modifications were made based on their comments. Moreover, quantitative content validity of the instrument was ascertained based on Lawshe’s content-validity ratio (CVR).11 CVR was calculated for each item, and all items had a CVR scores of at least 0.71. Items with CVR ≥0.7 are acceptable, and if an item does not reach this threshold, it is normally deleted from the final instrument.12 Then, a content-validity index (CVI) was obtained by calculating the mean of the CVR values for all items meeting the CVR threshold of 0.7 and retained for the final instrument. The final reported content validity–index value for the instrument was 0.71, indicating acceptable content validity.13 In addition, for reliability a pilot study was done on 100 students from Ajman University and necessary changes made accordingly. Those who participated in the pilot study were excluded from the final analysis. Reliability analysis of the instrument was performed by calculating Cronbach’s α. The α-value of the questionnaire was 0.73, indicating acceptable internal consistency.
Research-instrument sections
The survey was written in Arabic and English, and consisted of 38 questions divided into four sections. The first section highlighted demographic information, ie, sex, age, nationality, major, college, and study year. Section two comprised 12 questions and evaluated knowledge of participants regarding drug sensitivity, susceptibility, and resistance and side effects of antibiotics. The third section had six questions and assessed respondents’ attitudes on the seriousness of antibiotic abuse, its effect on the student and his/her family, causes of antibiotic abuse, and introducing an educational course and campaign on the proper use of antibiotics. The fourth section had 15 questions and examined the frequency of antibiotic use in fever, illnesses, and other symptoms and understanding of prescription drugs and doctors' prescriptions. Questions evaluating knowledge of antibiotic use were associated with categorical responses: (yes/no). Each correct answer was scored 1 point, while a wrong answer was given 0 points. Similarly, questions evaluating attitudes toward antibiotic use associated with categorical responses (yes/no). “Yes” scored 1 point and no given 0 points.Questions assessing the practice of antibiotic use had options of “always”, “often”, “rarely” or “never”. Rarely or never scored 1 point, while always and often were given 0 points. This scoring system was applied for all practice questions, except for the last two — 14 and 15. Sum scores for KAP were calculated, from minimum 0 to maximum 33 for each participant.
Ethical considerations
The study was approved by the University Institutional Ethical Review Committee (F-A-17-05-01), and an approval letter was obtained to allow the researchers to distribute and collect the questionnaires among Ajman University students including those aged <18 years. Participation of students in this study was entirely voluntary and without compensation. Before data collection, the purpose of the survey was explained, and they were also informed that completion and submission of the questionnaire would be undertaken upon their consent. All students signed the informed consent.
Statistical analysis
Data were analyzed using Stata version 14.2. Qualitative variables were summarized using frequencies and percentages as appropriate, whereas quantitative variables were summarized using means ± SD. Unpaired Student t-tests and their nonparametric versions, as well as one-way ANOVAs, were used to test average differences in quantitative variables across groups. KAP scores were created to measure KAP regarding antibiotic use and resistance. Each score was defined as the proportion of questions for which the answers were correct. This score ranged 0–100% and was used as a good approximation of overall KAP. Simple, multiple linear and logistic regression were used to investigate associations between KAP scores for antibiotic use and other significant risk factors. This method used the derived KAP score as the dependent variable in a regression model. The stepwise method was used for variable selection and model building. P<0.05 was considered statistically significant.
Results
Demographic and socioeconomic characteristics
A total of 1,200 subjects participated in the study and completed the whole questionnaire. Among these participants, 59.5% were female and approximately 40.5% male. Regarding their majors, 50% were medical students and 50% nonmedical students. Approximately 55.5% of participants were in their first year and 44.5% in their final year. The vast majority were non–UAE nationals. For more details, see Table 1.
 |
Table 1 Number and percentage of the questions on demographic characteristics |
Prevalence of antibiotic self-medication
In this study, 38.2% (95% CI 35%–41%) of the participants had self-medicated with antibiotics during the previous 6 months. Of these, 43.6% used amoxicillin, 32.9% cephalosporin, 13.9% macrolides, and 9.6% quinolone antibiotics (see Figure 1).
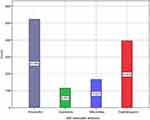 |
Figure 1 Bar chart of self-medicated antibiotics. |
KAP regarding antibiotic self-medication: analysis of overall KAP scores
The average KAP score was 56% (95% CI 55%–57%). This means that on a KAP scale of 0–100, participants scored an average of 56 points for KAP pertaining to antibiotic use (Figure 2).
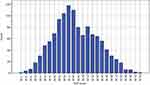 |
Figure 2 Histogram of knowledge, attitudes, and practice scores. |
Table 2 shows the distribution of KAP scores according to demographic and socioeconomic status. The table also provides 95% CIs for the estimates and P-values. These P-values were derived from results of unpaired-sample t-tests and one-way ANOVAs for testing the assumption that the average KAP score would be the same across groups. Medical students scored relatively higher than nonmedical students: 58% compared to 52% for nonmedical students. Additionally, final-year students scored better than first-year students: 58% compared to 55% for first-years. Female scored better on KAP scores than males: 58% vs 53%. Similarly, older participants were more likely to score better than younger participants. For more details on score comparisons according to demographic and socioeconomic factors, see Table 2.
 |
Table 2 Knowledge, attitude and practice (KAP) scores according to demographic and socio-economic variables |
Knowledge,attitude and practice (KAP) towards antibiotics: analysis of individual questions
This study investigated KAP regarding antibiotic self-medication by both looking at individual questions in the questionnaire and using the derived overall KAP score.
Table 3 presents the results of each questions related to knowledge of antibiotic use. In general, a satisfactory proportion of students showed good knowledge of the majority of the knowledge items, except in seven items/questions. The first of these seven questions (12) was related to knowledge of drug-susceptibility testing of bacteria. Only 18.3% of students correctly defined drug-susceptibility testing of bacteria. The second question (8) was related to the fact that the efficacy of antibiotics is better if they are newer and the price higher. The third question (5) was about the source of antibiotics. More than half the students (55.1%) obtained antibiotics without a prescription. The fourth question (3) related to the effectiveness of antibiotics against viral infections. Nearly half the students (48%) incorrectly believed that antibiotics can be used to cure infections caused by viruses. Another set of questions involved knowledge of different classes of antibiotics (9–11).
 |
Table 3 Number and percentage of the questions on the knowledge of antibiotic use |
Table 4 displays results from questions related to attitudes toward antibiotic use. In general, a good proportion of students showed good attitudes on the majority of the attitude items, except one (Q14). More than half the students (55.5%) did not perceive that bacterial antibiotic resistance was a problem in the UAE.
 |
Table 4 Number and percentage of the questions on the attitude of antibiotic use |
Table 5 shows results from questions related to practices of antibiotic use. In general, a low proportion of students showed good practice toward the majority of items. Of the total, 54.6% advocated the use of antibiotics on patients with low fever (<38.5°C). Moreover, 58% and 68.5% of the students would use antibiotics with high frequency for common colds and sore throats, respectively. Furthermore, high proportions of study participants would advocate the use of antibiotics more frequently when symptoms of respiratory tract infection occur.
 |
Table 5 Number and percentage of the questions on the practice of antibiotic use |
Factors influencing KAP scores
Table 6 displays results of simple linear regression applied to each demographic and socioeconomic variable separately.
 |
Table 6 Simple linear regression model applied to each demographic and socio-economic variable separately |
Table 7 displays results of simple binary logistic regression applied to each demographic and work variable. ORs show the magnitude of associations. Medical students were more likely to score better for KAP regarding antibiotic use than nonmedical students (OR 1.36, 95% CI 1.31–1.42; P=0.000). Final-year student scored better for KAP regarding antibiotic use compared to first-year students (OR 1.12, 95% CI 1.08–1.17; P=0.000). Female students had higher KAP scores than male students (OR 1.22, 95% CI 1.17–1.27; P=0.000). Students aged 21–25 years scored better for KAP regarding antibiotic use than those aged 16–20 years (OR 1.07, 95% CI 1.03–1.11; P=0.002). The same pattern of results was observed between students aged ˃25 years and those aged 16–20 years (OR 1.17, 95% CI 1.06–1.29; P=0.002).
 |
Table 7 Simple binary logistic regression model applied to each demographic and socio-economic variable separately |
To select the set of factors that together influenced KAP regarding antibiotic use, we used a stepwise procedure applied to multiple linear regression. This showed that major, study level, sex, and age were jointly highly associated with KAP regarding antibiotic use (Table 8).
 |
Table 8 Final multiple liner regression model (stepwise procedure) for knowledge, attitudes, and practice regarding antibiotic use |
Discussion
This is the first nationwide study to assess KAP toward antibiotic self-medication among UAE university students, and showed that they had a high rate of antibiotic self-medication. The average KAP score was 56% (95% CI 55%–57%). This means that the overall level of KAP regarding antibiotic use is poor. Statistical modeling showed that major, study year, age, and sex were strong determinants of KAP regarding antibiotic use.
Strengths and limitations
An important strength of this study was that it used a large random sample of university students; therefore, there can be confidence that the findings are generalizable to the whole population. The sampling frame was a list of students and their mobile telephone numbers that were registered at the Admission and Registration Department. These lists are regularly updated by the department. Students were randomly sampled from the university not more than once to avoid bias. The sample size was estimated before the start of the study and considered to provide adequate predictive power. The questionnaire was adapted from published instruments and revised by experts to ensure content validity. It was accurately translated into Arabic and tested to ensure clarity of questions and respondents’ ability to provide accurate answers. There were several limitations to the study. First, as with any cross-sectional design, it is not possible to infer cause and effect or the direction of any associations between the dependent and independent variables. While there is reasonable confidence in the generalizability of the results, selection and response bias may affect this. It was not possible to compare nonresponders with responders to investigate this source of bias further. Additionally, since the study was conducted in one university, it is not directly generalizable to other universities.
Comparison with prior studies
Given the importance of antimicrobial resistance worldwide and the irrational use of antibiotics, we evaluated university students’ self medication and KAP toward antibiotics to help guide development of optimal training in antibiotic practice. To our knowledge, this is the first study in the UAE to evaluate KAP among university student toward antibiotic use and the first to examine the impact of the medical curriculum on same. In the current study, 38.2% of the students reported self-medicating with antibiotics during the previous 6 months. This finding is similar to that of a study14 conducted on undergraduates in northern Nigeria (38.8%), but higher than found in studies in China (27%)15 and Jordan (28%).16 These rates were much lower than found in Kosovo (63.2%),17 Jordan (63.9%),18 Pakistan (60%),19 southern China (47.8%),20 western China (40.2%),21 Khartoum (41%),22 and Italy (45%)23 Even higher rates of antibiotic self-medication have been observed in Australia (91.7%),24 Beijing (90.4%),25 Kashmir (80.89%),26 and Punjab (74%).27 Such a high prevalence of antibiotic self-medication among university students reflects the irrational use of antibiotics, which in turn increases the risk of antimicrobial resistance, adverse effects, and an economic health burden. Moreover, the high rate of self-medication seen in this study may be attributed to the underregulated sales of these medicines in the UAE and the students’ wish to have quick recovery from illness.
In the present study, penicillin and cephalosporin followed by macrolides were the most commonly used antibiotics. Previous studies are also consistent with this result.15,28
Overall KAP regarding antibiotic use was poor. The average KAP score was 56% (95% CI 55%–57%). This finding was consistent with those of a prior report that found that knowledge of the majority of students was moderate–poor.16,29–33 These results are inconsistent with other studies that showed adequate knowledge regarding antibiotic use and resistance.34 This discrepancy might be due to the difference in study settings, structure of antimicrobial curriculum of each university, and details of the questionnaires. In this study, it appears that the majority of the respondents (91.4%) knew that antibiotics can kill bacteria and can be used to cure bacterial infections. This was consistent with the 52% of Brahmbhatt and Patel.35 It is also noteworthy that other questions regarding knowledge of antibiotic use were also rated by a high proportion of respondents. About 76% of respondents had heard about resistance of bacteria and that frequent use of antibiotics decreases treatment efficacy when using the antibiotic again. Moreover, 70% of respondents correctly answered that use will not speed up recovery from colds, coughs, and other diseases. The present study also reports limited knowledge on such items as drug-susceptibility testing of bacteria and antibiotic classes. This implies that a rigorous assessment of university students of where knowledge is lacking would be helpful in developing an educational program.
In terms of attitudes toward antibiotics, a majority of the participants believed that there was current irrational use of antibiotics, that this was the main cause of bacterial resistance and, and that it affected their family’s health. These results are in line with other studies.30,36–38 Interestingly, more than half the participants (55%) did not perceive antibiotic resistance to be a problem in the UAE. This finding is lower than results reported by other studies in which a majority believed that antibacterial resistance was a serious global and national problem.30,35,36,39 These findings suggest that education on this issue is good at our university.
The results of this study reflect some confusion and misinterpretation of student knowledge regarding antibiotic use. About 44.5% reportedly stopped using antibiotics upon symptom improvement. This finding is higher than that found in previous studies.23,40,41 Several studies from around the world have shown that students interrupt and do not not complete their course of antibiotics.29,42
Moreover, this study shows that study participants were not aware of the ineffectiveness of antibiotics against viruses, which would put them at unnecessary risk of contracting infections with resistant pathogens. Over half the students took antibiotics when they had a common cold or sore throat. Other studies have shown similar results that cold, flu, cough, and sore throat were the most common reasons for antibiotic use by university students.16,29,43–46 This finding agrees with the results of many other studies.21,26,41,47
In the present study, students from the medical college scored remarkably better than those from the nonmedical college in KAP toward antibiotic use and resistance (P<0.001). This agrees with other findings about knowledge of antibiotic use reported in the literature.16,29,48,49 Other studies in Malaysia45,50 among final-year dentistry and pharmacy students reported good knowledge of antibiotic use among medical students. These findings are consistent with a study in Italy23 among students of a school of medicine that reported good knowledge about antibiotic use. Therefore, these results suggest that medical students have more knowledge about antibiotics than other students or the public.
Our study also analyzed levels among different grades to assess the impact of the medical curriculum on KAP toward antibiotics. This increased as they progressed in their years of study (P<0.001). Likewise, previous studies have obtained results that are consistent with this result.26,46 This was in contrast to Keihanian et al,30 who claimed that grade of interns did not affect the level of KAP.
This study revealed a sex difference in KAP toward antibiotic use and resistance (P˂0.001). Female students showed higher scores than their male counterparts. This is similar to a study performed in Italy among medical, dental, and nursing students.23 In contrast, the sex of the students did not significantly influence their self-medication with antibiotics.45,46 The findings from current study imply that university students do not practice what they know and educational interventions should be implemented to bridge the existing gap between knowledge and practice.
Implications of this study
Currently, little is known about KAP regarding antibiotic use in the UAE. This study presents useful data on KAPof university students with respect to antibiotic use and resistance. This vital information can be used to better understand the magnitude of the problem to plan or propose effective educational interventions that aim at improving KAP regarding antibiotic use among university students. Moreover, it will allow researchers to identify challenges through academic research and make evidence-based policy recommendations to support the rational use of these medicines in the UAE. In addition, future research can be presented to policy-makers at national and international meetings.
Conclusion
Students’ KAPregarding antibiotic use, which drives the practice of self-medication, reflects a gap in medical curricula in UAE institutes and medical colleges. These findings warrant the development of an effective and comprehensive antibiotic-stewardship program in undergraduate education. Additionally, reinforcement of antibiotic-use policies involving pharmacies and drug supply, distribution, and sale is urgently needed.
Abbreviation list
KAP, knowledge, attitudes, and practice; UAE, United Arab Emirates; GCC, Gulf Cooperation Council
Acknowledgments
We would like to thank our colleagues for their participation in the survey, who supported our work in this way and helped us get results of better quality. We also want to express much extremely indebtedness and thanks to Dr Mohamed Shammasin for all of the support, guidance, advice, and knowledge he has given us. This research did not receive any grants from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
All authors contributed toward data analysis, drafting and revising the paper, gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zain A. Unregulated antibiotic use could kill 10 million people by 2050 [homepage on the Internet]. 2018. Available from: https://www.khaleejtimes.com/news/uae-health//unregulated-antibiotic-use-could-kill-10-million-people-by-2050. Accessed July 6, 2017.
2. Cohen ML. Epidemiology of drug resistance: implications for a post–antimicrobial era. Science. 1992;257(5073):1050–1055. doi:10.1126/science.257.5073.1050
3. World Health Organization. Guidelines for the Regulatory Assessment of Medicinal Products for Use in Self-Medication. Geneva: World Health Organization; 2000.
4. Gyssens IC. Quality measures of antimicrobial drug use. Int J Antimicrob Agents. 2001;17(1):9–19. doi:10.1016/S0924-8579(00)00208-9
5. Dantas G, Sommer M. How to fight back against antibiotic resistance. Am Sci. 2014;102(1):42–51. doi:10.1511/2014.106.42
6. Borg MA, Cookson BD, Gur D, et al. Infection control and antibiotic stewardship practices reported by south-eastern Mediterranean hospitals collaborating in the ARMed project. J Hosp Infect. 2008;70(3):228–234. doi:10.1016/j.jhin.2008.07.002
7. Aly M, Balkhy HH. The prevalence of antimicrobial resistance in clinical isolates from gulf corporation council countries. Antimicrob Resist Infect Control. 2012;1(1):26. doi:10.1186/2047-2994-1-26
8. Al Rasheed A, Yagoub U, Alkhashan H, et al. Prevalence and predictors of self-medication with antibiotics in Al Wazarat health center, Riyadh City, KSA. Biomed Res Int. 2016;2016:1–8. doi:10.1155/2016/3916874
9. Shibl A. The problem of antibiotic resistance. Arab Health Mag. 2007;12:20–21.
10. Balkhy HH, Assiri AM, Mousa HA, et al. The strategic plan for combating antimicrobial resistance in gulf cooperation council states. J Infect Public Health. 2016;9(4):375–385. doi:10.1016/j.jiph.2016.03.003
11. Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res Nurs Health. 2007;30(4):459–467. doi:10.1002/(ISSN)1098-240X
12. Lawshe C. A quantitative approach to content validity. Pers Psychol. 1975;28(4):563–575. doi:10.1111/j.1744-6570.1975.tb01393.x
13. Tilden VP, Nelson CA, May BA. Use of qualitative methods to enhance content validity. Nurs Res. 1990;39(3):172–175. doi:10.1097/00006199-199005000-00015
14. Fadare J, Tamuno I. Antibiotic self-medication among university medical undergraduates in northern Nigeria. J Public Health Epidemiol. 2011;3:217–220.
15. Hu Y, Wang X, Tucker JD, et al. Knowledge, attitude, and practice with respect to antibiotic use among chinese medical students: a multicentre cross-sectional study. Int J Environ Res Public Health. 2018;15(6):1165. doi:10.3390/ijerph15061188
16. Suaifan G, Shehadeh M, Darwish D, Al-Ije H, Darwish R. A cross-sectional study on knowledge, attitude and behavior related to antibiotic use and resistance among medical and non-medical university students in Jordan. Afr J Pharm Pharmacol. 2012;6:763–770.
17. Fejza A, Kryeziu Z, Kadrija K, Musa M. Pharmacy students’ knowledge and attitudes about antibiotics in Kosovo. Pharm Pract (Granada). 2016;14(1):715. doi:10.18549/PharmPract.2016.01.715
18. Abu-Helalah M, Alshraideh H, Hijazeen J, et al. Antibiotic use and misuse among university students in Jordan. Bull Environ Pharmacol Life Sci. 2014;4:62–71.
19. Saleem Z, Saeed H, Ahmad M, et al. Antibiotic self-prescribing trends, experiences and attitudes in upper respiratory tract infection among pharmacy and non-pharmacy students: a study from Lahore. PLoS One. 2016;11(2):e0149929. doi:10.1371/journal.pone.0149929
20. Pan H, Cui B, Zhang D, Farrar J, Law F, Ba-Thein W. Prior knowledge, older age, and higher allowance are risk factors for self-medication with antibiotics among university students in southern China. PLoS One. 2012;7(7):e41314. doi:10.1371/journal.pone.0041314
21. Lv B, Zhou Z, Xu G, et al. Knowledge, attitudes and practices concerning self-medication with antibiotics among university students in western China. Trop Med Int Health. 2014;19(7):769–779. doi:10.1111/tmi.12251
22. Ahmed A, Eltayeb I, Eltahir M. Patterns of self-medication with antibiotics in Khartoum State, Sudan. World J Pharm Res. 2014;3:678–692.
23. Scaioli G, Gualano MR, Gili R, Masucci S, Bert F, Siliquini R. Antibiotic use: a cross-sectional survey assessing the knowledge, attitudes and practices amongst students of a school of medicine in Italy. PLoS One. 2015;10(4):e0122476. doi:10.1371/journal.pone.0122476
24. Williams A, Crawford K. Self-medication practices among undergraduate nursing and midwifery students in Australia: a cross-sectional study. Contemp Nurse. 2016;52(4):410–420. doi:10.1080/10376178.2016.1197782
25. Xing Y, Kang R. Antibiotic abuse of 500 undergraduates. Chin J Sch Doctor. 2007;21:287–288.
26. Ahmad MS. A cross-sectional study on knowledge, attitude, and behavior related to antibiotic use among undergraduate medical students in a tertiary care medical college, Kashmir. Int J Basic Clin Pharmacol. 2015;4(6):1156–1162.
27. Bala R, Singh H, Kaur K, Girish P, Kohli K. Knowledge and attitude towards antimicrobial self medication usage: a cross sectional study among medical and nursing students. Int J Basic Clin Pharmacol. 2013;2(4):428–432. doi:10.5455/2319-2003.ijbcp20130816
28. Sharif SI, Sharif RS. Antibiotics use with and without a prescription in healthcare students. Am J Pharmacol Sci. 2013;1(5):96–99.
29. Shehadeh M, Suaifan G, Darwish RM, Wazaify M, Zaru L, Alja’fari S. Knowledge, attitudes and behavior regarding antibiotics use and misuse among adults in the community of Jordan. A pilot study. Saudi Pharm J. 2012;20(2):125–133. doi:10.1016/j.jsps.2011.11.004
30. Jorak A, Keihanian F, Saeidinia A, Heidarzadeh A, Saeidinia F. A cross sectional study on knowledge, attitude and practice of medical students toward antibiotic resistance and its prescription, Iran. Adv Environ Biol. 2014;8:675–681.
31. Humphreys H, Dillane T, O’Connell B, Luke LC. Survey of recent medical graduates’ knowledge and understanding of the treatment and prevention of infection. Ir Med J. 2006;99(2):58–59.
32. Ibia E, Sheridan M, Schwartz R. Knowledge of the principles of judicious antibiotic use for upper respiratory infections: a survey of senior medical students. South Med J. 2005;98(9):889–895. doi:10.1097/01.smj.0000177439.89762.ee
33. Hussain A, Alleyne S, Jenkins D. A survey of attitudes towards methicillin-resistant Staphylococcus aureus bacteraemias amongst United Kingdom microbiologists. J Antimicrob Chemother. 2010;65(2):347–349. doi:10.1093/jac/dkp456
34. Dutt H, Sarkhil M, Abdul M, Singh G. A comparative knowledge, attitude, and practice study of antimicrobial use, self-medication and antimicrobial resistance among final year students of MBBS, BDS, and BSc Nursing at a tertiary care hospital at Kannur. Natl J Physiol Pharm Pharmacol. 2018;8(9):1305–1311. doi:10.5455/njppp.2018.8.0518130052018
35. Brahmbhatt KR, Patel AB. Knowledge of antimicrobial resistance among undergraduate medical students in a medical college of Gujarat: institution based cross-sectional study. Int J Community Med Public Health. 2018;5(2):754–758. doi:10.18203/2394-6040.ijcmph20180263
36. Padmanabha T, Nandini T, Manu G, Savkar M, Shankar R. Knowledge, attitude and practices of antibiotic usage among the medical undergraduates of a tertiary care teaching hospital: an observational cross-sectional study. Int J Basic Clin Pharmacol. 2016;5:2432–2437.
37. Thriemer K, Katuala Y, Batoko B, et al. Antibiotic prescribing in DR Congo: a knowledge, attitude and practice survey among medical doctors and students. PLoS One. 2013;8(2):e55495. doi:10.1371/journal.pone.0055495
38. Abbo LM, Cosgrove SE, Pottinger PS, et al. Medical students’ perceptions and knowledge about antimicrobial stewardship: how are we educating our future prescribers? Clin Infect Dis. 2013;57(5):631–638. doi:10.1093/cid/cit370
39. Dyar OJ, Pulcini C, Howard P, Nathwani D; ESGAP (ESCMID Study Group for Antibiotic Policies). European medical students: a first multicentre study of knowledge, attitudes and perceptions of antibiotic prescribing and antibiotic resistance. J Antimicrob Chemother. 2014;69(3):842–846. doi:10.1093/jac/dkt440
40. Limaye D, Naware S, Bare P, et al. Knowledge, attitude and practices of antibiotic usage among students from Mumbai University. Int J Res Med Sci. 2018;6:1908–1912. doi:10.18203/2320-6012.ijrms20182270
41. Khan AKA, Banu G. Antibiotic resistance and usage-a survey on the knowledge, attitude, perceptions and practices among the medical students of a southern Indian teaching hospital. J Clin Diagn Res. 2013;7(8):1613–1616.
42. Virmani S, Nandigam M, Kapoor B, Makhija P, Nair S. Antibiotic use among health science students in an Indian University: a cross sectional study. Clin Epidemiol Glob Health. 2017;5(4):176–179. doi:10.1016/j.cegh.2017.04.005
43. Mukharjee SK, Mahmud I, Akter S, Hossain S. Knowledge, attitudes and practices regarding antibiotic use among the students of microbiology department at Noakhali Science and Technology University, Bangladesh. J Drug Deliv Ther. 2017;7(4):34–37.
44. James H, Handu SS, Al Khaja KA, Otoom S, Sequeira RP. Evaluation of the knowledge, attitude and practice of self-medication among first-year medical students. Med Princ Pract. 2006;15(4):270–275. doi:10.1159/000092989
45. Ahmad A, Khan MU, Patel I, Maharaj S, Pandey S, Dhingra S. Knowledge, attitude and practice of B.Sc. Pharmacy students about antibiotics in Trinidad and Tobago. J Res Pharm Pract. 2015;4(1):37–41. doi:10.4103/2279-042X.150057
46. Asogwa I, Offor S, Mbagwu H. Knowledge, attitude and practice towards antibiotics use among non-medical university students in Uyo, Nigeria. J Adv Med Pharm Sci. 2017;15(1):1–11.
47. Ohl CA, Luther VP. Health care provider education as a tool to enhance antibiotic stewardship practices. Infect Dis Clin North Am. 2014;28(2):177–193. doi:10.1016/j.idc.2014.02.001
48. Huang Y, Gu J, Zhang M, et al. Knowledge, attitude and practice of antibiotics: a questionnaire study among 2500 Chinese students. BMC Med Educ. 2013;13:163. doi:10.1186/1472-6920-13-99
49. Ganesh M, Sridevi S, Paul C. Antibiotic use among medical and para medical students: knowledge, attitude and its practice in a tertiary health care centre in Chennai – a scientific insight. Int J Sci Res. 2014;3(7):332–335.
50. Jamshed SQ, Elkalmi R, Rajiah K, et al. Understanding of antibiotic use and resistance among final-year pharmacy and medical students: a pilot study. J Infect Dev Ctries. 2014;8(6):780–785. doi:10.3855/jidc.3833
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
